Abstract
Purpose
There is a lack of data-driven, risk-adjusted mortality estimates for injured children outside of high-income countries (HIC). To inform injury prevention and quality improvement efforts, an upper middle-income country (UMIC) pediatric trauma registry was compared to that of a HIC.
Methods
Clinical data, injury details, and mortality of injured children (< 18 years) hospitalized in two centers (USA and South African (SA)) from 2013 to 2017 were abstracted. Univariate and multivariable analyses evaluated risk of mortality and were expressed as odds ratios (OR) with 95% confidence intervals (CI).
Results
Of 2089 patients, SA patients had prolonged transfer times (21.1 vs 3.4 h) and were more likely referred (78.2% vs 53.9%; both p < 0.001). Penetrating injuries were more frequent in SA (23.2% vs 7.4%, p < 0.001); injury severity (9 vs 4) and shock index (0.90 vs 0.80) were greater (both p < 0.001). SA utilized cross-sectional imaging more frequently (66.4% vs 37.3%, p < 0.001). In-hospital mortality was similar (1.9% SA, 1.3% USA, p = 0.31). Upon multivariable analysis, ISS > 25 [210.50 (66.0-671.0)] and penetrating injury [5.5 (1.3–23.3)] were associated with mortality, while institution [1.7 (0.7–4.2)] was not.
Conclusions
Despite transfer time, the centers demonstrated comparable survival rates. Comparison of registry data can alert clinicians to problematic practice patterns, assisting initiatives to improve trauma systems.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Surgical care is an indicator of the human, economic, and physical capital of a well-functioning healthcare system [1]. Trauma care is the surgical condition par excellence, best managed with a system capable of effective care delivery and promotion of its socio-political objectives. High-income countries (HICs) have deployed such systems, most notably the American College of Surgeons (ACS) trauma verification system, with positive results in public health and patient care arenas [2,3,4]. These examples, however, stand in the context of stable populations and well-defined burdens of trauma. It is unknown if these systems can be applied to low- or middle-income countries with young mobile populations, strained resources, and different profiles of trauma, “Appendix 1” [5].
Insufficient data limit the understanding of disease burden and outcomes in low- and middle-income country settings, but implementation of trauma registries will facilitate risk-adjusted estimates of patient outcomes. This study uses mortality rates, the fourth Lancet Commission on Global Surgery (LCoGS) indicator, to assess the quality of pediatric trauma care in a major South African trauma service compared to a trauma center in the US [6]. South Africa is an upper middle-income country (UMIC) with a relatively young population and huge discrepancies in wealth and access to health care. Like neighboring low- or middle-income countries, much of the population (40–50%) lives in rural areas but is beginning to urbanize rapidly. Children comprise almost one-third of the South African population and the burden of injury is high in this age group. The purpose of this study was to evaluate patient characteristics and outcomes using trauma registry data from a South African pediatric trauma center in comparison to a United States trauma center. We hypothesized that differences in injury patterns, practice, and outcomes would be identified and may be used to inform injury prevention and quality improvement.
Methods
This is a dual institution review and institutional review board approval was obtained prior to study at both sites. This study was performed at the Pietermaritzburg Metropolitan Trauma Service (PMTS), Pietermaritzburg, South Africa and at the Mayo Clinic (MC) in Rochester, Minnesota, United States. The trauma registries at both institutions were reviewed for the 5-year period, January 2013–December 2017 [7, 8]. The PMTS provides definitive trauma care to the city of Pietermaritzburg, the capital of KwaZulu-Natal (KZN) province, Fig. 1. It is one of the largest academic trauma centers in KZN which also serves as the referral center for 19 other rural hospitals within the province, with a total catchment population of over 3 million [9]. PMTS is not a level I trauma center and refers patients that meet transfer criteria to Durban, SA. Transfers occur for patients with neurosurgical emergencies and diversion due to hospital’s capacity. Mayo Clinic has both an ACS-verified adult and pediatric level I trauma center and is a quaternary referral center that serves predominantly a rural population.
