Abstract
Background
In this study, our aim was to investigate the role of cardiac biomarkers in predicting the presence of significant coronary artery disease in hypertrophic cardiomyopathy (HCM) patients.
Methods
The study population was composed of hypertrophic cardiomyopathy patients who underwent coronary angiography at a single center between June 2021 and March 2023, and whose cardiac biomarkers were evaluated before the procedure. HCM patients were screened retrospectively. Significant CAD was defined as > 50% stenosis of the left main coronary artery or > 70% stenosis in a major coronary vessel. Demographic, echocardiographic and cardiac biomarker values were compared between the two groups.
Results
A total of 123 patients were evaluated. Significant CAD was detected in 39 (31.7%) patients. Patients with significant CAD had higher CK-MB values than those without CAD [2.8 (2.1–4.0) vs. 3.4 (2.8–4.6), p = 0.036], and a higher level of high-sensitivity troponin T (hs-TnT) than those without CAD (24 vs. 17.8, p = 0.022). the NT-proBNP/hs-TnT ratio was found to be significantly lower in patients with CAD than in those with CAD (31.4 vs. 21.4, p = 0.019). In multivariate anaylsis, NT-proBNP/hs-TnT was determined as an independent predictor for significant CAD. In ROC analysis, NT-proBNP/hs-TnT ratio lower than the cut-off value of 30.7 could detect the presence of significant CAD with 76.9% sensitivity and 53.6% specificity (AUC: 0.632, 95% CI: 0.528–0.736, p = 0.019).
Conclusion
To sum up, we suggest that cardiac biomarkers were valuable and simple parameters in terms of significant CAD in HCM patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Hypertrophic cardiomyopathy (HCM) is a genetic heart condition that affects the structure of the heart muscle. It is a relatively common condition, with a prevalence of approximately 1 in 500 individuals. While many HCM patients remain asymptomatic, others may experience symptoms such as chest pain, shortness of breath, palpitations, or dizziness. In some cases, HCM can also increase the risk of developing coronary artery disease (CAD) [1]. The causes of chest pain in HCM patients include myocardial ischemia, increased metabolic demand, and decreased myocardial blood supply [2]. The presence of CAD in HCM patients can lead to severe complications, including heart attack, arrhythmias, or sudden cardiac death [1, 3]. Therefore, identifying and managing CAD in HCM patients is essential to reduce the risk of adverse outcomes. Previous studies have reported that CAD is present in 10–53% of HCM patients [4,5,6].
Cardiac biomarkers are a group of proteins that are released into the bloodstream following heart muscle damage or stress. They are widely used in the diagnosis and management of acute coronary syndrome, a condition characterized by the sudden onset of chest pain or other symptoms due to decreased blood flow to the heart [7]. However, the utility of cardiac biomarkers is not limited to the acute setting. In fact, they can also provide valuable information in the context of chronic heart diseases, such as heart failure or hypertrophic cardiomyopathy [8, 9]. In these conditions, cardiac biomarkers can help assess the severity of the disease, monitor disease progression, and guide treatment decisions. There are publications showing that cardiac biomarkers can be used to differentiate acute coronary syndrome and stress cardiomyopathy [10, 11]. However, data on the use of biomarkers in stable coronary artery patients are limited.
In this study, our aim was to investigate the role of cardiac biomarkers in predicting the presence of significant coronary artery disease in HCM patients.
Materials and methods
Study population
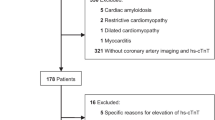
The study population was composed of hypertrophic cardiomyopathy patients who underwent coronary angiography at a single center between June 2021 and March 2023, and whose cardiac biomarkers were evaluated before the procedure. Patients with acute coronary syndrome, storage/infiltrative diseases causing hypertrophy, hypertensive CM, advanced left ventricular dysfunction (EF < 40%), end-stage kidney disease (GFR < 30 ml/min) and a history of coronary revascularization were excluded from the study. The flowchart regarding the inclusion and exclusion criteria of the study is shown in Fig. 1.
The diagnosis of HCM was based on maximal left ventricular wall thickness, assessed by two-dimensional transthoracic echocardiography and/or cardiac magnetic resonance imaging (CMR) by standard technique. A maximal left ventricular wall thickness ≥ 15 mm in one or more myocardial segments, or ≥ 13 mm with a family history of HCM in the absence of other conditions associated with ventricular hypertrophy, was considered diagnostic for HCM according to current guidelines. All HCM patients in the center were evaluated in a single cardiomyopathy outpatient clinic, and the cardiac biomarkers of all patients scheduled for angiography were included in the evaluation. Patients whose cardiac biomarkers were not found in the hospital electronic system were also excluded from the study.
