Abstract
Background and importance
Angiosarcoma is a rare malignant tumor with an aggressive course and poor prognosis. It is typically seen in adults but very rarely seen in children. Angiosarcoma of the skull with brain metastasis is exceptionally rare. Due to the rare nature of these tumors, much is left unknown about clinical progression and treatment guidelines are not well established.
Clinical presentation and course
A 14-year-old male patient presented with an enlarging mass on the parietal region of the head. Further investigations revealed a mass lesion involving scalp and skull tissue. Biopsy result showed angiosarcoma and the patient underwent multiple surgical interventions including scalp excision, craniectomy on tumor site, and excision of brain metastases. He also received chemotherapy and radiation therapy. Despite aggressive treatment, disease progression could not be controlled.
Conclusion
Here we report a pediatric patient with intracranially invasive angiosarcoma of the scalp and skull, with recurrent hemorrhagic metastases to the brain. This is a very rare case in pediatric age group with very poor prognosis. Our patient had impressively longer survival than those reported in the literature despite multiple hemorrhagic brain metastasis and this is most likely related to our aggressive treatment strategy that includes multiple craniotomies for metastatic tumor resection in addition to neoadjuvant chemotherapy and radiation therapy. We believe optimal treatment of skull angiosarcoma in children should aim gross total resection of the skull tumor including involving scalp and dura as well as neoadjuvant chemotherapy and radiation therapy, and the patient should be followed closely with repeated brain MRI studies to pursue additional surgeries to remove brain metastasis if feasible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background and importance
Angiosarcoma is a rare endothelial cell tumor that accounts for less than 1% of all sarcomas [1, 2]. These malignant tumors are aggressive, with high propensity for recurrence and early metastasis, and often poor prognosis [1, 3]. Angiosarcoma most commonly presents as head and neck lesions in elderly males and infrequently involves the skull and central nervous system (CNS) as either primary or metastatic lesions [1,2,3,4,5]. Cranial angiosarcoma occurs even more rarely in children, with only 9 reported cases in literature [4, 6,7,8,9,10,11,12,13] (Table 1).
Treatment for angiosarcoma involves surgery, chemotherapy, and radiotherapy. Due to the rarity of angiosarcoma of the skull and brain, diverse management approaches are seen, and treatment guidelines and efficacy remain unclear [5].
We present a case of scalp and skull angiosarcoma in an adolescent male with intracranial invasion and recurrent hemorrhagic metastasis to the brain.
Clinical presentation
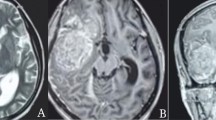
A 14-year-old male presented with a 15-month history of a progressively expanding 3.5-cm mass on the left posterior parietal region of the scalp. The lesion was first noticed after minor local trauma and was accompanied by tenderness. A biopsy was taken by plastic surgery and initially reported as atypical epithelioid neoplasm. However, positive margins on repeat scalp excision and lymph node reactivity prompted further workup. Nuclear bone scan and computed tomography (CT) demonstrated neoplasm extension with a sizeable lytic lesion in the parietal skull and minimal enhancement of adjacent meninges (Fig. 1). The patient was seen by oncologist and he was referred to neurosurgery. A neoadjuvant multidrug chemotherapy (paclitaxel, doxorubicine, and cisplatine) in total 3 cycles was given starting before surgical excision of the skull tumor and continuing postoperatively as well. The patient underwent resection of the skull tumor including invaded scalp and dura. Craniectomy was extended until healthy bone was encountered and cranioplasty was performed to cover the skull defect. The final pathology diagnosis was made as epithelioid angiosarcoma of the scalp and skull. The biopsies that were obtained from the edges of the craniectomy and dural excision sites were negative for tumor invasion. No evidence of further metastasis was observed on CT. Then, the remaining chemotherapy cycles were given postoperatively and completed 3 months after the surgery.
One year after the patient’s initial presentation, he noticed a swelling in his neck which proved to be benign on biopsy. However, MRI revealed metastasis in the brain, with new lesions in the right frontal lobe and right occipital lobe. Despite palliative whole brain radiotherapy and stereotactic boost of intensity-modulated radiation therapy (IMRT), these lesions persisted. Two years later, the patient presented with severe headaches, vomiting, and blurry vision, and MRI showed an intraparenchymal hematoma in the right occipital lobe (Fig. 2a). He underwent second surgery with gross total removal of the metastatic brain tumor, affected dura, and hematoma. Pathology confirmed it as an intracranial metastasis of the patient’s original angiosarcoma.
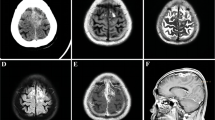
CT scan axial cuts: a right occipital enhancing, small metastatic nodule, b right frontal and occipital hemorrhagic metastatic lesion (March 2011), c increased hemorrhage in the right frontal tumor site (April 2011), d new hemorrhagic metastasis in right temporoparietal region (May 2012), e new hemorrhagic focus in the left frontoparietal region (May 2012)
A recurrence of angiosarcoma in the right occipital lobe was identified 1 year later and he underwent a 3rd craniotomy and tumor resection procedure. Follow-up MRIs in following months showed multiple metastatic tumor foci with intraparenchymal and intraventricular hemorrhages (Fig. 2b, c). No further surgery or radiation therapy was found viable and it was proceeded for palliative chemotherapy. After an acute multifocal hemorrhage from metastases in both hemispheres (Fig. 2d–e), the patient died approximately 6 years after the initial diagnosis.
