Abstract
Purpose
The primary objective of this study is to investigate post-operative morbidity and shunt revision rates of patients with shunt-dependent hydrocephalus (SDH) undergoing posterior vault distraction osteogenesis (PVDO) compared to patients undergoing conventional posterior vault reconstruction (PVR).
Methods
A retrospective case-controlled cohort analysis of all patients with SDH undergoing PVDO and PVR for syndromic or complex craniosynostosis was performed. Demographic information, perioperative variables, distraction protocols, and shunt-related complications—infection, surgical revision of shunt, increased length of stay (LOS), and readmission within 90 days of surgery—were compared using the appropriate statistical tests.
Results
Fourteen patients with ventricular shunts who underwent PVDO and eight patients with shunts who underwent PVR were identified. Shunt-related complication rates were significantly higher with PVDO (n = 5) compared to PVR (n = 0), p = 0.0093. Among the five patients who suffered complications, the most common were shunt infection (n = 4), shunt malfunction (n = 4), and wound infections (n = 3). All patients with complications required additional operations for shunt revision and/or replacement; four patients required multiple takebacks for such procedures, with an average of three additional procedures per patient.
Conclusions
In complex or syndromic craniosynostosis patients who have previously undergone ventricular shunting, PVDO is associated with higher shunt-related complications and need for additional procedures when compared to traditional PVR. While the benefits of PVDO in the treatment of syndromic craniosynostosis are well documented, the risks of PVDO in the face of a VP shunt must be considered. Further investigation into patient-specific risk factors and risk reduction strategies is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients with syndromic craniosynostosis often require cranial expansion to allow for brain growth and prevent development of raised intracranial pressure (ICP) [1,2,3]. Among the commonly used techniques are fronto-orbital advancement, extended strip craniectomy with helmet therapy, spring-assisted cranial expansion, and open cranial vault remodeling. Each of these techniques has advantages, disadvantages, and indications that may differ based on the timing of surgery and location of fused suture [4,5,6]. Posterior cranial vault distraction osteogenesis (PVDO) is a newer method, first described in 2009 [7], that has gained in popularity as an initial intervention in patients with syndromic craniosynostosis to expand intracranial volume, prevent or relieve increased ICP, and improve cranial morphology [8,9,10,11]. PVDO has been shown to provide for greater expansion per unit volume [12], greater expansion overall compared to conventional remodeling techniques [13], and a favorable perioperative morbidity profile [14]. Utilization of PVDO potentially delays surgical intervention of the anterior cranium which may preserve frontal growth and improve frontal morphologic changes over the long term.
Some patients with premature closure of the cranial sutures develop progressive hydrocephalus requiring shunting of cerebrospinal fluid (CSF) irrespective of cranial expansion [15,16,17]. This presentation is most common in patients with syndromic craniosynostosis or complex non-syndromic craniosynostosis [17, 18]. Ventricular shunting is historically the main treatment for hydrocephalus [19]. Ventricular shunting provides a rapid means to normalize increased ICP and in turn minimize neuronal damage and alleviate immediate symptoms such as vomiting, sleepiness, poor feeding, irritability, or seizures [20]. Unfortunately, ventricular shunts have a high complication and revision rate [21]. Shunt failure and infection require urgent surgical attention to prevent significant neurological sequelae of acute elevated ICP and meningitis [22]. Thus, shunt exposure and manipulation is a significant consideration for patients undergoing any surgical procedure that may put the shunt at risk.
Within this past decade in our unit, PVDO has been utilized as a first-line expansion technique to manage patients with multi-suture and syndromic craniosynostosis [23], some of whom have concomitant hydrocephalus. Thus, we have encountered patients who require cranial expansion that have already had placement of a ventricular shunt. The surgical technique for placement of the posterior vault distractors often requires the temporary exposure of a portion of the shunt that lies on the cranial surface [24]. As an artificial implant, the ventricular shunt is expected to be subject to the same risks of infection when exposed to the external environment. However, the rates of complications and subsequent revisions related to the temporary exposure of the ventricular shunt in PVDO are unknown and are of importance in the appropriate management, surgical or non-surgical, of this complex patient population.