The study protocol was approved by the Local Ethics Committee was conducted in accordance with the principles outlined in the Declaration of Helsinki.
Coronary artery disease assessment
Patients were referred for coronary angiography based on the presence of ischemic symptoms or evidence of ischemia according to the non-invasive tests. We utilized three non-invasive tests to assess evidence of myocardial ischemia: exercise stress test (EST), myocardial perfusion scintigraphy (MPS), and echocardiography. During the EST, a positive result was defined as a 1.0 mm horizontal or down-sloping ST depression in 2 or more contiguous leads or if the patient experienced symptoms during the test. In MPS, the presence of significant myocardial ischemia (≥ 10%) was considered positive. Evidence of ischemia in echocardiography was evaluated by assessing segmental wall motion abnormalities. Standard coronary angiography procedures were performed via femoral or radial access. In cases where a coronary stent was required, a separate session was scheduled. Significant CAD was defined as > 50% stenosis of the left main coronary artery or > 70% stenosis in a major coronary vessel, as determined by invasive coronary angiography. Patients were divided into two groups based on the presence or absence of significant CAD, with images examined from the Picture Archiving and Communication System (PACS) system. Patients who had undergone coronary computed tomography (CT) were not included in the study, as the focus was on invasive coronary angiography.
Biomarker measurement
In this study, blood samples were collected using 10 mL syringes containing ethylenediaminetetraacetic acid (EDTA) anticoagulant. The collected blood was centrifuged to separate the plasma, which was then analyzed using third-generation electrochemiluminescent immunoassay for cardiac high-sensitive troponin T (hs-cTnT) and the Elecsys automated analyzer for N-terminal pro-B-type natriuretic peptide (NT-proBNP) (Elecsys pro-BNP® and Elecsys Troponin-T® assays from Roche Diagnostics GmbH).
Statistical anaylsis
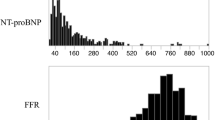
Statistical analysis of the study was performed with the SPSS Version 25.0 program (SPSS Inc., Chicago, Illinois, USA). Whether the variables showed normal distribution was evaluated using visual (histograms, probability curves) and analytical methods (Kolmogorov–Smirnov's or Shapiro–Wilk). Normally distributed numerical variables were expressed as mean ± standard deviation (SD), while non-normally distributed numerical variables were expressed as median (interquartile range), and categorical variables were expressed as percent (%). Receiver operating characteristic (ROC) curve and Youden index [max (sensitivity + selectivity − 1)] were used to determine the hs-troponin-t and NT-proBNP/hs-TnT ratio predictive cut-off values for detecting significant CAD in HCM patients, and the area under the ROC curve over 0.5 was considered significant. Statistical analysis of numerical variables between groups was performed with Student's t unpaired test or Mann Whitney U test, and analysis of categorical variables with Chi-square or Fisher's exact test. In order to determine the independent predictors of significant CAD, univariable logistic regression analysis was performed first, followed by a multivariable logistic regression analysis using parameters that were significant in univariate analysis. A p-value of < 0.05 was considered significant throughout this study).
Results
The study compared clinical and imaging characteristics between two groups of patients with hypertrophic cardiomyopathy (HCM): those with a significant coronary artery disease (CAD+) and those without (CAD−). The demographic characteristics of the two groups were not significantly different, with a similar age range and gender distribution. The prevalence of hypertension, diabetes mellitus, atrial fibrillation, cerebrovascular disease, and chronic kidney disease was not significantly different between the two groups. However, patients in the CAD+ group had significantly higher prevalence of hyperlipidemia (41.0% vs 15.5%, p = 0.002). Also, smoking rates were higher in CAD+ group [26 (30.9) vs. 21 (53.8), p = 0.015].
There were no significant differences in echocardiographic parameters, including left ventricular ejection fraction (LVEF), left atrial diameter, interventricular septum thickness, posterior wall thickness, and tricuspid annular plane systolic excursion (TAPSE). However, patients in the CAD- group had a higher prevalence of systolic anterior motion (SAM) of the mitral valve (54.8% vs 35.9%, p = 0.051), but there was no statistical difference. The prevalence of significant mitral regurgitation was not significantly different between the two groups.
