Abstract
Purpose
The aim of this study was to determine the appropriate surgical intervention strategies for congenital tracheal stenosis (CTS) associated with a tracheal bronchus based on the location of stenosis.
Methods
The medical records of 13 pediatric patients with CTS associated with a tracheal bronchus at a single institution between January 2006 and December 2015 were retrospectively reviewed.
Results
Type 1: tracheal stenosis above the right upper lobe bronchus (RULB) (n = 1). One patient underwent slide tracheoplasty and was successfully extubated. Type 2: tracheal stenosis below the RULB (n = 7). Tracheal end-to-end anastomosis was performed before 2014, and one patient failed to extubate. Posterior–anterior slide tracheoplasty was performed since 2014, and all three patients were successfully extubated. Type 3: tracheal stenosis above the RULB to the carina (n = 5). One patient underwent posterior–anterior slide tracheoplasty and was successfully extubated. Two patients with left–right slide tracheoplasty and another two patients with tracheal end-to-end anastomosis for the stenosis below the RULB could not be extubated.
Conclusion
Tracheal end-to-end anastomosis or slide tracheoplasty can be selected for tracheal stenosis above the RULB according to the length of stenosis. Posterior–anterior slide tracheoplasty appears feasible for tracheal stenosis below the RULB or above the RULB to the carina.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
A tracheal bronchus is defined as a congenital anomaly in which the right upper lobe bronchus (RULB) arises directly from the trachea and above the carina in the narrow sense [1]. Patients with congenital tracheal stenosis (CTS) occasionally have this anomaly, and the incidence of a tracheal bronchus in patients with CTS ranges between 11.9 % [2] and 24.7 % [3]. Since the stenotic trachea is commonly found near the RULB, from the viewpoint of preservation of the RULB, tracheal reconstruction for CTS associated with a tracheal bronchus remains a difficult challenge. Although various surgical procedures have been reported, the appropriate surgical intervention strategies are still controversial.
The present study analyzed the surgical outcomes of tracheal reconstruction in pediatric patients with CTS associated with a tracheal bronchus. The aim was to determine the appropriate surgical intervention strategies for CTS associated with a tracheal bronchus based on the location of stenosis.
Materials and methods
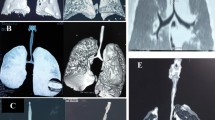
This study was performed with the approval of the institutional review board (R27-21) and complied with the Helsinki Declaration of 1964 (revised 2013). Fifty-one pediatric patients with CTS underwent tracheal reconstruction at a single institution between January 2006 and December 2015, and 14 patients (27.5 %) had CTS associated with a tracheal bronchus. All patients preoperatively underwent bronchoscopic examination and were diagnosed with CTS associated with complete tracheal rings. All cases of CTS associated with a tracheal bronchus were classified into the following three types based on the location of stenosis on preoperative enhanced three-dimensional computed tomography findings according to the classification proposed by Speggiorin and Torre [2]: type 1, tracheal stenosis above the RULB (n = 1); type 2, tracheal stenosis below the RULB (n = 8); and type 3, tracheal stenosis above the RULB to the carina (n = 5) (Fig. 1). One patient with type 2 who had severe cerebral hypoxia before surgery was excluded from this study. The medical records of the 13 included patients were reviewed retrospectively. The information collected included patient demographics (sex, age, and body weight at operation), preoperative status (respiratory symptoms, ventilator dependence, and cardiopulmonary bypass dependence), associated cardiovascular anomalies, location and length of stenosis, details of tracheal reconstruction, morbidity and mortality, duration of postoperative hospital stay, and postoperative tracheostomy dependence.
Classification of congenital tracheal stenosis associated with a tracheal bronchus based on the location of stenosis on preoperative three-dimensional computed tomography findings. a Tracheal stenosis (arrow) above the right upper lobe bronchus (RULB) (type 1). b Tracheal stenosis (arrow) below the RULB (type 2). c Tracheal stenosis (arrows) above the RULB to the carina (type 3)
Surgical technique
We generally performed tracheal end-to-end anastomosis for short segment tracheal stenosis less than 30 % of the tracheal length, and slide tracheoplasty for long segment tracheal stenosis over 30 % of the tracheal length.
