Abstract
Data on the mid-term clinical outcomes after endovascular treatment (EVT) using a Crosser catheter (C. R. Bard, Inc.) as a crossing or flossing device for a heavily calcified lesion in the common femoral artery (CFA) or popliteal artery (PA) are lacking. The aim of this study was to investigate the safety and efficacy of EVT using a Crosser catheter for isolated and heavily calcified CFA or PA disease. We retrospectively analyzed 64 consecutive patients (72 lesions; CFA 30, PA 42) who underwent EVT for heavily calcified CFA or PA lesions with Crosser catheters between April 2015 and April 2019. The primary endpoint was clinically driven target lesion revascularization (CD-TLR). The median follow-up was 18.5 months. The mean age of the study population was 70 ± 9.5 years, with a male prevalence of 73.6%. The mean Proposed Peripheral Artery Calcification Scoring System grade was 2.9 ± 0.9. Procedure success, defined as 50% or less residual stenosis without suboptimal results, was achieved in 94.4% of lesions. There were no cases of bailout stenting or target lesion-related complications. After EVT, the 1-year CD-TLR-free rate for CFA and PA lesions was 87.4 and 76.8%, respectively. The corresponding rates at 2 years were 82.2 and 62.8%, respectively. In the multivariate analysis used to define CD-TLR predictors for CFA and PA lesions, hemodialysis was the only independent predictor (HR 3.35, 95% CI 1.02–13.95, P = 0.045). EVT with a Crosser device for heavily calcified CFA and PA lesions seems to be safe and feasible.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Endovascular treatment (EVT) has emerged as the first-line therapy for most patients with claudication or critical limb ischemia (CLI). It has gained widespread acceptance among vascular physicians and patients because of its minimal invasiveness [1]. The common femoral artery (CFA) and popliteal artery (PA) are considered ‘non-stenting zones’ due to the difficulty of deploying stents in vessels around highly flexible joints. Plain balloon angioplasty is widely performed in non-stenting zones, and stents are used only for the bailout. However, the clinical outcomes of plain balloon angioplasty without stenting are inferior compared with surgical treatment [2,3,4,5]. To improve the clinical outcomes of plain balloon angioplasty in the non-stenting zone, we previously reported high-pressure expansion effectiveness [6].
The Crosser catheter (C. R. Bard, Inc., Murray Hill, NJ, U.S.A.) is a unique device that facilitates antegrade intraluminal recanalization by high-frequency vibration energy and cavitation. It vibrates 20,000 times/s against chronic total occlusions (CTOs), causing microbubbles to expand and implode, breaking the molecular bonds and eroding the surface of CTOs [7]. Previous reports have demonstrated the usefulness of the Crosser catheter as a CTO crossing and flossing device [8, 9]. Although several papers were concerned with the initial success rate [9,10,11,12,13], the mid-term clinical results of EVT with a Crosser device in the non-stenting zone have not been reported. Therefore, the purpose of this study was to investigate the efficacy and safety of EVT using a Crosser catheter for isolated and heavily calcified CFA and PA disease.
Materials and methods
Study design and patient population
We retrospectively enrolled consecutive patients who received EVT for de novo isolated CFA and PA lesions with Crosser catheters between April 2015 and April 2019 at Tokyo Women’s Medical University Hospital in Tokyo, Japan. We excluded the lesions that extended proximally or distally and not much calcified enough to require a Crosser system. A total of 64 consecutive patients (72 lesions; CFA 30, PA 42) who underwent EVT were included. The optimal treatment strategy for lower extremity lesions in our hospital is routinely discussed within the cardiology team, consisting of cardiovascular interventionists and surgeons. EVT is generally selected as the first-line treatment for CFA and PA lesions, if possible. Endarterectomy is chosen only when EVT is not feasible because of vascular access problems (for example, bilateral CFA occlusion) or when restenosis has occurred repeatedly. Indications for intervention were the presence of a significant and symptomatic atherosclerotic occlusive lesion (Rutherford category: 2, 3, 4, 5, and 6), more than 90% stenosis on angiography, or more than 50% stenosis with a pressure gradient of more than 20 mmHg. We evaluated the pressure gradient using a pressure wire or extraction with a 4-Fr JR diagnostic catheter in patients with intermediate stenosis. Bifurcated CFA lesions were classified according to the Medina classification [4]. Patients who were lost to follow-up within 6 months were excluded.
