Abstract
Introduction
Complications following cranioplasty with either autografts or cranial implants are commonly reported in pediatric patients. However, data regarding cranioplasty strategies, complications and long-term outcomes are not well described. This study systematically reviews the literature for an overview of current cranioplasty practice in children.
Methods
A systematic review of articles published from inception to July 2018 was performed. Studies were included if they reported the specific use of cranioplasty materials following craniectomy in patients younger than 18 years of age, and had a minimum follow-up of at least 1 year.
Results
Twenty-four manuscripts, describing a total of 864 cranioplasty procedures, met the inclusion criteria. The age of patients in this aggregate ranged from 1 month to 20 years and the weighted average was 8.0 years. The follow-up ranged from 0.4 months to 18 years and had a weighted average of 40.4 months. Autologous bone grafts were used in 484 cases (56.0%). Resorption, infection and/or hydrocephalus were the most frequently mentioned complications. In this aggregate group, 61 patients needed a revision cranioplasty. However, in 6/13 (46%) papers studying autologous cranioplasties, no data was provided on resorption, infection and revision cranioplasty rates. Cranial implants were used in 380 cases (44.0%), with custom-made porous hydroxyapatite being the most commonly used material (100/380, 26.3%). Infection and migration/fracturing/loosening were the most frequently documented complications. Eleven revision cranioplasties were reported. Again, no data was reported on infection and revision cranioplasty rates, in 7/16 (44%) and 9/16 (56%) of papers, respectively.
Conclusion
Our systematic review illuminates that whether autografts or cranial implants are used, postcranioplasty complications are quite common. Beyond this, the existing literature does not contain well documented and comparable outcome parameters, suggesting that prospective, long-term multicenter cohort studies are needed to be able to optimize cranioplasty strategies in children who will undergo cranioplasty following craniectomy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniectomy is a commonly performed procedure in adult and pediatric patients, mainly suffering from medically refractory elevated intracranial pressure (ICP) in the setting of traumatic brain injury (TBI), vascular pathologies, or various other conditions [6, 45]. With advances in operative and perioperative care, more craniectomy patients survive their initial insult and eventually require subsequent cranioplasty procedures [6, 47].
Cranioplasty is necessary to restore cosmesis and to protect the underlying dura and brain from physical insult. Furthermore, restoration of normal cranial vault geometry contributes to neurological recovery by reversing the abnormalities in cerebral blood flow, cerebrospinal fluid hydrodynamics, and metabolic activity that result from craniectomy [47].
In adults, numerous materials have been used for cranioplasty to repair the cranial defect. Cranial vault reconstruction with the original autologous bone flap has gained support over time and is favored for its strength and elasticity, biocompatibility, durability, general accessibility, resistance to infection, and natural recovery of its feature to maintain the cranial contour [7, 22, 45, 46]. In cases with destruction or loss of the original calvarium (particularly for re-do cranioplasty after initial infection), synthetic materials are still frequently used for reconstruction. Methyl methacrylate is the most extensively used cranial implant material in patients above 18 years of age [3], but there are many alternatives such as glass-fiber-reinforced composite, titanium-based plates and mesh, hydroxyapatite, acrylic compounds (polymethyl methacrylate), ceramic compounds (the calcium phosphate-based cements), and plastic polymers such as porous polyethylene [22, 41, 42].
In pediatric patients, the skull is still growing and the bony contour is dynamic, which places specific constraints on materials that can be used for cranial vault reconstruction [15]. Also, thinner scalp and a better long-term survival prognosis further restrict usable bone replacements [10, 15]. Cranioplasty materials to be used in children should be able to grow with the skull, be durable for a long period of time and have a high resistance to late infection [13].
The most commonly used cranioplasty materials in adults do not meet these pediatric criteria [15]. Therefore, autologous bone grafts such as particulate bone graft, split calvarial bone graft, as well as extracranial bone sources, have been historically favored for children over synthetic materials such as acrylic or metals [2, 13, 22, 28, 30, 34, 38, 43]. These autologous grafts have their own set of complications, the most common of which is bone resorption, with reported rates ranging from 21 to over 80% [6, 27, 34, 44]. Autologous bone can be difficult to mold, and the limited amount that can be harvested may not sufficiently cover the whole cranial defect [22].
When autograft fails, or is not available or chosen as initial reconstruction method, cranial implant cranioplasty has been reported to be up to 90% efficacious [6], with success attributed to shapeable fit with the cranial contour and unlimited amount. However, these cranial implants may carry a risk of infection and immunological reactions, contamination, pathologic ossification, and fragmentation [22, 36].