Tracheal end-to-end anastomosis
Endotracheal intubation above the RULB was performed for perioperative ventilation. Through a median sternotomy, cardiopulmonary bypass was initiated. The stenotic trachea below the RULB to the carina was circumferentially dissected and resected. The proximal and distal tracheal segments were anastomosed with interrupted 5-0 absorbable sutures with care not to occlude the orifice of the RULB.
Slide tracheoplasty
Cardiopulmonary bypass was initiated in the same manner as for tracheal end-to-end anastomosis. The stenotic trachea was circumferentially dissected and divided transversely a few millimeters below the midpoint. The proximal and distal segments were incised in the posterior and anterior aspects or in the left and right aspects with care not to injure the RULB. An inverted Y-shaped incision of the carina was added in patients with carinal stenosis. The entire oblique circumference of the proximal and distal tracheal segments was anastomosed with interrupted 5-0 absorbable sutures.
Results
Clinical characteristics
Thirteen patients (eight male, five female) who had CTS associated with a tracheal bronchus were included in this study. The median age at operation was 4.0 months (range 0.3–110 months). The median body weight at operation was 4.97 kg (range 3–26.5 kg). All patients showed severe dyspnea or recurrent respiratory tract infections before surgery. Nine patients (69.2 %) were ventilator-dependent preoperatively, and one patient (7.7 %) was cardiopulmonary bypass-dependent preoperatively. Nine patients (69.2 %) had cardiovascular anomalies. The clinical and operative data of the patients with each type are summarized in Tables 1, 2.
Type 1: tracheal stenosis above the RULB (n = 1)
One patient had a localized tracheal stenosis above the RULB. Since the stenotic trachea was distant from the RULB, typical posterior–anterior slide tracheoplasty could be performed. The patient’s postoperative course was uneventful. She was successfully extubated 21 days after surgery, and her respiratory symptoms were improved.
Type 2: Tracheal stenosis below the RULB (n = 7)
Tracheal end-to-end anastomosis was performed before 2014, and posterior–anterior slide tracheoplasty was performed since 2014. Dehiscence of the anastomotic site occurred in one patient who underwent tracheal end-to-end anastomosis, and re-anastomosis was performed. He required tracheostomy postoperatively due to tracheomalacia at the re-anastomotic site. Another six patients were successfully extubated at a median of 11 days (range 7–21 days) after surgery, and their respiratory symptoms were improved. There were no deaths.
Type 3: tracheal stenosis above the RULB to the carina (n = 5)
Tracheal end-to-end anastomosis was performed in two patients. They had severe tracheal stenosis below the RULB and mild tracheal stenosis above the RULB. One patient underwent resection of the severe stenotic trachea below the RULB only and tracheal end-to-end anastomosis. Extubation failed due to deterioration of the remaining tracheal stenosis above the RULB. Another patient underwent not only resection of the severe stenotic trachea below the RULB, but also release from the stenosis above the RULB with incision of the left aspect and oblique tracheal end-to-end anastomosis. He failed to extubate due to stenosis of the anastomotic site and required balloon dilatation of the anastomotic site. He was extubated at 33 days after surgery. Slide tracheoplasty was performed in three patients. Two patients underwent left–right slide tracheoplasty. They required tracheostomy due to severe tracheomalacia at the anastomotic site or a remaining complete tracheal ring above the anastomotic site. One patient underwent posterior–anterior slide tracheoplasty, and he was successfully extubated 7 days after surgery, and his respiratory symptoms were improved. There were no deaths.
