Abstract
Purpose
Few reports have focused on the management of congenital tracheal stenosis (CTS) in the neonatal period. The aim of this study was to determine appropriate management strategies for CTS in the neonatal period.
Methods
The medical records of eight neonatal patients with CTS at a single institution between January 2007 and December 2016 were retrospectively reviewed.
Results
Three patients with frequent ventilatory insufficiency despite assisted ventilation underwent surgical intervention (balloon tracheoplasty: n = 1, slide tracheoplasty: n = 2). Ventilatory insufficiency improved after surgery in all three patients. One patient who underwent slide tracheoplasty died due to non-airway-related causes. Observation or conservative management was performed in five patients with minimal respiratory symptoms or stable ventilation under assisted ventilation. All five patients were safely managed non-operatively in the neonatal period.
Conclusion
Depending on the severity of ventilatory insufficiency, there are two management strategies for CTS in the neonatal period. Surgical intervention, such as balloon tracheoplasty or slide tracheoplasty, is indicated for patients with unstable ventilatory status despite assisted ventilation. Observation or conservative management is a more suitable option for neonates with stable ventilation.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Congenital tracheal stenosis (CTS) is characterized by narrowing of the tracheal lumen, most commonly secondary to complete tracheal cartilage rings and absence of the membranous trachea [1]. Although rare, when it does occur, it often causes life-threatening respiratory insufficiency. Various surgical procedures for CTS have been reported, and slide tracheoplasty for long-segment CTS described by Tsang [2] and Grillo [3] has become a standard surgical procedure, which has been shown to greatly improve outcomes. However, the mortality rate of patients with CTS who undergo tracheal reconstruction, including various surgical procedures, before the age of 1 month is reportedly very high (73%) [4]. Therefore, management of CTS in the neonatal period remains a difficult challenge, and the indications of surgical intervention and appropriate surgical procedures for CTS in the neonatal period are not clarified.
The present study analyzed the clinical features and outcomes of patients diagnosed with CTS in the neonatal period. The aim of this study was to determine appropriate management strategies for CTS in the neonatal period.
Materials and methods
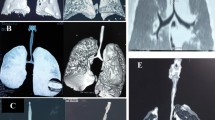
This study was performed with the approval of the institutional review board (approval number: R28-18) and complied with the Helsinki Declaration of 1964 (revised 2013). The medical records of eight patients with CTS managed in the neonatal period at a single institution between January 2007 and December 2016 were reviewed retrospectively. Patients who were diagnosed with CTS in the neonatal period at other institutions and managed at our institution after infancy were excluded from this study. All patients underwent rigid or flexible bronchoscopic examination in the neonatal period and were diagnosed with CTS associated with complete tracheal rings. All cases were assessed by 3-dimensional computed tomography. The information collected included patient demographics (sex, gestational age, birth weight, and associated anomalies), respiratory status (respiratory symptoms and ventilator dependence), computed tomography findings (minimum diameter and length of stenotic trachea), details of management in the neonatal period, complications, and mortality. In this study, long-segment tracheal stenosis was diagnosed when the stenotic trachea encompassed more than 30% of the total tracheal length. All results are expressed as medians (range); statistical evaluation could not be performed because of the small number of patients.
Surgical techniques
Balloon tracheoplasty
The procedure is performed under general anesthesia using Storz rigid ventilating bronchoscopy. A balloon catheter developed for percutaneous transluminal angioplasty is inserted through the stenotic site under bronchoscopy. Under fluoroscopy, the stenotic site is gradually dilated to 5.5 mm, splitting the complete tracheal rings. An endotracheal tube with an inner diameter of 3.0 mm (outer diameter of 4.4 mm) is passed through the stenotic site after the procedure.
Slide tracheoplasty
The technique of slide tracheoplasty performed at our institution has been described in detail in previous publications [5, 6]. The procedure is performed under cardiopulmonary bypass initiated through a median sternotomy. The stenotic trachea is circumferentially dissected and divided transversely a few millimeters below the midpoint of the stenotic trachea. The proximal and distal segments are incised along the posterior and anterior aspects. The entire oblique circumference of the proximal and distal tracheal segments is anastomosed with interrupted 5–0 absorbable sutures.
