Abstract
Objectives
This study reviews the results of our previously described modification of the minimally invasive (Nuss) procedure for correction of pectus excavatum. It utilizes a subxyphoid incision with central fixation to maximize safe bar passage and minimize bar displacement.
Methods
Consecutive patients corrected with the modified Nuss procedure between 2010 and 2015 form the basis of this study.
Results
During the study period, 73 patients had correction of their pectus excavatum by the modified Nuss procedure, utilizing subxyphoid incision and central fixation. Average age was 14.3 (range 8–19). 54 patients were male, 19 female. The average Haller index was 4.3 (range 3.2–7.2). No episodes of cardiac perforation, hemothorax or significant pneumothorax were recorded. Bar displacement occurred in two patients (2.7%) with one late recurrence after bar removal.
Conclusions
Our modification of the Nuss procedure is effective at preventing intrathoracic complications and cardiac perforation. Central fixation had a lower rate of bar displacement compared to published reports. Additional efforts are needed to further reduce bar displacement.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pectus excavatum is the most common anterior chest wall deformity affecting approximately 1 in 400 live births with a male-to-female ratio of approximately 4:1 [1]. Correction is largely undertaken for symptoms of shortness of breath or chest pain. In addition, imaging demonstrating a significant Haller index (usually > 3.2) and ECHO abnormalities of cardiac compression or valvular deformities are indications for operative intervention [2]. There are two standard approaches to its repair—the open repair (Ravitch) [3], and the Nuss procedure [4]. The latter has had several modifications [5], including one we reported which involves a subxyphoid incision to elevate the sternum to safely pass the bar and three-point fixation [6]. At the time of bar passage, sutures are looped around the bar through the subxyphoid incision and sewn to the costal margin in an effort to limit cephalad displacement. It is our operational design to avoid cardiac perforation which has been documented in patients undergoing the Nuss procedure, and to limit the incidences of bar displacement, recurrence, and need for subsequent reoperation [5, 7]. This study is a compilation of our results since reporting this modification of the Nuss procedure.
Methods
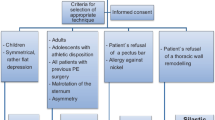
Consecutive patients from 2010 to 2015 who underwent surgical intervention by the senior surgeon (S. Bond) for pectus excavatum are included in the study. Some of the patients are those whose operation was performed in our initial experience and description of the operation (2010–2012) [6]. Age, gender, the presence or absence of symptomatology, including shortness of air, palpatations, and chest pain were tabulated for each patient. All patients underwent echocardiography and CT scanning of the chest. Pulmonary function tests were done selectively. Operative indications were a Haller index of greater than 3.2, with cardiac compression on CT scan, or echocardiography. Patients were given the option of Ravitch procedure or the modified Nuss with central incision and 3-point fixation previously described [6]. A subxyphoid incision was used to facilitate passage of the pectus bar without thoracoscopy. Three incisions are made, two lateral and one subxyphoid. The sternum is lifted up, and a heavy clamp is passed from the left lateral incision through the appropriate interspace to the subxyphoid incision. An umbilical tape is passed from the subxyphoid incision to the left lateral incision. Likewise, an instrument is passed from the right lateral incision to the subxyphoid incision and umbilical tape is transferred from the subxyphoid incision to the right lateral incision. We now have an umbilical tape connecting both lateral incisions behind the sternum. The tunnel is then dilated. Following the dilators removal, the umbilical tape, which is still behind the sternum, is grasped through the subxyphoid incision, and two heavy number one absorbable sutures are passed around it with the needles intact (Fig. 1). The pectus bar is then passed using the umbilical tape to guide it. The bar is flipped and secured laterally. Following the lateral stabilization, the two subxyphoid sutures which are now around the bar are secured to the costal margins and tied providing three-point fixation in an attempt to limit the displacement of the pectus bar which is usually cephalad.
Modified Nuss bars were left in place for 2 years. All patients were corrected with a single bar. Ravitch bars were removed after 6 months to 1 year. Intraoperative complications of cardiac perforation, pneumothorax, hemothorax, or bar infections were recorded. Long-term complications of bar shifting and recurrence were also noted.
Results
During the study period, 105 total patients underwent operative correction of their pectus excavatum by modified Nuss or Ravitch procedure. The average age of repair is 14.3 years. Symptoms of chest pain or shortness of air were present in approximately 56% of patients. The mean Haller index was 4.3. All patients demonstrated cardiac compression on CT scan or ECHO. During the time period, a total of 73 patients underwent a modified Nuss procedure, and 32 elected to have a Ravitch procedure performed. No instances of hemothorax or cardiac perforation were noted. Some small post-operative pneumothoraces were present but no patients required a chest tube (Table 1). All patients have subsequently had their bar removed. In the modified Nuss group, there were two instances of bar displacement after 6 months, requiring revision. One was removed and corrected with a Ravitch operation. The other underwent a redo Nuss procedure. Both with satisfactory results. There was another recurrence at 1.5 years following the removal of the pectus bar. That patient has not undergone reoperation because cardiac compression is no longer demonstrated.
