Abstract
Purpose
The purpose of this study is to investigate the incidence of cavernous angioma (CVA) in long-term survivors of childhood embryonal tumors treated by cranial irradiation.
Materials and methods
Between 1990 and 2012, we treated 25 patients (13 males, 12 females) with embryonal tumors (17 medulloblastomas, 5 primitive neuroectodermal tumors (PNET), 3 pineoblastomas) with craniospinal irradiation. Follow-up ranged from 15.5 to 289.9 months, the irradiation dose to the whole neural axis from 18 to 36 Gy, and the total local dose from 49.6 to 60 Gy. All patients underwent follow-up magnetic resonance imaging (MRI) studies at least once a year, and the diagnosis of posttreatment CVA was based solely on MRI findings.
Results
At the time of this writing, 18 were alive and free of the recurrence of the original disease or the development of secondary neoplasms other than CVA; another 2 were alive with medulloblastoma or diffuse astrocytoma. Posttreatment, 14 patients developed CVAs in the course of a median of 56.7 months; 13 of these presented with multiple CVAs. Patients who underwent radiation therapy (RT) at an age younger than 6 years developed multiple CVAs significantly earlier than those treated at a later age (p = 0.0110). Patients with PNET or pineoblastoma developed Zabramski type 1 and 2 CVA significantly earlier than did medulloblastoma patients (p = 0.0042).
Conclusion
We attribute the high rate of post-RT CVA in our long-term follow-up study of pediatric patients to the delivery of cranial irradiation for embryonal tumors, especially PNET and pineoblastoma, and recommend the regular, long-term follow-up of patients whose embryonal tumors were treated by cranial irradiation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Children with central nervous system neoplasms treated by cranial or craniospinal irradiation or radiation combined with chemotherapy may several years later present with intracranial hemorrhage at sites other than that of the primary tumor [1, 2]. Based on histological studies, such intracerebral hemorrhages were attributed to the postirradiation development of cavernous angioma (CVA) [3–10]. Despite the growing number of reports on this phenomenon [8–15], much remains unknown including the relationship between cavernoma formation and the radiation dose, the site and volume of the lesion, the contribution of chemotherapy, the cumulative incidence, and the incidence of symptomatic and asymptomatic hemorrhagic events.
The aim of this study was to evaluate the cumulative incidence of CVA in patients with childhood embryonal tumors including medulloblastoma, pineoblastoma, and primitive neuroectodermal tumor (PNET) treated by craniospinal radiation therapy (RT) at a single institution. They were followed long-term (from 15.5 to 289.9 months) and underwent at least annual post-RT MRI studies. We compared follow-up observations made on patients with pediatric medulloblastoma and those with pineoblastoma or PNET. As embryonal tumors tend to arise at a young age and have relatively high survival rates, the possible long-term sequelae of whole-brain irradiation in childhood must be understood and minimized.
Materials and methods
Patients
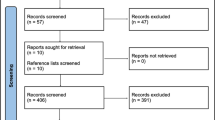
This retrospective study was approved by our institutional review board; written patient consent was waived. To protect patient privacy, we removed all identifiers from our records upon completion of our analyses. Between 1990 and 2012, we treated 31 patients (16 males, 15 females) with childhood embryonal tumors (22 medulloblastomas, 6 PNET, 3 pineoblastomas); 25 who underwent cranial irradiation were included in this study (17 medulloblastomas, 5 PNET, 3 pineoblastomas). Three patients each were subsequently excluded because they were younger than 3 years and underwent chemotherapy only or because the follow-up period was less than 1 year. Preoperative MR studies denied the presence of CVA before treatment in all included patients. The irradiation dose to the whole neural axis ranged from 18 to 36 Gy and the total local dose from 49.6 to 60 Gy. No patients had a history of previous surgery, chemotherapy, or RT.
Of the 25 patients, 13 were censored during their follow-up due to recurrence of the original disease (n = 5), the detection of secondary leukemia (n = 1) or of secondary diffuse astrocytoma (n = 1), or the absence of CVA on the last follow-up MRI study (n = 6). Of the 25 patients, 14 developed CVA during follow-up; 2 of these were subsequently censored due to the development of secondary diffuse astrocytoma or secondary leukemia.