The study protocol was based on the regulations of the institutional ethics committee of Tokyo Women’s Medical University Hospital. All participating patients provided written informed consent. Patient enrollment was performed according to the principles of the Declaration of Helsinki.
Endovascular procedures
All patients received antiplatelet therapy (aspirin 100 mg/day or clopidogrel 75 mg/day) before the procedure. After inserting a 4- to 6-Fr sheath from the ipsilateral or contralateral CFA, unfractionated heparin (1000–5000 IU) was injected from the sheath and supplemented as required to maintain an activated clotting time of above 200 s. Calcium in the lesions was assessed using unsubtracted angiograms, and the degree of lesion calcification was categorized utilizing the proposed Peripheral Artery Calcification Scoring System (PACSS): Grade 0 was defined as no visible calcium at the target lesion site; Grade 1 was defined as unilateral calcification less than 5 cm; Grade 2 was defined as unilateral calcification greater than 5 cm; Grade 3 was defined as bilateral calcification less than 5 cm, and Grade 4 was defined as bilateral calcification greater than 5 cm [14]. Our EVT strategy for heavily calcified CFA and PA lesions had four steps. First, we chose an adequate intraplaque route, not subintimal tracking, for occlusive CFA and PA lesions with biplane cineangiography using a 0.014-in. guidewire. Second, we used the Crosser system in heavily calcified cases either as a crossing or flossing device. Third, we expanded the lesions up to the rated pressure or at the highest pressure tolerated by the patient without vascular pain, using a non-compliant balloon. Fourth, we set the clear endpoint of EVT as less than 5 mmHg of the pressure gradient after angioplasty. The residual pressure gradient was evaluated by measuring the extraction using a 4-Fr JR diagnostic catheter in all cases. When there were suboptimal angiographic results, repeated inflations were performed at the discretion of the attending physician to achieve a residual stenosis percentage of less than 50% and an optimized residual pressure gradient less than 5 mmHg. We used a stent only when flow-limiting dissection occurred after balloon angioplasty. In this study, we did not use drug-coated balloons. We treated lesions involving the deep femoral artery (DFA) simultaneously with the kissing balloon technique only when CFA lesions occurred within DFA lesions (Medina classification 1-1-0 or 1-1-1), except for cases involving occlusive DFA. After the procedures, we evaluated the presence of distal embolization by angiography in all cases. All procedures were performed in the catheter laboratory using local anesthesia.
Endpoint and definitions
Procedural success was defined as successful vascular access, endovascular procedure completion, and immediate morphologic success with less than 50% of residual diameter reduction according to angiography and the residual pressure gradient less than 5 mmHg. Clinical success was defined as a combination of procedural success and at least one improvement of the Rutherford criteria.
The primary endpoint was clinically driven target lesion revascularization (CD-TLR) for CFA or PA, either percutaneous or surgical. The secondary endpoints were freedom from loss of patency, overall survival, freedom from major adverse cardiovascular events (MACE; all-cause death, non-fatal myocardial infarction, and stroke), freedom from major adverse limb events (MALE; major amputation and revascularization for target limb), and freedom from complications. Loss of patency was defined as a reduction in the ankle-brachial index (ABI) of 0.2 or more [15, 16]. We also examined the ABI and Rutherford category classes before and after the procedures. The timing of the ABI and Rutherford category evaluation after the procedure was at the patients’ first visit (1 month after the procedure) to our hospital. In cases where patients were hospitalized for more than 1 month, the evaluation was performed 1 month after EVT. Poor runoff was defined as one vessel or none of the infrapopliteal runoff. [17]
Statistical analysis
Categorical variables are presented as counts (percentages), whereas continuous variables are reported as means ± standard deviation. Categorical variables were compared using Fisher’s exact test or the chi-squared test. Continuous variables with normal and non-normal distributions were compared using the unpaired t test and Mann–Whitney U test. The cumulative incidence rate of CD-TLR was analyzed based on time to the first adverse event and estimated using the Kaplan–Meier method with the log-rank test. Univariable and multivariable logistic regression analyses were performed to detect CD-TLR predictors. A two-sided P value of less than 0.05 was considered to statistical significance. All statistical analyses were performed by an independent physician using statistical software (JMP 11; SAS Institute Inc., Cary, NC, USA).