Methods
Data collection
This study was designed as a retrospective cohort study. PVDO and posterior vault reconstruction (PVR) cases were identified by reviewing case logs of the Division of Plastic Surgery from 2003 to 2017. Cases were included if the patient underwent PVDO or PVR at the Children’s Hospital of Philadelphia (CHOP) between January 1, 2003 and December 31, 2017 and had pre-existing ventricular shunts or initial shunt placement at the time of surgery. Follow-up information through October 31, 2018 was reviewed. From this list, subjects who had ventricular shunts at the time of surgery were isolated. Patients were divided into two cohorts based on whether they had PVDO or PVR.
Subject demographics were examined, including age at the time of surgery, sex, primary diagnosis, syndromes/comorbidities, and previous surgeries. Tables 1 and 2 summarize the study demographics in each cohort. Other data elements that were included were perioperative variables, pertinent surgical history, distraction protocols, and post-operative complications as detailed in Tables 3, 4, 5, 6, and 7. Shunt-related complications included prolonged CSF leaks, shunt infections, surgical site infections, and surgical revision of the shunt. Complications were only included if they were initially documented within the distraction period. Surgical revisions/replacements of shunts were included outside of the distraction period only if the initial insult occurred within the distraction period (i.e., internalization of a shunt after distractor removal would be included if the shunt was externalized during the distraction period). Other post-operative complications studied were readmissions, wound infections, and wound dehiscence. Perioperative variables included length of surgery, estimated blood loss, transfusion volume, type and location of shunt, length of stay in the ICU, and length of stay in the hospital. Distraction protocols included time (days) of distraction, distance distracted, and complications with distractors. Shunt locations were determined for all patients. The locations of shunts were described as frontal, parietal, parieto-occipital, or occipital, as well as laterality.
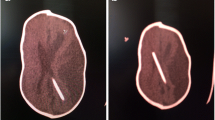
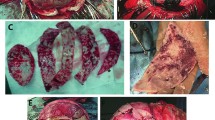
Surgical technique for PVDO in the face of a VP shunt
An exhaustive description of our surgical technique for PVDO has been published previously, and the following is a brief description highlighting the key technical aspects [20]. Posterior circumferential cranial osteotomy is performed such that the posterior cranium can be driven posteriorly in the desired vector, which for syndromic patients is antero-posterior with slight downward angulation to improve turricephaly. In non-syndromic patients, the vector of distraction is more variable given the increased variability of the cranial dysmorphology. Barrel stave osteotomies and greenstick out-fracturing of the inferior occiput are used to prevent occipital bone interference or an inferior step-off deformity, and we occasionally place resorbable fixation across patent lambdoid sutures to prevent diastasis of the suture during distraction. After completing osteotomies, the ventriculoperitoneal (VP) shunt tubing is reconnected, and thorough irrigation of the operative site is performed. Semi-buried, co-linear distraction devices are placed bi-temporally, with barrels often exiting the scalpthrough separate stab incisions immediately anterior to the coronal incision. Distractor base plates are fixated with non-self-drilling, self-tapping screws to minimize potential injury to the underlying dura. After testing the distractors to ensure completeness of the osteotomy, the scalp is closed in layers.
Surgical technique for PVR
The technique used for PVR involves a posterior 2/3 remodeling with reconstruction of the cranium posterior to the coronal sutures. With the patient in prone position, a coronal incision is opened, and the posterior and middle vaults are exposed in the sub-galeal plane. The cranial bone removed is generally divided into segments, often two or three, so as to allow for maximal freedom for surgical remodeling and positioning. The low occipital bones, temporal bones, and anterior aspects of the parietal bones are generally barrel-staved and greensticked in order to allow for reshaping, as desired, in those areas. The bone flaps that have been removed, once reshaped, are rigidly fixed to the occipital, temporal, and parietal bones with a combination of resorbable plates and screws and resorbable sutures.
Statistical analysis
Data were stored in Excel (Microsoft Corp, Redmond, WA, USA) and analyzed with STATA (Stata Corp, College Station, Texas, USA).