Discussion
Slide tracheoplasty for long-segment CTS described by Tsang [4] and Grillo [5] has been widely accepted and has become a standard surgical procedure in addition to tracheal end-to-end anastomosis for short-segment CTS. However, the appropriate surgical intervention strategies for CTS associated with a tracheal bronchus are still not clear. One of the common reasons for this is that various types have been reported in CTS associated with a tracheal bronchus. Therefore, we simply classified CTS associated with a tracheal bronchus into three types based on the location of stenosis and then analyzed the surgical outcomes of tracheal reconstruction for each type. To our knowledge, this is the first systematic proposal of the appropriate surgical intervention strategies for CTS associated with a tracheal bronchus based on the location of stenosis.
Tracheal stenosis above the RULB was rare in patients with CTS associated with a tracheal bronchus in this study (7.1 %), and the present result is in line with that of the largest previous series (5.3 %) [3]. Since the stenotic trachea is not associated with the carina, unlike other types, tracheal reconstruction for CTS of this type is simple. We can perform tracheal end-to-end anastomosis or slide tracheoplasty for this type according to the length of stenosis, as long as we avoid occluding the orifice of the RULB.
We performed tracheal end-to-end anastomosis for tracheal stenosis below the RULB before 2014, and many authors reported similar procedures [3, 6]. More recently, although the length of stenosis was short, we performed slide tracheoplasty for this type, and respiratory symptoms were improved in all three patients. In tracheal end-to-end anastomosis for this type, since the orifice of the distal tracheal stump is small, the orifice of the anastomotic site also tends to be small. On the other hand, slide tracheoplasty offers an advantage by enlarging the orifice of the anastomotic site to avoid failure of extubation due to stenosis of the anastomotic site in patients with severe tracheal stenosis. There are two common reasons for this. First, the tension of the anastomosis causing the stenosis of the anastomotic site can be decreased in slide tracheoplasty [7]. Second, the stenosis of the anastomotic site is distributed obliquely in slide tracheoplasty, rather than circumferentially as in tracheal end-to-end anastomosis [7].
Tracheal stenosis above the RULB to the carina is the most complex type for tracheal reconstruction, and high complication and postoperative tracheostomy-dependent rates were found in this study. The present study revealed two important points for tracheal reconstruction for this type. First, the stenotic trachea with complete tracheal rings should be completely reconstructed. If tracheal stenosis above the RULB remains, deterioration of the stenosis above the RULB occurs after surgery due to edema of the tracheal mucosa, which prevents extubation. Second, posterior–anterior slide tracheoplasty is a simple and effective procedure for this type, as for long-segment CTS without a tracheal bronchus. Some authors noted that this type was considered a relative contraindication for posterior–anterior slide tracheoplasty because the suture lines were near the orifice of the RULB [8], and Elliott et al. reported the left–right slide tracheoplasty procedure [9]. Although left–right slide tracheoplasty has the advantage of avoiding distortion of the orifice of the RULB, details of the surgical outcomes have not been reported. One patient had severe tracheomalacia after left–right slide tracheoplasty and required tracheostomy in the present study. Few reports describe etiology of tracheomalacia after left–right slide tracheoplasty, and we assume that there are two reasons why severe tracheomalacia can occur in left–right slide tracheoplasty. First, the transverse figure-eight deformity of the reconstruction can occur in left–right slide tracheoplasty, and the tracheal lumen of this shape is easily collapsed [10]. Second, tracheal walls receive their blood supply from the longitudinal arterial anastomoses along the lateral surface of the trachea [11], and ischemia due to excessive tracheal dissection can be an operation-specific factor of anastomotic failure during tracheal reconstruction [12]. Wang et al. pointed out that left–right slide tracheoplasty had a risk of damaging this lateral blood supply due to long-segment lateral dissection of the trachea [3]. On the other hand, posterior–anterior slide tracheoplasty has a low risk of damaging the lateral blood supply. Furthermore, since the RULB arises from the posterolateral aspect of the trachea in most patients, we consider that it is possible to incise the anterior aspect of the distal segment safely and anastomose without suturing the orifice of the RULB. Le Bret et al. also reported that posterior–anterior slide tracheoplasty could be safely performed for a patient with this type [13].