Results
During the study period, 64 consecutive patients underwent 72 percutaneous CFA and PA interventions (CFA 30, PA 42). Baseline patient characteristics, lesion characteristics, and procedural parameters and techniques are reported in Tables 1 and 2. Compared with patients with CFA disease, those with PA disease were more likely to have diabetes and CLI and had better left ventricular ejection fraction. In the lesion-based analysis, the CFA lesion was more likely to have bifurcation (CFA vs. PA = 56.7 vs. 4.8%, P < 0.0001). PACSS grade 3 or 4 was seen in 83.3% of CFA lesions and 85.7% of PA lesions. Clinical outcomes are shown in Table 3. Procedural success was achieved in 96.7% (29 of 30) of CFA lesions and 92.9% (39 of 42) of PA lesions. Complications only occurred in CFA lesions, with 2 cases of the detachment of the metal chip of the Crosser system. There were no other complications related to the Crosser catheter. There were no cases of bailout stenting for flow-limiting dissection.
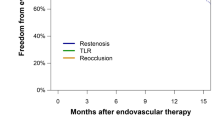
The median follow-up period was 18.5 months (interquartile range 9–30.2). Figure 1 shows the Kaplan–Meier curves of freedom from the CD-TLR. The overall rate of freedom from CD-TLR at 1 and 2 years was 80.8 and 70.1%, respectively. After EVT, the 1- and 2-year rates of freedom from CD-TLR for CFA lesions were 87.4 and 82.2%, respectively. The 1- and 2-year rates of freedom from CD-TLR for the PA were 76.8 and 62.2%, respectively. There was no significant difference in CD-TLR between CFA and PA.
In the multivariate analysis used to define CD-TLR predictors for both CFA and PA lesions, hemodialysis was the only independent predictor (Table 4; Fig. 2).
Discussion
This study had 2 main findings. First, EVT for isolated CFA and PA lesions with severe calcification using the Crosser system is associated with a high success rate and low complication rate. Second, hemodialysis was identified as an independent CD-LTR predictor in the multivariate analysis.
Several previous studies have reported the technical success rate of EVT using the Crosser system for calcified lesions in the lower limbs [9,10,11,12,13]. However, the majority of these studies used the Crosser device as a crossing device. Our study used the Crosser catheter as a CTO crossing device or as a flossing device after using a guidewire to pass the lesion. Tan et al. [9] reported that the overall primary technical success rate was 93.3%, consistent with our findings.
To the best of our knowledge, the present study is the first to evaluate the mid- and long-term clinical outcomes of EVT using the Crosser catheter for highly calcified CFA or PA lesions. Davies et al. performed a retrospective review of 115 patients who underwent intervention for CFA lesions [18]. As with our study, the main outcome was the re-intervention rate. The 1- and 3-year re-intervention-free survival rates were 77 and 57%, respectively. In their retrospective review of 93 patients who underwent CFA intervention identified from a Japanese registry, Soga et al. [17] found that the 1- and 5-year primary patency rates for CFA lesions after EVT were 73.3 and 46.9%, respectively. Only a few studies to date have evaluated outcomes after EVT for PA lesions compared with CFA lesions. Semaan et al. [19] found that the primary patency of PA angioplasty at 3, 6, and 12 months was 89, 82, and 73%, respectively. Rastan et al. [20] reported that during the 2 years of follow-up of patients treated with PA angioplasty alone, CD-TLR at 1 year was 59.5%. Although our study was limited to severely calcified cases, our results showed superior peri-procedural and long-term outcomes of EVT for CFA or PA lesions relative to the outcomes in previous studies [17, 18, 23]. Our EVT strategy, such as high-pressure balloon dilatation, usage of the Crosser system, and the wiring policy mentioned above, might affect the lower rate of CD-TLR in our series. In the previous study, the calcified lesion was one of the predictors of primary patency [17]. The usage of the Crosser system could have had a positive effect on the calcified lesions.
