Abstract
Background
Finding a proper scaffold for augmentation is a serious challenge in bladder tissue engineering. We hereby aimed to determine the histological aspects of a decellularized colon graft for bladder augmentation in healthy rats.
Methods
Rat colon tissues were decellularized using perfusion-based method. After partial cystectomy, bladders were grafted with a patch of decellularized colon. Bladder specimens were investigated in 12 rats at 1, 3, and 9 months postoperatively for further histological changes and immunohistochemistry analyses were also performed.
Results
One month after implantation, partial seeding of new cells was observed. After 3 months continuity of transitional epithelium of natural bladder on the decellularized grafted colon tissue was confirmed with histological and immunohistochemical examinations. All augmented bladders demonstrated a spherical shape without stone formation, necrosis or graft rejection. The presence of urothelium with similar morphology to the natural urothelium and visible blood vessels were found within 3 months of operation. All immunohistochemical markers (except markers of colonic stem cells) were expressed in biopsies obtained 3 months after surgery demonstrating a progressive vascular and smooth muscle cell infiltration into the graft after implantation.
Conclusion
This study suggests that decellularized colon may provide a viable material for bladder augmentation in rats to pave the road for future applications of this natural collagen scaffold.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite the recent advances in the management of low-compliant and overactive bladders, when other therapeutic options fail, bladder augmentation still offers a solution to protect the upper urinary tract, alleviate the complications, and provide urinary continence [1]. Although gastrointestinal segments are frequently used for cystoplasty, several short- and long-term complications like fistula formation, perforation, urolithiasis, and metabolic acidosis occur [1, 2]. Using non-biodegradable synthetic materials was also unsuccessful due to stone formation, recurrent urinary tract infection, and tissue contracture [1]. Need for advanced preparation techniques and inconsistent outcomes with small intestinal submucosa (SIS) and bladder acellular matrix graft (BAMG) also limit the application of these xenogeneic materials [3, 4]. Non-gastrointestinal alternatives like fascia, skin, omentum, and placenta have been also applied for bladder augmentation with unsatisfactory and limited applicability due to complications [1, 5]. So, the challenge to find a better alternative for successful bladder augmentation with satisfactory long-term outcomes still persists.
In recent years, tissue engineering has drawn more attention for bladder augmentation and tissue-engineered bladders have been used in pilot human studies [6, 7] although the long-term results are not as promising as initially perceived [8]. An ideal biocompatible scaffold should maintain its three-dimensional framework with appropriate mechanical and immunomodulatory characteristics [9]. Seeded and unseeded acellular grafts from different origins are being studied for bladder augmentation on animals in an attempt to find a promising method for future bladder augmentation. However, we are still far from an ideal tissue-engineered graft with appropriate inherent characteristics for bladder augmentation in humans.
Colon is commonly considered as an alternative to ileum for bladder augmentation because of the large lumen and advantageous mechanical properties; however, rich bacterial flora, more mucus production, and assumed risk of long-term malignancy makes it an imperfect alternative for this purpose [1]. Colon has a large thick-walled lumen and acellular colon also retains suitable mechanical characteristics, consistent thickness, and resistance [10]. When decellularized, the aforementioned drawbacks are no longer concerning and it may theoretically serve as a promising scaffold for bladder augmentation. This background prompted our interest in augmenting the bladder using this type of decellularized tissue graft. So in this study, we aimed to use a decellularized colon scaffold for bladder augmentation in a rat model and also investigated the histological characteristics of this tissue in the follow-up period.
Materials and methods
Perfusion-based colon decellularization
Colons were dissected en bloc with vascular tree and mesentery from four male rats aseptically. The superior mesenteric artery was catheterized and used for perfusion-based decellularization of the prepared colon. The lumen of colon was washed several times with normal saline to clear any colonic secretions and remnants. Decellularization was performed using a perfusion pump via the catheter infusing 0.1 % SDS for 24 h and then multiple rounds of washing was performed with phosphate buffered saline (PBS). The acellular grafts were preserved in antibiotic solution containing penicillin, gentamycin, and ceftriaxone at 4 °C until implantation and were used within 24 h of preparation.