Pathological findings
Brain tumor, dura, parietal bone, scalp, and lymph node resections all revealed epithelioid angiosarcoma pathology. Epithelioid, spindle, and rhabdoid-like cells were present with areas of necrosis, infiltrating vascular proliferation, and hemorrhage. Immunohistochemistry demonstrated CD31, factor VIII-related antigen, and epithelial membrane antigen (EMA) positivity. Tumors were negative for CD34, pan-cytokeratin, and desmin.
Discussion
Angiosarcoma is a malignant tumor comprised of vascular endothelial cells with an aggressive clinical course and extremely poor prognosis. Diagnosis of angiosarcoma is challenging as numerous benign and malignant lesions, such as kaposiform hemangioendothelioma and Kaposi sarcoma, have similar histologic profiles and presentations [13, 14]. This causes potential delay in diagnosis of a progressive malignancy. Immunohistochemistry, in addition to pathological appearance, is vital in confirming diagnosis. Angiosarcoma has characteristic expression of endothelial markers CD31, CD34, factor VIII-related antigen, and vascular endothelial growth factor (VEGF) [1, 14]. The lack of CD34 expression can aid in distinguishing angiosarcomas from mimicking lesions [14]. This is consistent with our findings.
Mainstay treatment for angiosarcoma is surgical resection with wide negative margins [15, 16]. As in the present case, radiotherapy and chemotherapy to prevent recurrence and metastasis has limited effect [12, 13, 15]. Primary CNS angiosarcoma patients who undergo early complete excision have been shown to be disease free for up to 2 years [16]. However, the rarity of angiosarcoma has made developing guidelines for treatment difficult [15]. Recent studies suggest the anti-angiogenic and synergistic efficacy of paclitaxel and doxorubicin and the effectiveness of VEGF receptor inhibitors in improving prognosis of angiosarcoma of the scalp and soft tissues [17,18,19]. But, studies in pediatric angiosarcoma failed to demonstrate prevention of relapses [15]. Moreover, less is known about treatment for primary skull or cerebral metastases of angiosarcoma [16].
Only 9 cases of primary skull angiosarcoma in children have been reported and none involves brain metastasis [4, 6,7,8,9,10,11,12,13]. Among them, only 3 patients survived longer than 3 years and all three had just local diseases without distant metastasis. The cases with metastatic lesions in lymph nodes and brain have poorer outcomes in general. Our patient had impressively longer survival than expected despite multiple brain metastasis and this is most likely related to the aggressive treatment strategy that includes multiple craniotomies for metastatic tumor resection, neoadjuvant chemotherapy in 3 cycles, and radiation therapy. He had approximately 1 year without clinical signs of progression following first craniotomy and resection of skull tumor with neoadjuvant chemotherapy and 2 years following radiation, but then developed both local recurrence and new metastatic brain lesions and underwent two additional craniotomies for resection of brain metastasis. Although it did not halt the disease progression, this aggressive treatment have lengthened his survival to nearly 6 years, which is significantly longer than that of other cases with cerebral metastasis for which data is available [15]. Tumor location also probably plays a significant role in poor outcome by limiting the gross total resection chance of the skull tumors such as cases 5 and 7 (Table 1) that were located in skull base with venous sinus involvement. We believe optimal treatment of skull angiosarcoma in children should aim gross total resection of the skull tumor and neoadjuvant chemotherapy. Surgical excision should include invaded scalp and dura adjacent to skull tumor and should be followed by postoperative radiation therapy. Then, the patient should be followed closely with repeated brain MRI studies to pursue additional surgeries to remove brain metastasis if feasible. Another challenge in these cases is excessive blood loss during surgery because of vascular nature of these tumors. We avoided excessive bleeding during craniectomy by keeping our craniectomy lines away from the tumor tissue as much as possible. However, presurgical embolization may also be useful to decrease blood loss during surgery in these cases.
Conclusion
We present the unique case of a 14-year-old male with intracranial invasion of angiosarcoma of the scalp and skull, presenting as scalp swelling. Surgical excision, multidrug chemotherapy, and radiation therapy were employed. On follow-up, multiple hemorrhagic cerebral metastases were identified and had poor response to additional chemotherapy, radiation, and surgeries. The patient ultimately died of hemorrhage from metastatic disease. This case provides a rare instance of scalp and skull angiosarcoma with metastasis to the brain in an adolescent, emphasizing the need for treatment guidelines and contributing to understanding of the clinical course and management of rare tumors in young patients.
