Abstract
Purpose
Kasai portoenterostomy (KP) is the primary procedure for biliary atresia (BA). However, due to reports of poor outcomes of KP, primary liver transplantation (LT) is preferred in selected cases. In Japan, primary LT is limited with no study reports details, particularly regarding the indications. We conducted the first nationwide survey to assess the status of primary LT in Japan.
Methods
Questionnaires were sent to institutions where procedures other than KP were performed as the initial procedure for BA and registered to the Japan Biliary Atresia Registry. Parameters related to procedure selection were analyzed.
Results
Of 2895 patients registered (1989–2013), primary LT (n = 15) or exploratory laparotomy (EL) followed by LT (n = 9) without KP was performed in 24 cases (0.8%). The main reason for primary LT was late diagnosis, and for EL followed by LT, lack of fibrous tissue at the porta hepatis (ο-type). The prognoses of LT without KP was good.
Conclusion
Non-KP initial procedures were limited. Clear criteria regarding the timing of diagnosis or patient condition could not be determined. Reasons for not initially selecting KP varied, but late diagnosis was predominant. Further study is needed to create guidelines for the initial treatment of BA patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Kasai portoenterostomy (KP) has been accepted as the primary procedure for biliary atresia (BA) worldwide. In Japan, where KP originated, KP is the preferred procedure and is performed more often than in Western countries. In fact, the outcome of KP tends to be good in terms of native liver survival [1, 2]. Limited access to deceased donor liver transplantation (LT) was another reason for the priority of KP in Japan, where living donor LT (LDLT) account for more than 95% of all LTs. There have been reports that some factors, such as older age at KP, have a negative impact on KP outcomes [3]. If these factors are identified at the time of diagnosis, they may influence the decision for the selection of primary LT rather than KP, as reported previously [4]. In contrast, even relatively late KP has been reported to have good outcomes in some cases [5]. KP at 132 days of age has been reported to have a satisfactory result [6]. These reports suggest that even a late diagnosis cannot exclude the possibility of KP as the primary procedure. With the establishment of LT in Japan, especially with LDLT, the hurdles for LT in Japan are lower than ever before. So far, however, there is no consensus regarding the timeframe or under what conditions LT should be considered over KP as the primary procedure in Japan. As the first step toward defining the appropriate indications for LT without KP, the present status of primary LT in Japan should be clarified. The aim of this study was to identify the indications of primary LT for BA in Japan.
Methods and patients
BA patients who did not undergo KP as the initial surgical procedure were identified from the registry data of the Japan Biliary Atresia Registry (JBAR) containing data accumulated between 1989 and 2013. A questionnaire was sent to the institutions that treated these patients regarding the selection of primary LT or exploratory laparotomy (EL) followed by LT. In this study, the diagnosis of BA was defined based on macroscopic findings of the porta hepatis, with or without an intraoperative cholangiogram. The answers from the questionnaires were analyzed at Kumamoto University Hospital. This study was approved by the institutional review board of Kumamoto University Hospital (Kumamoto University Hospital IRB #827).
Results
A questionnaire was sent out to 16 facilities, and responses were received from 15 of them. A total of 2895 patients were identified in the registry from 1989 to 2013, and 24 patients (0.8%) underwent LT (n = 15) or EL (n = 9) followed by LT as the primary procedures (Table 1).
The patient demographics and characteristics are shown in Tables 2 and 3. In 15 patients with primary LT, all but 2 patients presented initially with the diagnosis of jaundice after 100 days of age. The youngest case in the primary LT group was 45 days old at the time of the first presentation and was initially diagnosed as primary sclerosing cholangitis (PSC), not BA. However, during the follow-up period, the patient became cirrhotic, LT was performed, and BA was definitively determined, both macroscopically and pathologically. Another patient who presented younger than 100 days of age in the primary LT group first visited a physician at 89 days of age for persistent jaundice. Eighty-nine days old is relatively young for patients in the group but a little older than the average of BA patient in Japan. As the standard for that institution, primary LT was chosen after obtaining informed consent from the parents. Primary LT, in this case, confirmed BA with liver cirrhosis macroscopically and pathologically. The case with the latest presentation was a girl who presented at 316 days old. This patient had been diagnosed with cytomegalovirus hepatitis in a foreign country and visited the institution 1 month later, after moving to Japan. The intrahepatic bile duct was dilated but there was no passage of the contrast dye to the extrahepatic bile duct in the percutaneous transhepatic cholangiogram. The finding of the liver biopsy was consistent with BA. LT was performed at day 484, after waiting with percutaneous transhepatic biliary drainage and for recovery of the hepatic steatosis of her mother, the living liver donor. All of the other 13 patients who underwent primary LT with delayed diagnosis after 100 days showed various degrees of symptoms and findings of hepatic failure, such as ascites, gastrointestinal bleeding, encephalopathy, growth inhibition, and no visualization of portal blood flow on ultrasonography or computed tomography, among others.
