Abstract
Purpose
It is unclear whether simple diverticulectomy, rather than segmental bowel resection (SBR), is adequate treatment for gastrointestinal bleeding (GIB) secondary to Meckel diverticulum (MD). There is concern that ulcers in the adjacent bowel may continue to bleed if only the diverticulum is removed. This study seeks to determine if diverticulectomy is satisfactory treatment for bleeding MD.
Methods
A multi-institution, retrospective review was performed for patients with a diagnosis of MD and GIB who underwent simple diverticulectomy or small bowel resection. Exclusion criteria were comorbid surgical conditions and other causes of GIB. The primary outcome was post-operative bleeding during the initial hospitalization. Secondary outcomes were bleeding after discharge, transfusion or additional procedure requirement, re-admission, and overall complications.
Results
There were 59 patients who met study criteria (42 diverticulectomy, 17 SBR). One patient in the SBR group had early post-operative bleeding (p = 0.288). There was one re-admission (p = 0.288) and three total complications in the SBR group (p = 0.021). There were no cases of bleeding or other complications in the diverticulectomy group.
Conclusion
This study suggests that simple diverticulectomy is adequate for treatment of GIB caused by MD. Furthermore, diverticulectomy appears to have a lower overall complication rate.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Meckel diverticulum (MD) is the most common congenital anomaly of the gastrointestinal tract, resulting from persistence of the omphalomesenteric duct [1, 2]. The popular memory aid for MD is the rule of 2’s, which states that the diverticulum is present in 2% of the population, has 2:1 male predominance, becomes symptomatic by 2 years of age, is located within 2 feet of the ileocecal valve, tends to be 2 inches in length, and may possess two types of ectopic mucosa (gastric and pancreatic) [3]. According to St-Vil et al., in symptomatic MD there is a 3.5:1 male: female predominance and mean age of presentation is 5.5 years of age [1].
Gastrointestinal bleeding (GIB) is one of the most common presentations and is found in more than half of symptomatic, pediatric cases of MD [2]. The hemorrhage is thought to originate from the otherwise normal mucosa of the ileum which ulcerates and bleeds due to the acidic secretions from the heterotopic tissue within the MD [3, 4]. While it is agreed upon that management of bleeding MD involves surgical resection, there is debate as to whether diverticulectomy is acceptable or small bowel resection (SBR) is required. Advocates of SBR state that such a procedure prevents continued or recurrent gastrointestinal hemorrhage by removing the ulcerated ileum [2, 3] and ensuring that all of the ectopic mucosa is resected, particularly for MD with certain physical characteristics [5].
The study hypothesis is that diverticulectomy is sufficient to remove the ectopic mucosa and allow the ulcerated mucosa to heal with minimal risk of further bleeding. The purpose of this study is to demonstrate that diverticulectomy is satisfactory for treatment of bleeding MD and SBR is not required.
Methods
Following institutional review board approval at all participating institutions, a retrospective chart review was performed of all patients admitted to three, separate children’s teaching hospitals from 2002 to 2017 with a diagnosis of MD, using International Classification of Disease codes 751.0 (ICD, version 9) or Q43.0 (ICD, version 10). Inclusion criteria were patients with GIB who underwent simple diverticulectomy or small bowel resection for removal of a MD. Exclusion criteria were comorbid surgical disease (such as small bowel obstruction, volvulus, and/or perforated viscus), causes of bleeding other than MD (which included intussusception associated with MD), and patients with incomplete chart information. No age restriction was placed on patients who were enrolled in the study. All operations were performed by fellowship-trained, attending pediatric surgeons with prior experience performing Meckel diverticulectomy and small bowel resections. A total of 25 surgeons operated as part of the study. All surgeries were performed at the main campus of each respective children’s hospital. The decision to perform open or laparoscopic surgery, as well as diverticulectomy or small bowel resection, was entirely at the discretion of the operating surgeon.
The primary outcome was post-operative GIB prior to discharge from the hospital (“early bleeding”). Secondary outcomes were post-operative requirement for transfusion, repeat surgery and/or endoscopy during initial hospitalization, evidence of gastrointestinal hemorrhage following discharge (“long-term bleeding”), re-admission related to the MD (e.g., bleeding or post-operative complications), and overall post-operative events (the sum of the primary and secondary outcomes and any additional post-operative complications).
Data analysis
Observational statistics were collected for the patients. The follow-up period was measured as the time between patient surgery and patient chart review. The Kruskal–Wallis test (also known as the Mann–Whitney U test) was used to compare the two groups in terms of patient age at surgery, as well as follow-up period. Fisher’s exact test was used to compare the SBR and diverticulectomy groups, for the primary and secondary outcomes. All testing was two-tailed and evaluated at the type I error rate of α = 0.05 level of statistical significance.