There are some other atherectomy devices in addition to the Crosser system, such as excimer laser (Philips, Amsterdam, Netherlands), Rotablator (Boston Scientific, Natick, MA, USA), Turbohawk (TurboHawk, Medtronic, Minneapolis, Minnesota, USA), Jetstream (Boston Scientific, Natick, MA, USA), and Diamondback (Cardiovascular Systems, Inc., Saint Paul Hill, Minnesota, USA). The oldest atherectomy technologies are the excimer laser and the Rotablator. The excimer laser technology is based on photoablation, converting occlusive material into microbubbles immediately dissolved into the blood. Rotablator, Jetstream, and Diamondback are high speed rotational “sanding” devices mainly developed to treat highly calcified plaque. The Turbohawk system is a directional atherectomy device primarily designed for eccentric infrainguinal lesions [21]. The mechanism of the Crosser system is different from other systems. Micro-bubbles made by the high-frequency vibration of the Crosser system breaking the molecular bonds of the calcified lesion. Although there have been many reports on EVT outcomes for femoro-popliteal lesions using such atherectomy devices, there were no reports on the outcomes about the combination of atherectomy and POBA for a non-stenting zone without a drug-coated balloon or stent.
Previous studies have reported better long-term patency after surgical management of CFA disease than after EVT [22]. The patency rates in these studies were better than those in our study. However, several complications have been reported. Minor perioperative complications after CFA surgery were reported to have occurred in 6.6–17.7% of cases [5, 22]. Rates of major complications after surgical CFA revascularization requiring surgical re-intervention have been reported to range from 0 to 1.8% [5, 22]. CFA endarterectomy is also associated with complications such as lymphatic leakage and local infection. There were no large hematomas requiring blood transfusions or infections related to the procedure in our study, which is a significant advantage of EVT.
In contrast to CFA lesions, endarterectomy is rarely selected as a treatment for PA lesions due to the complexity of the surgical technique. Bypass procedures are generally performed, and the 5-year primary patency of bypass for isolated popliteal lesions has been reported as 59% (reversed saphenous vein: 74%, polytetrafluoroethylene: 55%) and secondary patency as 61% (reversed saphenous vein: 79%, polytetrafluoroethylene: 56%) [24]. In our study, the 1- and 2-year primary patency after EVT with the Crosser system for calcified PA lesions was 76.8 and 62.2%, respectively, equivalent to the patency rates reported for bypass surgery.
We have experienced only two cases of complications related to the Crosser system. In both cases, the Crosser tip was completely detached from the shaft and was successfully retrieved. A possible reason for tip separation may be differences between the size of the metal tip (1.1 mm) and that of the proximal shaft (1.3 mm). Unlike previous studies with reported complications such as slow flow and vessel perforation, we did not experience any other complications [9, 11]. In our procedures, the Crosser catheter was utilized not only with its preceding but also with a guidewire preceding, in part, due to the difficulty in making the Crosser catheter turn in specific directions when it was preceding. As a result, we have not experienced vessel perforation, which is related to the Crosser proceeding.
Data on the effects of renal insufficiency on CD-TLR, MALE, and MACE after endovascular intervention are limited. In this study, we found that hemodialysis was the only independent predictor for CD-TLR. The OLIVE (Endovascular Treatment for Infrainguinal Vessel) registry revealed that hemodialysis was associated with an unfavorable outcome for MALE in patients with CLI undergoing EVT [25]. Soga et al. reported that renal insufficiency was a predictor of primary patency in 111 treated CFA lesions [17]. Therefore, our results are consistent with those of previous studies.
Study limitations
Our study had several limitations. First, this study was a retrospective analysis of an observational cohort. Because of the absence of a surgical (endarterectomy) control group, we could not directly compare the safety and efficacy of EVT and endarterectomy. Therefore, this exploratory analysis should be interpreted as hypothesis-generating. Second, there was no systematically collected information regarding arterial patency determined by duplex sonography or angiography because those were not mandatory. Third, our study population included only Japanese individuals, which could affect the generalizability of our findings to non-Japanese patients. Fourth, the pressure gradient measured using the 4-Fr diagnostic catheter just before interventions potentially overestimated the lesion severity. Finally, we did not use IVUS in most cases; the assessment using IVUS may improve the outcomes, especially in the CTO cases.
