Abstract
Background
Long-term outcome after endarterectomy of the femoral bifurcation has not been widely investigated, and the aim of this study was to assess its late results from a community-wide perspective.
Patients and Methods
Between 1983 and 2006 111 isolated endarterectomies of the common femoral artery and/or the proximal part of the superficial femoral artery or profunda femoris were performed in 90 patients at the Oulu University Hospital, Oulu, Finland. A total of 77 limbs were treated surgically for claudication and 34 others for critical limb ischemia. Angiographic findings of 100 extremities were evaluated.
Results
The in-hospital mortality rate was 1.8%. The mean follow-up period was 5.9 years. At 5-, 10-, and 15-year follow-up the overall survival was 60.5%, 32.7%, and 17.6%, respectively (S.E < 0.05). A C-reactive protein value ≥ 10 mg/l was predictive of poor late survival (p = 0.008). Limb salvage rates after isolated femoral endarterectomy at 5-, 10-, and 15-year follow-up were 93.7%, 93.7%, and 85.2%, respectively (S.E. < 0.08). Critical limb ischemia (p = 0.006) and current smoking (p = 0.027) were independent predictors of major lower limb amputation. A total of 41 limbs were subjected to ipsilateral vascular procedures after femoral endarterectomy, only one of which was re-endarterectomy. Freedom from any ipsilateral revascularization procedure at 5-, 10-, and 15-year follow-up was calculated at 68.0%, 50.6%, and 42.5%, respectively (S.E. < 0.08). The overall linearized rate of reintervention on the ipsilateral limb was 0.16 ± 0.44/year. The linearized rate among patients who had any ipsilateral vascular reintervention was 0.43 ± 0.66/year.
Conclusions
Isolated femoral endarterectomy is a rather low-risk and durable procedure. However, a significant number of reinterventions distal or proximal to the endarterectomized site can be expected in one third of patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Thromboendarterectomy for treatment of lower limb ischemia was introduced in the 1940s [1] and was later replaced by bypass surgery, among other endovascular procedures. Isolated endarterectomy of the common femoral artery and its branches is still performed for treatment of lower limb claudication, and to some extent, for critical limb ischemia (CLI). According to the Finnish Vascular Registry (Finnvasc), femoral endarterectomy has been performed in about 12% of patients undergoing infrainguinal surgical revascularization for CLI [2]. When associated with profundoplasty, the procedure is often indicated in high-risk patients, in cases of previous failed bypass surgery, or in the case of an infected graft.
Although femoral endarterectomy has been widely performed during the last 6 decades, its related long-term outcome has not been extensively investigated. The present report reflects a retrospective community-wide analysis of the long-term results after isolated endarterectomy of the femoral bifurcation.
Patients and methods
From January 1983 to May 2006, 111 isolated endarterectomies of the femoral bifurcation were performed at the Oulu University Hospital, Oulu, Finland, in 90 consecutive patients who were residents in an area close to Oulu (range of about 50 km). Our institution is a tertiary referral center for cardiothoracic and vascular surgery. Patients residing in this area are referred to us for any surgical/endovascular revascularization procedure, as well as minor and major amputation. Data were collected retrospectively from records including files of all departments of this hospital.
This study included patients who underwent endarterectomy of the common femoral artery and/or endarterectomy of the proximal part of the profunda femoris as well as of the superficial femoral artery, with or without patch angioplasty. Patients who underwent additional simultaneous vascular procedures on the same limb as well as isolated endarterectomy of the superficial femoral artery (other than its ostial segment) were excluded from this study.
Claudication was the indication for isolated femoral endarterectomy in 77 cases, and critical limb ischemia in 34 cases. Preoperative clinical data are reported in Table 1. In nineteen cases (17%), patients had previously undergone an ipsilateral infrainguinal revascularization procedure. Among these, an endovascular procedure was performed 14 cases, and bypass surgery in 4 cases. Four procedures (3.6%) were redo operations.
Preoperative angiographies were available for review in 100 cases, and angiographic findings were categorized according to the Revised Recommended Standards for Reports Dealing with Lower Extremity Ischemia [3]. The status of the pedal arch was not evaluated in this study because of missing images or poor visualization in the available angiographic studies. According to the angiographic findings of the superficial femoral artery, a stenosis >50% was present in 30 cases (30%), an occlusion of the artery of less than half of length in 6 (6%), and occlusion through the entire length in 19 (19%). Ankle/brachial index values were available for review in 90 cases, and the mean value was 0.54 ± 0.30.
The endarterectomy involved the common femoral artery in 100 cases, the proximal part of the superficial femoral artery in 29 cases, and the deep femoral artery in 39 cases. In 16 patients femoral endarterectomy was performed simultaneously on both sides. A patch was used in 89 procedures: a prosthesis patch was used in 45 cases, a vein patch in 40, and an arterial patch derived from the ipsilateral superficial femoral artery in 4.