Discussion
This study summarizes our last 6 years of operative intervention for pectus excavatum. Both open and minimally invasive operations were performed and offered to most patients. The open (Ravitch) procedure requires a longer, more prominent incision. This is offset by a shorter time until bar removal. Many of the patients who choose the Ravitch procedure are adolescent males who are actively involved in high school sports. We have felt that contact sports such as football and wrestling are prohibited when a pectus bar is in place. Wanting to resume full activity without restriction they choose the Ravitch over the modified Nuss. Uniformly these patients have been happy to get back to full activity. The central scar is not a concern as they have chosen a larger scar in lieu of a shorter duration of bar placement. In addition, patients who have an asymmetrical depression or a one-sided depression with contralateral carinatum deformity are probably the best served by an open procedure since the sternum can be modified to better accommodate the discrepancy. Additionally, the perichondrium can be shortened on the side that is protruding forward to additionally correct the sternal tilt. There was no difference in length of stay or pain scores in our series which is similar to prior publications comparing the Ravitch and Nuss procedures [8,9,10]. The senior author feels that both operations have merit, and should continue to be taught in pediatric surgical fellowships and offered to patients with pectus excavatum.
Overall, the subxyphoid incision appears to be safer than what is reported in the literature for many of the thoracoscopic-guided bar placements. We had small pneumothoraces, none of which required a chest tube. There were no incidences of hemothorax and most importantly no incidences of cardiac perforation. In most patients, the subxyphoid incision allows direct digital contact with the large clamps as they are placed from the left-sided chest incision and guided to the midline. This limits the possibility of cardiac injury. We did, however, have two episodes of bar displacement despite central fixation. Our displacement rate of 2.7% was lower compared with other studies of 7% [11] and 5.7% [2]. These appear to be gradually occurring, non-traumatic and may coincide with the dissolution of the absorbable subxyphoid sutures. It has been described in the literature that adolescent males of older age have significant chest wall musculature, and were most likely to displace their pectus bars [12]. That was not our experience as both of these patients, one male and one female, had very slight build. While our slip rate is recorded at only 2.7%, central fixation did not completely remove this complication. Both of these patients required revision of their initial procedures and now have satisfactory results. Authors have used placement of bar stabilizers to reduce the incidence of bar displacement. This, however, has not eliminated this complication [2].
If those who are more prone to bar migration could be predicted, one could envision additional modifications to eliminate bar displacement. Placing permanent sutures through the subxyphoid incision around the bar and securing it to the lower ribs may help to prevent cephalad migration. The limitation of this is that upon bar removal one may have to reopen all three incisions to facilitate bar removal. Currently, only two lateral incisions are opened to extract the bar.
In summary, our method of subxyphoid incision with central fixation as a modification of the Nuss procedure has proved effective in avoiding the immediate complications of pneumothorax, hemothorax and cardiac perforation. We have been successful in limiting bar displacement, and further consideration should be given to additional modifications, possibly central fixation with permanent sutures, especially if those patients prone to bar displacement can be identified.
References
Cartoski MJ, Nuss D, Goretsky MJ et al (2006) Classificaiton of the dysmorphology of pectus excavatum. J Pediatr Surg 41(9):1573–1581
Kelly RE, Goretsky MJ, Obermeyer R et al (2010) 21 years experience with minimally invasive repair of pectus excavatum by the Nuss procedures in 1215 patients. Ann Surg 252:1072–1081
Ravitch MM (1949) The operative treatment of pectus excavatum. Ann Surg 129:429–44
Nuss D, Kelly RE Jr et al (1998) A 10-year review of a minimally invasive technique for the correction of pectus excavatum. J Pediatr Surg 33:545–55
Ohno K, Nakamura T, Azuma T et al (2009) Modification of the Nuss procedure for pectus excavatum to prevent cardiac perforation. J Pediatr Surg 44:2426–2430
Bond SJ, Nagaraj HS (2013) Correction of pectus excavatum through a minimally invasive approach with subxyphoid incision and three-point fixation. J Thorac Cardiovasc Surg 146(5):1294–1296
Johnson WR, Fedor D, Singhal S (2013) A novel approach to eliminate cardiac perforation in the Nuss procedure. Ann Thorac Surg 95:1109–1111
Lam MWC, Klassen AF, Montogomery CJ (2008) Quality-of-life outcomes after surgical correction of pectus excavatum: a comparison of the Ravitch and Nuss procedures. J Pediatr Surg 43:819–825
Antonoff MB, Erickson AE, Hess DJ et al (2009) When patients choose: comparison of Nuss, Ravitch, and Leonard procedures for primary repair of pectus excavatum. J Pediatr Surg 44:1113–1119
Nasr A, Fecteau A, Wales P (2010) Comparison of the Nuss and the Ravitch procedure for pectus excavatum repair: a meta-analysis. J Pediatr Surg 45L:880–886
Kelly RE, Mellins RB, Shamberger RC et al (2013) Multicenter study of pectus excavatum, final report: complications, static/exercise pulmonary function, and anatomic outcomes. J Am Coll Surg 217:1080–1089
Kim DM, Hwang JJ, Lee MK et al (2005) Analysis of the Nuss procedure for pectus excavatum in different age groups. Ann Thorac Surg 80:1037–1077
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to report.
Funding
There is no funding provided for this work.
Additional information
University of Louisville IRB Approval Number: 16.0515.
Rights and permissions
About this article
Cite this article
Bond, S.J., Rapstine, E. & Bond, J.M. Results of pectus excavatum correction using a minimally invasive approach with subxyphoid incision and three-point fixation. Pediatr Surg Int 34, 75–78 (2018). https://doi.org/10.1007/s00383-017-4195-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-017-4195-z