MRI studies
All patients underwent MRI including T2-weighted imaging (WI) (TR 4800 ms, TE 100 ms, echo train length 18, field-of-view (FOV) 22 × 22 cm, matrix size 512 × 320/2 NEX, section thickness 6 mm, intersection gap 1.0 mm, 1 acquisition) or FLAIR imaging (TR 10,000 ms, TE 140.0 ms, inversion recovery time 2400.0 ms, FOV 22 × 22 cm, matrix size 288 × 160/1 NEX, section thickness 6 mm, intersection gap 1.0 mm, 2 acquisitions), and pre- and post-gadolinium-enhanced T1-WI (TR 450 ms, TE 18 ms, FOV 22 × 22 cm, matrix size 256 × 192/1 NEX, section thickness 6 mm, intersection gap 1.0 mm, 2 acquisitions). The parameters for T2*-WI were gradient echo, TR 600 ms, TE 12 ms, flip angle 20°, FOV 22 × 22 cm, matrix size 320 × 192/1 NEX, slice thickness 6 mm, intersection gap 1.0 mm, scan time 1:30.
CVA evaluation
The diagnosis of CVA was based solely on post-RT MRI findings. The CVAs were classified by the consensus of three authors (F.Y., T.T., R.N.) into four types based on the classification of Zabramski et al. [16]. None of the patients underwent surgery for CVA, and none of the lesions were confirmed histologically.
Statistical analysis
Statistical analyses were with PRISM version 5.0 (GraphPad Software Inc, La Jolla, CA, USA). The interval between the delivery of craniospinal irradiation and the subsequent detection of CVA was the time between the first RT session and the post-RT diagnosis of CVA. To evaluate the diagnostic value, we performed Kaplan-Meier analysis (log-rank test) that incorporated the diagnosis of CVA based on MRI findings. The time to the development of the first post-RT CVA, to the progression to multiple CVAs, and to the classification of Zabramski type 1 or 2 CVA was compared between patients who received RT at an age >6 and ≤6 years and between patients with medulloblastoma or with PNET or pineoblastoma.
Results
The characteristics of the 25 original patients with embryonal tumors are summarized in Table 1. At the time of this writing, 18 were alive and free of the recurrence of the original disease or the development of secondary neoplasms other than CVA; the median follow-up term was 89.7 months (range 15.5–289.9 months, mean 108.6 months). Of the 25 patients, 14 (56 %) developed CVAs 26.0–227.3 months (median 56.7 months, mean 81.9 months) post-RT (Fig. 1); in 13, the CVAs were multiple. The cumulative incidence was 14.3, 38.9, 68.8, and 93.3 %, at 3-, 5-, 10-, and 20-year post-RT, respectively. The time to the development of multiple CVAs in 13 patients ranged from 34.3 to 269.4 months (median 62.8 months, mean 93.5 months). The interval between the detection of single and multiple CVAs ranged from 0 (cases 6 and 25) to 42.5 months (case 12) (median 10.3 months, mean 15.7 months). We were unable to detect a trend with respect to the development site of the secondary CVAs.
Next, we analyzed the effect of the patient age at the time of RT on the development of post-RT CVAs. Compared to children who underwent RT when they were at least 6 years old, those treated at an age younger than 6 years developed CVAs significantly earlier (median 41.6 vs 86.1 months, p = 0.0496, log-rank test), and they developed multiple CVAs significantly earlier than the older children (Fig. 2, median 44.0 vs 141.0 months, p = 0.0110, log-rank test).
Then, we divided our patients into two groups, a medulloblastoma group who underwent whole neural axis irradiation with a boost delivered mainly at the posterior fossa (group 1, n = 17) and a second group with PNET or pineoblastoma who also received whole neural axis irradiation with a boost delivered mainly at the cerebral hemisphere (group 2, n = 10). Patients with PNET or pineoblastoma developed CVA significantly earlier than did patients with childhood medulloblastoma (Fig. 3, p = 0.0481, log-rank test).
