Abstract
This study aimed to investigate the combined efficacy in prediction of major adverse cardiac events (MACE) by coronary regional physiological indices including coronary flow reserve (CFR) or fractional flow reserve (FFR) and high-sensitivity cardiac troponin-I (hs-cTnI) or N-terminal pro brain natriuretic peptide (NT-proBNP). Impaired CFR, decreased FFR, elevated cardiac troponin, and NT-proBNP are all associated with increased MACE, while these interaction or collinearity remains uncertain. The study included 429 patients with stable coronary artery disease (CAD) evaluated hs-cTnI and NT-proBNP levels before regional physiological measurement during coronary angiography. Patients were followed up for MACE including all-cause death, myocardial infarction, hospital admission for heart failure and target vessel remote revascularization. Median hs-cTnI and NT-proBNP values were 4 ng/L and 85 ng/L, respectively. Regional CFR was significantly albeit weakly correlated with hs-cTnI and NT-proBNP, while fractional flow reserve (FFR) was only linked to hs-cTnI. The addition of hs-cTnI and NT-proBNP on clinical backgrounds and angiographic score significantly improved predictive accuracy for MACE incidence, and further consideration of FFR and CFR could refine the model. The combined stratification using hs-cTnI, NT-proBNP, FFR and CFR could efficiently stratify patient risk for MACE. In patients with stable CAD, integrated assessment of cardiac biomarkers and physiological indices could be useful for predicting future cardiovascular events.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Coronary flow reserve (CFR) is an index of integrated coronary vasomotor function including epicardial stenosis, diffuse narrowing, and microvascular dysfunction. Impairment in CFR is associated with a high incidence of adverse cardiac events [1]. Although the prognostic value of global CFR measured by positron emission tomography (PET) has been recognized, the technique has limited availability in a majority of institutions. A Doppler-flow wire can be used to measure regional coronary flow velocity reserve together with fractional flow reserve (FFR), which might be useful in patient risk stratification [2]; however, this Doppler-based technique is time-consuming and may not be practical in clinical settings.
Cardiac troponins (cTn) and N-terminal pro-brain natriuretic peptide (NT-proBNP) are the two major cardiac biomarkers whose increased levels are independently linked to the risk of future adverse events [3]. Recently introduced high-sensitivity assays for cTn can detect circulating troponin levels in healthy individuals. The minor differences in the values within the upper reference limit (URL) can allow patient stratification for the future event risk [4]. Indeed, the high detection sensitivity of these assays has revolutionized clinical practice, because conventional assays cannot distinguish cTn values below the URL. NT-proBNP is an established marker of heart failure (HF), and its elevation is associated with major adverse cardiac events (MACE) in patients with or without HF [5]. However, more robust risk stratification is required for improving current clinical practice.
A previous study demonstrated both a relationship between PET-derived global CFR and the cTn level measured using conventional assays, and the independent contributions of the respective values to the prediction of MACE [6]. Therefore, the present study aimed to investigate the association of regional FFR/CFR, determined using a pressure–temperature sensor-tipped wire, and high-sensitivity cardiac troponin-I (hs-cTnI) and NT-proBNP in the prediction of cardiovascular outcomes of patients with stable coronary artery disease (CAD). We hypothesized that regional CFR, hs-cTnI and NT-proBNP can be used complementarily to predict future cardiovascular events.
Methods
Patient population
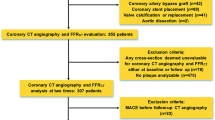
Patients with stable CAD who underwent hs-cTnI and NT-proBNP measurements before their scheduled coronary angiography (CAG) and subsequent physiological study at Tsuchiura Kyodo General Hospital between June 2014 and August 2017 were prospectively, but not consecutively, enrolled. A physiological study was indicated for the most diseased vessel with intermediate coronary lesions (30–80% diameter stenosis on visual assessment). Patients with angiographically significant left main disease,>80% diameter stenosis on visual assessment, visible collateral development, extremely tortuous or calcified coronary arteries, previous coronary artery bypass or other cardiac surgery, unstable symptoms (worsening angina or rest angina within a month) or acute changes on electrocardiogram (ECG), acute coronary syndrome or cardiac catheterisation within 6 months before index CAG, cardiogenic shock, renal insufficiency with baseline creatinine > 2.0 mg/dL, severe valvular diseases, left ventricular ejection fraction (LVEF) < 50%, previous heart failure, documented atrial fibrillation or other tachyarrhythmia, previous pacemaker implantation, suboptimal physiological recording, and unavailable informed consent were excluded from the study. From the 1022 patients who were screened, a total of 429 patients were included in the study. The Institutional Ethics Committee of our hospital approved the study protocol. Prompt optimal medical therapy was initiated in all patients after enrolment, and early revascularization based on the index CAG results was performed following current guidelines [7]. All patient data and procedural details were obtained from medical records and telephone interviews.