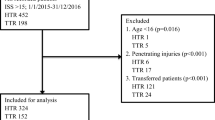
Patients evaluated by the pediatric trauma services at both centers were included in this study. Demographic data, admission physiology, and laboratory values were reviewed. Injury severity was measured for each patient using the Injury Severity Score (ISS), and admission Glasgow Coma Scale (GCS) were calculated. Details of the injury mechanism and 30-day mortality were recorded. Patients without an ISS were excluded from the primary outcome analysis, Fig. 2.
The primary outcome of this study was to determine whether the risk of pediatric trauma injury mortality was different between PMTS and MC after controlling for severity using ISS [10]. Secondary outcomes included duration of hospital stay, intensive care unit utilization and duration of stay, and duration of mechanical ventilation.
Continuous variables with normal distribution summarized with mean and standard deviation, while non-parametric continuous variables were summarized with medians, interquartile ranges (IQRs), and ranges; categorical variables were summarized with frequency counts and percentages. Patient characteristics and outcomes were compared by institution using Chi-square tests for categorical variables, independent t tests for continuous normally distributed variables, and Wilcoxon rank sum for continuous non-parametric variables. Multivariable logistic regression assessing for factors predictive of mortality was performed. Covariates were selected based on clinical relevance and significance (p < 0.05) on univariate analyses. The multivariable analysis results were expressed as odds ratios (ORs) with 95% confidence intervals (CIs) calculated using likelihood ratio tests. Model sensitivity and calibration were calculated. All data analyses were performed using JMP (SAS Institute Inc., Cary, NC).
Results
Overall cohort
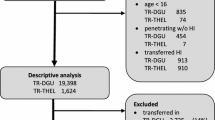
In this study, there were 2439 patients reviewed. A total of 346 patients (all from PMTS) did not have an ISS assigned and 4 patients missing age or with an inappropriate value (also from PMTS) were excluded. More than half of the missing ISS score occurred in 2014, and > 99% of missing ISS occurred before 2016 (trend < 0.0001), Fig. 2. Ultimately, 2089 patients were included for the primary outcome analysis. Among these, 656 were female (31%). The overall median [IQR] age was 9 [4–14] years. Overall median time from injury to hospital admission was 6.8 [2.2–21.2] hours. Broadly, patient injury mechanisms included blunt (n = 1753, 84%), penetrating (n = 280, 13%), and other (n = 56, 3%). There were 270 patients (13%) that were assaulted. Table 1 shows the specific injury mechanisms for the entire cohort. The median ISS for the entire cohort was 5 [4–9]. A total of 1010 patients (48%) received cross-sectional imaging and 512 patients (25%) required operative intervention. A total of 331 patients (16%) required ICU level care and the hospital duration of stay was 1 [1–3] days. Thirty-two patients (1.5%) expired within 30-days.
Comparison of PMTS and Mayo Clinic
There were 797 patients from PMTS and 1292 from the MC. An higher proportion of penetrating trauma occurred in PMTS (23% vs 7%, p < 0.001) compared to the MC and less blunt trauma was seen at PMTS (76% vs 89%, p < 0.0001). Differences in the specific injury patterns are demonstrated in Table 2. Notable differences included an increased frequency of pedestrian injuries in PMTS compared to MC (19.6% vs 2.6%, p < 0.0001) but there were fewer sport injuries at the PMTS compared to MC (< 1% vs 16%, p < 0.0001). There was an increased proportion of bite injuries in PMTS compared to MC (9% vs 1%, p < 0.0001). Finally there were no injuries related to all-terrain vehicles at PMTS, but 93 occurred at MC.
Comparison of pediatric trauma injury characteristics, clinical and laboratory values, hospital resource utilization and outcomes are reported in Table 3. There was a statistically but not clinically significant difference in age between patients at PMTS and MC (median age 9.8 vs 9.0 years, p = 0.0077), and no differences in sex were seen between institutions (p = 0.0761). The rate of assault was higher at PMTS compared to MC (23% vs 7%, p < 0.0001). Between centers, the median time from injury to hospital admission was prolonged in PMTS (21.1 vs 3.4 h, p < 0.0001). There was no difference between centers based on GCS but the ISS [IQR] was elevated in patients in PMTS compared to those in the MC (9 [4–10] vs 4 [4–9], p < 0.0001). The proportion of severely injured, however, was similar (3.4 in PMTS vs 3.5 in MC, p = 0.9077).