While there are several retrospective studies assessing complications of cranioplasty in adults [2, 7, 15, 24, 36, 42, 47], similar pediatric cranioplasty studies remain scarce—primarily focused on the influence of bone flap size, timing of cranioplasty, and patient age on the durability of the bone flap replacement [17, 34, 40, 49]. Although new methods and techniques for the use of cranioplasty in pediatric patients have recently emerged, most manuscripts have only discussed one particular cranioplasty material at a time [8,9,10, 16, 19, 20, 23, 28, 37, 39, 41, 51, 52]. It is hard to draw significant conclusions from these studies since long-term outcomes are lacking and only small sample sizes were used [8,9,10, 16, 20, 39, 41, 51, 52]. This systematic review of cranioplasties in the pediatric population aims to synthesize these smaller studies into a coherent aggregate for a better understanding of cranioplasty strategies, complications, and possible long-term outcomes in children.
Methods
This review was performed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines, an evidence-based set of criteria for reporting in systematic reviews and meta-analyses [35].
Search strategy
To capture as many relevant publications as possible, an elaborate search of the electronic medical databases of PubMed (1950 to 2018), Embase (1981 to 2018), and Medline (1981 to 2018) was performed.
These databases were searched using the key words “cranioplasty” and “children” in conjunction with either “long-term,” “materials,” or “craniectomy”. The reference sections of included studies were also examined to identify relevant papers. Of this total number of studies (n = 655), duplicates were removed. Searches were limited to the English language and to clinical studies (Fig. 1).
Study selection
The remaining records (n = 393) were screened for “cranioplasty,” “decompressive craniectomy,” and “materials” in their titles or abstracts. After screening of the citations on these key words, the abstracts of articles of interest were then reviewed in detail by using inclusion and exclusion criteria, specified a priori as follows:
-
Pediatric patients were defined as those younger than 18 years of age.
-
The minimal follow-up of these patients needed to be more than 1 year.
-
To be included, the papers had to share results of the use of specific cranioplasty materials after decompressive craniectomy in pediatric patients. Cranioplasty materials included autologous bone and/or one or more synthetic material(s).
-
Retrospective analyses, cohort studies, and clinical trials were all deemed eligible for inclusion.
-
Individual case reports and systematic reviews (with no original data) were excluded from this review. When the papers contained results of the use of cranioplasty for treatment of any form of craniostenosis or craniosynostosis, they were also excluded from the review.
Of the 393 studies, 240 could be excluded after reading the abstract alone, and another 129 could be excluded after reading the full text (illustrated in Fig. 1). Twenty-four articles remained from this screening process, involving 864 cranioplasty procedures, and these were analyzed [5, 6, 8,9,10, 13, 16, 17, 19, 20, 22, 27,28,29, 33, 34, 39,40,41, 43, 48, 50,51,52].
Statistical analysis was performed using IBM SPSS Statistics, version 25 [IBM Corp., Armonk, NY, USA].
Results
Twenty-four manuscripts describing outcomes and complications following cranioplasty in the pediatric population after decompressive craniectomy met search criteria for this study (Table 1). Several articles also reported information about time until bone flap replacement, patient age, or other potential risk factors [6, 17, 27, 40]. Twenty-one of the 24 included articles met CEBM criteria for level 4 as case series [5, 6, 8,9,10, 13, 16, 17, 22, 27,28,29, 33, 39,40,41, 43, 48, 50,51,52], and the remaining studies met criteria for level 3 as either a controlled cohort study or post-marketing surveillance studies [19, 20, 34]. Three multicenter studies [19, 20, 33] and one prospective study of eight cases [41] were included. The remainder were all retrospective, single-center studies. All studies collectively described 864 total cranioplasty procedures.
The age of all included patients in the aggregate ranged from 1 month to 20 years [6, 8,9,10, 13, 16, 17, 19, 20, 22, 27,28,29, 33, 34, 39,40,41, 43, 48, 50,51,52] and the weighted average was 8.0 years [5, 6, 8,9,10, 16, 19, 20, 22, 27,28,29, 39, 40, 43, 48, 50,51,52].
The duration of follow-up ranged from 0.4 months to 18 years [6, 8,9,10, 13, 16, 20, 22, 27, 28, 33, 34, 39,40,41, 43, 48, 51] and had a weighted average of 40.4 months [5, 6, 8,9,10, 16, 19, 20, 22, 27, 28, 33, 34, 39,40,41, 43, 48, 50, 51].
Autologous bone grafts were used in 484 cases (56.0%) [6, 13, 17, 22, 27,28,29, 33, 34, 40, 43, 48, 50] and cranial implants in 380 cases (44.0%) [5, 8,9,10, 16, 19, 20, 22, 29, 33, 34, 39, 41, 50,51,52].