Nine patients underwent LT after EL without KP. In the 9 cases, the timing of the initial presentation varied from day 0 to 194. In 4 cases, the presentation was before day 100, and in the other 5 it was later (Table 3). The reason for the choosing EL as the primary procedure is more complicated than for primary LT cases. In the group with the age at initial presentation less than 100 days (n = 4), 2 patients had ο-type portal structure. The surgeons considered that ο-type portal structure might predict poor drainage of the bile after KP and that the trial of KP might cause difficulty in the following LT. In 1 case in the group less than 100 days old at presentation, BA had been suspected from birth, but pediatricians were reluctant to make a definitive diagnosis. Finally, it was diagnosed on day 107 by EL. At this point surgeons considered that the advanced hepatic damage might eventually require LT after KP, and they proceeded to perform the LT without KP. In the other patient who had undergone EL at 76 days old, surgeons found advanced liver damage with signs of portal hypertension. They tried dissecting the fibrous portal tissue, but they were unable to visualize biliary discharge. They decided not to anastomose the intestine and only placed a drainage tube. The patient underwent LT later, on day 186. Even though the date of EL was not particularly late in this case, liver cirrhosis had advanced significantly. In the other 5 cases of the EL group, the date of initial presentation was later than 100 days. In 4 of them, the EL revealed the definitive diagnosis of BA with advanced liver cirrhosis. For this reason, the surgeons elected to not perform KP at that time. In the other EL group patient with later presentation, the ο-type portal structure was determined during the EL at day 124. The patient underwent LT on day 168.
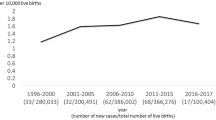
The total bilirubin (T-Bil) levels at the time of primary LT varied from 8.0 to 58.2 mg/dL, and the median was 18.5 mg/dL (Fig. 1). Pediatric End-stage Liver Disease (PELD) score ranged from 7 to 35, and the median at the time of primary LT was 18. In the EL group, the T-Bil level and PELD score at the time of LT after the EL ranged from 8.7 to 32.1 mg/dL (median: 18.5) and from 11 to 24 (median: 18), respectively. There were no differences in the T-Bil level or PELD score at the time of LT between the primary LT group and the EL followed by LT group.
Liver function. The total bilirubin (T-Bil) level and pediatric end-stage liver disease (PELD) score at the time of operation. One case was excluded from exploratory laparotomy (EL) and two cases from liver transplantation (LT) based on PELD score because the height or prothrombin time international normalized ration (PT-INR) were unknown
Regarding the outcomes of LT in the studied patients, 1 patient in each group did not survive the LT. The patient who did not survive in the primary LT group underwent LDLT at day 178 with a body weight of 7.2 kg. T-Bil was 17.7 mg/dL and the PELD score at the time of LT was 19. The donor was his mother, and the left lateral segment was used as the graft. The operation took more than 15 h, and this was longest in the primary LT group. Difficulty was caused by poor outcome of the portal vein reconstruction. The patient died on day 42 after the transplant due to portal vein thrombosis. The only other patient who did not survive was in the EL group, where the EL was performed on day 76 and KP was aborted due to advanced liver cirrhosis, as described earlier. The patient died 15 days after the transplant, but the detailed cause was not clear, in part due to the case having occurred 20 years ago.
Patient survival after primary LT or LT after EL was comparable to the outcome after failed KP in a similar age range (Fig. 2).
Discussion
This study revealed that the rate of liver transplantation without KP in Japan is quite small in comparison with other western countries. Only 24 cases were found, which is not sufficient for scientific analysis but is important as basic data for further discussion.