Surgical technique
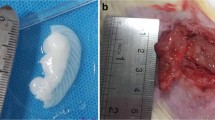
Initially, 15 male Sprague–Dawley rats, weighing 210–240 g, were used for bladder augmentation surgeries. The bladder wall was dissected and partial cystectomy (approximately 35–40 %) was performed for further grafting of the decellularized colon (Fig. 1). The decellularized graft (relatively larger than the defect approximately 1–2 cm2) was placed on the dissected bladder wall and it was grafted onto the host bladder using fine 6.0 Vicryl continuous stitches; care was taken not to penetrate the inner luminal surface by applying seromuscular sutures. The procedures were performed under magnifying surgical microscope. Graft borders were marked by applying 6.0 nonabsorbable sutures (Fig. 1). Then, the bladder was filled with normal saline to check for leakage from the suture line. The bladder was covered with perivesical fat layer to provide a vascular-rich environment and support the vascularization process and was situated in situ. All animals were housed under standard laboratory conditions with free access to water and rat chow. Daily Enrofloxacin was administered intramuscularly for all animals for four consecutive days, postoperatively. Three rats were lost during the first 2 days after surgery due to graft site leakage as postoperative complication. Groups of four rats (total of 12) were sacrificed at 1, 3 and 9 months after grafting, and the bladder specimens were taken for further histological examinations.
Surgical technique: a dye injection through the catheter shows successful cannulation for further decellularization processes; b a decellularized colon segment; c, d complete bladder exposure and partial cystectomy; e, f acellular colon grafted to the bladder wall with identification sutures placed at corners
Laboratory assessment of specimens
Masson’s trichrome and hematoxylin and eosin (H&E) staining were performed on colon specimens before and after decellularization for confirmation of decellularization process. Morphological analyses were also performed on harvested specimens. Picrosirius red staining was used for collagen typing under polarized light [type-I collagen (thick fibers): yellow-orange birefringence; type-III collagen (thin fibers): green birefringence]. Pentachrome staining was used to differentiate connective tissue constituents (collagen: yellow-green; elastin: black; muscle: red; mucin: blue; and fibrin: bright red).
Immunohistochemical (IHC) markers including α-smooth muscle actin (α-SMA), vimentin, cytokeratin AE1/AE3, CD31, CD34, CD24, leucine-rich-repeat-containing G protein-coupled receptor-5 (LGR5), S100, and synaptophysin antibodies were used. Monoclonal antibodies to cytokeratin AE1/AE3 were used to assess the urothelial integrity. Neovascularization, angioblasts and progenitor hematopoietic stem cells on the grafted colon were marked using CD31 and CD34. CD24 and LGR5 were used to assess the presence of colonic epithelial stem cells. IHC staining with monoclonal antibodies to α-SMA and S100 was performed to evaluate the quality of the muscular layer and the presence of nerve fibers, respectively. Synaptophysin was also used as a neuroendocrine differentiation marker.
Photoshop v10.0 (Adobe Systems Inc., Mountain View, CA, USA), and Image Pro (Image Pro Inc., Boston, MA, USA) software were used for image analyses. For scoring the images, five photomicrographs (×100) were used and the mean scores were used as final values for analysis.
To evaluate the efficacy of decellularization process, 4′,6- diamidino-2-phenylindole (DAPI) staining (Sigma, St Louis, MO, USA) was used. Complete absence of visible nuclear material on histological examination (H&E and DAPI stains) was used as definition of decellularization. Collagen and sulfated glycosaminoglycan (sGAG) content of the native and decellularized tissues were quantified using the Sircol and Blyscan assay kits (Biocolor Ltd., UK), respectively.
Several scanning electron microscopy (SEM) images were taken from both natural and decellularized colons to evaluate the efficacy of the decellularization process for cell removal and assure the maintenance of the extra cellular matrix (ECM) structure. Samples were examined using field emission SEM (FE-SEM; JSM-6340F, JEOL, Tokyo, Japan).
RQ-TRAP assay
Telomerase activity in native rat’s bladder cells, normal colon cells, and grafted tissues was detected by real-time quantitative telomerase repeat amplification protocol (RQ-TRAP) assay, using the SYBR green kit (LightCycler Green FastStart DNA Master SYBR Green I; Roche Diagnostics, Germany). Lysis buffer used as negative control and Hela cells were used as positive controls. Telomerase activity in the cell line was calculated based on threshold cycle (Ct). All sample analyses were run twice.