Because a program to evaluate the patency of the treated arterial segment during such a long follow-up period was not available in our institution, we could not evaluate the patency of the endarterectomized vessels as an outcome endpoint. Date of death in these patients has been retrieved from our institutional database. To summarize the incidence of multiple re-interventions among these patients, the linearized rate was calculated as the number of events divided by the total patient-years.
Statistical analysis
Statistical analysis was performed using SPSS statistical software (SPSS v. 12.0.1, SPSS Inc., Chicago, IL, USA). Continuous variables are reported as the mean ± standard deviation. Correlation between continuous variables was estimated by the Spearman rank test. The Kaplan-Meier test and Cox regression method were used for univariate and multivariate analysis. Only variables with a p < 0.05 were included into the regression model. A value of p < 0.05 was considered statistically significant.
Results
The in-hospital mortality rate in this series was 1.8% (these two patients had a Finnvasc score of 3 and 4, respectively). One patient died of myocardial infarction and the other of sepsis and multiple systemic complications related to metastatic cancer of the pancreas.
Wound infection occurred in 19 cases (17.1%), hematoma in 10 (9.0%), seroma in 6 (5.4%), myocardial infarction in 1 (0.9%), acute renal failure in 2 (1.8%), early femoral thrombosis in 2 (1.8%), and early distal embolism in 1 (0.9%). Surgical revision for wound complication was performed in two cases. In one of these cases vein patching was performed at the time of reoperation for hemostasis.
Late survival
The mean follow-up period was 5.9 years. At 5-, 10-, and 15-year follow-up the overall survival was 60.5%, 32.7%, and 17.6%, respectively (S.E. < 0.05). At univariate analysis, foot gangrene (p < 0.0001), diabetes (p = 0.027), coronary artery disease (p = 0.010), C-reactive protein ≥ 10 mg/dl (p = 0.001), patient’s age (p < 0.0001), serum creatinine (p = 0.001), overall infrainguinal angiographic score (p = 0.038), and the angiographic score (p = 0.018) were predictors of late survival. When all these risk factors, were included into the Cox regression model (76 patients with complete data), only C-reactive protein ≥ 10 mg/l was an independent predictor of late mortality (p = 0.008, HR 2.52, 95% CI 1.27–5.01). C-reactive protein ≥ 10 mg/l was significantly associated with the severity of ischemia (claudication: 17%; rest pain: 50%; ulcer: 75%; and gangrene: 100%; p < 0.0001), Finnvasc score classes (0: 4%; 1: 31%; 2: 33%; and 3: 80%; p = 0.003), patient’s age (p = 0.02), ankle/brachial indexes (p < 0.0001), and preoperative serum creatinine (p = 0.003).
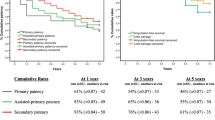
Limb salvage
Limb salvage rates after isolated femoral endarterectomy at 5-, 10-, and 15-year follow-up were 93.7%, 93.7%, and 85.2%, respectively (S.E. < 0.08). At univariate analysis, Finnvasc score > 2 (p < 0.0001), critical limb ischemia (p = 0.001, along with foot gangrene: p < 0.0001), current smoking (p = 0.026), and overall infrainguinal angiographic score (p < 0.0001), as well as crural angiographic score (p = 0.005), were predictors of late major lower limb amputation. The angiographic score was not predictive of late major lower limb amputation at univariate analysis (p = 0.11). Multivariate analysis failed to reveal any independent predictor of major amputation. However, when angiographic score was excluded from the analysis, thus extending the analysis to 109 cases, critical limb ischemia (p = 0.006, HR 19.81, 95% CI 2.32–168.81; Fig. 1) and current smoking (p = 0.027, HR 11.06, 95% CI 1.31–93.15) were found to be independent predictors of major lower limb amputation.
Need of further ipsilateral revascularization procedures
During follow-up, a total of 78 surgical and endovascular revascularization procedures have been performed on 41 extremities after isolated femoral endarterectomy. Twenty-two (19.8%) were infrainguinal procedures, 10 were aortoiliac (9.0%), and in 9 cases both aortoiliac and infrainguinal procedures were performed (8.1%). In 6 cases, reoperation was done for femoral pseudoaneurysm. Data on these procedures are reported in detail in Table 2.
Most of late aortoiliac-femoral revascularization procedures for ipsilateral lesions were endovascular. Among surgical revascularization procedures, there were three aortoiliac-femoral bypass reconstructions and two femoro-femoral crossover bypasses. Of 17 patients with available angiographic studies for review among 19 who had late aortoiliac-femoral revascularization, there were 2 cases of stenosis > 50% of the ipsilateral common iliac artery and 3 of stenosis of the external iliac artery. The others had no stenoses or a stenosis < 50%. One patient underwent redo endarterectomy of the femoral bifurcation because of severe restenosis of the common femoral artery.