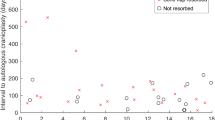
Autologous cranioplasty
Autologous cranioplasty was used in 484 cases (56.0%, Table 2). Time until bone flap replacement was reported in 220 (45.5%) of these, ranging from 1 week to 17 months [6, 22, 27, 34, 40, 50] with a weighted average of 4.7 months [6, 22, 27, 40, 50]. The follow-up period ranged from 0.4 to 216 months [6, 13, 22, 27, 28, 33, 34, 40, 43, 48] and had a weighted average of 43.9 months [6, 22, 27, 28, 33, 34, 40, 43, 48, 50].
An autologous bone flap replacement using the original bone flap was used in 359 of 484 cases (74.2%) [6, 17, 27, 29, 33, 34, 40, 43, 50]. In the remaining autologous grafts, 70 split calvarial bone grafts (14.4%) [13, 22, 29, 33], 42 particulate bone grafts (8.7%) [22, 28], and 13 rib grafts (2.7%) [48] were used. In six out of 13 (46%) papers that studied autologous grafts, no data on resorption, infection, and revision cranioplasty rates were reported.
Reported complications were associated with 32.6% of all autologous cranioplasties. Out of the 484 autologous cases, 80 (16.5%) documented resorption as a complication [6, 13, 17, 27, 34, 40, 43], with infection in 19 (3.9%) [6, 27,28,29, 34, 40, 43], and hydrocephalus in 35 (7.2%) [6, 17, 27, 34, 40]. Five patients did not achieve an acceptable cosmetic outcome (1.0%) [22, 29, 43] and three had problems with migration, fracturing, or loosening (0.6%) [17]. Seven patients developed subdural hygroma (1.4%) [17, 34]. Other postcranioplasty outcomes included existence of residual bone defects (0.6%), shunt infections (0.4%), behavioral issues (0.2%), sterile wound dehiscence (0.2%), seroanguinous sterile wound discharge (0.2%), and non-ossification of the graft (0.2%) [22, 28, 29, 34]. Sixty-one patients (12.6% of autologous grafts) required revision cranioplasty [6, 17, 27,28,29, 34, 43].
Cranial implants
Cranial implants were used in 380 cases (44.0%, Table 2). The interval between craniectomy and cranioplasty was reported in 51 of these, ranging from 15 days to 12.6 months [34, 50] with a weighted average of 31.1 months [16, 22, 50]. The duration of follow-up ranged from 0.4 to 130 months [8,9,10, 16, 20, 22, 33, 34, 39, 41, 51] and had a weighted average of 36.6 months [5, 8,9,10, 16, 19, 20, 22, 33, 34, 39, 41, 50, 51].
Custom-made porous hydroxyapatite (CustomBone Service) was the most common used cranial implant, used in 100 cases (26.3%) [19, 20]. Titanium was used for 60 cases (15.8%) [22, 29, 33, 50, 51], polymethyl methacrylate/polyhydroxyethyl methacrylate for 41 cases (10.8%) [5], hydroxyapatite for 40 cases (10.5) [9, 39, 52], polyetheretherketone for 36 cases (9.5%) [5, 22, 33], carbonated apatite cement for 34 cases (8.9%) [10], polymethyl methacrylate for 31 cases (8.2%) [16, 22, 34], demineralized bone matrix for 13 cases (3.4%) [8], porous polyethylene (MedPor) for 9 cases (2.4%) [22], glass-fiber reinforced composite in 8 cases (2.1%) [41], and methyl methacrylate for 7 cases (1.8%) [29, 50]. One cranioplasty was performed with an unspecified cranial implant (0.3%) [22].
From the 16 papers that addressed cranial implants, seven of those (44%) did not report on infection rate and nine (56%) papers failed to provide data on revision cranioplasty rates.
The overall reported complication rate in the cranial implant group was 14.2%. Documented complications were infection in 20 cases (5.3%) [5, 9, 19, 20, 33, 41], migration, fracturing, or loosening in 10 cases (2.6%) [16, 19, 20] and cerebrospinal fluid leakage in 2 cases (0.5%) [5, 41]. Furthermore, behavioral issues were reported in 2 cases (0.5%), headaches in 5 cases (1.3%), and increased sensitivity of the ear and lateral rectus muscle impingement both in 1 case (0.3% each) [22]. The authors did not report which of their various cranial implants let to the occurrence of these complications.
Other postcranioplasty outcomes included existence of residual bone defects (0.5%), postoperative implant adjustments (0.5%), subgaleal hematomas (0.5%), recurrent subgaleal fluid collections (0.3%), seroma (0.3%), intracranial hypotension (0.3%), EEG alterations (0.3%), granuloma formation (0.3%), left central retinal occlusion (0.3%), and skin retraction (0.3%) [5, 8, 9, 16, 19, 33, 51, 52]. Eleven patients (2.9% of cranial implants) required revision cranioplasty [16, 19, 20, 41].