Data collection and statistical analysis were performed in Excel (Microsoft Corporation, Redmond, WA).
Results
A total of 249 patients with MD were identified. Of these, 187 were excluded due to no evidence of GIB or the presence of comorbid conditions. Finally, an additional 18 were excluded as a result of incomplete data, leaving a total of 59 patients for study inclusion (Fig. 1).
There were 42 patients who underwent diverticulectomy and 17 receiving small bowel resection (Table 1). Of patients receiving diverticulectomy, 38 had stapled diverticulectomy while 4 had sharp resection of the diverticulum with sutured closure of the bowel.
There was no difference between the two groups in terms of patient age at the time of surgery (p = 0.875). Similarly, there was no difference between the two groups in the length of follow-up period (p = 0.514) with average follow-up being 2123 days (approximately 5.8 years) for the diverticulectomy group and 2043 days (approximately 5.6 years) for the SBR group.
There was one patient in the SBR group (5.9%) who met the primary outcome. This patient had a small amount of hematochezia post-operatively, but did not require transfusion or additional intervention. The bleeding spontaneously resolved prior to discharge. There were no patients in the diverticulectomy group with early bleeding. Using Fisher’s Exact test, there was no difference between the SBR and diverticulectomy groups for the primary outcome (p = 0.288).
No patient in either group required transfusion or an additional procedure or surgery. Similarly, no patient from either group was readmitted for long-term bleeding. However, there were two patients in the SBR group with post-operative complications not related to bleeding. One patient, who underwent laparoscopic SBR, developed an abscess at the umbilicus, which required incision and drainage performed as an outpatient. A second patient, who initially underwent laparotomy and SBR, presented with a small bowel obstruction (SBO) approximately 2 years following initial surgery. This ultimately required repeat laparotomy. There were no re-admissions or complications in the simple diverticulectomy group. SBR, therefore, has a re-admission rate of 5.9%, which was not statistically different from the diverticulectomy group (p = 0.288).
However, the cumulative post-operative event rate was 17.6% for the SBR group. This value represents a statistically significant difference from the diverticulectomy group (p = 0.021).
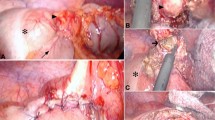
The majority of cases (52, 88%) were performed laparoscopically (Fig. 2). The distribution of open and laparoscopic cases demonstrated that 76% of SBR were performed laparoscopically and 93% of diverticulectomy cases were performed laparoscopically. This difference was not statistically significant (p = 0.176).
Discussion
In cases of bleeding MD, it has been advocated that to reduce the risk of ongoing or recurrent hemorrhage, not only should the MD itself be removed, but SBR should be performed to resect the bleeding ileum and ensure that all heterotopic mucosa is removed [2, 3, 5]. This study demonstrated that the outcomes between the SBR and diverticulectomy groups were comparable in terms of both early and late bleeding, re-admission, transfusion requirements, and need for additional procedures. There was one episode of early hemorrhage in the SBR group and one re-admission for SBO in the same group. The overall complication rate was higher in the SBR group and this relationship was statistically significant.
When specifically examining those patients in the SBR group who comprised the complications, some conclusions may be drawn. The three complications were early bleeding, wound infection requiring I&D, and SBO. The early bleeding potentially represented blood which was already present within the lumen of the gastrointestinal tract. The early hematochezia following surgery thus may have been “old” and did not represent additional, post-operative bleeding. Alternatively, the bleeding may have been actual post-operative bleeding from the anastomotic staple line. The wound infection potentially was due to an increased infection risk associated with performing SBR, which requires opening of the small bowel with associated spillage of enteric contents. Finally, the SBO occurred in a patient whose initial surgery was performed via laparotomy, which placed him at higher risk of SBO than if he had undergone laparoscopy [6]. Therefore, it was likely the form of surgery, open over laparoscopy that predisposed this patient to post-operative complication.
The results of this study are clinically significant primarily in that they allow for the avoidance of small bowel resection. Performing diverticulectomy over SBR avoids creation of a gastrointestinal anastomosis which is associated with shorter length of stay [4] and may reduce operative time, overall cost, time to return of bowel function, and infection. As an aside, the rate of anastomotic leak appears to be comparable between SBR and diverticulectomy [1, 7,8,9,10]. However, there may be a higher bleeding risk from the longer staple line involved in a stapled small bowel anastomosis. Furthermore, diverticulectomy is likely more easily performed laparoscopically. Finally, infection risk is predicted to also be lower due to the lack of spillage of enteric contents which inevitably occurs during small bowel anastomosis creation.