Finally, we focused on CVAs classified as Zabramski type 1 and 2 because these lesions present with hemorrhage and are clinically relevant. In our series, 6 (24 %) of 25 patients developed Zabramski type 1 or 2 CVAs 26.0–274.9 months (median 86.4 months, mean 109.7 months) post-RT. The lesions were symptomatic (headache/diplopia/abducens palsy) in 3 patients cases 15, 18, 24. We found that patients with PNET or pineoblastoma developed Zabramski type 1 and 2 CVAs significantly earlier than did patients with medulloblastoma (Fig. 4, p = 0.0042, log-rank test). A representative case (case 18) is shown in Fig. 5. The 3 patients with symptomatic Zabramski type 1 or 2 CVAs were treated conservatively and their symptoms improved. None required surgery, suffered rebleeding, or subsequently developed multiple lesion defined as Zabramski type 1 or 2.
A patient with a primitive neuroectodermal tumor who underwent radiochemotherapy at the age of 4 years, case 18. Five years and 8 months later, he presented with headache. Axial T1-weighted (a), T2-weighted (b), and T2*-weighted (c) images showed heterogeneous hemorrhage with a hemosiderin rim in the left frontal lobe (arrow). Sixteen months later, the lesion was demonstrably smaller (d) (arrow). Other Zabramski type 4 lesions were observed in the left frontal lobe 51-month postirradiation (e, arrowhead) and in the right frontal lobe 77-month postirradiation (f, arrowhead)
Discussion
Wilson first suggested that CVAs could arise after cranial irradiation [17]. Circillo et al. [3] subsequently reported 7 patients with CVA as a possible sequela of cranial irradiation. According to others [4–7, 18–21], the incidence of cavernoma after cranial irradiation ranged from 3.4 to 41.2 %. Of our 25 patients with embryonal tumors treated with RT, 14 (56 %) subsequently developed CVA. We also found that secondary CVA after cranial irradiation developed significantly earlier in patients with PNET or pineoblastoma than in those with medulloblastoma.
Zabramski et al. [16] classified CVAs into four types. On T1- and T2-WI, type1 shows a hyperintense signal, type 2 a reticulated core of mixed signal intensity surrounded by a hemosiderin ring, and type 3 an iso- to hypointense area. Type 4 is poorly visualized except on T2*-WI. Their type 1 and 2 CVAs manifest recent hemorrhage and may become symptomatic. According to Vinchon et al. [22], CVA may not be detected as long as 20 years after RT. On the other hand, Koike et al. [18] reported that CVAs arose 24 years after 6–12 Gy of cranial irradiation and hematopoietic stem cell transplantation and that all of their patients treated with 18–36 Gy manifested CVAs within 16 years. Among long-term survivors of medulloblastoma followed by Lew et al. [20], one presented with CVA 16.1 years after cranial irradiation and chemotherapy. We found that Zabramski type 1 or 2 CVA may arise 20 years after the treatment of embryonal tumors with high-dose cranial irradiation and document that the cumulative incidence of secondary postirradiation CVA increased year by year. Others [22, 23] warned that cranial irradiation may elicit secondary neoplasms; 10 years post-RT, gliomas, meningiomas, and sarcomas were found in 4 % of survivors. In fact, one of our patients (case 12) presented with secondary diffuse astrocytoma at the center of the irradiation field 10 years post-RT. Other complications include a volume loss of the brain, leukoencephalopathy, neurological and neuropsychological dysfunction, endocrine complications, social impairment, spinal deformities, and alopecia [24, 25]. The dose and/or field of irradiation in patients with embryonal tumors tends to be larger than that in patients with leukemia, germinoma, lymphoma, and glioma, and our findings suggest that patients with embyronal tumors subjected to cranial irradiation must be followed long-term to look for secondary changes.