Five studies [22, 29, 33, 34, 50] compared autologous bone to synthetic material cranioplasty. The remainder only included patients who had all undergone cranioplasty using either an autologous bone graft or a cranial implant.
Fu et al. documented a complication rate of 27.3% (3/11) in the autologous group and a 30.0% (9/30) complication rate in the cranial implant group [22].
Josan et al. documented an autologous complication rate of 20.8% (5/24) and an cranial implant complication rate of zero [29].
Ma et al. did not report any complications in the autologous group or in the group of patients with a synthetic PEEK implant, since there was a primary focus on outcomes following titanium cranioplasty. A complication rate of 9.1% (3/33) was documented in the titanium group [33].
Martin et al. documented an autologous complication rate of 73.9% (17/23). No complications were reported in the cranial implant group [34].
Waqas et al. reported on the major postcranioplasty complications (infection, cosmetic problems, wound dehiscence, and cerebrospinal fluid leak) noted in their cohort, but did not specify which material caused which complication. However, there was no significant difference in complication rates between autologous or cranial implant cranioplasty [50].
In this systematic review, an infectious complication was reported in 19 out of 484 cases in the autologous group and in 20 out of 380 cases in the cranial implant group, a difference that did not reach statistical significance (p = 0.56).
There was a need for cranioplasty replacement in 61 out of 484 autologous cases and 11 out of 380 cranial implant cases, but the difference was not statistically significant (p = 0.12).
Discussion
In the reviewed literature of pediatric cranioplasties, autologous cranioplasty was used in 484 cases (56.0%) in which a complication rate of 32.6% was experienced in a weighted mean follow-up period of 43.9 months.
Cranial implants were used in 380 cases (44.0%) with a total complication rate of 14.2% in a weighted mean follow-up period of 36.6 months.
Autologous cranioplasty
Autologous bone graft has been generally advocated as the gold standard of calvarial reconstruction in pediatric patients, due to its ability to remodel and become integrated with the growing pediatric skull over time [30].
However, it is not without its problems. As shown, the main complication following autologous cranioplasty is bone flap resorption (80/484, 16.5%). This resorption rate is reasonably high, but lower than what might have been expected from (individually) reported resorption rates in the literature, ranging from 21 to over 80% [6, 27, 34, 44]. This difference might be due to the lack of age stratification in the reported literature, since young age is considered to be a risk factor for bone flap resorption [6, 17, 18, 34, 40, 44]. However, not all included studies inquired the correlation between young age and the risk of bone flap resorption [13, 27, 43].
In addition, a considerable number of papers that studied autologous grafts did not report data on resorption (6/13, 46%). This missing data could also have contributed to the relatively low resorption rate.
Other, less-common, complications include infection and hydrocephalus, unacceptable cosmetic outcome, or a mechanical risk of migration, fracture, or loosening of the bone flap.
Autologous cranial bone is often available only in limited quantities and the harvest of extracranial sources of bone such as rib can be complicated by pain, pneumothorax, and chest wall deformity [31]. When an autograft is used for bone flap replacement, it is more likely that surgical time, wound size, and amount of soft tissue dissection will increase [4, 22, 29].
Cranial implants
Over time, effort has been devoted to the development of bone substitutes that can become integrated with the growing pediatric skull [1, 4, 16, 32, 39, 41, 52].
In adults, methyl methacrylate has been generally accepted as the preferred material for bone flap replacement. However, synthetic material is less frequently used in the pediatric population because of concern for growth restriction and/or implant instability.
It is believed that, because it is non-expansible, methyl methacrylate does not remodel to and integrate with the pediatric cranium. Thus, it has been suggested that this material should be avoided in pediatric patients less than 5 years of age [29]. However, Fu et al. found that there was no clinical evidence of growth restriction when cranial implants (such as methyl methacrylate) were used for pediatric cranioplasty [22].
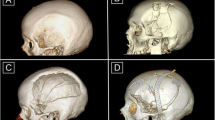
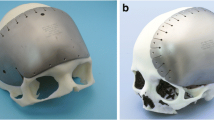
Other synthetic implant materials include titanium plates and meshes, hydroxyapatite, porous polyethylene, polyetheretherketone, and glass-fiber reinforced composite. Although titanium is a strong material and provides resistance to infection, it is difficult to contour to a child’s natural skull shape, and it creates large artifacts in CT scans [1, 27, 29].