Biochemical measurement analysis
Baseline hs-cTnI and NT-proBNP levels were determined from blood samples obtained using the radial sheath inserted before CAG. Sampling was conducted in the morning in clinically stable patients at a fasting state, to reduce diurnal variations of the biomarkers [8]. Hs-cTnI was measured using the ARCHITECT i2000SR STAT hs-cTnI assay (Abbott Laboratories, North Chicago, IL, USA); The 99th percentile cut-off values (URLs) were 32.7 ng/L for men and 17.9 ng/L for women, according to a previous Asian community-cohort study [9]. The lower limit of detection (LOD) was 1.5 ng/L. NT-proBNP levels were determined using the Elecsys proBNP assay (Roche Diagnostics, Basel, Switzerland). The LOD was 5 ng/L.
Angiographic assessment
Quantitative coronary angiography (QCA) analyzes were performed using dedicated offline software (QAngio XA 7.3; Medis Medical Imaging Systems BV, Leiden, The Netherlands). In order to assess the complexity of coronary lesions, SYNTAX score was determined using the online, most recently updated calculator (SYNTAX SCORE I from https://www.SYNTAXscore.com).
Cardiac catheterization and physiological studies
All patients underwent standard CAG via a radial artery and using a 5-French system. Physiological indices were measured using a pressure–temperature sensor-tipped wire, as described previously [10]. After calibration, a coronary 0.014-inch PressureWire™ (St. Jude Medical, St. Paul, MN, USA) was used to measure the intracoronary pressure distal to the coronary stenosis. Subsequently, 3 mL of saline at room temperature was administered three times, and the baseline mean transit time (Tmn) was determined. For both measurements, maximal hyperaemia was induced by an intravenous infusion of adenosine 5′-triphosphate (160 μg kg−1 min−1). FFR was calculated as the ratio of mean distal-to-aortic coronary pressure (Pd/Pa) during maximum hyperaemia. CFR was defined as the resting Tmn divided by the hyperaemic Tmn values.
Clinical follow-up
Clinical follow-up data were collected via a review of the medical records and/or telephonic interviews. The primary endpoint was a composite of death, non-fatal spontaneous myocardial infarction (MI) defined by current guidelines, hospital admission owing to congestive heart failure, and target vessel revascularization (TVR) occurring at least 3 months after CAG. All revascularizations based on the index CAG results were performed within 3 months after the procedure and were not counted as the endpoint. All MIs occurred>30 days after the CAG procedures.
Statistical analysis
Categorical data, expressed as frequencies and percentages, were compared using the χ2 or Fisher’s exact test, as appropriate. Continuous variables were expressed as the median (interquartile range [IQR]) and compared using Student’s t test or Mann–Whitney U test for variables with a normal or non-normal distribution, respectively. Kruskal–Wallis test was applied for comparisons among three or more groups. A Cox proportional hazards regression model was used to assess the association between FFR, CFR, hs-cTnI, NT-proBNP and clinical outcomes. The logarithmic transformed values of hs-cTnI and NT-proBNP were entered into the models. The prognostic information of each biomarker or physiological index was compared based on the c-statistic calculated from the model comprising the baseline characteristics and each factor. Baseline characteristics showing p < 0.05 in univariate COX regression models (age and SYNTAX score) were selected and entered into the models. Further, to evaluate the added effect of cardiac biomarkers and physiological indices on the discrimination of MACE, we constructed four clinical models and calculated the c-statistic, tested using integrated discrimination improvement (IDI) and net reclassification improvement (NRI). Receiver operating characteristic (ROC) analyzes were used to determine the best cut-offs of hs-cTnI and NT-proBNP in predicting the incidence of MACE. Based on the total number of worse profiles of hs-cTnI, NT-proBNP, FFR and CFR, patients were divided into five groups. In these groups, event rates over time were estimated using the Kaplan–Meier method, and linear trends were tested using log-rank tests. Statistical analyzes were performed using JMP 11.2.0 (SAS Institute Inc., Cary, NC) or R 3.4.4 (The R Foundation). A two-sided p value <0.05 was considered to indicate statistical significance.