Results
Twenty-two patients met the inclusion criteria: 14 (63.6%) patients underwent PVDO, and 8 (36.4%) underwent PVR. Four of eight patients in the PVR cohort underwent operations between 2003 and 2010, the period prior to routine use of PVDO at our institution. The remaining four patients in the cohort underwent traditional PVR instead of PVDO due to a greater need for reshaping. All patients had VP shunts either present before (n = 20, 90.9%) or placed during (n = 2, 9.1%) posterior vault expansion surgery. One patient from each cohort had their initial shunt placed at the time of surgery. No patients were included who had shunts placed after PVDO or PVR.
A summary of the demographic information is listed in Tables 1 and 2. There was no difference in age among the two cohorts (4.15 ± 3.15 years in PVDO versus 2.375 ± 1.808, p = 0.9168); however, there was a higher proportion of females in the PVDO cohort compared with PVR (n = 9, 64.3% versus n = 2, 25%, p = 0.0381). Patients in both cohorts had a high incidence of prior cranial vault or neurosurgical procedures (12, 85.7% PVDO; 6, 75% PVR). Most patients were syndromic (n = 16, 72.7%) as outlined in Table 2. Of the syndromic patients, specific syndromes consisted of Crouzon (n = 6, 27.3%), Pfeiffer (n = 4, 18.2%), Apert (n = 2, 9.1%), and Saethre-Chotzen (9.1%). Notably, there was also a higher proportion of syndromic patients in the PVDO cohort (n = 12, 85.7%) than the PVR cohort (n = 4, 50%) (p = 0.0352; 95%) which is a potential confounder.
Perioperative data were gathered and compared among the two cohorts and are summarized in Table 3. All perioperative variables including mean operative duration, estimated blood loss, transfusion volume, location of VP shunt, ICU length of stay, and hospital length of stay were similar with no significant differences between the groups (all p > 0.05) (Table 3). It should be noted that estimated blood loss and transfusion volumes within the PVDO group were higher on average than the PVR group, which trended toward significance. This is best explained by two outliers within the PVDO cohort that had an estimated blood loss of 1200 cc and 2300 cc with transfusion volumes of 1200 cc and 2345 cc, while the remainder of the cohort ranged from an estimated blood loss (EBL) of 100 to 800 cc and transfusion volumes of 240 to 50 cc. Of further note, these two outliers were not among the patients who suffered post-operative shunt-related complications.
Indications for surgery were reviewed for all patients. Many patients had multiple indications for surgery, most commonly concerns for elevated ICP, recurrent shunt malfunctions in the setting of hydrocephalus, and/or turribrachycephaly. Concern for increased ICP was an indication for surgery in 57.1% of patients in the PVDO cohort and 50% of patients in the PVR cohort, demonstrating no significant difference (p = 0.750). Within the PVDO cohort, increased ICP was an indication for surgery in 60% of patients with complications (n = 3) and 55.6% of patients without complications (n = 5).
The most common shunt location was right occipital (n = 6, 27.3%), followed by right parietal (n = 5, 22.7%) and right frontal (n = 5, 22.7%); see Table 4. The shunt locations of the patients who suffered complications were occipital (2), parieto-occipital (1), parietal (1), and frontal (1). Within the PVDO cohort, 92.3% (n = 12) of pre-existing shunts were encountered, disconnected, or exchanged during surgery. Only one frontally placed pre-existing shunt was not exposed in this group, and one patient had the initial shunt placed at the time of distraction. Within the PVR cohort, 100% (n = 7) of pre-existing shunts were encountered during surgery. All shunts placed at our institution were the Codman antibiotic-impregnated system; for nine patients (40.9%), the system could be further classified as a Delta or Strata II system with valves set between performance levels 1.0 and 2.0 (Valve performance levels range from 0.5 to 2.5) [25]. Some patients had shunts placed at outside facilities, and therefore, the shunt characteristics are unknown.
Patients in the PVDO cohort were more likely to suffer from shunt-related or post-operative complications (n = 5) when compared with PVR (n = 0), (p = 0.0093.) Each of the five patients required a repeat operation for either shunt revision, externalization, or replacement. Of the patients who required additional surgery, four (80%) required multiple additional operations as a direct result of their shunt-related complication (Table 5).