Results
Clinical characteristics
Eight neonatal patients (2 male, 6 female) who had CTS were included in this study. The median gestational age was 36 weeks (range 34–42 weeks), and median birth weight was 2.175 kg (range 1.758–3.320 kg). Five patients (62.5%) had cardiovascular anomalies, four (50.0%) had respiratory anomalies, and four (50.0%) had gastrointestinal anomalies as comorbidities. Details of the associated anomalies are shown in Table 1. Four patients (50.0%) had severe respiratory distress on admission, and required endotracheal intubation and assisted ventilation. There were no respiratory symptoms in the remaining four patients (50.0%), and CTS was diagnosed incidentally during screening or treatment of the other associated anomalies. Surgical intervention during the neonatal period was required in three of the patients, while the remaining were managed non-operatively.
Surgical intervention group (n = 3)
The clinical characteristics of the surgical intervention group are summarized in Table 2. Two patients developed respiratory distress and required tracheal intubation and assisted ventilation 0 and 5 days after birth. Another patient with ileal atresia who underwent ileostomy the day after birth required assisted ventilation postoperatively. All three patients developed frequent ventilatory insufficiency despite assisted ventilation in the neonatal period. Patient 1, weighing 1.844 kg at birth, had short-segment tracheal stenosis near the tracheal bifurcation. She underwent balloon tracheoplasty 19 and 20 days after birth, following which an endotracheal tube with an inner diameter of 3.0 mm was passed through the stenotic site. She was successfully extubated 17 days after surgery with improvement in her respiratory symptoms. However, due to the persistence of the stenosis postoperatively, as seen on computed tomography, she underwent slide tracheoplasty 3 months after birth. Patient 2, weighing 3.320 kg at birth, had short-segment tracheal stenosis above the tracheal bronchus. She underwent slide tracheoplasty 10 days after birth. She was successfully extubated 21 days after surgery with improvement in her respiratory symptoms. Patient 3, weighing 1.780 kg at birth, had long-segment tracheal stenosis and right pulmonary agenesis, and underwent slide tracheoplasty 20 days after birth. Although her ventilatory insufficiency improved after surgery, she died due to intestinal failure-related liver disease and septic shock 108 days after surgery.
Non-operative management group (n = 5)
The clinical characteristics of the non-operative management group are summarized in Table 2. Three of the patients had no respiratory symptoms, and observation management was attempted. The other two patients developed respiratory distress that required tracheal intubation and assisted ventilation 8 and 25 days after birth, respectively. Fortunately, they could conservatively keep stable ventilatory status under assisted ventilation and were successfully extubated 36 and 58 days after birth, respectively. The median follow-up period in this group was 534 days (range 63–1147 days). Two of the patients with no respiratory symptoms in the neonatal period developed respiratory distress as they grew older, and underwent slide tracheoplasty at 1 and 2 years of age. There were no deaths in this group.
Discussion
In neonates with CTS, the broad spectrum of length and degree of tracheal stenosis leads to a wide variability in clinical presentations. Some patients develop severe respiratory distress within a few days of life, requiring tracheal intubation and assisted ventilation. Others have no or minimal respiratory symptoms. They are often diagnosed with CTS incidentally during screening or treatment for other associated anomalies. In recent years, with advances in diagnostic techniques, such as 3-dimensional computed tomography, and the widespread recognition of CTS, the number of patients diagnosed with CTS in the neonatal period is increasing. However, there are few detailed reports focusing on the management strategies for CTS in the neonatal period. Therefore, we analyzed the clinical features and outcomes of patients diagnosed with CTS in the neonatal period. The present study describes three clinical factors that can serve to establish possible management strategies for CTS in the neonatal period: (1) indications for surgical intervention, (2) details of surgical intervention, and (3) details of non-operative management.