Results
Baseline clinical features
The baseline clinical characteristics of the total cohort are presented in Table 1. The mean age of the study population was 68.0 ± 9.5 years, and 336 patients (78.3%) were male. The median hs-cTnI and NT-proBNP values were 4 (2–8) ng/L and 85 (45–176) ng/L, respectively. Hs-cTnI levels exceeded the URL in 10 (2.3%) patients, and 33 patients (7.7%) had hs-cTnI levels below the LOD. One patient had an NT-proBNP level below the LOD. Hs-cTnI and NT-proBNP levels were mildly correlated (R = 0.22, p < 0.001). The median FFR and CFR values were 0.81 (0.75–0.86) and 2.8 (1.8–3.9), respectively. CFR <2.0 was determined in 126 (29.4%) patients. The association between FFR and CFR was significant (R = 0.43, p < 0.001). The distributions of hs-cTnI, NT-proBNP, FFR and CFR in the total cohort are shown in Fig. 1.
Distributions of hs-cTnI, NT-proBNP, FFR and CFR. Histograms showing the distributions of cardiac biomarkers and physiological indices. The median values (lower–upper interquartile range) of high-sensitivity cardiac troponin-I (hs-cTnI), N-terminal pro brain natriuretic peptide (NT-proBNP), fractional flow reserve (FFR), and coronary flow reserve (CFR) are 4 (2–7) ng/L, 85 (45–175) ng/L, 0.81 (0.75–0.86) and 2.8 (1.8–3.9), respectively
Association between regional physiological indices and cardiac biomarkers
Linear correlations were found for hs-cTnI and FFR, hs-cTnI and CFR, NT-proBNP and CFR (p = 0.049, 0.015, and <0.001, respectively) but not for NT-proBNP and FFR (p = 0.76). Figure 2 shows the biomarker levels in groups divided by the cut-offs of CFR =2.0 and FFR =0.80. Patients with CFR <2.0 or FFR ≤0.8 had higher hs-cTnI levels than those of patients with CFR ≥2.0 or FFR >0.8 (p < 0.001 and p = 0.005, respectively). NT-proBNP values were higher in patients with CFR <2.0 than in those with CFR ≥2.0 (p < 0.001), whereas the difference of values between patients with FFR ≤0.8 and FFR >0.8 was not significant (p = 0.11).
Association between biomarkers and coronary physiology. Circulating levels of hs-cTnI (ng/L) (a) and NT-proBNP (ng/L) (b) in patients divided according to the validated thresholds of CFR and FFR. Patients with FFR ≤0.8 or CFR <2.0 had higher hs-cTnI levels compared to those with FFR >0.8 or CFR ≥2.0. NT-proBNP values were higher in patients with CFR <2.0 than with CFR ≥2.0, although there was no significant difference between patients with FFR ≤0.8 and FFR >0.8. Abbreviations as in Fig. 1
Comparison of the prognostic information of cardiac biomarkers and physiological parameters
During a median follow-up period of 18 (12–29) months, 27 patients (6.3%) met the primary endpoint; specifically, 9 deaths, 3 non-fatal MIs, 2 admissions for worsening HF and 13 TVRs were documented. In univariate COX regression models, the cumulative incidence of MACE was significantly associated with patient age, SYNTAX score, impaired CFR, decreased FFR, elevated hs-cTnI and NT-proBNP levels (Table 2).
The prognostic accuracy of FFR, CFR, hs-cTnI and NT-proBNP was compared in models comprising age and SYNTAX score plus one of these factors. The c-statistic was 0.73 (0.63–0.84) for FFR, 0.78 (0.67–0.89) for CFR, 0.72 (0.61–0.83) for hs-cTnI, and 0.72 (0.61–0.83) for NT-proBNP (Fig. 3). There was no significant difference in the c-statistic of every pair among these four models (all p > 0.05).