The mechanism(s) underlying the development of post-RT CVA remains unclear. Heckl et al. [9] posited that the molecular mechanisms involved in their elicitation depend on vascular endothelial growth factor (VEGF) and hypoxy-inducible factor-1 (HIF-1). Irradiation results in narrowing of the vascular vessel lumen due to endothelial proliferation with hyalinization and fibrinoid necrosis of the vascular wall [2]. This leads to ischemia and microinfarction followed by reactive angiogenesis due to the induction of HIF-1, which in turn induces VEGF [26]. The expression of these factors is high in the very young and may explain the earlier development of CVA in patients subjected to irradiation at a young age [18–22, 25, 27]. Other mechanisms may involve direct injury to the parenchyma or an immunologic mechanism with an allergic hypersensitivity response [28]. The development of hemorrhages may reflect disruptions and changes in capillary vascular integrity elicited by RT as it can induce Moyamoya-like disease and capillary telangiectasia [29–31]. Maeder et al. [14] suggested venous restrictive disease as a sequela of radiation changes resulting in impaired venous flow and that the consequent increase in venous pressure results in the formation of cavernomas. As in some patient subgroups, the incidence of secondary post-RT CVA is higher and the time to their manifestation is shorter than in other patients, genetic or epigenetic heterogeneity may be involved. In fact, mutations in cerebral cavernous malformation 1 (CCM1)/Krev interaction trapped protein 1 (KRIT1)-, CCM2/MGC4607-, and CCM3/programmed cell death 10 (PDCD10) genes as well as CCM3 were associated with familial CVA [32, 33]. He et al. [34] reported that stabilization of VEGF receptor 2 signaling by CCM3 is critical for vascular development, and Jung et al. [35] pointed to the relationship between VEGF and CVA.
Sporadically occurring CVA developed symptomatic hemorrhage at the annual rate of 1.6–3.1 % [36]. It is unclear whether post-RT CVAs have a similar propensity to bleed. As they tend to be multiple, the incidence of hemorrhagic events can be expected to be higher than in sporadic CVA but not higher than in familial CVA. Brunereau et al. [37] reported that the clinical manifestations in patients with familial and sporadic CVA appear to be similar. Affected patients may be entirely asymptomatic, and some CVAs remain stable in size, grow, or shrink [20]. In patients with sporadic asymptomatic post-RT secondary CVA detected incidentally, the recommended standard practice is conservative observation even though their detection on conventional MRI scans may presage later complications [25].
Our study has some limitations. The number of long-term survivors of embryonal brain tumors was small, and we did not evaluate any of the CVAs histologically. Some Zabramski type 4 CVAs may have included areas of calcification or microbleeds due to etiologies such as senescence. We evaluated the CVA type without regard to the lesion size. The CVA size on T2*-WI scans is not accurate because on such images, the signal from hemorrhage is larger. The clinical implications of detecting Zabramski type 4 CVAs on T2*-WI scans remain to be determined. Nonetheless, we suggest that T2*-WI studies be included in the follow-up of patients whose embryonal tumors were addressed by cranial irradiation.
Conclusion
We attribute the higher incidence of post-RT CVA in our than earlier studies to our very long-term follow-up (range 15.5 to 289.9 months) of patients who had undergone RT to address embryonal tumors. The incidence of Zabramski type 1 or 2 CVA was high in our series, especially in patients with PNET and pineoblastoma. Based on our findings, we recommend that survivors of childhood embryonal tumors be followed long-term and regularly because secondary changes may be detected long after the delivery of RT.
References
Allen JC, Miller DC, Budzilovich GN, Epstein FJ (1991) Brain and spinal cord hemorrhage in long-term survivors of malignant pediatric brain tumors: a possible late effect of therapy. Neurology 41:148–150