The primary outcome for this study was post-operative recurrent or ongoing hemorrhage during the initial hospital stay. This was chosen because patients with gastrointestinal hemorrhage who have recurrent bleeding tend to experience this as an early post-operative event. Among patients with upper gastrointestinal hemorrhage controlled endoscopically, re-bleeding occurs within 72-h of intervention [11, 12]. Intuitively, if re-bleeding from the injured mucosa is to occur it will occur shortly after surgery, as there is still injured, bleeding intestinal mucosa. Patients are typically observed in the hospital post-operatively, such that any early bleeding should be detected during the initial hospitalization.
Technique
A study from 2011 demonstrated that 76% of patients who underwent surgery for problems related to MD received laparotomy. Of these, 27.3% had bleeding MD (but it is unclear which percentage of that subset underwent laparotomy) [13]. A full 88% of the patients in this study underwent laparoscopic surgery (the majority using a stapler), highlighting the trend toward minimally invasive approaches. Laparoscopic Meckel diverticulectomy has been demonstrated by multiple studies to be safe [14,15,16,17,18,19], and this present study represents one of the largest case series to date.
The diverticulectomy may be performed intracorporeally or extracorporeally. In the former method, a laparoscopic stapler is inserted into the abdomen and the diverticulum removed under direct vision. In the latter technique, the MD is exteriorized (most commonly via the umbilical incision) and the diverticulectomy is performed [3, 20]. This technique easily allows for stapled or sutured diverticulectomy. Single-port techniques have been described [21].
For all methods of diverticulectomy, it is recommended that the bowel is stapled or sutured transversely (perpendicular to the long axis of the bowel) to minimize narrowing of the intestinal lumen [22].
Laparoscopic-stapled diverticulectomy was the most commonly performed surgery in this study and it is the authors’ preferred technique due to the ease of performance and avoidance of opening the bowel. In some cases, SBR will be mandatory, such as for gangrenous bowel or intestinal perforation. As such, these patients were excluded from this study. Patients in whom there is concern that diverticulectomy will excessively narrow the lumen of the bowel are not necessarily obligated to receive SBR. In these cases, a sharp diverticulectomy with closure of the bowel in a Heineke–Mikulicz fashion may be the procedure of choice [3, 14]. However, a small group of patients with a very short MD that has a broad and thick base may still require a small bowel resection.
Due to its multi-institutional nature, this work represents one of the largest studies to date of bleeding Meckel diverticulum. However, one limitation of this study is that follow-up data were only collected from the hospital where the surgery was performed. Given that the primary outcome dealt with hemorrhage which occurred during the initial hospitalization, concerns about data integrity and follow-up are somewhat allayed. Additionally, the retrospective nature of the study means that there may be selection bias present. As the operating surgeon was able to choose the operative technique, it is possible that more stable patients (or patients with less pre-operative blood loss) were selected for one surgical approach over another. Likewise, the fact that study conclusion favored diverticulectomy over SBR and the surgeons predominantly chose diverticulectomy as their surgical approach increases the probability of a type I error. Lastly, the number of patients excluded due to incomplete data was larger than the authors would have liked. With the available information, it is impossible to tell how the exclusion of those patients biased the study, if at all.
Conclusion
We conclude that diverticulectomy, whether laparoscopic or open, is a safe treatment for bleeding MD. This approached is favored over SBR as it has a lower overall complication rate and avoids creation of a gastrointestinal anastomosis, eliminates the contaminated surgical field, may be easily performed laparoscopically, and is likely faster.