Hydroxyapatite is the principal component in the bone and is thus considered as a near-ideal bone substitute [12, 14, 26]. However, the hand-made bone cement appears to be unsuitable for the growing pediatric skull, can experience loss of structural integrity when exposed to cerebrospinal fluid or blood, and has high rates of infection and erosive material exposure [11, 12, 14, 26, 27, 36]. To overcome these problems, custom-made porous hydroxyapatite implants have been developed. These implants showed few complications and appeared to be an effective cranial reconstruction material in pediatric patients [19,20,21].
Porous polyethylene has been used extensively in adult cranial reconstruction since it theoretically has the capacity for fibrous ingrowth and revascularization [22]. Long-term data on the use of porous polyethylene in reconstructing pediatric calvarial defects are lacking, although one study reported successful early outcomes without documentation of growth disturbance [32]. Inert, polyetheretherketone implants, are durable and useful when a large defect with a complex contour has to be restored; they are easily removable should a recurrence of intracranial access be needed, but lack any osteoconductive or inductive properties [22, 25].
Early cranioplasty outcomes with the glass fiber-reinforced composite were found to be promising. Piittulainen et al. reported two patients that had their implant removed due to an underlying surgical site infection (out of 8 implants), but after adequate treatment, good and safe outcomes were achieved, both functionally and in terms of cosmetic appearance of the patients [41].
The results of this systematic review show that there is a substantial lack of equal and uniform outcome parameters regarding potential postcranioplasty complications following either autologous or cranial implant cranioplasty in the pediatric population.
Five years ago, Rocque et al. [45] performed a systematic review on potential risk factors that could predispose pediatric cranioplasty patients to postoperative complications and also concluded there is a significant lack of uniform data regarding this important issue. Since then, 12 additional papers appeared reviewing the outcomes of pediatric patients undergoing cranial reconstruction [5, 16, 19, 20, 22, 33, 34, 41, 44, 50,51,52]. Although all of them have contributed valuable data on this topic, it remains difficult to draw significant conclusions that could definitely guide clinical practice.
One of these papers concerns a recently published study [44]. This manuscript did not meet the inclusion criteria for this review (since it did not specifically list the used implant materials), but it does have pertinent results.
This North-American multicenter retrospective study presented data on a large cohort of 359 patients to determine risk factors for resorption and infection after pediatric cranioplasty [44]. In this cohort, an infection rate of 10.5% was reported. Bone resorption occurred in 21.7% out of the 240 patients who underwent autologous cranioplasty.
Important risk factors regarding perioperative management that led to these postcranioplasty complications were assessed. Young age and the use of external ventricular drains and lumbar shunts were important predictors of bone resorption, while ventilator dependence and the presence of a VP shunt or gastrostomy were significant risk factors for infection. The material used for cranioplasty was not found to be associated with infection. However, it remains unclear how cranioplasty material may affect more long-term complication risks like growth restriction, fracturing, loosening, and the onset of late infection.
It is essential to obtain a better understanding of more long-term outcomes following cranioplasty in the pediatric population since potential complications like a lack of osteointegration or insufficient growth capacity could occur after a long period of time. We would encourage that all patients should be monitored and should continue clinical reassessment regularly at least during the period of skull growth, but preferably over a longer period of time. Follow-up visits should include assessment of wound healing, stability or migration, ossification or resorption of the graft, as well as symmetry and skull shape. While migration, ossification, or resorption can be assessed by CT-scans, medical (2D and/or 3D) photography, sufficient cosmetic outcome can be determined by parents or patients via surveys.
This follow-up should be significantly longer than the existing follow-up duration of the most recent paper [44] and of the papers included in this systematic review, i.e., 32 and 40.4 months respectively.
It has not been possible to perform a meaningful comparison and/or meta-analysis on the association between cranioplasty material and postcranioplasty complications. There was lack of data and scarcity exists on uniform outcome parameters. Also, almost all studies were retrospective and single-center studies with a small number of patients. Therefore, based on the results of this systematic review, it is difficult to draw any meaningful conclusion to help guide clinical practice in the decision on when to opt for which type of cranioplasty.
While a randomized controlled trial would be the gold standard to analyze how cranioplasty material may effect postcranioplasty complication risk and outcomes, this is, ethically and logistically, very difficult to implement. A large-scale prospective multicenter study involving clear outcome parameters followed over a long period of time can overcome the issues discussed before.
Conclusion
Whether autografts or cranial implants are used, postcranioplasty complications and need for revision cranioplasty are quite common.
Beyond this, our systematic review illuminates that the existing literature does not contain well documented and comparable outcome parameters, suggesting that prospective, long-term multicenter cohort studies are needed to be able to optimize cranioplasty strategies in children who will undergo cranioplasty following craniectomy.
