Abstract
Purpose
This manuscript describes our management philosophy of Chiari I malformation in children based on a single neurosurgeon’s personal experience.
Methods
Based on 61 infants and children with Chiari I malformation treated from 2007 to 2017, typical symptoms, surgical indications, types of surgery, and evaluation of surgical decompression are reviewed.
Results
Sixty-one patients had 69 decompressions, with 90% having symptom improvement. Seven (11.5%) needed reoperation, 1 of which needed 2 reoperations for recurrence. The recurrence rates were 20% (5 of 25) after dural scoring and 5.6% (2 of 36) after duraplasty (p = 0.1116, Fisher’s exact test). Six (16%) of 36 patients developed pseudomeningocele or CSF leak.
Conclusions
We recommend surgical intervention for Chiari I malformation for clearly symptomatic patients and those with significant hydromyelia regardless of symptoms. A bony decompression with dural scoring is recommended for patients with typical occipital headaches with a lesser degree of tonsillar descent, while an expansile duraplasty is standard for those with high-grade tonsillar descent, medullary kink, or hydromyelia. Intraoperative ultrasound is often helpful to ensure the adequacy of the decompression. Most patients will have improvements in symptom and imaging after either type of decompressive surgery.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The Chiari I malformation (CMI), with a displacement of the cerebellar tonsils below the foramen magnum, remains perplexing both in terms of its pathophysiology and its ideal treatment. While there are ongoing randomized studies and patient registries designed to determine the ideal treatment paradigm, current management generally follows institutional bias and personal experience.
Typical symptoms
The most common presentation of Chiari I malformation is headaches, particularly in the midline sub-occipital region. These headaches are due to an overcrowded craniocervical junction and lack of free CSF flow between the intracranial and spinal subarachnoid spaces. They are aggravated by Valsalva maneuvers such as coughing, sneezing, and laughing. Non-verbal infants and toddlers present with irritability, nighttime waking, and arching back as a sign of discomfort [1]. Neurological disturbances are uncommon though some present with increasing gait unsteadiness or paresthesia, in the extremities associated with hydromyelia. In infants and young children, oropharyngeal symptoms such as snoring, gagging, and sleep apnea are common [1]. Thoracolumbar scoliosis is usually associated with holocord hydromyelia.
Surgical indications
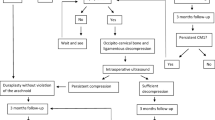
Surgical indications are based on presenting symptoms. Patients with above-described symptoms usually need surgical decompression. On MRI, pointy cerebellar tonsils descending to or below the C1 arch or with a medullary kink are considered to be of more indicated. The presence of hydromyelia is usually an indication for surgical decompression. Watchful waiting was recommended for minimally symptomatic patients and those with atypical headaches. This is in keeping with current global attitudes toward surgical intervention, as demonstrated in a recent international survey in which > 90% of responding pediatric neurosurgeons would observe an asymptomatic CMI, and over 80% would recommend surgery for a patient with a significant hydromyelia [2].
Types of surgery for Chiari I decompression
Two surgical techniques are practiced for Chiari decompression: one is bone decompression (posterior fossa craniotomy and C1 posterior arch resection) with dural scoring, and the other is bone decompression with duraplasty ± tonsillar reduction. The extent of bone removal is based on the preoperative MR sagittal images. The upper end of occipital craniectomy is limited below the superior nuchal line. C1 posterior arch resection is done routinely. Dural scoring vs. duraplasty is decided by the extent of the subarachnoid expansion dorsally to the herniated cerebellar tonsils based upon the intraoperative ultrasonography (US). Dural scoring is done by stripping the external layer of the cervical dura up to the level of the foramen magnum. The dural scoring is limited to the spinal dura because the intracranial dura is thin and difficult to score.
Dural opening and duraplasty are performed in the case of persistent tightness at the foramen magnum by intraoperative US, tonsils descending to C1 or below, significant medullary kinking, or presence of hydromyelia. Exploration of the cerebellar vallecula allows clearing of a veil-like structure, if present, at the obex in the case of hydromyelia. When the cerebellar tonsils are too large in the spinal subdural space, bilateral tonsillar tip reduction is performed with either bipolar cautery or microsurgical resection. This procedure brings up the tonsillar tip to the level of the foramen magnum, and the fourth ventricle communicates the CSF to subarachnoid space. Dural substitutes are used to augment the subdural space, and the dural closure should be water-tight.
Dural scoring leads to less augmentation of the subdural space compared to duraplasty, but there are concerns of CSF leak, pseudomeningocele, chemical meningitis, or subdural hygroma following duraplasty. Our institution has previously reported on the effectiveness of dural scoring as a treatment option, finding a 72.2% improvement rate for scoring as compared to 68.4% and 60.8% for duraplasty and tonsillar manipulation, respectively. Dural scoring was also associated with a significantly lower complication rate than these procedures (5.6% compared to 42.1% and 21.7%) [3].
Laminectomy of C2 should be avoided due to a large number of muscular attachments and the risk of post laminectomy kyphosis, which occurs more commonly in multi-level Chiari decompressions [4].
Evaluation of surgical outcome
Clinical improvement or resolution of symptoms is the most important indications of a good result. On postoperative MRI, less crowding of the posterior fossa, with expansion of CSF spaces around the cerebellum, brain stem, and upper cervical cord are indications of good anatomical response. In the case of hydromyelia, its reduction or resolution is a good indicator as well.