In children of all ages, the indications for surgical intervention for CTS are based on: (1) the clinical respiratory situation, and (2) the severity of tracheal stenosis [7, 8]. Since surgical intervention for CTS in the neonatal period is challenging, we propose rigid indications for surgical intervention in neonatal CTS patients. In the present study, the indication for surgical intervention for CTS in the neonatal period was unstable ventilatory status despite assisted ventilation. Furthermore, we focused on the minimum diameters of the stenotic trachea on computed tomography as more objective findings in surgical intervention group. In all three patients who underwent surgical intervention, the minimum diameters of the stenotic trachea on computed tomography were less than 2.0 mm. These findings are similar with Li’s report [9] that the minimum diameters of stenotic trachea were 1.5 and 2.0 mm from their experience with two slide tracheoplasties in the neonatal period. Although it is essential to note that trapped secretions around the stenotic site may artificially increase the degree of stenosis, we suggest that it is necessary to pay attention to computer tomographic observation of the minimum diameter of the stenotic trachea as being 2.0 mm or less.
Selection of the appropriate surgical procedure in each case depends on the following: (1) the extent and location of the tracheal stenosis, (2) the patient’s body weight, and (3) the presence of associated anomalies. Balloon tracheoplasty can be performed without cardiopulmonary bypass, and stable ventilation can be obtained immediately after stenting the stenotic site. Therefore, we consider balloon tracheoplasty to be a feasible surgical procedure for low-body weight neonates with short-segment tracheal stenosis, such as patient 1 in this study. In this patient, although the stenotic region persisted after balloon tracheoplasty and subsequent tracheal reconstruction became necessary, balloon tracheoplasty has the advantage of avoiding tracheal reconstruction and cardiopulmonary bypass in low-body weight neonates, and can, hence, serve as an effective bridging therapy for future open tracheal reconstruction. Ono et al. [10] reported three neonates with short-segment tracheal stenosis who underwent balloon tracheoplasty. Two of their patients were successfully extubated following balloon tracheoplasty alone, while the third patient required subsequent tracheal reconstruction. Although slide tracheoplasty using cardiopulmonary bypass in the neonatal period remains a difficult challenge, it is also a feasible procedure for tracheal reconstruction. In this study, two patients safely underwent slide tracheoplasty, with subsequent improvement in ventilatory insufficiency postoperatively (patient 3 died due to other non-airway-related causes). Manning et al. [11] from Cincinnati Children’s Hospital Medical Center proposed that slide tracheoplasty offers two advantages in all CTS cases, regardless of the length of stenosis. First, distribution of the suture line over a greater tracheal length reduces the risk of restenosis in short-segment tracheal stenosis. Second, with this procedure, anastomotic tension, which is a factor related to the occurrence of restenosis, can be decreased in long-segment tracheal stenosis. We believe that these theories are more effectively adapted for reconstruction of the small trachea in neonates.
Non-operative management includes observation management and conservative management. Observation management is indicated for patients with minimal respiratory symptoms in the neonatal period. Moreover, conservative management should be attempted in patients with stable ventilatory status under assisted ventilation even if they cannot be weaned from ventilatory support and extubated in the neonatal period. In this study, five patients with long-segment tracheal stenosis and stable respiratory status were safely managed non-operatively in the neonatal period. However, patient 3 with no respiratory symptoms at birth developed ventilatory insufficiency after treatment of the other associated anomaly and required surgical intervention in the neonatal period. In patients with severe tracheal stenosis, great caution is necessary during non-operative management. Furthermore, two of the patients subsequently required tracheal reconstruction after the age of 1-year. Cheng et al. [12] suggested the following as selection criteria for non-operative management at all pediatric ages: (1) CTS is not of the long-segment type, and (2) the diameter of the most stenotic segment is more than 60% that of the normal tracheal diameter at the same age. Since there is often a tendency to develop respiratory symptoms in association with an increase in activity, careful observation of these patients is also necessary after the neonatal period, especially in patients with long-segment tracheal stenosis.