KP with or without LT can ensure the long-term survival of a patient with BA with a 90% probability [7]. Even though KP may not ultimately achieve native liver survival, it can extend the life of the native liver and with reasonable growth to allow the patient to better tolerate a subsequent LT. However, it is evident too that the intended outcome of KP, survival of the native liver, could not be achieved in at least 39% of all the cases in the JBAR [2]. For those patients, LT was the best option for survival.
In relatively old reports, the outcome of LT after failed KP was poorer than that of primary LT [8]. However, in other reports, in terms of patient and graft survival, the outcome after KP was not different from that of primary LT, indicating that KP could prevent or postpone LT [9]. However, there is still a concern regarding the higher rate of post-transplant complications, such as biliary complications and bowel perforation, in cases with a history of previous KP [10]. Therefore, if the expected possibility of a subsequent LT is high in selected patients, primary LT should be considered. From the JBAR data, KP at a later stage is associated with higher incidence of poor bile discharge [2], and in turn, a shorter time to the subsequent transplant. In contrast, however, there have been reports that even patients diagnosed with BA after 150 days of age can achieve complete clearance of jaundice and a longer survival with their native liver [6]. Because complete differentiation is impossible, an arbitrarily defined age timeframe or set of conditions should be recommended for deciding between primary LT and KP. Japanese pediatric surgeons have reached a consensus that KP should be performed for BA. As a base for the discussion on the necessity and feasibility of primary LT, the current status of primary LT in Japan should be clarified. We have had some cases of primary LT in our own institution, but, as with other institutions in Japan, the number is quite small. Originally, it was our intent to use the registry data to identify the patients not treated with KP as the initial procedure for BA patients in Japan. For the initial primary procedure for possible BA patients, we had expected two options, primary LT and KP, but we discovered that there was a third option: EL for the diagnosis and assessment of the liver condition before proceeding to LT without KP.
In the primary LT group, the most common reason for the procedure was the age of the patient at presentation. Most of the patients in this group had later presentations (after 100 days). Superina suggested that the discrimination point should be 75 days of age [4], and in our study all but one were included in this category. However, older age alone cannot definitively indicate primary LT, because late KP can provide long-term native liver survival. An additional reason for non-KP procedures was findings or symptoms that suggest advanced liver failure. This included ascites, encephalopathy, gastrointestinal bleeding, and poor portal vein flow or regurgitation of portal vein flow. Growth inhibition is one of the earliest indications of liver failure, but it was not enough to influence pediatric surgeons to proceed to primary LT.
Two patients were diagnosed with BA before the age of 100 days in this group. One of them had been misdiagnosed as having PSC, but the other showed prominent liver failure even at 89 days of age at first presentation. For these two cases, the surgeons and pediatricians considered that primary LT would be better than KP. This means that an age of less than 100 days cannot completely exclude the possible indication of primary LT. Even though Superina recommended the cut-off age of 75 days, in Japan, a slightly later margin of perhaps 100 days of age may be acceptable. Therefore, at this moment, age older than 100 days and/or findings of advanced liver failure may be relevant factors for pediatric surgeons to consider primary LT.
EL with intraoperative cholangiography is the final and definitive procedure for the diagnosis of BA. Usually, KP is performed immediately after the confirmation of BA. However, in this analysis, a total of 9 cases did not undergo KP, even after the definitive diagnosis of BA. The reason why surgeons chose not to proceed with KP in these patients was an important finding in this study, and late diagnosis with liver failure was the leading cause for this in this group, as well as in the primary LT group, but the anatomical findings of the porta hepatis was another factor that was considered. A lack of fibrous tissue at the porta hepatis, or ο-type portal structure, comprises 3.5% (109 in 3155 cases in which the type was specified) of the registered cases in the JBAR data [11]. The jaundice clearance rate in the registry is 35.8% in this type and is evidently poorer than the overall jaundice clearance rate of 60.9%. In the ο-type portal structure, theoretically, no ductular system exists at the porta hepatis, and this may indicate poor outcome, even though one report mentioned that duct diameter at the porta hepatis did not correlate with surgical outcome [12]. In this analysis, this reason for not-performing KP was found in 3 cases, and 2 of them were diagnosed before 100 days. Unfortunately, there is no consensus on how to handle ο-type BA, even in Japan. If there is no fibrous tissue at the porta hepatis, KP cannot be technically performed. However, in our personal experience, only dissection and removal of the peritoneal membranous tissue over the bifurcation of the portal vein and a subsequent anastomosis of the intestinal conduit can achieve biliary drainage in some ο-type cases. That may be the reason why such a low percentage of jaundice clearance has been reported in this type. Considering the poor outcome of this type of portal structure after KP, which exist despite the milder findings of liver failure or cirrhosis compared to other types, surgeons may select LT without KP. However, this is not yet the standard procedure accepted by all pediatric surgeons in Japan.