Presentation of the personal series: results and complications
From 2007 to 2017, the senior author performed 69 decompressions on 61 patients with an isolated Chiari I malformation. Thirty-three patients were female (54%), and the average age at surgery was 8.9 years. Patients most commonly present with headaches, frequently in occipital location, occurring in 50 (72%) of cases. Eleven children (16%) had oropharyngeal dysfunction, 10 of whom were under age 5, and 7 (10%) had other cerebellar symptoms. The Chiari malformation was an incidental or minimum finding in 14 children, of which a majority had hydromyelia. Tonsillar descent ranged from 2 to 30 mm, with a mean of 11.6 mm. A hydromyelia was present in 25 cases (36%), ranging in size from a single level to the entire spinal cord (holocord), with a mean of 8.7 spinal levels.
All patients underwent a suboccipital bony decompression, approximately 2.5–3.0 cm by 2.5–3.0 cm dependent on the patient size together with a C1 laminectomy. The thick occipito-cervical junction dural band was removed. Intraoperative ultrasound was used to evaluate cerebrospinal fluid (CSF) flow after the initial bone opening. In only three children, all without hydromyelia, the bony decompression was sufficient to restore CSF flow. If the bony decompression did not appear adequate, dural scoring was performed. Intraoperative US is again performed after scoring. This was sufficient in 22 cases (36%), only 4 of whom had hydromyelia. Thus, 25 patients did not have intraoperative CSF exposure (dural scoring group) A redundant expansile duraplasty was performed using Durepair™ dural regeneration matrix (Medtronic) for the remaining 36 cases (duraplasty group), of whom nearly half (21) had a hydromyelia. Tonsillar tip reduction using bipolar cautery or microsurgery was subsequently performed in 20 cases (32%). All dural scoring and duraplasty were done under surgical microscope.
After the first surgery, 18 patients had symptom resolution and 37 had symptom improvement, for a total of 90% improvement rate. Five had unchanged symptoms and only one had worsened symptoms.
All but four children had improved imaging postoperatively. Three cases were still noted to have crowding at the neo-foramen magnum and underwent reoperation, although all three of these had improvement in their symptoms. One child with improved symptoms had no postoperative imaging completed at our institution.
Seven children (11.5%) required redo surgery, including one with 2 redo surgeries, comparable with reported results from 7% [5] to 32% [6] in the literature. Index surgery of these seven was dural scoring in five patients and duraplasty in the remaining two. Recurrence rates for our series were not statistically significant; 5 of 25 (20%) for dural scoring and 2 of 36 (5.6%) for duraplasty (p value of 0.1116 by Fisher’s Exact Test). This data endorses a recent meta-analysis suggesting that there is no difference in recurrence rates between duraplasty and non-duraplasty procedures [7].
Complications primarily occurred among children with a duraplasty group. Six patients of 36 (17%) had a pseudomeningocele or CSF leak. One of these was managed conservatively, the other five required six surgical repairs. One patient with a pseudomeningocele requiring surgery also developed ventriculitis and hydrocephalus requiring an external ventricular drain and eventual shunting. Two patients, both of whom had duraplasty and tonsillar manipulation, went on to develop subdural fluid collections and hydrocephalus. These were successfully treated with conservative management consisting of acetazolamide and high-dose dexamethasone [8].
Based on our experience, we recommend surgical intervention for Chiari I malformation for clearly symptomatic patients and those with significant hydromyelia regardless of symptoms. A bony decompression with dural scoring is recommended for patients with typical occipital headaches with a lesser degree of tonsillar descent, while an expansile duraplasty is standard for those with high-grade tonsillar descent, medullary kink, or hydromyelia. While the dural scoring procedure may have a higher recurrence rate, the duraplasty procedure tends to have more CSF related complications. Intraoperative ultrasound is often helpful to ensure the adequacy of the decompression. Most patients will have symptom and imaging improvement after either type of decompressive surgery.
References
Grahovac G, Pundy T, Tomita T (2018) Chiari type I malformation of infants and toddlers. Childs Nerv Syst 34(6):1169–1176
Singhal A, Cheong A, Steinbok P (2018) International survey on the management of Chiari 1 malformation and syringomyelia: evolving worldwide opinions. Childs Nerv Syst 34(6):1177–1182
Navarro R, Olavarria G, Seshadri R, Gonzales-Portillo G, McLone DG, Tomita T (2004) Surgical results of posterior fossa decompression for patients with Chiari I malformation. Childs Nerv Syst 20(5):349–356
McLaughlin MR, Wahlig JB, Pollack IF (1997) Incidence of postlaminectomy kyphosis after Chiari decompression. Spine 22(6):613–617
McGirt MJ, Attenello FJ, Atiba A, Garces-Ambrossi G, Datoo G, Weingart JD, Carson B, Jallo GI (2008) Symptom recurrence after suboccipital decompression for pediatric Chiari I malformation: analysis of 256 consecutive cases. Childs Nerv Syst 24(11):1333–1339
Krishna V, McLawhorn M, Kosnik-Infinger L, Patel S (2014) High long-term symptomatic recurrence rates after Chiari-1 decompression without dural opening: a single center experience. Clin Neurol Neurosurg 118:53–58
Lu VM, Phan K2 Crowley SP, Daniels DJ (2017) The addition of duraplasty to posterior fossa decompression in the surgical treatment of pediatric Chiari malformation type I: a systematic review and meta-analysis of surgical and performance outcomes. J Neurosurg Pediatr 20(5):439–449
Vivas AC, Shimony N, Jackson EM, Xu R, Jallo GI, Rodriguez L, Tuite GF, Carey CM (2018) Management of hydrocephalus and subdural hygromas in pediatric patients after decompression of Chiari malformation type I: case series and review of the literature. J Neurosurg Pediatr22(4): 426–438
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors report no conflict of interest concerning the material or methods used in this study or the findings specified in this paper.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gernsback, J., Tomita, T. Management of Chiari I malformation in children: personal opinions. Childs Nerv Syst 35, 1921–1923 (2019). https://doi.org/10.1007/s00381-019-04180-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-019-04180-6