References
Arnaud E (2000) Advances in cranioplasty with osteoinductive biomaterials: summary of experimental studies and clinical prospects. Childs Nerv Syst 16:659–668. https://doi.org/10.1007/s003810000321
Artico M, Ferrante L, Pastore FS, Ramundo EO, Cantarelli D, Scopelliti D (2003) Bone autografting of the calvaria and craniofacial skeleton: historical background, surgical results in a series of 15 patients, and review of the literature. Surg Neurol 60:71–79
Aydin S, Kucukyuruk B, Abuzayed B, Aydin S, Sanus GZ (2011) Cranioplasty: review of materials and techniques. J Neurosci Rural Pract 2:162–167. https://doi.org/10.4103/0976-3147.83584
Blum KS, Schneider SJ, Rosenthal AD (1997) Methyl methacrylate cranioplasty in children: long-term results. Pediatr Neurosurg 26:33–35. https://doi.org/10.1159/000121158
Bowers CA, McMullin JH, Brimley C, Etherington L, Siddigi FA, Riva-Cambrin J (2015) Minimizing bone gaps when using custom pediatric cranial implants is associated with implant success. J Neurosurg Pediatr 16:439–444. https://doi.org/10.3171/2015.2.PEDS14536
Bowers CA, Riva-Cambrin J, Hertzler DA 2nd, Walker ML (2013) Risk factors and rates of bone flap resorption in pediatric patients after decompressive craniectomy for traumatic brain injury. J Neurosurg Pediatr 11:526–532. https://doi.org/10.3171/2013.1.PEDS12483
Chang V, Hartzfeld P, Langlois M, Mahmood A, Seyfried D (2010) Outcomes of cranial repair after craniectomy. J Neurosurg 112:1120–1124. https://doi.org/10.3171/2009.6.JNS09133
Chao MT, Jiang S, Smith D, DeCesare GE, Cooper GM, Pollack IF, Girotto J, Losee JE (2009) Demineralized bone matrix and resorbable mesh bilaminate cranioplasty: a novel method for reconstruction of large-scale defects in the pediatric calvaria. Plast Reconstr Surg 123:976–982. https://doi.org/10.1097/PRS.0b013e31819ba46f
Choi SH, Levy ML, McComb JG (1998) A method of cranioplasty using coralline hydroxyapatite. Pediatr Neurosurg 29:324–327. https://doi.org/10.1159/000028747
Cohen AJ, Dickerman RD, Schneider SJ (2004) New method of pediatric cranioplasty for skull defect utilizing polyactic acid absorbable plates and carbonated apatite bone cement. J Craniofac Surg 15:469–472
Costantino PD, Chaplin JM, Wolpoe ME, Catalano PJ, Sen C, Bederson JB, Govindaraj S (2000) Applications of fast-setting hydroxyapatite cement: cranioplasty. Otolaryngol Head Neck Surg 123:409–412. https://doi.org/10.1067/mhn.2000.107679
Ducic Y (2002) Titanium mesh and hydroxyapatite cement cranioplasty: a report of 20 cases. J Oral Maxillofac Surg 60:272–276
Edwards MSB, Ousterhout DK (1987) Autogeneic skull bone grafts to reconstruct large or complex skull defects in children and adolescents. Neurosurgery 20:273–280
Eppley BL, Hollier L, Stal S (2003) Hydroxyapatite cranioplasty: II. Clinical experience with a new quick-setting material. J Craniofac Surg 14:209–214
Feroze AH, Walmsley GG, Choudhri O, Lorenz HP, Grant GA, Edwards MS (2015) Evolution of cranioplasty techniques in neurosurgery: historical review, pediatric considerations, and current trends. J Neurosurg 123:1098–1107. https://doi.org/10.3171/2014.11.JNS14622
Fiaschi P, Pavanello M, Imperato A, Dallolio V, Accogli A, Capra V, Consales A, Cama A, Piatelli G (2016) Surgical results of cranioplasty with a polymethylmethacrylate customized cranial implant in pediatric patients: a single-center experience. J Neurosurg Pediatr 17:705–710. https://doi.org/10.3171/2015.10.PEDS15489
Frassanito P, Massimi L, Caldarelli M, Tamburrini G, Di Rocco C (2012) Complications of delayed cranial repair after decompressive craniectomy in children less than 1 year old. Acta Neurochir 154:927–933. https://doi.org/10.1007/s00701-011-1253-5
Frassanito P, Massimi L, Caldarelli M, Tamburrini G, Di Rocco C (2014) Bone flap resorption in infants. J Neurosurg Pediatr 13:243–244. https://doi.org/10.3171/2013.6.PEDS13312
Frassanito P, Massimi L, Tamburrini G, Bianchi F, Nataloni A, Canella V, Caldarelli M (2018) Custom-made hydroxyapatite for cranial repair in a specific pediatric age group (7-13 years old): a multicenter post-marketing surveillance study. Childs Nerv Syst 34:2283–2289. https://doi.org/10.1007/s00381-018-3905-8