A limitation of this study is that the study population was very small. Further studies including a larger number of participants are needed to clarify the management strategies that are feasible for patients diagnosed with CTS in the neonatal period.
In conclusion, management strategies for CTS in the neonatal period depend on the severity of ventilatory insufficiency. We recommend surgical intervention, such as balloon tracheoplasty or slide tracheoplasty, for patients with ventilatory instability despite undergoing tracheal intubation and assisted ventilation. In our opinion, non-operative management should be attempted in patients with stable ventilation in the neonatal period.
References
Hofferberth SC, Watters K, Rahbar R, Fynn-Thompson F (2015) Management of congenital tracheal stenosis. Pediatrics 136:e660–e669. doi:10.1542/peds.2014-3931
Tsang V, Murday A, Gillbe C, Goldstraw P (1989) Slide tracheoplasty for congenital funnel-shaped tracheal stenosis. Ann Thorac Surg 48:632–635
Grillo HC (1994) Slide tracheoplasty for long-segment congenital tracheal stenosis. Ann Thorac Surg 58:613–619 (discussion 619–621)
Chiu PP, Kim PC (2006) Prognostic factors in the surgical treatment of congenital tracheal stenosis: a multicenter analysis of the literature. J Pediatr Surg 41:221–225. doi:10.1016/j.jpedsurg.2005.10.043
Tsugawa C, Nishijima E, Muraji T, Satoh S, Takamizawa S, Yamaguchi M, Yoshimura N, Oka S, Kimura K (2003) Tracheoplasty for long segment congenital tracheal stenosis: analysis of 29 patients over two decades. J Pediatr Surg 38:1703–1706
Morita K, Yokoi A, Fukuzawa H, Hisamatsu C, Endo K, Okata Y, Tamaki A, Mishima Y, Oshima Y, Maeda K (2016) Surgical intervention strategies for congenital tracheal stenosis associated with a tracheal bronchus based on the location of stenosis. Pediatr Surg Int 32:915–919. doi:10.1007/s00383-016-3928-8
Antón-Pacheco JL, Cano I, García A, Martínez A, Cuadros J, Berchi FJ (2003) Patterns of management of congenital tracheal stenosis. J Pediatr Surg 38:1452–1458
Terada M, Hotoda K, Toma M, Hirobe S, Kamagata S (2009) Surgical management of congenital tracheal stenosis. Gen Thorac Cardiovasc Surg 57:175–183. doi:10.1007/s11748-008-0399-4
Li X, Cheng LC, Cheung YF, Lun KS, Chau KT, Chiu SW (2010) Management of symptomatic congenital tracheal stenosis in neonates and infants by slide tracheoplasty: a 7-year single institution experience. Eur J Cardiothorac Surg 38:609–614. doi:10.1016/j.ejcts.2010.03.011
Ono S, Maeda K, Baba K, Usui Y, Tsuji Y, Kawahara I, Fukuta A, Sekine S (2014) Balloon tracheoplasty as initial treatment for neonates with symptomatic congenital tracheal stenosis. Pediatr Surg Int 30:957–960. doi:10.1007/s00383-014-3571-1
Manning PB, Rutter MJ, Lisec A, Gupta R, Marino BS (2011) One slide fits all: the versatility of slide tracheoplasty with cardiopulmonary bypass support for airway reconstruction in children. J Thorac Cardiovasc Surg 141:155–161. doi:10.1016/j.jtcvs.2010.08.060
Cheng W, Manson DE, Forte V, Ein SH, MacLusky I, Papsin BC, Hechter S, Kim PC (2006) The role of conservative management in congenital tracheal stenosis: an evidence-based long-term follow-up study. J Pediatr Surg 41:1203–1207. doi:10.1016/j.jpedsurg.2006.03.046
Acknowledgements
This research received no specific Grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Morita, K., Maeda, K., Yabe, K. et al. Management of congenital tracheal stenosis in the neonatal period. Pediatr Surg Int 33, 1059–1063 (2017). https://doi.org/10.1007/s00383-017-4137-9
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-017-4137-9