Abbreviations
- MD:
-
Meckel diverticulum
- GIB:
-
Gastrointestinal bleeding
- SBR:
-
Small bowel resection
- ICD:
-
International Classification of Disease
References
St-Vil D, Brandt ML, Panic S et al (1991) Meckel’s diverticulum in children: a 20-year review. J Pediatr Surg 26:1289–1292
Yahchouchy E (2001) Meckel’s diverticulum. J Am Coll Surg 192:658–662. https://doi.org/10.1016/S1072-7515(01)00817-1
Brown RL, Azizkhan RG (1999) Gastrointestinal bleeding in infants and children: Meckel’s diverticulum and intestinal duplication. Semin Pediatr Surg 8:202–209
Robinson JR, Correa H, Brinkman AS, Lovvorn HN (2017) Optimizing surgical resection of the bleeding Meckel diverticulum in children. J Pediatr Surg. https://doi.org/10.1016/j.jpedsurg.2017.03.047
Varcoe RL, Wong SW, Taylor CF, Newstead GL (2004) Diverticulectomy is inadequate treatment for short Meckel’s diverticulum with heterotopic mucosa. ANZ J Surg 74:869–872. https://doi.org/10.1111/j.1445-1433.2004.03191.x
Duepree H-J, Senagore AJ, Delaney CP, Fazio VW (2003) Does means of access affect the incidence of small bowel obstruction and ventral hernia after bowel resection? J Am Coll Surg 197:177–181. https://doi.org/10.1016/S1072-7515(03)00232-1
Cullen JJ, Kelly KA, Moir CR et al (1994) Surgical management of Meckel’s diverticulum. An epidemiologic, population-based study. Ann Surg 220:564–568 (discussion 568–9)
Bruce J, Krukowski ZH, Al-Khairy G et al (2001) Systematic review of the definition and measurement of anastomotic leak after gastrointestinal surgery. Br J Surg 88:1157–1168. https://doi.org/10.1046/j.0007-1323.2001.01829.x
Stone PA, Hofeldt MJ, Campbell JE et al (2004) Meckel diverticulum: ten-year experience in adults. South Med J 97:1038–1041. https://doi.org/10.1097/01.SMJ.0000125222.90696.03
Hyman N, Manchester TL, Osler T et al (2007) Anastomotic leaks after intestinal anastomosis: it’s later than you think. Ann Surg 245:254–258. https://doi.org/10.1097/01.sla.0000225083.27182.85
Maggio D, Barkun AN, Martel M et al (2013) Predictors of early rebleeding after endoscopic therapy in patients with nonvariceal upper gastrointestinal bleeding secondary to high-risk lesions. Can J Gastroenterol 27:454–458
Ouali El S, Barkun A, Martel M, Maggio D (2014) Timing of rebleeding in high-risk peptic ulcer bleeding after successful hemostasis: a systematic review. Can J Gastroenterol Hepatol 28:543–548
Ruscher KA, Fisher JN, Hughes CD et al (2011) National trends in the surgical management of Meckel’s diverticulum. J Pediatr Surg 46:893–896. https://doi.org/10.1016/j.jpedsurg.2011.02.024
Teitelbaum DH, Polley TZ, Obeid F (1994) Laparoscopic diagnosis and excision of Meckel’s diverticulum. J Pediatr Surg 29:495–497
Shalaby RY, Soliman SM, Fawy M, Samaha A (2005) Laparoscopic management of Meckel’s diverticulum in children. J Pediatr Surg 40:562–567. https://doi.org/10.1016/j.jpedsurg.2004.11.032
Prasad TRS, Chui CH, Jacobsen AS (2006) Laparoscopic-assisted resection of Meckel’s diverticulum in children. J Soc Laparoendosc Surg (Society of Laparoendoscopic Surgeons) 10:310–316
Chan KW, Lee KH, Mou JWC et al (2008) Laparoscopic management of complicated Meckel’s diverticulum in children: a 10-year review. Surg Endosc 22:1509–1512. https://doi.org/10.1007/s00464-008-9832-0
Palanivelu C, Rangarajan M, Senthilkumar R et al (2008) Laparoscopic management of symptomatic Meckel’s diverticula: a simple tangential stapler excision. J Soc Laparoendosc Surg (Society of Laparoendoscopic Surgeons) 12:66–70
Papparella A, Nino F, Noviello C et al (2014) Laparoscopic approach to Meckel’s diverticulum. World J Gastroenterol 20:8173–8178. https://doi.org/10.3748/wjg.v20.i25.8173
Chan KWE, Lee KH, Wong HYV et al (2014) Laparoscopic excision of Meckel’s diverticulum in children: what is the current evidence? World J Gastroenterol 20:15158–15162. https://doi.org/10.3748/wjg.v20.i41.15158
Cobellis G, Cruccetti A, Mastroianni L et al (2007) One-trocar transumbilical laparoscopic-assisted management of Meckel’s diverticulum in children. J Laparoendosc Adv Surg Tech 17:238–241. https://doi.org/10.1089/lap.2006.0036
Alemayehu H, Stringel G, Lo IJ et al (2014) Laparoscopy and complicated meckel diverticulum in children. J Soc Laparoendosc Surg (Society of Laparoendoscopic Surgeons) 18:e2014.00015. https://doi.org/10.4293/JSLS.2014.00015
Acknowledgements
No funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant conflicts of interest.
Rights and permissions
About this article
Cite this article
Glenn, I.C., el-shafy, I.A., Bruns, N.E. et al. Simple diverticulectomy is adequate for management of bleeding Meckel diverticulum. Pediatr Surg Int 34, 451–455 (2018). https://doi.org/10.1007/s00383-018-4239-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-018-4239-z