Statistical analysis
Statistical analysis was performed using SPSS®, v19 (IBM SPSS Statistics, IBM Corporation. Chicago, IL, USA). Relevant data are presented as mean ± SE. Biochemical analysis was performed using paired t test to compare the values before and after decellularization. Independent sample t-test was used to compare the results of IHC staining. P values <0.05 were considered statistically significant.
Results
Preservation of ECM, intactness of connective tissue, and complete cell removal were confirmed by H&E and Trichrome and DAPI staining in decellularized colons verifying that the acellular scaffolds were ready for implantation (Fig. 2). The concentration of collagen in decellularized colon (4.16 ± 1.16 µg/mg) was significantly higher than that of the native tissue (2.14 ± 0.32 µg/mg). There was no significant difference in sGAG content of the decellularized colon compared to the native one (0.58 ± 0.09 vs. 0.85 ± 0.15 µg/mg, respectively, P = 0.1).
Examination of the decellularized colon using SEM showed that the micro-structural features of the natural colon and the cryptic appearance were well preserved with intact ECM structure and without collagen degradation (Fig. 3).
Three animals were lost due to postoperative leakage of graft site during the first 2 days after surgery and were excluded. No sign of infection, fistulae, stone formation, and upper urinary tract complications was observed in any of the other animals in macroscopic evaluations. Minimal inflammation occurred 1 month postoperatively that decreased gradually from the time of grafting, tending to normalization 3 months postoperatively.
The results of the H&E staining at 1, 3, and 9 months postoperatively showed successful cell seeding with urothelial lining that increased continuously during the assessment period. Additionally, the uniform lining of the decellularized colon was covered with transitional cells after implantation (Fig. 4). One month after implantation, partial seeding of new cells was observed. After 3 months, continuity of transitional urothelium with similar morphology and visible blood vessels was confirmed in histological examination. Neural regeneration was partial at 3 months postoperatively that was also detectable submucosally. Smooth muscle layers were in a similar direction to the normal tissue with the presence of all the bladder wall components including urothelium, nerves, and blood vessel. Markers of colonic epithelial stem cells were negative in bladder specimens indicating the absence of colonic tissue in the grafted scaffold after recellularization. All IHC markers (except markers of colonic stem cells) were expressed in biopsies obtained 3 months after surgery demonstrating a progressive vascular and smooth muscle cell infiltration into the graft after implantation. Additionally, Pentachrome and Picrosirius red staining of tissue-engineered scaffolds demonstrated the maintenance of ECM in acellular graft with progressive infiltration of muscular components postoperatively (Fig. 5).
a–e, Upper row: Picroirius red staining (green birefringence indicates collagen type III, yellow-orange birefringence indicates thick collagen fibers type I; f–j, lower row: Pentachrome staining in natural rat colon (f), acellular colon (g), and 1, 3, 9 months after grafting to bladder (h, i, and j, respectively). Asterisk indicates areas of smooth muscle and unfilled circle indicated submucosa and collagen
The cycle threshold (Ct) for HeLa cells, normal bladder, normal colon, and grafted tissues according to their concentration were measured. The average total number of cell lines was 106. The linearity of RQ-TRAP assay was verified also by comparison to standard curves. The Ct value increased linearly with decreasing concentration of protein extract. The Ct values of grafts were not different from that of normal colon and bladder.
Discussion
The histological and immunological results of this preliminary study suggest that grafting decellularized colon matrix to bladder causes minimal host immune response and tissue reaction in a rat model. Additionally full-thickness bladder regeneration (including urothelium, smooth muscle, vessels, and nerves) occurs in the acellular matrix as early as 1 month after bladder augmentation and progressively continues in a 9-month follow-up with minimal complications.
An appropriate scaffold supports the cellular matrix and helps the surrounding native tissues to proliferate and differentiate on the new scaffold by providing a microenvironment rich in collagen, elastin, and growth factors [11]. Natural acellular matrices may serve as suitable scaffolds since they retain their beneficial ECM structure, but lose their immunogenic characteristics during the decellularization process [11]. Similarly, an ideal scaffold for bladder augmentation should preserve its mechanical properties and also facilitate progressive proliferation of muscular and urothelial layers of the native bladder wall [3, 12].