More patients received cross-sectional imaging at PMTS compared to those at MC (66% vs 37%, p < 0.0001), but they received operative intervention less frequently (19.7% vs 27.5%) and were less likely to be admitted to an intensive care unit (10.9% vs. 18.9%, p ≤ 0.0001 for both). Among only patients with penetrating injuries, overall CT rate was 25% (15% at MC and 30% at PMTS, p = 0.0055). The median hospital duration of stay was prolonged in PMTS compared to MC (1 [1, 2] vs 1 [0–4]) days. Despite these differences, the mortality rates were similar between centers (1.3% MC vs 1.9% PMTS, p = 0.31).
Results of the multivariable analysis for factors predictive of mortality
On regression, the following were independently associated with mortality [OR (95%CI)]: ISS > 25 [210.5 (66.0–671.0)] and penetrating injury [5.5 (01.3–23.3)]. Patient sex, age, institution [1.7 (0.7–4.2)], or operative intervention failed to show significance. Table 4. The sensitivity of the model (area under the curve) was 0.94 and the Hosmer–Lemeshow test indicated good fit (p = 0.62).
Discussion
South Africa has a significant burden of trauma affecting its young populace. While many of its patients arrive outside the “golden hour,” mortality rates are comparable on univariate and adjusted comparisons to an HIC. As expected, the comparison of these two trauma registries highlighted striking differences in the epidemiology of injury in each setting—South Africa had more penetrating injuries, more frequent pedestrian trauma, higher rates of interpersonal violence, and more injuries sustained after contact with wildlife. Given the differences in acuity and epidemiology of trauma in the South African setting, it was not surprising that resource utilization differed between PMTS compared to MC. The data provided from the trauma registry and benchmarking against an HIC not only provides actionable areas for prevention and practice improvement but demonstrates the importance of maintaining such registries.
Trauma registries in low- and middle-income countries are pivotal due to the large burden of disease in this setting. Globally, 950,000 children die each year as a result of injury or violence and 95% of these deaths occur outside of HICs [11]. In Africa, interpersonal violence mortality rates among males aged 0–15 years are more than double that of worldwide average [12]. Mortality estimates reported elsewhere in sub-Saharan Africa are high, from 5.5% to as high as 19%, and double that of HICs [13,14,15,16,17,18]. While the epidemiologic trends shown in this paper reflect these same conditions, the overall mortality seen in PMTS was similar to that of a HIC. These data suggest that outcomes are satisfactory for patients who are able to be treated definitively at PMTS. Since patients with severe head injury are transferred from PMTS for definitive management, it cannot be concluded that overall mortality is similar between UMIC and HIC pediatric trauma centers based on this study. The promising results with respect to PMTS, however, should prompt further research and investment in low- and middle-income trauma centers.
Trauma centers have the capacity and responsibility to lead change and influence policy. In PMTS, higher penetrating trauma, pedestrian injury, and animal attack rates demonstrated areas for primary prevention and advocacy. Penetrating injury rates at PMTS have in fact increased from 16.3% from 2012 to 2014 to 23.2% in our review and reflect an overall high incidence of penetrating trauma in sub-Saharan Africa [9, 19]. Violence prevention programs can better target populations where intentional injury burden is highest using data from this registry [20]. Road traffic accidents and resulting pedestrian injury remain a huge burden upon trauma systems in low- and middle-income countries, and our study was no exception with nearly 20% of injuries resulting from pedestrians injured by some form of motorized transport [21]. Surgeons have been important non-partisan actors pushing legislation to improve road safety in a number of HICs, and these data from PMTS provide important perspectives to local and national legislators [22]. Approximately one in every ten injuries in our study was secondary to animal encounter, mostly snake bites. This finding expectedly deviated from that seen in the comparison MC setting (where there are no indigenous venomous snakes). While no deaths in PMTS were secondary to snakebite, snake envenomation has been reported to have mortality rates as high as 2.3% and represents a neglected tropical disease that peaks from ages 1–15 [23, 24]. This again represents a center-specific area where prevention and quality improvement efforts could have real impacts on morbidity and mortality.