Frassanito P, Tamburrini G, Massimi L, Di Rocco C, Nataloni A, Fabbri G, Caldarelli M (2015) Post-marketing surveillance of CustomBone Service implanted in children under 7 years old. Acta Neurochir 157:115–121. https://doi.org/10.1007/s00701-014-2254-y
Frassanito P, Tamburrini G, Massimi L, Peraio S, Caldarelli M, Di Rocco C (2017) Problems of reconstructive cranioplasty after traumatic brain injury in children. Childs Nerv Syst 33:1759–1768. https://doi.org/10.1007/s00381-017-3541-8
Fu KJ, Barr RM, Kerr ML, Shah MN, Fletcher SA, Sandberg DI, Teichgraeber JF, Greives MR (2016) An outcome comparison between autologous and alloplastic cranioplasty in the pediatric population. J Craniofac Surg 27:593–597. https://doi.org/10.1097/SCS.0000000000002491
Gilardino MS, Cabiling DS, Bartlett SP (2009) Long-term follow-up experience with carbonated calcium phosphate cement (Norian) for cranioplasty in children and adults. Plast Reconstr Surg 123:983–994. https://doi.org/10.1097/PRS.0b013e318199f6ad
Gilardino MS, Karunanayake M, Al-Humsi T, Izadpanah A, Al-Ajmi H, Marcoux J, Atkinson J, Farmer JP (2015) A comparison and cost analysis of cranioplasty techniques: autologous bone versus custom computer-generated implants. J Craniofac Surg 26:113–117. https://doi.org/10.1097/SCS.0000000000001305
Goldstein JA, Paliga JT, Bartlett SP (2013) Cranioplasty: indications and advances. Curr Opin Otolaryngol Head Neck Surg 21:400–409. https://doi.org/10.1097/MOO.0b013e328363003e
Goodrich JT, Sandler AL, Tepper O (2012) A review of reconstructive materials for use in craniofacial surgery bone fixation materials, bone substitutes and distractors. Childs Nerv Syst 28:1577–1588. https://doi.org/10.1007/s00381-012-1776-y
Grant GA, Jolley M, Ellenbogen RG, Roberts TS, Gruss JR, Loeser JD (2004) Failure of autologous bone-assisted cranioplasty following decompressive craniectomy in children and adolescents. J Neurosurg 100:163–168. https://doi.org/10.3171/ped.2004.100.2.0163
Greene AK, Mulliken JB, Proctor MR, Rogers GF (2008) Pediatric cranioplasty using particulate calvarial bone graft. Plast Reconstr Surg 122:563–571. https://doi.org/10.1097/PRS.0b013e31817d61c1
Josan VA, Sgouros S, Walsh AR, Dover MS, Nishikawa H, Hockley AD (2005) Cranioplasty in children. Childs Nerv Syst 21:200–204. https://doi.org/10.1007/s00381-004-1068-2
Lam S, Kuether J, Fong A, Reid R (2015) Cranioplasty for large-sized calvarial defects in the pediatric population: a review. Craniomaxillofac Trauma Reconstr 8:159–170. https://doi.org/10.1055/s-0034-1395880
Laurie SW, Kaban LB, Mulliken JB (1984) Donor-site morbidity after harvesting rib and iliac bone. Plast Reconstr Surg 73:933–938
Lin AY, Kinsella CR Jr, Rottgers SA, Smith DM, Grunwaldt LJ, Cooper GM, Losee JE (2012) Custom porous polyethylene implants for large-scale pediatric skull reconstruction: early outcomes. J Craniofac Surg 23:67–70. https://doi.org/10.1097/SCS.0b013e318240c876
Ma IT, Symon MR, Bristol RE, Beals SP, Joganic EF, Adelson PD, Shafron DH, Singh DJ (2018) Outcomes of titanium mesh cranioplasty in pediatric patients. J Craniofac Surg 29:99–104. https://doi.org/10.1097/SCS.0000000000004045
Martin KD, Franz B, Kirsch M, Polanski W, Von der Hagen M, Schackert G, Sobottka SB (2014) Autologous bone flap cranioplasty following decompressive craniectomy is combined with a high complication rate in pediatric traumatic brain injury patients. Acta Neurochir 156:813–824. https://doi.org/10.1007/s00701-014-2021-0
Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group (2009) Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med 151:264–269
Moreira-Gonzalez A, Jackson IT, Miyawaki T, Barakat K, DiNick V (2003) Clinical outcome in cranioplasty: critital review in long-term follow-up. J Craniofac Surg 14:144–153
Morice A, Kolb F, Picard A, Kadlub N, Puget S (2017) Reconstruction of a large calvarial traumatic defect using a custom-made porous hydroxyapatite implant covered by a free latissimus dorsi muscle flap in an 11-year-old patient. J Neurosurg Pediatr 19:51–55. https://doi.org/10.3171/2016.8.PEDS1653