A limitation of this study is that the study population was small. Further studies including a large number of participants are needed to clarify which procedure is feasible for each type of CTS associated with a tracheal bronchus.
In conclusion, the appropriate surgical intervention strategies for CTS associated with a tracheal bronchus differ with the location of stenosis. We can select tracheal end-to-end anastomosis or slide tracheoplasty for tracheal stenosis above the RULB according to the length of stenosis. We consider that posterior–anterior slide tracheoplasty is a safe and feasible procedure for tracheal stenosis below the RULB or above the RULB to the carina.
References
Barat M, Konrad HR (1987) Tracheal bronchus. Am J Otolaryngol 8:118–122
Speggiorin S, Torre M, Roebuck DJ, McLaren CA, Elliott MJ (2012) A new morphologic classification of congenital tracheobronchial stenosis. Ann Thorac Surg 93:958–961. doi:10.1016/j.athoracsur.2011.12.019
Wang S, Zhang H, Zhu L, Zhen J, Liu J, Xu Z (2015) Surgical management of congenital tracheal stenosis associated with tracheal bronchus and congenital heart disease. Eur J Cardiothorac Surg. doi:10.1093/ejcts/ezv317 (Epub ahead of print)
Tsang V, Murday A, Gillbe C, Goldstraw P (1989) Slide tracheoplasty for congenital funnel-shaped tracheal stenosis. Ann Thorac Surg 48:632–635
Grillo HC (1994) Slide tracheoplasty for long-segment congenital tracheal stenosis. Ann Thorac Surg 58:613–619 (discussion 619–21)
Stock C, Nathan M, Murray R, Rahbar R, Fynn-Thompson F (2015) Modified end-to-end anastomosis for the treatment of congenital tracheal stenosis with a bridging bronchus. Ann Thorac Surg 99:346–348. doi:10.1016/j.athoracsur.2014.06.084
Wright CD, Graham BB, Grillo HC, Wain JC, Mathisen DJ (2002) Pediatric tracheal surgery. Ann Thorac Surg 74:308–313 (discussion 314)
Elliott M, Roebuck D, Noctor C, McLaren C, Hartley B, Mok Q, Dunne C, Pigott N, Patel C, Patel A, Wallis C (2003) The management of congenital tracheal stenosis. Int J Pediatr Otorhinolaryngol 67(Suppl 1):S183–S192
Beierlein W, Elliott MJ (2006) Variations in the technique of slide tracheoplasty to repair complex forms of long-segment congenital tracheal stenosis. Ann Thorac Surg 82:1540–1542
Yokoi A, Arai H, Bitoh Y, Nakao M, Oshima Y, Nishijima E (2012) Aortopexy with tracheal reconstruction for postoperative tracheomalacia in congenital tracheal stenosis. J Pediatr Surg 47:1080–1083. doi:10.1016/j.jpedsurg.2012.03.009
Salassa JR, Pearson BW, Payne WS (1977) Gross and microscopical blood supply of the trachea. Ann Thorac Surg 24:100–107
Madariaga ML, Gaissert HA (2016) Reresection for recurrent stenosis after primary tracheal repair. J Thorac Dis 8(Suppl 2):S153–S159. doi:10.3978/j.issn.2072-1439.2016.01.66
Le Bret E, Teissier N, Belli E, Sigal-Cinqualbre A, Couloignier V, Narcy P, Demontoux S, Gharbi N, Roussin R, Van Den Abbeele T, Serraf A (2006) Slide tracheoplasty in the presence of tracheal bronchus in an infant. J Thorac Cardiovasc Surg 132:e15–e16
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Morita, K., Yokoi, A., Fukuzawa, H. et al. Surgical intervention strategies for congenital tracheal stenosis associated with a tracheal bronchus based on the location of stenosis. Pediatr Surg Int 32, 915–919 (2016). https://doi.org/10.1007/s00383-016-3928-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3928-8