Poussaint TY, Siffert J, Barnes PD, Pomeroy SL, Goumnerova LC, Anthony DC, Sallan SE, Tarbell NJ (1995) Hemorrhagic vasculopathy after treatment of central nervous system neoplasia in childhood: diagnosis and follow-up. AJNR Am J Neuroradiol 16:693–699
Ciricillo SF, Cogen PH, Edwards MS (1994) Pediatric cryptic vascular malformations: presentation, diagnosis and treatment. Pediatr Neurosurg 20:137–147
Baumgartner JE, Ater JL, Ha CS, Kuttesch JF, Leeds NE, Fuller GN, Wilson RJ (2003) Pathologically proven cavernous angiomas of the brain following radiation therapy for pediatric brain tumors. Pediatr Neurosurg 39:201–207
Chang SD, Vanefsky MA, Havton LA, Silverberg GD (1998) Bilateral cavernous malformations resulting from cranial irradiation of a choroid plexus papilloma. Neurol Res 20:529–532
Humpl T, Bruhl K, Bohl J, Schwarz M, Stoeter P, Gutjahr P (1997) Cerebral haemorrhage in long-term survivors of childhood acute lymphoblastic leukaemia. Eur J Pediatr 156:367–370
Maraire JN, Abdulrauf SI, Berger S, Knisely J, Awad IA (1999) De novo development of a cavernous malformation of the spinal cord following spinal axis radiation. Case report. J Neurosurg 90:234–238
Amirjamshidi A, Abbassioun K (2000) Radiation-induced tumors of the central nervous system occurring in childhood and adolescence. Four unusual lesions in three patients and a review of the literature. Childs Nerv Syst 16:390–397
Heckl S, Aschoff A, Kunze S (2002) Radiation-induced cavernous hemangiomas of the brain: a late effect predominantly in children. Cancer 94:3285–3291
Larson JJ, Ball WS, Bove KE, Crone KR, Tew JM Jr (1998) Formation of intracerebral cavernous malformations after radiation treatment for central nervous system neoplasia in children. J Neurosurg 88:51–56
Alexander MJ, DeSalles AA, Tomiyasu U (1998) Multiple radiation-induced intracranial lesions after treatment for pituitary adenoma. Case report. J Neurosurg 88:111–115
Bejjani GK, Caputy AJ, Kurtzke RN, Duong DH, Sekhar LN (1997) Remote hemorrhage of a pontine cavernous angioma fifty-two years after cerebral irradiation. Acta Neurochir (Wien) 139:583–584
Laitt RD, Chambers EJ, Goddard PR, Wakeley CJ, Duncan AW, Foreman NK (1995) Magnetic resonance imaging and magnetic resonance angiography in long term survivors of acute lymphoblastic leukemia treated with cranial irradiation. Cancer 76:1846–1852
Maeder P, Gudinchet F, Meuli R, de Tribolet N (1998) Development of a cavernous malformation of the brain. AJNR Am J Neuroradiol 19:1141–1143
Novelli PM, Reigel DH, Langham Gleason P, Yunis E (1997) Multiple cavernous angiomas after high-dose whole-brain radiation therapy. Pediatr Neurosurg 26:322–325
Zabramski JM, Wascher TM, Spetzler RF, Johnson B, Golfinos J, Drayer BP, Brown B, Rigamonti D, Brown G (1994) The natural history of familial cavernous malformations: results of an ongoing study. J Neurosurg 80:422–432
Wilson CB (1992) Cryptic vascular malformations. Clin Neurosurg 38:49–84
Koike S, Aida N, Hata M, Fujita K, Ozawa Y, Inoue T (2004) Asymptomatic radiation-induced telangiectasia in children after cranial irradiation: frequency, latency, and dose relation. Radiology 230:93–99
Burn S, Gunny R, Phipps K, Gaze M, Hayward R (2007) Incidence of cavernoma development in children after radiotherapy for brain tumors. J Neurosurg 106:379–383
Lew SM, Morgan JN, Psaty E, Lefton DR, Allen JC, Abbott R (2006) Cumulative incidence of radiation-induced cavernomas in long-term survivors of medulloblastoma. J Neurosurg 104:103–107
Strenger V, Sovinz P, Lackner H, Dornbusch HJ, Lingitz H, Eder HG, Moser A, Urban C (2008) Intracerebral cavernous hemangioma after cranial irradiation in childhood. Incidence and risk factors. Strahlenther Onkol 184:276–280
Vinchon M, Leblond P, Caron S, Delestret I, Baroncini M, Coche B (2011) Radiation-induced tumors in children irradiated for brain tumor: a longitudinal study. Childs Nerv Syst 27:445–453