In conclusion, EVT with a Crosser device for heavily calcified CFA and PA lesions, so-called non-stenting zones, seems to be safe and feasible. The results of this study should be confirmed in further large-scale, randomized-control studies for a better understanding of the potential advantages of the Crosser device in contemporary practice.
Data availability
The data of our study are unavailable to access because it is confidential.
References
Bhatt DL, Steg PG, Ohman EM, Hirsch AT, Ikeda Y, Mas JL, Goto S, Liau CS, Richard AJ, Röther J, Wilson PW, REACH Registry Investigators (2006) International prevalence, recognition, and treatment of cardiovascular risk factors in outpatients with atherothrombosis. JAMA 295:180–189
Baumann F, Ruch M, Willenberg T, Dick F, Do DD, Keo HH, Baumgartner I, Diehm N (2011) Endovascular treatment of common femoral artery obstructions. J Vasc Surg 53:1000–1006
Silva JA, White CJ, Quintana H, Collins TJ, Jenkins JS, Ramee SR (2004) Percutaneous revascularization of the common femoral artery for limb ischemia. Catheter Cardiovasc Interv 62:230–233
Bonvini RF, Rastan A, Sixt S, Noory E, Schwarz T, Frank U, Roffi M, Dorsaz PA, Schwarzwälder U, Bürgelin K, Macharzina R, Zeller T (2011) Endovascular treatment of common femoral artery disease: medium-term outcomes of 360 consecutive procedures. J Am Coll Cardiol 58:792–798
Ballotta E, Gruppo M, Mazzalai F, Da Giau G (2010) Common femoral artery endarterectomy for occlusive disease: an 8-year single-center prospective study. Surgery 147:268–274
Nakao M, Yamaguchi J, Otsuki H, Arashi H, Hagiwara N (2019) Clinical outcomes of high-pressure balloon angioplasty for common femoral artery disease in contemporary practice. Cardiovasc Interv Ther 34:340–344
Liang GZ, Zhang FX (2013) Novel devices and specialized techniques in recanalization of peripheral artery chronic total occlusions (CTOs)—a literature review. Int J Cardiol 165:423–429
Laird J, Joye J, Sachdev N, Huang P, Caputo R, Mohiuddin I, Runyon J, Das T (2014) Recanalization of infrainguinal chronic total occlusions with the Crosser system: results of the PATRIOT trial. J Invasive Cardiol 26:497–504
Tan M, Urasawa K, Koshida R, Haraguchi T, Kitani S, Nakagawa Y, Igarashi Y, Sato K (2018) Evaluation for the efficacy and safety of the Crosser catheter as a CTO crossing device and a flossing device. Cardiovasc Interv Ther 33:77–83
Igari K, Kudo T, Toyofuku T, Inoue Y (2016) A novel approach to infrainguinal arteries with chronic total occlusions using the high frequency vibrational device. Int Angiol 35:212–216
Khalid MR, Khalid FR, Farooqui FA, Devireddy CM, Robertson GC, Niazi K (2010) A novel catheter in patients with peripheral chronic total occlusions: a single center experience. Catheter Cardiovasc Interv 76:735–739
Gandini R, Volpi T, Pipitone V, Simonetti G (2009) Intraluminal recanalization of long infrainguinal chronic total occlusions using the Crosser system. J Endovasc Ther 16:23–27
Staniloae CS, Mody KP, Yadav SS, Han SY, Korabathina R (2011) Endoluminal treatment of peripheral chronic total occlusions using the Crosser® recanalization catheter. J Invasive Cardiol 23:359–362
Okuno S, Iida O, Shiraki T, Fujita M, Masuda M, Okamoto S, Ishihara T, Nanto K, Kanda T, Takahara M, Uematsu M (2016) Impact of calcification on clinical outcomes after endovascular therapy for superficial femoral artery disease: assessment using the peripheral artery calcification scoring system. J Endovasc Ther 23:731–737