Adjusted ROC curves in the prediction of MACE. Receiver operating characteristic (ROC) curves for determining major adverse cardiac events (MACE) by hs-cTnI (a), NT-proBNP (b), FFR (c) and CFR (d). These models were adjusted by age and SYNTAX score, which were selected based on criteria of p < 0.05 in univariate COX-proportional regression analyses. There was no significant difference in the predictive accuracy in every pair of the models (all: p > 0.05). Abbreviations as in Fig. 1
Integrated assessment of hs-cTnI, NT-proBNP, FFR and CFR in the prediction of future adverse events
We constructed four clinical models in order to assess the additive prognostic ability of the biomarkers and physiological indices on baseline and angiographic variables (Table 3). The addition of cardiac biomarkers to a model consisting of age and SYNTAX score significantly improved the predictive accuracy (NRI 0.479, p = 0.015; IDI 0.099, p = 0.016). Consideration of FFR in the model increased the predictive accuracy (NRI 0.563, p = 0.004; IDI 0.012, p = 0.18). The addition of CFR could further refine the model (NRI 0.507, p = 0.006; IDI 0.020, p = 0.005).
Patients were then categorized into five groups according to the total number of worse profiles in hs-cTnI, NT-proBNP, FFR and CFR (0/4 to 4/4). The cut-off values of hs-cTnI and NT-proBNP were determined according to the ROC analysis of each factor in the prediction of MACE (8 ng/L for hs-cTnI and 104 ng/L for NT-proBNP), and the established cut-off values of FFR =0.80 and CFR =2.0 were used. Figure 4 illustrates survival from MACE in patients of each group. The categorization powerfully stratified patient risk for MACE (log-rank chi-square =112.1, p < 0.001). Of note, patients with elevated levels of both biomarkers and impaired FFR as well as CFR had an extremely high incidence of MACE (11/24, 45.8%). The incidence of MACE was low if patients had fewer than two risk factors (9/353, 2.5%). Integrated assessment of cardiac biomarkers and physiological indices was practically useful for estimation of future risk in patients with stable CAD.
Survival from MACE in patients divided according to the combination of biomarkers and physiological indices. Kaplan–Meier curves demonstrating survival from MACE in patients divided according to the total number of worse profiles in hs-cTnI, NT-proBNP, FFR and CFR (0/4 to 4/4). The cut-offs were 8 ng/l for hs-cTnI, 104 ng/l for NT-proBNP, 0.80 for FFR and 2.0 for CFR. The categorization powerfully stratified patient risk for MACE (log-rank chi-square =112.1, p < 0.001). The table shows the adjusted hazard ratio (HR) and the corresponding 95% confidence interval (CI) in each group. Abbreviations as in Figs. 1 and 3
Discussion
To the best of our knowledge, this is the first study to demonstrate the association of regional coronary physiological parameters with circulating levels of hs-cTnI and NT-proBNP in patients with stable CAD, and the combined efficacy of these measurements in the prediction of future cardiovascular events. The novel findings of this study are as follows: (1) hs-cTnI levels were significantly related to CFR and FFR whereas NT-proBNP levels were associated only with CFR; (2) the addition of hs-cTnI and NT-proBNP levels to clinical backgrounds and angiographic score significantly improved the predictive accuracy for the incidence of MACE, and further consideration of FFR and CFR could refine the model; (3) the combination of cardiac biomarkers and physiological indices could enable efficient stratification of future risk for adverse events; and (4) patients were at an extremely high risk for MACE if they had elevated hs-cTnI and NT-proBNP levels as well as impaired CFR and FFR.