Resource utilization differed between the two centers, and CT scan use was greater at PMTS. To our knowledge, aside from this study and the aforementioned Zambian study, trauma registries have not been deployed in sub-Saharan Africa to examine resource utilization in trauma [27]. South Africa differs from many low- and middle-income countries in that its urban trauma centers have capabilities for advanced imaging. With ease of access to computed tomography comes increased utilization, as seen in the United States with respect to the diagnosis of blunt solid organ injury in pediatric trauma and acute appendicitis in children. Subsequently in the United States, efforts have been undertaken to reduce exposure to ionizing radiation for children and rates of CT use in pediatric trauma the United States have seen measured decrease [25]. Use of CT in pediatric trauma patients in South Africa requires further study to determine optimal utilization and the role of similar efforts to reduce ionizing radiation exposure for children, especially in the setting of greater penetrating trauma. Penetrating trauma usually necessitates exploration in the operating room, and non-operative management of childhood penetrating trauma, aside from select cases, has been discouraged in the HIC setting [26]. It is important to recognize, however, that the decision to forgo CT in pediatric trauma patients is dependent on the environment and coexisting resources. The findings of this study pertaining to CT use in PMTS will drive quality improvement initiatives to optimize use at the institution.
Comparison of trauma registry data has been a cornerstone of the ACS and World Health Organization efforts to improve trauma care nationally and internationally. Such benchmarking has demonstrated differences in outcomes that have led to coordinated efforts to improve patient care. For example, higher rates of mortality in traumatic brain injury in the United Kingdom compared to Australia led the National Health Service to refer such patients to dedicated neurosurgical centers [28]. This solution came after reviewing the data from poor-performing centers, which appeared to have less experience with such injuries compared to their Australian counterparts. Most comparative studies like this one have been in HICs. Haider et al. published a feasibility study of benchmarking trauma registry data from both an HIC and LMIC against the NTDB, showing that it was feasible [21]. In 2017, Spence et al. reported a comparison of trauma at Cape Town’s largest academic referral center against matched patients from the NTDB, showing that patients in South Africa with penetrating trauma did comparable to matched patients in the NTDB [20]. Their findings of poorer outcomes in severely head injured and blunt trauma patients have prompted the hospital to consider both its own management of such patients and potential preventative efforts such as stricter traffic laws and enforcement of seatbelt use. The successes and shortcomings of trauma centers can only be measured by both internal and external quality assessments. As this paper and others have shown, implementation of trauma registry systems, like those in Cape Town and PMTS, allows for such appraisals in the low- and middle-income country settings.
The results of this study must be interpreted in the context of its limitations. Our analysis was retrospective in nature and compared two different trauma settings. While an attempt was made to adjust for these differences, the pre-hospital care and trauma profile are vastly different between PMTS and MC. PMTS is also not a level-1 trauma center, and while this limitation is partially mitigated by adjusting for Injury Severity Score, there could be patients who were referred to a higher level of care not included in the PMTS cohort. In particular, the transfer of some neurological trauma cases likely left some deaths unaccounted for in our data. Thus, the findings regarding resource utilization and outcomes should be interpreted with some caution. Future studies will work to pool data collectively from the system to better account for all mortality.
We were also unable to look closely at complications and morbidity; and it is possible that the comparable mortality outcomes seen would not translate into similar morbidity. Prehospital deaths were not accounted for in this study though are expected to be greater in PMTS due to limitations in patient retrieval and prehospital care. Data from autopsies in the Transkei region of South Africa would support the high number of traumatic deaths seen in mortuaries. In a study of 594 child deaths, 2 out of every 3 children died as a result of traumatic injury [29]. Lack of pre-hospital care systems in low- and middle-income countries makes capturing pre-hospital deaths difficult, and the other papers looking at childhood mortality in injury in sub-Saharan Africa share this limitation. Future studies should aim to gather mortuary data from hospital catchment areas to supplement trauma registries. Last, the patients excluded due to missing ISS were concentrated in the earlier years, suggesting that oversight of the registry improved over the course of its implementation.