All of the patients who had complications were found to have more than one. In the sub-analysis of the patients who had complications, each of these five patients had multiple readmissions (Table 6) (n = 5). In total, they accounted for 17 hospital readmissions. The most common complications were shunt malfunctions (n = 4, 80%) and shunt infections (n = 4, 80%). Other complications included wound infections (n = 3, 60%), prolonged CSF leaks (n = 2, 40%), and wound dehiscence (n = 1, 20%). Further, of the patients with complications, two used a Delta system and one used a Strata system, while the remaining two patients had no documentation of their shunt type due to initial placement at an outside facility.
Variables were compared between PVDO patients with and without complications (Table 7). There were no significant differences in the demographics, although the mean age of patients with complications was 2.36 years (± 1.99) compared to 5.14 years (±4.50) which approaches significance (p = 0.0686). Patients with complications also had an average of three prior surgeries to revise or replace existing VP shunts while the patients without complications had and average of 1.11 (p = 0.1114), which again approaches significance. Despite complications, patients with complications had no significant reduction in distraction distance or days in activation of distraction. Patients with complications had a significantly longer length of stay (LOS) compared to those without complications (11.20 days vs 3.89 days, p = 0.0237). Of note, PICU LOS trended towards longer in the complications group (7.4 days vs 2.11 days, p = 0.0753)
Discussion
Since PVDO was first described by White et al. [7] in 2009, it has become a popular technique for volumetric expansion of the posterior cranial vault. Its safety [12, 14, 24] and efficacy [26, 27] for the syndromic craniofacial population has been well documented, and the clinical applications have since been expanded to include non-syndromic patients [28]. Despite a wealth of encouraging literature over the past decade, our unit was able to identify a unique subset of patients that seemed to have higher rates of complications than would have been expected. This manuscript is the first to detail the complication rates and profile associated with PVDO in patients with pre-existing VP shunts.
The reported complication rates in relevant literature on PVDO patients (without shunt-dependent hydrocephalus) is about 30%, with the two most common complications being CSF leaks (10%) and local infections +/− incisional wound healing difficulties (6.9%) [29]. The complication rates of patients in our PVDO cohort were slightly more frequent (35.7%), with similar frequency of CSF leaks (14%) but considerably higher rates of wound infection +/− dehiscence (28.5%).
VP shunt infection rates have been reported as 5–20% [30,31,32,33], while the infection rate in our cohort was 28.5%. A sub-analysis of shunt type and location did not provide insight into potential causes for the high rates of complications. In all patients that had shunt placements at CHOP, the Delta or Strata II systems were used with Codman antibiotic-impregnated shunt tubing. Two of the five patients that sustained complications after PVDO had their initial VP shunts placed at other facilities.
We chose to compare patients with PVR and shunts to patients with PVDO and shunts because of the similar surgical soft tissue manipulations and cranial osteotomies; important differences between these two procedures include presence of vascularized bone and transcutaneous hardware in the PVDO cohort and devascularized bone and indwelling hardware in the PVR cohort. Thus, while the PVR group can serve as a control, it is important to note the differences between the techniques. Additionally, the indications for surgery may be different between the two groups, and this is an important factor that may lead surgeons to choose one procedure over another despite our data. As hypothesized and clinically recognized, patients with VP shunts who underwent PVDO were significantly more likely to have complications than those with shunts who underwent traditional PVR. Patients that sustained complications had significantly longer hospital LOS, multiple readmissions, and multiple return trips to the OR. It is difficult to explain the differences in complication rates, but the fact that infection was so prevalent in the PVDO cohort leads us to hypothesize a role for seeding of the shunt by the transcutaneous route given the presence of transcutaneous hardware. The high rates of shunt malfunction may be hypothesized to occur due to gradual repositioning of the shunt tubing during the activation phase of distraction. Neither hypothesis for infections nor malfunctions can be proven by our study methodology—we can only report associations given the retrospective nature—and other hypotheses must be entertained.