Our results revealed significant relationships between CFR and hs-cTnI or NT-proBNP, whereas FFR was significantly associated only with hs-cTnI, suggesting that circulating subclinical hs-cTnI and NT-proBNP levels provide different coronary physiological information. Given that previous studies identified CFR as a potential marker of reduced vasomotor function or endothelium-independent coronary microvascular disease, an impaired CFR would be strongly associated with future adverse events [11]. Elevated cardiac troponin levels are also associated with an increased incidence of cardiovascular death and HF in patients with stable CAD and a preserved LVEF, suggesting an interaction between decreased vasomotor function and subclinical myocardial injury in the course of microvascular dysfunction, diastolic dysfunction and HF [12,13,14]. Increased BNP or NT-proBNP level has been proposed as markers of preclinical cardiovascular disease, including endothelial dysfunction [15, 16]. Our findings suggest that elevated Hs-cTn and NT-proBNP are indicators of a shared process of vasomotor dysfunction, whereas NT-proBNP release might be linked to atherosclerosis that is not necessarily linked to epicardial obstruction.
Taqueti et al. demonstrated the independent association of an impaired global CFR with cardiac troponin elevation measured by conventional assays, and that CFR modified the effect of a positive troponin level on cardiovascular outcomes [6]. In accordance with that study, we showed the complementary effects of regional CFR and cardiac biomarker levels on the prediction of future adverse cardiovascular events. Although the prognostic implication of global CFR determined by PET myocardial perfusion imaging has been established, that of coronary regional CFR has yet to be fully validated. Hoef et al. showed that Doppler-flow wire-derived regional CFR was related to the incidence of MACE with a normal or abnormal FFR [2]. The present study indicated the significant association between the incidence of MACE and impaired regional CFR, determined using a pressure–temperature sensor-tipped wire. This technique is highly feasible and practically available in clinical settings, unlike Doppler-flow wire methods, and the simultaneous measurement of FFR may provide a better understanding of the regional coronary physiology [17].
The high-sensitive assays for cardiac troponin can detect subtle myocardial injury, which could not be determined by the conventional ones. Less than 3% of the patients in this study had hs-cTnI levels above the URL. Previous studies included a number of patients with ‘positive troponin’ levels determined by conventional assays, although those assays are unable to distinguish troponin levels below the URL [6, 18]. In our population, we were able to demonstrate the prognostic implication of hs-cTnI based on a cut-off value of 8 ng/L, which could be determined only by the high-sensitivity assay. We also demonstrated the prognostic efficacy of NT-proBNP on patient outcomes. In contrast to the relationship between cardiac troponin and CAD, the relationship between NT-proBNP and CAD has not been well investigated. A recent study showed that myocardial ischemia was an independent predictor of increased NT-proBNP level [19]. As our study included only patients with a preserved LVEF and no history of HF, the association between high NT-proBNP and the incidence of MACE may be linked to an impaired coronary circulation, that is, low CFR. In our study, almost all the future cardiovascular events occurred in patients with combined elevated biomarkers and impaired physiological function. This implies that the prognostic information of these biomarkers is largely contributed from that of the regional physiological parameters or vice versa, with partly the same mechanistic relevance in terms of coronary vasomotor dysfunction or ischemia.
An integrated approach to vasomotor function via a focused therapeutic strategy aiming at the revascularization of an epicardial stenosis may improve patient prognosis. To date, no clinical trial has shown that improving CFR strategy lowers the risk of MACE. Nonetheless, previous studies have suggested that statins can improve measures of endothelial dysfunction, microvascular dysfunction or coronary flow [20, 21]. Accordingly, the simultaneous assessment of regional physiological indices and cardiac biomarkers may be useful to evaluate the causal effects of medical interventions on the reduction of future cardiovascular events. A recent prospective study showed a decrease in hs-cTn levels by statin therapy [22]. Prospective studies are warranted to further elucidate the prognostic efficacy and clinical utility of the integrated assessment of cardiac biomarkers and coronary physiology.
Limitations
The results of the present study should be interpreted with several important limitations. As this was an observational study conducted at a single center, it cannot escape selection bias. Strict exclusion criteria were required in order to investigate the tiny differences of the highly sensitive cardiac biomarkers; however, this could lead to selection bias, and the present population would not reflect real clinical settings. Further, patients with unrecognized cardiomyopathy, which could have influenced hs-cTnI or NT-proBNP values, were not excluded. Our relatively modest sample size limited extensive subgroup analysis related to, for example, diabetes mellitus, sex, dyslipidaemia and revascularization. The difference in the hs-cTnI and NT-proBNP levels of the patients was statistically significant but numerically small, potentially within the diurnal individual variation. Thus, hs-cTnI level itself could not be used to reliably predict the relationship with physiological indices at the individual patient level. However, higher hs-cTnI levels in patients with CAD who showed reduced CFR suggest ongoing, low-grade myocyte damage. Finally, as this study included only patients with stable CAD, the event rate and number were limited, and the study may have been underpowered for multivariate analyses. The independent association between biomarkers or physiological indices and MACE incidence could not be determined in this sample size. However, the incidence of MACE in patients with elevated hs-cTnI and NT-proBNP as well as impaired physiological indices was extremely high, and the clinical implication is clear. A larger, prospective study is warranted in this regard.