Ozerdem OR, Sen O, Anlatici R, Erdoğan B, Aydin V (2002) Osteogaleal flaps in pediatric cranioplasty. Ann Plast Surg 49:127–132
Pang D, Tse HH, Zwienenberg-Lee M, Smith M, Zovickian J (2005) The combined use of hydroxyapatite and bioresorbable plates to repair cranial defects in children. J Neurosurg 102:36–43. https://doi.org/10.3171/ped.2005.102.1.0036
Piedra MP, Thompson EM, Selden NR, Ragel BT, Guillaume DJ (2012) Optimal timing of autologous cranioplasty after decompressive craniectomy in children. J Neurosurg Pediatr 10:268–272. https://doi.org/10.3171/2012.6.PEDS1268
Piittulainen JM, Posti JP, Aitasalo KM, Vuorinen V, Vallittu PK, Serlo W (2015) Paediatric cranial defect reconstruction using bioactive fibre-reinforced composite implant: early outcomes. Acta Neurochir 157:681–687. https://doi.org/10.1007/s00701-015-2363-2
Plum AW, Tatum SA (2015) A comparison between autograft alone, bone cement, and demineralized bone matrix in cranioplasty. Laryngoscope 125:1322–1327. https://doi.org/10.1002/lary.25158
Posnick JC, Goldstein JA, Armstrong D, Rutka JT (1993) Reconstruction of skull defects in children and adolescents by the use of fixed cranial bone grafts: long-term results. Neurosurgery 32:785-791
Rocque BG, Agee BS, Thompson EM, Piedra M, Baird LC, Selden NR, Greene S, Deibert CP, Hankinson TC, Lew SM, Iskandar BJ, Bragg TM, Frim D, Grant G, Gupta N, Auguste KI, Nikas DC, Vassilyadi M, Muh CR, Wetjen NM, Lam SK (2018) Complications following pediatric cranioplasty after decompressive craniectomy: a multicenter retrospective study. J Neurosurg Pediatr 8:1–8. https://doi.org/10.3171/2018.3.PEDS17234
Rocque BG, Amancherla K, Lew SM, Lam S (2013) Outcomes of cranioplasty following decompressive craniectomy in the pediatric population. J Neurosurg Pediatr 12:120–125. https://doi.org/10.3171/2013.4.PEDS12605
Sanan A, Haines SJ (1997) Repairing holes in the head: a history of cranioplasty. Neurosurgery 40:588–603
Schuss P, Vatter H, Marquardt G, Imöhl L, Ulrich CT, Seifert V, Güresir E (2012) Cranioplasty after decompressive craniectomy: the effect of timing on postoperative complications. J Neurotrauma 29:1090–1095. https://doi.org/10.1089/neu.2011.2176
Taggard DA, Menezes AH (2001) Successful use of rib grafts for cranioplasty in children. Pediatr Neurosurg 34:149–155. https://doi.org/10.1159/000056010
Vignes JR, Jeelani NU, Dautheribes M, San-Galli F, Liguoro D (2007) Cranioplasty for repair of a large bone defect in a growing skull fracture in children. J Craniomaxillofac Surg 35:185–188. https://doi.org/10.1016/j.jcms.2007.04.002
Waqas M, Ujjan B, Hadi YB, Najmuddin F, Laghari AA, Khalid S, Bari ME, Bhatti UF (2017) Cranioplasty after craniectomy in a pediatric population: single-center experience from a developing country. Pediatr Neurosurg 52:77–79. https://doi.org/10.1159/000452808
Williams L, Fan K, Bentley R (2016) Titanium cranioplasty in children and adolescents. J Craniomaxillofac Surg 44:789–794. https://doi.org/10.1016/j.jcms.2016.03.010
Zaccaria L, Tharakan SJ, Altermatt S (2017) Hydroxyapatite ceramic implants for cranioplasty in children: a single-center experience. Childs Nerv Syst 33:343–348. https://doi.org/10.1007/s00381-016-3327-4
Acknowledgements
KJM is supported by the Van Wagenen Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
With the submission of this manuscript, I would like to state that the authors report no conflict of interest concerning the materials and methods used or the findings specified in this paper. Furthermore, the authors declare that this study was performed in accordance with the research ethical guidelines.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Klieverik, V.M., Miller, K.J., Singhal, A. et al. Cranioplasty after craniectomy in pediatric patients—a systematic review. Childs Nerv Syst 35, 1481–1490 (2019). https://doi.org/10.1007/s00381-018-4025-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-018-4025-1