A recent study showed that decellularized colon tissue provides a novel non-immunogenic scaffold that preserves its biomechanical characteristics and may be a suitable option for grafting in experimental models [10]. Preservation of ECM and integrity of the structural proteins in the decellularized colon play an important role in successfulness of using these scaffolds as different grafts. In the current study, we used perfusion-based decellularization technique and successfully developed a natural acellular matrix with preserved ECM components using a rat colon tissue. After implantation of the grafts, a temporary mild inflammation was present at 1 month postoperatively that completely resolved in 9-month specimens. Inflammatory responses are expected during the first 2 weeks postoperatively due to initial congestion, inherent surgical site inflammation, and stimulation of the host tissue by graft components [13]. Additionally, no evidence of graft rejection was observed in any of the rats.
Bladder stone formation commonly complicates enterocystoplasty [1] and also happens after using SIS for bladder augmentation in animals [14]. It is also a common problem after bladder augmentation in rat models even when acellular matrices are used [15]. In enterocystoplasty, this complication is mostly due to mucus secretion by intestinal cells. Also stone formation in seeded or unseeded acellular matrices may be attributable to incomplete decellularization technique, incomplete absorption of the grafted tissue, and intravesical foreign bodies like mesh or suture remnants [1, 16]. Implementing careful suture techniques to avoid the inner surface of bladder is important since stiches may act as a nidus for stone formation when are in contact with urine [13]. Additionally, urinary tract infections predispose the animals to stone formation that may be prevented by prophylactic antibiotics [13]. Absence of colonic stem cells in the grafted tissue also indicates the effectiveness of the decellularization protocol, absence of colonic tissue, and no mucus production that might translate into better function of the bladder and less complications after using acellular colon. In our study we also used telomerase activity as a surrogate for cell-line immortalization and early malignant transformation capacity and showed that the telomerase activity in the in vivo recellularized colon graft was similar to the native bladder tissue indicating that the risk of malignancy was not increased in the graft during the study follow-up. However, this finding should be interpreted with caution since telomerase activity is only one of the several indicators of malignant transformation and also the follow-up period is too short to assess the long-term risks.
The application of conventional matrices can culminate in significant morbidity after bladder augmentation. For example, Probstet et al. [12] reported urinary leakage and bladder neck obstruction with 32 % mortality rate that occurred following the application of BAMG for bladder augmentation in rats. Although SIS is the most commonly used bioscaffold for bladder augmentation with promising results in animal studies, the application of this material is more controversial in humans with conflicting results [17, 18]. Additionally, for small intestine scaffolds like SIS, the anatomical site of the graft (e.g., jejunum vs. ileum) may serve a determining role in postoperative results and complications, and may not be easily recognizable when using commercial SIS preparations [14, 19]. Taken together, these results show that we may be still far from the ideal bioscaffold for bladder augmentation calling for new scaffolds with better characteristics.
Although seeded matrices have been previously used as a promising method for bladder augmentation, several methodological and financial obstacles (e.g., the need for sophisticated bioreactors and recellurarization techniques) limit the widespread applicability of this method [11]. On the other hand, unseeded matrices are recently used in bladder augmentation with acceptable outcomes and studies have shown that when the grafted scaffold is able to support smooth muscle and urothelial regeneration, native bladder can work as a natural bioreactor [20, 21]. Additionally, recent evidence suggests that seeded/cellular matrices may not necessarily provide better outcomes in animal models [22].
The results of this experimental study support the idea that decellularized colon may serve as a framework of collagen and elastin for proliferation and ingrowths of the natural bladder wall components. Decellularized colon may be a viable alternative for SIS, collagen-based biomatrix and gastrointestinal segments for bladder augmentation. It is also well tolerated and can promote adequate smooth muscle regeneration, neovascularization, large vessels formation, and new nerve formation. These findings might pave the road for future applications of acellular colon as a promising bioscaffold in larger animals and also diseased bladder models.