Conclusion
In patients with stable CAD, integrated assessment of cardiac biomarkers and physiological indices could be useful for predicting future cardiovascular events. Patients with mildly elevated hs-cTnI and NT-proBNP along with impaired physiological function had eminently poor prognosis.
References
Taqueti VR, Hachamovitch R, Murthy VL, Naya M, Foster CR, Hainer J, Dorbala S, Blankstein R, Di Carli MF (2015) Global coronary flow reserve is associated with adverse cardiovascular events independently of luminal angiographic severity and modifies the effect of early revascularization. Circulation 131:19–27
van de Hoef TP, van Lavieren MA, Damman P, Delewi R, Piek MA, Chamuleau SA, Voskuil M, Henriques JP, Koch KT, de Winter RJ, Spaan JA, Siebes M, Tijssen JG, Meuwissen M, Piek JJ (2014) Physiological basis and long-term clinical outcome of discordance between fractional flow reserve and coronary flow velocity reserve in coronary stenoses of intermediate severity. Circ Cardiovasc Interv 7:301–311
Ndrepepa G, Braun S, Schulz S, Fusaro M, Keta D, Pache J, Seyfarth M, Mehilli J, Schomig A, Kastrati A (2011) Sensitive troponin and N-terminal probrain natriuretic peptide in stable angina. Eur J Clin Invest 41:1054–1062
Roos A, Bandstein N, Lundback M, Hammarsten O, Ljung R, Holzmann MJ (2017) Stable high-sensitivity cardiac troponin T levels and outcomes in patients with chest pain. J Am Coll Cardiol 70:2226–2236
Kragelund C, Gronning B, Kober L, Hildebrandt P, Steffensen R (2005) N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med 352:666–675
Taqueti VR, Everett BM, Murthy VL, Gaber M, Foster CR, Hainer J, Blankstein R, Dorbala S, Di Carli MF (2015) Interaction of impaired coronary flow reserve and cardiomyocyte injury on adverse cardiovascular outcomes in patients without overt coronary artery disease. Circulation 131:528–535
Wijns W, Kolh P, Danchin N, Di Mario C, Falk V, Folliguet T, Garg S, Huber K, James S, Knuuti J, Lopez-Sendon J, Marco J, Menicanti L, Ostojic M, Piepoli MF, Pirlet C, Pomar JL, Reifart N, Ribichini FL, Schalij MJ, Sergeant P, Serruys PW, Silber S, Sousa Uva M, Taggart D (2010) Guidelines on myocardial revascularization. Eur Heart J 31:2501–2555
Klinkenberg LJ, van Dijk JW, Tan FE, van Loon LJ, van Dieijen-Visser MP, Meex SJ (2014) Circulating cardiac troponin T exhibits a diurnal rhythm. J Am Coll Cardiol 63:1788–1795
Aw TC, Phua SK, Tan SP (2013) Measurement of cardiac troponin I in serum with a new high-sensitivity assay in a large multi-ethnic Asian cohort and the impact of gender. Clin Chim Acta 422:26–28
Pijls NH, De Bruyne B, Smith L, Aarnoudse W, Barbato E, Bartunek J, Bech GJ, Van De Vosse F (2002) Coronary thermodilution to assess flow reserve: validation in humans. Circulation 105:2482–2486
Petersen JW, Pepine CJ (2015) Microvascular coronary dysfunction and ischemic heart disease: where are we in 2014? Trends Cardiovasc Med 25:98–103
Ndrepepa G, Braun S, Mehilli J, Birkmeier KA, Byrne RA, Ott I, Hosl K, Schulz S, Fusaro M, Pache J, Hausleiter J, Laugwitz KL, Massberg S, Seyfarth M, Schomig A, Kastrati A (2011) Prognostic value of sensitive troponin T in patients with stable and unstable angina and undetectable conventional troponin. Am Heart J 161:68–75