References
Young RJ, Brown NJ, Reed MW, Hughes D, Woll PJ (2010) Angiosarcoma. Lancet Oncol 11:983–991. https://doi.org/10.1007/978-1-4471-6578-1_36
Scholsem M, Raket D, Flandroy P, Sciot R, Deprez M (2005) Primary temporal bone angiosarcoma: a case report. J Neuro-Oncol 75:121–125. https://doi.org/10.1007/s11060-005-0375-0
Choi K-S, Chun H-J, Yi H-J, Kim J-T (2008) Intracranial invasion from recurrent angiosarcoma of the scalp. J Korean Neurosurg Soc 43:201–204. https://doi.org/10.3340/jkns.2008.43.4.201
Bourekas EC, Cohen ML, Kamen CS et al (1996) Malignant hemangioendothelioma (angiosarcoma) of the skull: plain film, CT, and MR appearance. Am J Neuroradiol 17:1946–1996
Drosos E, Kalyvas A, Komaitis S, Skandalakis GP, Kalamatianos T, Liouta E, Neromyliotis E, Alexiou GA, Stranjalis G, Koutsarnakis C (2019) Angiosarcoma-related cerebral metastases: a systematic review of the literature. Neurosurg Rev:1–20. https://doi.org/10.1007/s10143-019-01127-y
Kinkade JM (1948) Angiosarcoma of the petrous portion of the temporal bone; report of a case. Ann Otol Rhinol Laryngol 57:235–240
Larsson SE, Lorentzon R, Boquist L (1975) Malignant hemangioendothelioma of bone. J Bone Joint Surg 57:84–89
Masieh M (1980) Clinical records haemangiosarcoma of the petrous temporal bone. J Laryngol Otol 94:205–210
Eliashar R, Saah D, Osin P, Sichel JY (1997) Hemangioendothelioma of the temporal bone in a child. Int J Pediatr Otorhinolaryngol 40:67–71. https://doi.org/10.1016/S0165-5876(96)01480-2
Ibarra RA, Kesava P, Hallet KK, Bogaev C (2001) Hemangioendothelioma of the temporal bone with radiologic findings resembling hemangioma. Am J Neuroradiol 22:755–758
Renukaswamy GM, Boardman SJ, Sebire NJ, Hartley BEJ (2009) Angiosarcoma of skull base in a 1-year-old child—a case report. Int J Pediatr Otorhinolaryngol 73:1598–1600. https://doi.org/10.1016/j.ijporl.2009.07.025
Samadian M, Rakhshan M, Haddadian K, Rezaei O, Zamani SA, Khormaee F (2012) Angiosarcoma of skull in a pregnant woman: case report and review of the literature. Turk Neurosurg 22:113–115. https://doi.org/10.5137/1019-5149.JTN.3148-10.1
Khan IS, Thakur JD, Ahmed O, Shorter CD, Thomas-Ogunniyl J, Kim MT, Jeroudi MA, Guthikonda B (2012) Primary calvarial angiosarcoma: a case report and review of the literature. Surg Neurol Int 3:134. https://doi.org/10.4103/2152-7806.102952
Lee KB, Lee KS, Lee HS (2019) Tumor-Associated Protein Profiles in Kaposi Sarcoma and Mimicking Vascular Tumors, and Their Pathological Implications. Int J Mol Sci 20. https://doi.org/10.3390/ijms20133142
Bien E, Stachowicz-Stencel T, Balcerska A, Godzinski J, Kazanowska B, Perek-Polnik M, Madziara W, Rybczynska A, Kurylak A, Zalewska-Szewczyk B, Peregud-Pogorzelski J (2009) Angiosarcoma in children still uncontrollable oncological problem. The report of the Polish Paediatric Rare Tumours Study. Eur J Cancer Care (Engl) 18:411–420. https://doi.org/10.1111/j.1365-2354.2008.01063.x
Zakaria Z, Tambirajoo K, Sattar MT, Farrell MA (2015) Rapid clinical course of multiple metastatic cerebral angiosarcoma. Turk Neurosurg 25:643–648. https://doi.org/10.5137/1019-5149.JTN.9042-13.1
Fury MG, Antonescu CR, Van Zee K et al (2005) A 14-year retrospective review of angiosarcoma: clinical characteristics, prognostic factors, and treatment outcomes with surgery and chemotherapy. Cancer J 11:241–247. https://doi.org/10.1097/00130404-200505000-00011
Skubitz KM, Haddad PA (2005) Paclitaxel and pegylated-liposomal doxorubicin are both active in angiosarcoma. Cancer. https://doi.org/10.1002/cncr.21140
Liu M, Liu Y, Guo H, et al (2019) Apatinib , combined with chemotherapy or alone is effective in treating angiosarcoma : a case report. Anti-Cancer Drugs 30:762–765. https://doi.org/10.1097/CAD.0000000000000738
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval for case studies
Authors checked with their institution review board and verified that this case report does not require IRB review and approval.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Lee, V., Gessler, D. & Cataltepe, O. Case report: cranial angiosarcoma with multiple hemorrhagic brain metastasis in a child. Childs Nerv Syst 36, 2103–2107 (2020). https://doi.org/10.1007/s00381-020-04568-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-020-04568-9