This study has its limitations. First of all the study lacks a control group and no comparison is made with other commonly used materials; however, this study was the first to use a decellularized colon as a pilot project and we did not aim to compare different materials with decellularized colon at this stage. The main focus of this study was on the immunological and histological responses of the decellularized colon in terms of bladder wall regeneration. Also functional characteristics of the augmented bladders (like compliance and volume) were not assessed. However, since the augmented bladders were healthy, it is predictable that the volume and compliance would be preserved in cystometric studies after augmentation as previously shown [13]. We used a healthy rat model in this study and the success in augmentation of healthy bladders may not be extrapolated to diseased bladder or larger animals. Regarding the strength, to the best of our knowledge, this is the first study in which the decellularized colon without native colocystoplasty was used for bladder augmentation in a rat model with satisfactory postoperative results and without major complications. A perfusion-based decellularization technique was used that allows the tissue to maintain its physical properties and ECM structure. Various laboratory measures were used to assess the decellularization success and also postoperative outcomes and also telomerase activity in the grafted tissue.
Conclusion
Decellularized colon promotes urothelial and smooth muscle regeneration without major complications for bladder augmentation in rat model. In this study, we showed that bladder acts as a natural bioreactor when decellularized colon is used as a scaffold that supports tissue formation and angiogenesis. Augmentation cystoplasty with decellularized colon is a simple and inexpensive method that can efficiently regenerate all the bladder wall components in a healthy rat model.
Abbreviations
- α-SMA:
-
α-Smooth muscle actin
- BAMG:
-
Bladder acellular matrix graft
- ECM:
-
Extra cellular matrix
- H&E:
-
Hematoxylin and eosin
- IHC:
-
Immunohistochemical
- PBS:
-
Phosphate buffered saline
- SDS:
-
Sodium dodecyl sulfate
- sGAG:
-
Sulfated glycosaminoglycan
- SIS:
-
Small intestinal submucosa
- RQ-TRAP:
-
Real-time quantitative telomerase repeat amplification protocol
References
Biers SM, Venn SN, Greenwell TJ (2012) The past, present and future of augmentation cystoplasty. BJU Int 109(9):1280–1293. doi:10.1111/j.1464-410X.2011.10650.x
Gilbert SM, Hensle TW (2005) Metabolic consequences and long-term complications of enterocystoplasty in children: a review. J Urol 173(4):1080–1086. doi:10.1097/01.ju.0000155248.57049.4e
Ayyildiz A, Akgul KT, Huri E, Nuhoglu B, Kilicoglu B, Ustun H, Gurdal M, Germiyanoglu C (2008) Use of porcine small intestinal submucosa in bladder augmentation in rabbit: long-term histological outcome. ANZ J Surg 78(1–2):82–86. doi:10.1111/j.1445-2197.2007.04361.x
Song L, Murphy SV, Yang B, Xu Y, Zhang Y, Atala A (2014) Bladder acellular matrix and its application in bladder augmentation. Tissue Eng Part B Rev 20(2):163–172. doi:10.1089/ten.TEB.2013.0103
Elbahnasy AM, Shalhav A, Hoenig DM, Figenshau R, Clayman RV (1998) Bladder wall substitution with synthetic and non-intestinal organic materials. J Urol 159(3):628–637
Atala A, Bauer SB, Soker S, Yoo JJ, Retik AB (2006) Tissue-engineered autologous bladders for patients needing cystoplasty. Lancet 367(9518):1241–1246. doi:10.1016/S0140-6736(06)68438-9
Atala A (2011) Tissue engineering of human bladder. Br Med Bull 97:81–104. doi:10.1093/bmb/ldr003
Joseph DB, Borer JG, De Filippo RE, Hodges SJ, McLorie GA (2014) Autologous cell seeded biodegradable scaffold for augmentation cystoplasty: phase II study in children and adolescents with spina bifida. J Urol 191(5):1389–1395. doi:10.1016/j.juro.2013.10.103
Horst M, Madduri S, Gobet R, Sulser T, Milleret V, Hall H, Atala A, Eberli D (2013) Engineering functional bladder tissues. J Tissue Eng Regen Med 7(7):515–522. doi:10.1002/term.547