Cardiac magnetic resonance (CMR) imaging revealed no significant differences in LVEF and maximal wall thickness between the two groups. However, the prevalence of late gadolinium enhancement (LGE) was numerically higher in the CAD+ group (96.4% vs 81.9%, p = 0.052), but there was no statistical difference between the two groups. The extent of fibrosis was not significantly different between the two groups. Table 1 summarises the data on the demographic and imaging findings of the patients.
In terms of laboratory variables, patients with significant CAD had higher CK-MB values than those without CAD "[(3.4 (2.8–4.6) vs. 2.8 (2.4–4.0), p = 0.036], and a higher level of high-sensitivity troponin T (hs-TnT) than those without CAD (24 vs. 17.8, p = 0.022). There were no significant differences in haemoglobin, LDL cholesterol, total cholesterol, HDL cholesterol, triglycerides, glomerular filtration rate or N-terminal pro-brain natriuretic peptide (NT-proBNP) levels between the two groups. However, the NT-proBNP/hs-TnT ratio was found to be significantly higher in patients without CAD than in those with CAD (31.4 vs. 21.4, p = 0.019). Table 2 shows the comparison of biochemical variables and cardiac biomarkers between the two groups.
Logistic regression analysis showed significant results for hyperlipidemia, hypertension, diabetes, smoking, CK-MB levels and NT-proBNP/hs-TnT ratio levels in univariate analysis, and multivariate analysis was performed with these variables. As a result of multivariate analysis, hyperlipidemia [(OR = 2.603, 95% CI (1.038–6.529, p = 0.042], smoking [(OR = 0.353, 95% CI (1.024–5.410, p = 0.044], and NT-proBNP/hs-TnT ratio [(OR = 0.987, 95% CI (0.976–0.999, p = 0.027] were found to be independent predictors for the presence of significant CAD in patients with HCM (Table 3).
In the receiver operating characteristic (ROC) curve analysis, NT-proBNP/hs-TnT ratio lower than the cut-off value of 30.7 could detect the presence of significant CAD with 76.9% sensitivity and 53.6% specificity (AUC: 0.632, 95% CI 0.528–0.736, p = 0.019). In Hs-TnT analysis, it could detect significant coronary artery disease in HCM patients with a cutoff value of 17.8, a sensitivity of 76.9%, and a specificity of 52.2% (AUC: 0.629, 95% CI 0.531–0.726, p = 0.022) (Fig. 2).
Discussion
Our study has shown that cardiac biomarkers are significant predictors of the presence of significant coronary artery disease (CAD) in patients with hypertrophic cardiomyopathy (HCM). The NT-proBNP/hs-TnT ratio, which has rarely been evaluated in the literature, along with hs-TnT, was found to have high predictive value in ROC analyses and a significant association with CAD. Moreover, the NT-proBNP/hs-TnT ratio was an independent predictor of CAD in multivariate regression analysis, which is another noteworthy finding of our study. To our knowledge, this is the first study to investigate the role of cardiac biomarkers in determining the presence of CAD in patients with HCM.
Hypertrophic cardiomyopathy (HCM) is a genetic cardiovascular disorder that is characterized by left ventricular hypertrophy and diastolic dysfunction. Although HCM primarily affects the myocardium, it has been shown to be associated with an increased risk of developing coronary artery disease (CAD), which is a common form of cardiovascular disease that is caused by the narrowing or blockage of coronary arteries [3, 12, 13]. The mechanisms underlying the relationship between HCM and CAD are complex and multifactorial, but some proposed explanations include shared risk factors, such as hypertension and dyslipidemia, impaired myocardial perfusion, and a pro-inflammatory state [14]. The prevalence of coronary artery disease (CAD) in patients with hypertrophic cardiomyopathy (HCM) varies widely depending on the population studied and the diagnostic criteria used. Based on existing literature, the prevalence of CAD in patients with HCM can vary widely, with reported rates ranging from 10 to 53% [6]. In our study population, the prevalence of significant CAD was found to be 31.7%. These findings emphasize the importance of using symptom assessment and relevant parameters to predict the presence of CAD in patients with suspected disease, as approximately 1 in 3 patients with HCM may also have significant CAD.