Shunt location, type, surgical soft tissue, and cranial approach were not significant predictive variables for shunt malfunctions after PVDO in our cohort. In a recent multivariate analysis, a study of over 1500 pediatric VP shunt patients listed multiple prior shunt revisions and an age less than 5 years as independent risk factors of shunt revisions [34]. In our PVDO group, shunt revisions as an independent factor of malfunction or infection may indicate that multiple exposures to the external environment may predispose the shunt to contamination by bacteria [34, 35]. The authors consider whether anteriorly placed shunts are less likely to be encountered, thereby contaminated, during PVDO. Our data indicate that 12/13 pre-existing shunts were exposed during surgery. The single unexposed shunt was frontally placed and was not among the patients with shunt infections. Still, there were two frontally placed shunts that were exposed in this cohort, one of whom did have shunt infections.Within the PVR cohort, operative reports and 3D reconstruction CT images indicated that all pre-existing shunts within this cohort were exposed, including those that were frontally placed.
An alternative theory for the increased incidence of shunt infection with PVDOs is that a semi-buried distractor arm creates a path to the external environment that may create a hostile environment for the shunt. In contrast, PVR represents a one-time exposure that is recovered without the same continued source of external contamination. In addition, the distraction process involves micro movement of the cranial bones that house the extracranial valve and tubing of the VP shunt. This micro motion and eventual displacement of the posterior segment may result in a small but consequential movement of the shunt itself. In a review of neurosurgery operative reports for shunt-related procedures after distraction, there was no indication that shunts had moved or become dislodged.
The average age of the shunted PVDO patients (4.15 years) in this study is considerably higher than PVDO without shunts. It is difficult to completely determine the need for shunts in all these patients. Some were referrals from outside institutions that managed elevated ICP with shunts primarily instead of offering cranial expansion. In addition, in some patients, there is an inherent hydrocephalus component that cannot be corrected with just expansion alone and requires the utilization of shunting the excess CSF production or facilitate appropriate removal. In our protocol, the utilization of PVDO in the syndromic multi-suture synostosis patient has two benefits: 1. It allows maximum cranial expansion to remove any doubt of increased intracranial pressure and impairment of brain development due to craniosynostosis. 2. This also allows us to bypass a front-orbital advancement (at age 1–2) in certain cases and treat the forehead retrusion, exophthalmos, and midface concavity with a monobloc distraction. It has been our experience that reducing the number of frontal surgeries allows for a better aesthetic contouring and integrity of bone in the forehead.
There are significant limitations to our study, the most important of which are its retrospective nature, variability in cohorts, and small sample size. We were unable to identify statistical significance in perioperative variables or surgical indications that would help identify specific risk factors for complications, a problem that may be solved by increasing numbers. For example, the average number of shunt revisions prior to PVDO in patients with complications (3) was higher than those without complications (1.11); however, we are unable to demonstrate significance. The PVDO and PVR cohorts had statistically significant differences in proportion of syndromic patients, not surprising given the difference in hydrocephalus rates between syndromic and non-syndromic craniosynostosis [16, 17]. Since syndromic patients have a higher propensity toward shunt dependency and made up the majority (80%) of the complications in our study, underrepresentation in one cohort is certainly limiting. This study also includes data from multiple craniofacial surgeons and multiple neurosurgeons who each have slight variations in technique. The small cohort size precludes analysis by individual surgeon team, but it is possible that such variability in technique may bias results.
Conclusion
In complex or syndromic craniosynostosis patients who have previously undergone ventricular shunting, PVDO is associated with higher shunt-related complications and need for additional procedures when compared to traditional PVR. While the benefits of PVDO in the treatment of syndromic craniosynostosis are well documented, the risks of PVDO in the face of a VP shunt must be considered. Further investigation into patient-specific risk factors and risk reduction strategies is warranted.