Kajbafzadeh AM, Masoumi A, Hosseini M, Borjian MA, Akbarzadeh A, Mohseni MJ (2014) Sheep colon acellular matrix: immunohistologic, biomechanical, scanning electron microscopic evaluation and collagen quantification. J Biosci Bioeng 117(2):236–241. doi:10.1016/j.jbiosc.2013.07.006
Badylak SF, Weiss DJ, Caplan A, Macchiarini P (2012) Engineered whole organs and complex tissues. Lancet 379(9819):943–952. doi:10.1016/S0140-6736(12)60073-7
Probst M, Dahiya R, Carrier S, Tanagho EA (1997) Reproduction of functional smooth muscle tissue and partial bladder replacement. Br J Urol 79(4):505–515
Kajbafzadeh AM, Payabvash S, Salmasi AH, Sadeghi Z, Elmi A, Vejdani K, Tavangar SM, Tajik P, Mahjoub F (2007) Time-dependent neovasculogenesis and regeneration of different bladder wall components in the bladder acellular matrix graft in rats. J Surg Res 139(2):189–202. doi:10.1016/j.jss.2006.11.003
Lin HK, Godiwalla SY, Palmer B, Frimberger D, Yang Q, Madihally SV, Fung KM, Kropp BP (2014) Understanding roles of porcine small intestinal submucosa in urinary bladder regeneration: identification of variable regenerative characteristics of small intestinal submucosa. Tissue Eng Part B Rev 20(1):73–83. doi:10.1089/ten.TEB.2013.0126
Sutherland RS, Baskin LS, Hayward SW, Cunha GR (1996) Regeneration of bladder urothelium, smooth muscle, blood vessels and nerves into an acellular tissue matrix. J Urol 156(2 Pt 2):571–577
Zhang Y, Frimberger D, Cheng EY, Lin HK, Kropp BP (2006) Challenges in a larger bladder replacement with cell-seeded and unseeded small intestinal submucosa grafts in a subtotal cystectomy model. BJU Int 98(5):1100–1105. doi:10.1111/j.1464-410X.2006.06447.x
Zhang F, Liao L (2014) Tissue engineered cystoplasty augmentation for treatment of neurogenic bladder using small intestinal submucosa: an exploratory study. J Urol 192(2):544–551. doi:10.1016/j.juro.2014.01.116
Schaefer M, Kaiser A, Stehr M, Beyer HJ (2013) Bladder augmentation with small intestinal submucosa leads to unsatisfactory long-term results. J Pediatr Urol 9(6 Pt A):878–883. doi:10.1016/j.jpurol.2012.12.001
Ashley RA, Roth CC, Palmer BW, Kibar Y, Routh JC, Fung KM, Frimberger D, Lin HK, Kropp BP (2010) Regional variations in small intestinal submucosa evoke differences in inflammation with subsequent impact on tissue regeneration in the rat bladder augmentation model. BJU Int 105(10):1462–1468. doi:10.1111/j.1464-410X.2009.08965.x
Tu DD, Chung YG, Gil ES, Seth A, Franck D, Cristofaro V, Sullivan MP, Di Vizio D, Gomez P, Adam RM, Kaplan DL, Estrada CR, Mauney JR (2013) Bladder tissue regeneration using acellular bi-layer silk scaffolds in a large animal model of augmentation cystoplasty. Biomaterials 34(34):8681–8689. doi:10.1016/j.biomaterials.2013.08.001
Kajbafzadeh AM, Esfahani SA, Sadeghi Z, Elmi A, Monajemzadeh M (2012) Application of different scaffolds for bladder wall regeneration: the bladder as a natural bioreactor. Tissue Eng Part A 18(7–8):882–887. doi:10.1089/ten.TEA.2011.0202
Sloff M, Simaioforidis V, de Vries R, Oosterwijk E, Feitz W (2014) Tissue engineering of the bladder—reality or myth? A systematic review. J Urol 192(4):1035–1042. doi:10.1016/j.juro.2014.03.116
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Funding
This work received no funding from any extra-institutional or commercial source.
Ethical approval
All applicable international, national, and institutional guidelines for the care and use of animals were followed. Principles of laboratory animal care were followed and the Animal Ethics Committee of the Tehran University of Medical Sciences, School of Medicine and Education Section of Basic Sciences, approved the animal selection, managements and surgical protocols.
Rights and permissions
About this article
Cite this article
Kajbafzadeh, AM., Khorramirouz, R., Sabetkish, S. et al. In vivo regeneration of bladder muscular wall using decellularized colon matrix: an experimental study. Pediatr Surg Int 32, 615–622 (2016). https://doi.org/10.1007/s00383-016-3871-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-016-3871-8