The utilization of cardiac biomarkers as a means of risk assessment is gaining momentum. Although traditionally used solely in the diagnosis and follow-up of acute coronary syndrome, its application in various diseases' course and prognosis has become prevalent in contemporary clinical practice [15]. Cardiac biomarkers, particularly Hs-Troponin-T and N-terminal pro-B-type natriuretic peptide (NT-proBNP), play a pivotal role in the management of patients with hypertrophic cardiomyopathy (HCM) [9, 16, 17]. Elevated levels of these biomarkers in HCM patients are correlated with disease severity, myocardial fibrosis, and the risk of adverse clinical events. Hs-Troponin-T, specifically, is linked with an increased probability of sudden cardiac death and adverse cardiovascular events, whereas NT-proBNP levels are associated with symptom severity and prognosis. Consequently, biomarker evaluation is indispensable in the follow-up of HCM patients. Earlier research has demonstrated that cardiac biomarkers provide valuable diagnostic and prognostic contributions in chronic coronary syndrome patients [18, 19]. Elevated serum troponin T levels are prevalent in patients with stable coronary artery disease (CAD) [20]. The association between troponin level and the presence and severity of CAD has also been established. Certain studies have even asserted that cardiac biomarkers surpass exercise stress testing in stable CAD diagnosis [21]. Hs-TnT is among the biomarkers with the most significant effect, as evidenced in our study. Indeed, our study confirms that even a slight increase in hs-troponin-T values is indicative of significant coronary artery disease.
In the present study, we also evaluated the predictive effect of a rarely mentioned biomarker, NT-proBNP/TnT ratio, that has been previously studied for its ability to differentiate acute coronary syndrome from stress cardiomyopathy and to exclude acute coronary syndrome [11, 22]. Despite limited literature on the subject, our study suggests that this simple parameter, integrating cardiac biomarkers, could be an invaluable tool in determining the presence of significant CAD in HCM patients. Our results indicate that values below 30.3 can be used to predict significant CAD, making it a potential game-changer in risk assessment. However, we should note that while this biomarker shows promising results, it is not sufficient on its own to determine the presence of significant CAD. Therefore, utilizing patients' symptoms, clinical findings, ECG, and other imaging and diagnostic tools in combination with this biomarker may improve the accuracy of identifying patients at risk. This study highlights the importance of ongoing research into the use of cardiac biomarkers in clinical practice, and we are excited to contribute to this field with our findings.
Study limitations
There are several limitations to our study that must be acknowledged. Firstly, our study is limited by its single-center and retrospective design, which may introduce bias to the results. Additionally, the relatively small sample size may limit the generalizability of our findings. Moreover, the patient population underwent coronary angiography using different methods, including referral due to symptoms alone, exercise testing, and other imaging techniques. Furthermore, the determination of significant coronary artery disease was based solely on visual assessment, and hemodynamic significance was not evaluated using fractional flow reserve (FFR). It is also important to note that reference values and ranges for cardiac biomarkers may vary between different centers, which may impact the interpretation of our results.
Conclusion
In conclusion, our research underscores the critical role of cardiac biomarkers in assessing the risk and management of cardiovascular diseases, particularly in HCM and stable CAD patients. It emphasizes the importance of integrating cardiac biomarkers with other diagnostic tools to enhance disease diagnosis, prognosis, and follow-up.
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Sorajja P, Ommen SR, Nishimura RA, Gersh BJ, Berger PB, Tajik AJ (2003) Adverse prognosis of patients with hypertrophic cardiomyopathy who have epicardial coronary artery disease. Circulation 108:2342–2348
Elliott PM, Kaski JC, Prasad K, Seo H, Slade AK, Goldman JH, McKenna WJ (1996) Chest pain during daily life in patients with hypertrophic cardiomyopathy: an ambulatory electrocardiographic study. Eur Heart J 17:1056–1064