This study demonstrates the ability of trauma registries in a developing world surgical service to evaluate performance, alert clinicians to problematic practice patterns, and assist public health initiatives to reduce the disease burden of injury. They specifically facilitate measurement of mortality, one of the LCoGS indicators. Support of such registries furthers the WHO goal of establishing and improving trauma systems worldwide.
References
Farmer PE, Kim JY (2008) Surgery and global health: a view from beyond the OR. World J Surg 32:533–536. https://doi.org/10.1007/s00268-008-9525-9
West JG, Cales RH, Gazzaniga AB (1983) Impact of regionalization. The Orange County experience. Arch Surg Chic Ill 1960 118:740–744
MacKenzie EJ, Rivara FP, Jurkovich GJ et al (2006) A national evaluation of the effect of trauma-center care on mortality. N Engl J Med 354:366–378. https://doi.org/10.1056/NEJMsa052049
Gabbe BJ, Simpson PM, Sutherland AM et al (2012) Improved functional outcomes for major trauma patients in a regionalized, inclusive trauma system. Ann Surg 255:1009–1015. https://doi.org/10.1097/SLA.0b013e31824c4b91
World Bank Country and Lending Groups—World Bank Data Help Desk (2019) https://datahelpdesk.worldbank.org/knowledgebase/articles/906519. Accessed 9 Jan 2019
Meara JG, Leather AJ, Hagander L et al (2015) Global Surgery 2030: evidence and solutions for achieving health, welfare, and economic development. The Lancet 386:569–624
Laing GL, Bruce JL, Skinner DL et al (2014) Development, implementation, and evaluation of a hybrid electronic medical record system specifically designed for a developing world surgical service. World J Surg 38:1388–1397. https://doi.org/10.1007/s00268-013-2438-2
Laing G, Bruce J, Skinner D et al (2015) Using a hybrid electronic medical record system for the surveillance of adverse surgical events and human error in a developing world surgical service. World J Surg 39:70–79. https://doi.org/10.1007/s00268-014-2766-x
Manchev V, Bruce J, Oosthuizen G et al (2015) The incidence, spectrum and outcome of paediatric trauma managed by the Pietermaritzburg Metropolitan Trauma Service. Ann R Coll Surg Engl 97:274–278. https://doi.org/10.1308/003588414X14055925061595
Brown JB, Gestring ML, Leeper CM et al (2017) The value of the injury severity score in pediatric trauma: time for a new definition of severe injury? J Trauma Acute Care Surg 82:995–1001. https://doi.org/10.1097/TA.0000000000001440
Bickler SW, Rode H (2002) Surgical services for children in developing countries. Bull World Health Organ 80:829–835
World Health Organization (2002) The injury chart book: a graphical overview of the global burden of injuries. World Health Organization, Geneva
Peclet MH, Newman KD, Eichelberger MR et al (1990) Patterns of injury in children. J Pediatr Surg 25:85–90 (discussion 90–91)
Bayreuther J, Wagener S, Woodford M et al (2009) Paediatric trauma: injury pattern and mortality in the UK. Arch Dis Child Educ Pract Ed 94:37–41. https://doi.org/10.1136/adc.2007.132787
Kristiansen T, Rehn M, Gravseth HM et al (2012) Paediatric trauma mortality in Norway: a population-based study of injury characteristics and urban-rural differences. Injury 43:1865–1872. https://doi.org/10.1016/j.injury.2011.08.011
Abantanga FA, Mock CN (1998) Childhood injuries in an urban area of Ghana A hospital-based study of 677 cases. Pediatr Surg Int 13:515–518. https://doi.org/10.1007/s003830050387
Simon R, Gilyoma JM, Dass RM et al (2013) Paediatric injuries at Bugando Medical Centre in Northwestern Tanzania: a prospective review of 150 cases. J Trauma Manag Outcomes 7:10. https://doi.org/10.1186/1752-2897-7-10
Eighemhenrio A, Campbell F, Fred FE et al (2015) Paediatric trauma at a tertiary hospital in Niger-Delta, Nigeria: a 5-year review. East Cent Afr J Surg 20:66–72
Spence RT, Scott JW, Haider A et al (2017) Comparative assessment of in-hospital trauma mortality at a South African trauma center and matched patients treated in the United States. Surgery 162:620–627. https://doi.org/10.1016/j.surg.2017.04.024