Tsujimura T, Iida O, Fujita M, Masuda M, Okamoto S, Ishihara T, Nanto K, Kanda T, Okuno S, Matsuda Y, Fujihara M, Yokoi Y, Mano T (2018) Two-year clinical outcomes post implantation of Epic self-expanding nitinol stents for the aortoiliac occlusive disease in patients with peripheral arterial disease. J Atheroscler Thromb 25:344–349
Katsuki T, Yamaji K, Tomoi Y, Hiramori S, Soga Y, Ando K (2020) Clinical impact of improvement in the ankle-brachial index after endovascular therapy for peripheral arterial disease. Heart Vessels 35:177–186
Soga Y, Tomoi Y, Sato K, Iida O, Yokoi H (2013) Clinical outcome after endovascular treatment for isolated common femoral and popliteal artery disease. Cardiovasc Interv Ther 28:250–257
Davies RS, Adair W, Bolia A, Fishwick G, Sayers RD, McCarthy MJ (2013) Endovascular treatment of the common femoral artery for limb ischemia. Vasc Endovascular Surg 47:639–644
Semaan E, Hamburg N, Nasr W, Shaw P, Eberhardt R, Woodson J, Doros G, Rybin D, Farber A (2010) Endovascular management of the popliteal artery: comparison of atherectomy and angioplasty. Vasc Endovascular Surg 44:25–31
Rastan A, Krankenberg H, Baumgartner I, Blessing E, Müller-Hülsbeck S, Pilger E, Scheinert D, Lammer J, Beschorner U, Noory E, Neumann FJ, Zeller T (2015) Stent placement vs. balloon angioplasty for popliteal artery treatment: two-year results of a prospective, multicenter, randomized trial. J Endovasc Ther 22:22–27
Schwarzwalder U, Zeller T (2010) Debulking procedures: potential device specific indications. Tech Vasc Interv Radiol 13(1):43–53
Kang JL, Patel VI, Conrad MF, Lamuraglia GM, Chung TK, Cambria RP (2008) Common femoral artery occlusive disease: contemporary results following surgical endarterectomy. J Vasc Surg 48:872–877
Kechagias A, Ylonen K, Biancari F (2008) Long-term outcome after isolated endarterectomy of the femoral bifurcation. World J Surg 32:51–54
Kram HB, Gupta SK, Veith FJ, Wengerter KR, Panetta TF, Nwosisi C (1991) Late results of two hundred seventeen femoropopliteal bypasses to isolated popliteal artery segments. J Vasc Surg 14:386–390
Iida O, Nakamura M, Yamauchi Y, Kawasaki D, Yokoi Y, Yokoi H, Soga Y, Zen K, Hirano K, Suematsu N, Inoue N, Suzuki K, Shintani Y, Miyashita Y, Urasawa K, Kitano I, Yamaoka T, Murakami T, Uesugi M, Tsuchiya T, Shinke T, Oba Y, Ohura N, Hamasaki T, Nanto S, OLIVE Investigators (2013) Endovascular treatment for infrainguinal vessels in patients with critical limb ischemia: OLIVE registry, a prospective, multicenter study in Japan with 12-month follow-up. Circ Cardiovasc Interv 6:68–76
Acknowledgements
We thank Editage (www.editage.jp) for the English language editing.
Funding
This research received no grant from any funding agency in public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. AEH and MN performed material preparation, data collection, and analysis. The first draft of the manuscript was written by AEH, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
Junichi Yamaguchi and Hisao Otsuki belong to the division (Clinical Research division for Cardiovascular Catheter Intervention) financially maintained by the donation from Abbott Vascular, Boston Scientific, Medtronic Terumo. The other authors declare that they have no conflict of interest.
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by the institutional ethics committee of Tokyo Women’s Medical University Hospital (No 3502-R).
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hassan, A.E., Nakao, M., Katsumata, H. et al. Clinical outcomes after balloon angioplasty with Crosser device for heavily calcified common femoral and popliteal artery disease. Heart Vessels 36, 1359–1365 (2021). https://doi.org/10.1007/s00380-021-01816-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-01816-z