van der Velde N, Huurman R, Yamasaki Y, Kardys I, Galema TW, Budde RP, Zijlstra F, Krestin GP, Schinkel AF, Michels M, Hirsch A (2020) Frequency and significance of coronary artery disease and myocardial bridging in patients with hypertrophic cardiomyopathy. Am J Cardiol 125:1404–1412
Walston A, Behar VS (1976) Spectrum of coronary artery disease in idiopathic hypertrophic subaortic stenosis. Am J Cardiol 38:12–16
Lazzeroni E, Rolli A, Aurier E, Botti G (1992) Clinical significance of coronary artery disease in hypertrophic cardiomyopathy. Am J Cardiol 70:499–501
Puwanant S, Trongtorsak A, Wanlapakorn C, Songsirisuk N, Ariyachaipanich A, Boonyaratavej S (2021) Acute coronary syndrome with non-obstructive coronary arteries (ACS-NOCA) in patients with hypertrophic cardiomyopathy. BMC Cardiovasc Disord 21:556
Jacob R, Khan M (2018) Cardiac biomarkers: what is and what can be. Indian J Cardiovasc Dis Women WINCARS 3:240–244
Nadar SK, Shaikh MM (2019) Biomarkers in routine heart failure clinical care. Card Fail Rev 5:50–56
Matthia EL, Setteducato ML, Elzeneini M, Vernace N, Salerno M, Kramer CM, Keeley EC (2022) Circulating biomarkers in hypertrophic cardiomyopathy. J Am Heart Assoc 11:e027618
Topf A, Mirna M, Paar V, Motloch LJ, Bacher N, Franz M, Hoppe UC, Kretzschmar D, Lichtenauer M (2022) Differential diagnosis between Takotsubo syndrome and acute coronary syndrome—a prospective analysis of novel cardiovascular biomarkers for a more selective triage. J Clin Med 11:2974
Fröhlich GM, Schoch B, Schmid F, Keller P, Sudano I, Lüscher TF, Noll G, Ruschitzka F, Enseleit F (2012) Takotsubo cardiomyopathy has a unique cardiac biomarker profile: NT-proBNP/myoglobin and NT-proBNP/troponin T ratios for the differential diagnosis of acute coronary syndromes and stress induced cardiomyopathy. Int J Cardiol 154:328–332
Cokkinos DV, Krajcer Z, Leachman RD (1985) Hypertrophic cardiomyopathy and associated coronary artery disease. Tex Heart Inst J 12:147–151
Shin YJ, Lee JH, Yoo JY, Kim JA, Jeon Y, Yoon YE, Chun EJ (2019) Clinical significance of evaluating coronary atherosclerosis in adult patients with hypertrophic cardiomyopathy who have chest pain. Eur Radiol 29:4593–4602
Harjai KJ, Cheirif J, Murgo JP (1996) Ischemia and atherosclerotic coronary artery disease in patients with hypertrophic cardiomyopathy: a review of incidence, pathophysiological mechanisms, clinical implications and management strategies. Coron Artery Dis 7:183–187
Khan S, Rasool ST (2021) Current use of cardiac biomarkers in various heart conditions. Endocr Metab Immune Disord Drug Targets 21:980–993
Cambronero F, Marín F, Roldán V, Hernández-Romero D, Valdés M, Lip GYH (2009) Biomarkers of pathophysiology in hypertrophic cardiomyopathy: implications for clinical management and prognosis. Eur Heart J 30:139–151
Ho JE, Shi L, Day SM, Colan SD, Russell MW, Towbin JA, Sherrid MV, Canter CE, Jefferies JL, Murphy A, Taylor M, Mestroni L, Cirino AL, Sleeper LA, Jarolim P, Lopez B, Gonzalez A, Diez J, Orav EJ, Ho CY (2017) Biomarkers of cardiovascular stress and fibrosis in preclinical hypertrophic cardiomyopathy. Open Heart 4:e000615
Rusnak J, Fastner C, Behnes M, Mashayekhi K, Borggrefe M, Akin I (2017) Biomarkers in stable coronary artery disease. Curr Pharm Biotechnol 18:456–471
McCarthy CP, McEvoy JW, Januzzi JL (2018) Biomarkers in stable coronary artery disease. Am Heart J 196:82–96
Daněk J, Hnátek T, Malý M, Táborský M, Běláček J, Škvaril J, Pospíšilová L, Černohous M, Sedloň P, Hajšl M, Zavoral M (2017) Troponin levels in patients with stable CAD. Cor Vasa 59:e229-234
Tveit SH, Myhre PL, Hanssen TA, Forsdahl SH, Iqbal A, Omland T, Schirmer H (2022) Cardiac troponin I and T for ruling out coronary artery disease in suspected chronic coronary syndrome. Sci Rep 12:945
Kim DH, Lee SH, Kim SC, Kim T, Kang C, Jeong JH, Park YJ, Lim D, Lee SB (2019) The ratio of N-terminal pro-B-type natriuretic peptide to troponin I for differentiating acute coronary syndrome. Am J Emerg Med 37:1013–1019
Funding
The authors have no disclosures of funding.
Author information
Authors and Affiliations
Contributions
All authors have read and approved of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guler, A., Turkmen, I., Atmaca, S. et al. Influence of cardiac biomarkers on predicting significant coronary artery disease in hypertrophic cardiomyopathy patients. Heart Vessels 38, 1329–1336 (2023). https://doi.org/10.1007/s00380-023-02287-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-023-02287-0