In addition to the consideration of the outcome of a KP, relatively harder access to LT for BA patients may influence the selection of the EL followed by LT. At Kumamoto University, the same team that performs the KP performs the pediatric LT. This is a unique situation. Most BA patients in Japan are transferred to the transplant team in the same or a different institution after a definitive diagnosis by EL. In this analysis, age, T-Bil level, and PELD score at LT were not different between the two groups, and this means that the timing of LT after EL can be selected properly with timely consultation with transplant centers. These findings may reflect the current trend of pediatric surgeons deciding the timing of LT in BA patients, for example, after a failed KP, after EL, and as primary LT. In Japan, compared to Europe and the United States, it is inevitable to rely on LDLT [2, 13]. When making the criteria for primary liver transplantation, donor availability in cases of DDLT should be added.
The number of patients with late KP (later than 91 days old) can be obtained from the registry data, but the final outcome of each patient was not reported. So, we have no exact data about the number of such patients who die without liver transplantation. However, we can make some speculations from the available data. The study period in this series is quite long, and the situation of pediatric LT in Japan has changed in this time frame. Since 1989, when the first LDLT was done in Japan, to 1998, when the national insurance system started to cover the cost of LDLT for pediatric patients (younger than 15 years), around 20 BA patients have died each year with their native livers [14]. In 1998, 117 new BA patients were registered to the registry, and late KP (later than 91 days old) was undergone in 22 patients (18.8% of total registered cases) [15]. Clearance of jaundice was obtained in 12 of those patients. In that year, no primary LT was registered. In 2013, the last year of the study period, late KP was undergone in 17 (18.3%) of the newly registered BA patients [16]. Jaundice was cleared in 7 of those patients. No primary LT was registered in 2013, either. Interestingly, in 2013, only one death with the native liver was registered. Since 2012, only one death has been registered each year in the registry data. So the rate of late KP does not significantly change during the study period, and the jaundice clearance rate also does not change prominently, but the death with native liver is almost null. This means that most failed KP cases, even though the KP is done late, may be salvaged with LT, which has resulted in a significant reduction in mortality rate with the native liver during the study period. This is caused by the establishment of LDLT in Japan. Deceased donor LT is still very limited, but pediatric cases are favored by splitting the deceased donor liver. Currently, in Japan the barrier to LT has dramatically been lowered in the last 30 years. In other words, this is the reason why primary LT has not gained popularity in Japan.
The next step of the research is the analysis of patients who were transplanted soon after KP (within a few months). This may present clinical or pathological findings that may indicate the avoidance of treatments that are “time-wasting as a result”. Complete discrimination will be impossible but tendencies favoring primary LT should be indicated. In this study, late presentation, advanced liver failure, and a special type of porta hepatis were shown for candidates of LT. Compared to western countries, it is possible to rely more on LDLT in Japan. If LDLT is possible, it presents less stress for the selection of the timing of LT. However, if LT is unavoidable, especially in the short term, KP should be avoided. This is the rationale in Japan for making the criteria for primary LT. Based on the basic data in this study, we would like to proceed to the next step.
Conclusions
From the registry data, patients who underwent LT as the initial or the subsequent procedure after EL comprised 0.8% of cases in Japan. The most common reason for selecting a procedure other than KP was older age at diagnosis. A determination of ο-type was a factor for consideration of not doing KP after EL. Even though it is a very limited possibility, in future studies, a consensus must be reached regarding the criteria for the selection of a procedure other than KP as the initial procedure for BA.