Everett BM, Brooks MM, Vlachos HE, Chaitman BR, Frye RL, Bhatt DL (2015) Troponin and cardiac events in stable ischemic heart disease and diabetes. N Engl J Med 373:610–620
deFilippi CR, de Lemos JA, Christenson RH, Gottdiener JS, Kop WJ, Zhan M, Seliger SL (2010) Association of serial measures of cardiac troponin T using a sensitive assay with incident heart failure and cardiovascular mortality in older adults. JAMA 304:2494–2502
Pauriah M, Khan F, Lim TK, Elder DH, Godfrey V, Kennedy G, Belch JJ, Booth NA, Struthers AD, Lang CC (2012) B-type natriuretic peptide is an independent predictor of endothelial function in man. Clin Sci (Lond) 123:307–312
Rubattu S, Sciarretta S, Valenti V, Stanzione R, Volpe M (2008) Natriuretic peptides: an update on bioactivity, potential therapeutic use, and implication in cardiovascular diseases. Am J Hypertens 21:733–741
Barbato E, Aarnoudse W, Aengevaeren WR, Werner G, Klauss V, Bojara W, Herzfeld I, Oldroyd KG, Pijls NH, De Bruyne B (2004) Validation of coronary flow reserve measurements by thermodilution in clinical practice. Eur Heart J 25:219–223
Blankenberg S, Zeller T, Saarela O, Havulinna AS, Kee F, Tunstall-Pedoe H, Kuulasmaa K, Yarnell J, Schnabel RB, Wild PS, Munzel TF, Lackner KJ, Tiret L, Evans A, Salomaa V (2010) Contribution of 30 biomarkers to 10-year cardiovascular risk estimation in 2 population cohorts: the MONICA, risk, genetics, archiving, and monograph (MORGAM) biomarker project. Circulation 121:2388–2397
Caselli C, Prontera C, Liga R, De Graaf MA, Gaemperli O, Lorenzoni V, Ragusa R, Marinelli M, Del Ry S, Rovai D, Giannessi D, Aguade-Bruix S, Clemente A, Bax JJ, Lombardi M, Sicari R, Zamorano J, Scholte AJ, Kaufmann PA, Knuuti J, Underwood SR, Clerico A, Neglia D (2016) Effect of coronary atherosclerosis and myocardial ischemia on plasma levels of high-sensitivity troponin T and NT-proBNP in patients with stable angina. Arterioscler Thromb Vasc Biol 36:757–764
Guethlin M, Kasel AM, Coppenrath K, Ziegler S, Delius W, Schwaiger M (1999) Delayed response of myocardial flow reserve to lipid-lowering therapy with fluvastatin. Circulation 99:475–481
Fujii K, Kawasaki D, Oka K, Akahori H, Iwasaku T, Fukunaga M, Eguchi A, Sawada H, Masutani M, Lee-Kawabata M, Tsujino T, Ohyanagi M, Masuyama T (2011) The impact of pravastatin pre-treatment on periprocedural microcirculatory damage in patients undergoing percutaneous coronary intervention. JACC Cardiovasc Interv 4:513–520
Ford I, Shah AS, Zhang R, McAllister DA, Strachan FE, Caslake M, Newby DE, Packard CJ, Mills NL (2016) High-sensitivity cardiac troponin, statin therapy, and risk of coronary heart disease. J Am Coll Cardiol 68:2719–2728
Acknowledgements
We thank the physicians, nurses, other catheter laboratory staffs, and patients involved in this study.
Funding
No funding was used to support this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All the authors have nothing to declare.
Rights and permissions
About this article
Cite this article
Hamaya, R., Yonetsu, T., Kanaji, Y. et al. Interrelationship in the prognostic efficacy of regional coronary flow reserve, fractional flow reserve, high-sensitivity cardiac troponin-I and NT-proBNP in patients with stable coronary artery disease. Heart Vessels 34, 410–418 (2019). https://doi.org/10.1007/s00380-018-1260-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1260-z