Freedom from late revascularization procedure on the ipsilateral limb at 5-, 10- and 15-year follow-up was calculated at 68.0%, 50.6%, and 42.5%, respectively (S.E. < 0.08). Preoperative serum creatinine was predictive of late ipsilateral revascularization (p = 0.026), and critical limb ischemia tended to be associated with an increased risk of late revascularization (p = 0.053). The overall linearized rate of reintervention on the ipsilateral limb was 0.16 ± 0.44/year. The linearized rate among patients who had any ipsilateral vascular reintervention was 0.43 ± 0.66/year. No risk factors were associated with an increased risk of linearized rate of late revascularization. Preoperative serum creatinine was significantly correlated with linearized rate of ipsilateral revascularization (ρ = 0.198, p = 0.043).
Impact of the angiographic status of the femoropopliteal segment on outcome
The revised angiographic score of the superficial femoral artery and profunda was predictive of late survival (p = 0.018), but not of major amputation or reoperation. The presence of any occlusion of the femoropopliteal segment (angiographic score > 2) was not significantly associated with late adverse outcome.
Discussion
This study confirmed that isolated femoral endarterectomy is an effective procedure associated with satisfactory late results. Even if it can be considered a minor procedure in terms of extent, it is nevertheless associated with some degree of mortality and morbidity. A few studies reported early postoperative mortality rates up to 1% [4–6]. However, in a Finnvasc registry study dealing with patients with CLI, the immediate postoperative mortality was 2.7% [2], which is similar to our experience.
Cardon et al. [5] reported late survival rates similar to those of our study (88%, 67.7%, and 36.7% at 2-, 5-, and 10-years of follow-up, respectively), which suggests that the expectancy of life in these patients is rather limited. Interestingly, our study showed that a preoperative value of the C-reactive protein ≥ 10 mg/l is an independent predictor of overall survival after isolated femoral endarterectomy. This is in accord with the findings of previous studies showing a major prognostic impact of preoperative C-reactive protein after lower limb revascularization [7] and coronary artery revascularization [8, 9].
Because of the lack of a specific follow-up program on such a long term, we do not have data on long-term patency. However, previously reported patency rates ranged from 74% to 89% at 5 years [5, 6], and Mukherjee and Inahara [4] reported a 10-year patency of about 94%.
The observed limb salvage rates in our study at 10- and 15-years of 94% and 85%, respectively, as well as a rate of 92% at 5 years reported by Cardon et al. [5], suggest that isolated femoral endarterectomy is an effective and durable procedure. Its efficacy is not limited by the coexistence of an occlusion of the femoropopliteal segment, as results at 10–15 years are similar to those of patients with better femoropopliteal angiographic run-off.
Finally, it is important to mention that such good long-term results after femoral endarterectomy have been achieved with a rather significant number of aortoiliac and infrainguinal revascularization procedures in about 37% of our patients. The need of various surgical or endovascular procedures done proximal or distal to the site involved by atherosclerosis suggests the multisegmental character and progressive nature of occlusive disease of the lower limb [10].
In conclusion, isolated femoral endarterectomy is a rather low-risk and durable procedure. However, a significant number of reinterventions distal or proximal to the endarterectomized site are to be expected in one third of patients.
References
Dos Santos JC (1947) Sur la desobstruction des thromboses arterielles anciennes. Mem Acad Chir 73:409–411
Biancari F, Salenius JP, Heikkinen M, et al. (2007) Risk-scoring method for prediction of 30-day postoperative outcome after infrainguinal surgical revascularization for critical lower-limb ischemia: a Finnvasc registry study. World J Surg 31:217–225
Rutherford RB, Baker JD, Ernst C, et al. (1997) Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg 26:51–538
Mukherjee D, Inahara T (1989) Endarterectomy as the procedure of choice for atherosclerotic occlusive lesions of the common femoral artery. Am J Surg 122:498–500
Cardon A, Aillet S, Jarno P, et al. (2001) Endarterectomy of femoral tripod: long-term results and analysis of predictive factors of failure. Ann Chir 126:777–782
Springhorn ME, Kinney M, Littooy FN, et al. (1991) Inflow atherosclerotic disease localized to the common femoral artery: treatment and outcome. Ann Vasc Surg 5:234–240
Barani J, Nilsson JA, Mattiasson I, et al. (2005) Inflammatory mediators are associated with 1-year mortality in critical limb ischemia. J Vasc Surg 42:75–80
Kangasniemi OP, Biancari F, Luukkonen J, et al. (2006) Preoperative C-reactive protein is predictive of long-term outcome after coronary artery bypass surgery. Eur J Cardiothorac Surg 29:983–985
Palmerini T, Marzocchi A, Marrozzini C, et al. (2005) Preprocedural levels of C-reactive protein and leukocyte counts predict 9-month mortality after coronary angioplasty for the treatment of unprotected left main coronary artery stenosis. Circulation 112:2332–2338
Veith FJ, Gupta SK, Wengerter KR, et al. (1990) Changing arteriosclerotic disease patterns and management strategies in lower-limb-threatening ischemia. Ann Surg 212:402–412
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kechagias, A., Ylönen, K. & Biancari, F. Long-term Outcome after Isolated Endarterectomy of the Femoral Bifurcation. World J Surg 32, 51–54 (2008). https://doi.org/10.1007/s00268-007-9309-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00268-007-9309-7