References
Shinkai M, Ohhama Y, Take H, Kitagawa N, Kudo H, Mochizuki K, Hatata T (2009) Long term outcome of children with biliary atresia who were not transplanted after the Kasai operation. %3e 20-year experience at a children’s hospital. J Pediatr Gastroenterol Nutr 48:443–450
Nio M (2017) Japanese biliary atresia registry. Pediatr Surg Int 33:1319–1325
Nio M, Wada M, Sasaki H, Tanaka H (2015) Effects of age at Kasai portoenterostomy on the surgical outcome: a review of the literature. Surg Today 45:813–818
Superina R (2017) Biliary atresia and liver transplantation: results and thoughts for primary liver transplantation in select patients. Pediatr Surg Int 33:1297–1304
Schoen BT, Lee H, Sullivan K, Ricketts RR (2001) The Kasai portoenterostomy: when is it too late? J Pediatr Surg 36:97–99
Bielamowicz A, Weitzman JJ, Alshak NS, Rosenthal P (1992) Successful late Kasai portoenterostomy. J Pediatr Gastroenterol Nutr 14:232–236
Nizery L, Chardot C, Sissaoui S, Capito C, Henrion-Caude A, Debray D, Girard M (2016) Biliary atresia: clinical advances and perspectives. Clin Res Hepatol Gastroenterol 40:281–287
Serinet MO, Wildhaber BE, Broué P, Lachaux A, Sarles J, Jacquemin E, Gauthier F, Chardot C (2009) Impact of age at Kasai operation on its results in late childhood and adolescence: a rationale basis for biliary atresia screening. Pediatrics 123:1280–1286
Sandler AD, Azarow KS, Superina RA (1997) The impact of a previous Kasai procedure on liver transplantation for biliary atresia. J Pediatr Surg 32:416–419
Neto JS, Feier FH, Bierrenbach AL et al (2015) Impact of Kasai portoenterostomy on liver transplantation outcomes: a retrospective cohort study of 347 children with biliary atresia. Liver Transpl 21:922–927
Japanese Biliary Atresia Society Workshop (2017) Biliary atresia national registration 2015 count result. J Jpn Soc Pediatr Surg 53:319–325 (in Japanese)
Baruah RR, Bhatnagar V, Agarwala S, Gupta SD (2015) Correlation of pre- and post-operative liver function, duct diameter at porta hepatis and porta fibrosis with surgical outcomes in biliary atresia. J Indian Assoc Pediatr Surg 20:184–188
Eurotransplant International Foundation. Statistics Report Library. Liver transplants in 2018, by country, by donor type, by organ combination. https://statistics.eurotransplant.org/. Accessed 10 Aug 2019
Japanese Biliary Atresia Society Workshop (2016) Biliary atresia national registration 2014 count result. J Jpn Soc Pediatr Surg 54:307–313 (in Japanese)
Japanese Biliary Atresia Society Workshop (2000) Biliary atresia national registration 1998 count result. J Jpn Soc Pediatr Surg 36:348–353 (in Japanese)
Japanese Biliary Atresia Society Workshop (2015) Biliary atresia national registration 2013 count result. J Jpn Soc Pediatr Surg 51:268–274 (in Japanese)
Acknowledgements
We would like to express our sincere gratitude to the Japan Biliary Atresia Society for supplying the registry data. In addition, we are deeply thankful for the cooperation of the institutions and the pediatric surgeons in gathering the patient data; Dr. Tatsuya Suzuki from Fujita Health University, Dr. Shigeru Ono from Jichi Medical University, Dr. Masato Shinkai from Kanagawa Children's Medical Center, Dr. Hideaki Okajima from Kyoto University, Dr. Taizo Furukawa from Kyoto Prefectural University of Medicine, Dr. Toshiharu Matsuura from Kyushu University, Dr. Mikihiro Inoue from Mie University, Dr. Akihide Tanano from Nagoya University, Dr. Satoshi Kondo from Nagoya City University, Dr. Mureo Kasahara from National Center for Child Health and Development, Dr. Kengo Nakaya from Niigata University, Takehisa Ueno from Osaka University, Dr. Hiroaki Kitagawa from St. Marianna University School of Medicine, Dr. Hiromu Tanaka from Tohoku University. We would like to thank Editage (https://www.editage.com) for English language editing.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (Kumamoto University Hospital IRB #827) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Uto, K., Inomata, Y., Sakamoto, S. et al. A multicenter study of primary liver transplantation for biliary atresia in Japan. Pediatr Surg Int 35, 1223–1229 (2019). https://doi.org/10.1007/s00383-019-04553-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-019-04553-7