Lasecki CH, Mujica FC, Stutsman S et al (2018) Geospatial mapping can be used to identify geographic areas and social factors associated with intentional injury as targets for prevention efforts distinct to a given community. J Trauma Acute Care Surg 84:70–74. https://doi.org/10.1097/TA.0000000000001720
Haider AH, Hashmi ZG, Gupta S et al (2014) Benchmarking of trauma care worldwide: the potential value of an international trauma data bank (ITDB). World J Surg 38:1882–1891. https://doi.org/10.1007/s00268-014-2629-5
Breen J (2004) Road safety advocacy. The BMJ 328:888–890
Herbert HK, van As AB, Bachani AM et al (2012) Patterns of pediatric injury in South Africa: an analysis of hospital data between 1997 and 2006. J Trauma Acute Care Surg 73:168–174. https://doi.org/10.1097/TA.0b013e31824d67c3
Ochola FO, Okumu MO, Mwangi GM et al (2018) Epidemiology of snake bites in selected areas of Kenya. Pan Afr Med J. https://doi.org/10.11604/pamj.2018.29.217.15366
Roudsari BS, Psoter KJ, Vavilala MS et al (2013) CT use in hospitalized pediatric trauma patients: 15-year trends in a level I pediatric and adult trauma center. Radiology 267:479–486. https://doi.org/10.1148/radiol.13120865
Dicker RA, Sartorelli KH, McBrids WJ, Vane DW (1996) Penetrating hepatic trauma in children: operating room or not? J Pediatr Surg 31:1189–1191 (discussion 1191–1193)
Seidenberg P, Cerwensky K, Brown RO et al (2014) Epidemiology of injuries, outcomes, and hospital resource utilisation at a tertiary teaching hospital in Lusaka, Zambia. Afr J Emerg Med 4:115–122. https://doi.org/10.1016/j.afjem.2014.01.006
Gabbe BJ, Biostat GD, Lecky FE et al (2011) The effect of an organized trauma system on mortality in major trauma involving serious head injury: a comparison of the United kingdom and victoria, australia. Ann Surg 253:138–143. https://doi.org/10.1097/SLA.0b013e3181f6685b
Meel BL (2003) Mortality of children in the Transkei region of South Africa. Am J Forensic Med Pathol 24:141–147. https://doi.org/10.1097/01.PAF.0128052262.54227.DD
Funding
The authors have no financial relationships relevant to this article to disclose.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All authors declare no conflicts of interest.
Informed consent
This research was reviewed by both the Mayo Clinic and the Biomedical Research Committee (BREC) of the University of KwaZulu-Natal and determined to be exempt from the requirement for IRB approval and informed consent (45 CFR 46.101, item 4).
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix 1
Appendix 1
The definitions of low-, middle-, lower middle-, upper middle-, and high-income countries are included below. These definitions are based upon Gross National Income (GNI) per capita using the World Bank Atlas method for the 2019 fiscal year. They can be found at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519.
Classification | World Bank definition |
|---|---|
Low income | Low-income economies are those with GNI per capita of $995 or less in 2017 |
Lower middle income | Lower middle-income economies are those with a GNI per capita of more than $995 but less than $3896 |
Middle income | Middle-income economies are those with a GNI per capita between $996 and $12,055 |
Upper middle income | Upper middle-income economies those with a GNI per capita of more than $3895 but less than $12,056 |
High income | High-income economies are those with a GNI per capita of $12,056 or more |
Rights and permissions
About this article
Cite this article
Traynor, M.D., Hernandez, M.C., Shariq, O. et al. Trauma registry data as a tool for comparison of practice patterns and outcomes between low- and middle-income and high-income healthcare settings. Pediatr Surg Int 35, 699–708 (2019). https://doi.org/10.1007/s00383-019-04453-w
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-019-04453-w