References
Buchanan EP, Xue AS, Hollier LH (2014) Craniofacial syndromes. Plast Reconstr Surg 134(1):128e–153e. https://doi.org/10.1097/PRS.0000000000000308
Panchal J, Uttchin V (2003) Management of craniosynostosis. Plast Reconstr Surg 111(6):2032–2048; quiz 2049. https://doi.org/10.1097/01.PRS.0000056839.94034.47
Morris L (2016) Management of craniosynostosis. Facial Plast Surg 32(2):123–132. https://doi.org/10.1055/s-0036-1582228
David LR, Proffer P, Hurst WJ, Glazier S, Argenta LC (2004) Spring-mediated cranial reshaping for craniosynostosis. J Craniofac Surg. 15(5):810–818
Wong GB, Kakulis EG, Mulliken JB (2000) Analysis of fronto-orbital advancement for Apert, Crouzon, Pfeiffer, and Saethre-Chotzen syndromes. Plast Reconstr Surg 105(7):2314–2323
Mackenzie KA, Davis C, Yang A (2009) R MM. Evolution of surgery for sagittal synostosis: the role of new technologies. J Craniofac Surg. 20(1):129–133. https://doi.org/10.1097/SCS.0b013e318190e1cf
White N, Evans M, Dover MS, Noons P, Solanki G, Nishikawa H (2009) Posterior calvarial vault expansion using distraction osteogenesis. Childs Nerv Syst 25(2):231–236. https://doi.org/10.1007/s00381-008-0758-6
Renier D, Lajeunie E, Arnaud E, Marchac D (2000) Management of craniosynostoses. Childs Nerv Syst 16(10-11):645–658. https://doi.org/10.1007/s003810000320
Sgouros S, Goldin JH, Hockley AD (1996) System MJC. Posterior skull surgery in craniosynostosis. Child’s Nerv Syst
Choi M, Flores RL, Havlik RJ (2012) Volumetric analysis of anterior versus posterior cranial vault expansion in patients with syndromic craniosynostosis. J Craniofac Surg. 23(2):455–458
Goodrich JT (2004) Craniofacial surgery: complications and their prevention. Semin Pediatr Neurol 11(4):288–300
Goldstein JA, Paliga JT, Wink JD, Low DW, Bartlett SP, Taylor JA (2013) A craniometric analysis of posterior cranial vault distraction osteogenesis. Plast Reconstr Surg 131(6):1367–1375. https://doi.org/10.1097/PRS.0b013e31828bd541
Derderian CA, Wink JD (2015) L MJ, Collinsworth A, Bartlett SP, Taylor JA. Volumetric changes in cranial vault expansion: comparison of fronto-orbital advancement and posterior cranial vault distraction osteogenesis. Plast Reconstr Surg 135(6):1665–1672. https://doi.org/10.1097/PRS.0000000000001294
Taylor JA, Derderian CA, Bartlett SP, Fiadjoe JE, Sussman EM, Stricker PA (2012) Perioperative morbidity in posterior cranial vault expansion: distraction osteogenesis versus conventional osteotomy. Plast Reconstr Surg 129(4):1–3. https://doi.org/10.1097/PRS.0b013e3182443164
Copeland AE, Hoffman CE, Tsitouras V, Jeevan DS, Ho ES, Drake JM, Forrest CR (2018) Clinical significance of venous anomalies in syndromic craniosynostosis. Plast Reconstr Surg - Glob Open 6(1):e1613. https://doi.org/10.1097/GOX.0000000000001613
Collmann H, Sörensen N, Krauss J, Mühling J (1988) Hydrocephalus in craniosynostosis. Childs Nerv Syst 4(5):279–285
Collmann H, Sörensen N, Krauß J (2005) Hydrocephalus in craniosynostosis: a review. Childs Nerv Syst 21(10):902–912. https://doi.org/10.1007/s00381-004-1116-y
Sgulò FG, Spennato P, Aliberti F, Di Martino G, Cascone D, Cinalli G (2017) Contemporary occurrence of hydrocephalus and Chiari I malformation in sagittal craniosynostosis. Case report and review of the literature. Childs Nerv Syst 33(1):187–192. https://doi.org/10.1007/s00381-016-3189-9
Bhasin RR, Chen MK, Pincus DW (2007) Salvaging the “lost peritoneum” after ventriculoatrial shunt failures. Childs Nerv Syst 23(5):483–486. https://doi.org/10.1007/s00381-006-0292-3
Del Bigio MR (2004) Cellular damage and prevention in childhood hydrocephalus. Brain Pathol 14(3):317–324