von Hoff K, Hinkes B, Gerber NU, Deinlein F, Mittler U, Urban C, Benesch M, Warmuth-Metz M, Soerensen N, Zwiener I, Goette H, Schlegel PG, Pietsch T, Kortmann RD, Kuehl J, Rutkowski S (2009) Long-term outcome and clinical prognostic factors in children with medulloblastoma treated in the prospective randomised multicentre trial HIT'91. Eur J Cancer 45:1209–1217
Frange P, Alapetite C, Gaboriaud G, Bours D, Zucker JM, Zerah M, Brisse H, Chevignard M, Mosseri V, Bouffet E, Doz F (2009) From childhood to adulthood: long-term outcome of medulloblastoma patients. The Institut Curie experience (1980-2000). J Neuro-Oncol 95:271–279
Peters S, Pahl R, Claviez A, Jansen O (2013) Detection of irreversible changes in susceptibility-weighted images after whole-brain irradiation of children. Neuroradiology 55:853–859
Rivard A, Berthou-Soulie L, Principe N, Kearney M, Curry C, Branellec D, Semenza GL, Isner JM (2000) Age-dependent defect in vascular endothelial growth factor expression is associated with reduced hypoxia-inducible factor 1 activity. J Biol Chem 275:29643–29647
Tsao MN, Li YQ, Lu G, Xu Y, Wong CS (1999) Upregulation of vascular endothelial growth factor is associated with radiation-induced blood-spinal cord barrier breakdown. J Neuropathol Exp Neurol 58:1051–1060
Ball WS Jr, Prenger EC, Ballard ET (1992) Neurotoxicity of radio/chemotherapy in children: pathologic and MR correlation. AJNR Am J Neuroradiol 13:761–776
Bitzer M, Topka H (1995) Progressive cerebral occlusive disease after radiation therapy. Stroke 26:131–136
Valk PE, Dillon WP (1991) Radiation injury of the brain. AJNR Am J Neuroradiol 12:45–62
Gaensler EH, Dillon WP, Edwards MS, Larson DA, Rosenau W, Wilson CB (1994) Radiation-induced telangiectasia in the brain simulates cryptic vascular malformations at MR imaging. Radiology 193:629–636
Denier C, Goutagny S, Labauge P, Krivosic V, Arnoult M, Cousin A, Benabid AL, Comoy J, Frerebeau P, Gilbert B, Houtteville JP, Jan M, Lapierre F, Loiseau H, Menei P, Mercier P, Moreau JJ, Nivelon-Chevallier A, Parker F, Redondo AM, Scarabin JM, Tremoulet M, Zerah M, Maciazek J, Tournier-Lasserve E (2004) Mutations within the MGC4607 gene cause cerebral cavernous malformations. Am J Hum Genet 74:326–337
Bergametti F, Denier C, Labauge P, Arnoult M, Boetto S, Clanet M, Coubes P, Echenne B, Ibrahim R, Irthum B, Jacquet G, Lonjon M, Moreau JJ, Neau JP, Parker F, Tremoulet M, Tournier-Lasserve E (2005) Mutations within the programmed cell death 10 gene cause cerebral cavernous malformations. Am J Hum Genet 76:42–51
He Y, Zhang H, Yu L, Gunel M, Boggon TJ, Chen H, Min W (2010) Stabilization of VEGFR2 signaling by cerebral cavernous malformation 3 is critical for vascular development. Sci Signal 3:ra26
Jung KH, Chu K, Jeong SW, Park HK, Bae HJ, Yoon BW (2003) Cerebral cavernous malformations with dynamic and progressive course: correlation study with vascular endothelial growth factor. Arch Neurol 60:1613–1618
Moriarity JL, Wetzel M, Clatterbuck RE, Javedan S, Sheppard JM, Hoenig-Rigamonti K, Crone NE, Breiter SN, Lee RR, Rigamonti D (1999) The natural history of cavernous malformations: a prospective study of 68 patients. Neurosurgery 44:1166–1171, discussion 1172-1163
Brunereau L, Labauge P, Tournier-Lasserve E, Laberge S, Levy C, Houtteville JP (2000) Familial form of intracranial cavernous angioma: MR imaging findings in 51 families. French Society of Neurosurgery. Radiology 214:209–216
Acknowledgments
We thank Ursula Petralia for editorial review. This study was supported by a research grant from the Japanese Society of Neuroradiology and a grant-in-aid from the Japan Society for the Promotion of Science Grant-in-Aid for Scientific Research (C) number 25462262.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yamasaki, F., Takayasu, T., Nosaka, R. et al. The postirradiation incidence of cavernous angioma is higher in patients with childhood pineoblastoma or primitive neuroectodermal tumors than medulloblastoma. Childs Nerv Syst 31, 901–907 (2015). https://doi.org/10.1007/s00381-015-2626-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00381-015-2626-5