Cochrane DD, Kestle JR (2003) The influence of surgical operative experience on the duration of first ventriculoperitoneal shunt function and infection. Pediatr Neurosurg 38(6):295–301. https://doi.org/10.1159/000070413
Gottfried ON, Binning MJ, Sherr G, Couldwell WT (2005) Distal ventriculoperitoneal shunt failure secondary to Clostridium difficile colitis. Acta Neurochir {(Wien)} 147(3):335–338; discussion 338. https://doi.org/10.1007/s00701-004-0444-8
Tamburrini G, Caldarelli M, Massimi L, Gasparini G, Pelo S, Di Rocco C (2012) Complex craniosynostoses: a review of the prominent clinical features and the related management strategies. Childs Nerv Syst 28(9):1511–1523. https://doi.org/10.1007/s00381-012-1819-4
Derderian CA, Bastidas N, Bartlett SP (2012) Posterior cranial vault expansion using distraction osteogenesis. Childs Nerv Syst 28(9):1551–1556. https://doi.org/10.1007/s00381-012-1802-0
Lollis SS, Mamourian AC, Vaccaro TJ, Duhaime AC (2010) Programmable CSF shunt valves: radiographic identification and interpretation. Am J Neuroradiol 31(7):1343–1346. https://doi.org/10.3174/ajnr.A1997
Wiberg A, Magdum S, Richards PG, Jayamohan J, Wall SA, Johnson D. Posterior calvarial distraction in craniosynostosis—an evolving technique. J Craniomaxillofac Surg 2012;40(8):799-806. doi:https://doi.org/10.1016/j.jcms.2012.02.018
Thomas GP, Wall SA, Jayamohan J et al (2014) Lessons learned in posterior cranial vault distraction. J Craniofac Surg 25(5):1721–1727. https://doi.org/10.1097/SCS.0000000000000995
Zhang RS, Wes AM, Naran S, Hoppe IC, Sun J, Mazzaferro D, Bartlett SP, Taylor JA (2018) Posterior vault distraction osteogenesis in nonsyndromic patients: an evaluation of indications and safety. J Craniofac Surg. 29(3):566–571. https://doi.org/10.1097/SCS.0000000000004230
Greives MR, Ware BW, Tian AG, Taylor JA, Pollack IF, Losee JE (2016) Complications in posterior cranial vault distraction. Ann Plast Surg 76(2):211–215. https://doi.org/10.1097/SAP.0000000000000518
Woo PY, Wong HT, Pu JK et al (2016) Primary ventriculoperitoneal shunting outcomes: a multicentre clinical audit for shunt infection and its risk factors. Hong Kong Med J 22(5):410–419. https://doi.org/10.12809/hkmj154735
Prusseit J, Simon M, von der Brelie C, Heep A, Molitor E, Volz S, Simon A (2009) Epidemiology, prevention and management of ventriculoperitoneal shunt infections in children. Pediatr Neurosurg 45(5):325–336. https://doi.org/10.1159/000257520
Choux M, Genitori L, Lang D, Lena G (1992) Shunt implantation: reducing the incidence of shunt infection. J Neurosurg 77(6):875–880. https://doi.org/10.3171/jns.1992.77.6.0875
McGirt MJ, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ (2003) Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect Dis 36(7):858–862. https://doi.org/10.1086/368191
Erps A, Roth J, Constantini S, Liat L-G, Galia G-S (2018) Risk factors and epidemiology of pediatric ventriculoperitoneal shunt infection. Pediatr Int. https://doi.org/10.1111/ped.13709
MJ MG, Zaas A, Fuchs HE, George TM, Kaye K, Sexton DJ (2003) Risk factors for pediatric ventriculoperitoneal shunt infection and predictors of infectious pathogens. Clin Infect. https://doi.org/10.1086/368191
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Azzolini, A., Magoon, K., Yang, R. et al. Ventricular shunt complications in patients undergoing posterior vault distraction osteogenesis. Childs Nerv Syst 36, 1009–1016 (2020). https://doi.org/10.1007/s00381-019-04403-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04403-w