Abstract
Fenestration closure is considered to remove the persistent right-to-left shunt after the Fontan operation. However, the criteria for effective transcatheter closure of fenestration to avoid both acute and chronic Fontan failure have not been clarified. The objective of this study was to describe the hemodynamic data with test occlusion of the Fontan fenestration for patients who underwent a closure and those who did not, along with subsequent development of Fontan-associated diseases (FAD) at follow-up. This was a retrospective study conducted to assess the outcome of Fontan fenestration closure at Children’s Hospital of Michigan over 27 years (1993–2019). The inclusion criteria were patients undergoing cardiac catheterization indicated for Fontan fenestration closure. Data were compared between the two groups: closure and non-closure patients. Baseline characteristics and hemodynamic variables with the fenestration occlusion test were analyzed. The primary outcome was the development of composite events of death/transplant, deteriorated New York Heart Association class symptoms, or FAD. Among the 38 patients who were brought to the catheterization laboratory, 33 received fenestration closure and 5 did not. On a median follow-up of 3.4 years (range, 1 month–12.6 years), the incidence of primary adverse outcomes was 13% (5/38). The incidence of primary outcome was significantly higher in the non-closure group (60% vs. 6%, p < 0.01). The non-closure group had a higher incidence of moderate or severe atrioventricular valve regurgitation, New York Heart Association class III symptoms, use of angiotensin-converting enzyme inhibitor/angiotensin receptor blocker, furosemide use, and sildenafil use. The multivariable logistic regression model showed that the hemodynamic variables associated with the non-closure group were mean left atrial pressure (odds ratio 1.74, p < 0.05) and change of mean Fontan pressure at the balloon occlusion (odds ratio 2.2, p < 0.05). The judgment of fenestration closure appeared appropriate in our cohort. Fontan fenestration closure may not be advisable in cases with a high baseline left atrial pressure or a significant increase in Fontan pressure on balloon occlusion testing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The creation of a fenestration during the Fontan operation has been shown to improve the early postoperative course and shorten the length of hospital stay [1]. Fontan fenestration may persist over years and cause systemic desaturation and exertional dyspnea due to a persistent right-to-left shunt, with an increase in the risk of thromboembolic events and brain abscess. Therefore, transcatheter device closure of the fenestration is often considered after Fontan operation. Although fenestration closure increases systemic saturation, previous reports have not shown clear benefits in exercise capacity and functional status [2, 3]. Spontaneous fenestration closure may indicate good Fontan physiology and a favorable clinical outcome, whereas persistent fenestration can be an indicator of physiologic intolerance and Fontan-associated diseases and mortality [4, 5]. Although late fenestration patency may suggest the physiological necessity of a fenestration, there is a concern that intentional fenestration closure may lead to worse clinical outcomes over time. Though previous reports exist on the patients’ eligibility criteria for safe and effective fenestration closure over short follow-up periods, there is a paucity of data on the eligibility criteria over a longer follow-up period. Our hypothesis was that certain clinical factors and catheterization data would predict successful fenestration closure. The objective of this study was to describe the hemodynamic data with test occlusion of the Fontan fenestration and compare them between closure and non-closure patients, along with subsequent development of Fontan-associated diseases at follow-up. Based on our study results and a review of the literature, the optimal criteria for Fontan fenestration closure have been discussed.
Materials and methods
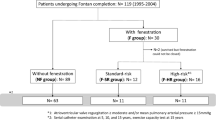
This was a retrospective study conducted at the Children’s Hospital of Michigan and approved by the Institutional Review Board of Wayne State University School of Medicine. The study included patients who were brought to the cardiac catheterization laboratory for an indication of fenestration closure at least 6 months after the Fontan operation, which was conducted during the study period of 27 years (1993–2019). The cardiac catheterization database was used to identify eligible patients. The exclusion criterion was significant pulmonary arteriovenous malformation. The study cohort was divided into two groups: fenestration closure group and non-closure group. Data on demographics, cardiac diagnosis, clinical symptoms, comorbidities, surgical history, history of hospitalization, medications, and follow-up were collected from the medical records. The primary adverse outcomes were the development of any of the following: first incidence of Fontan-associated diseases including protein-losing enteropathy and plastic bronchitis, progression to the New York Heart Association (NYHA) class III/IV symptoms, heart transplant, or death. Protein-losing enteropathy was defined as the presence of at least one clinical symptom (peripheral edema, diarrhea, abdominal pain, or effusions within the pericardial or pleural space) and one laboratory abnormality, such as elevated fecal alpha-1 antitrypsin clearance (> 50 mL/24 h), elevated spot fecal alpha 1 antitrypsin concentration (> 100 mg/mL) or serum albumin (< 3.0 g/dL) [6]. Plastic bronchitis was defined as the identification of casts in the airway tract.
Cardiac catheterization and fenestration device closure
For fenestration closure, cardiac catheterizations were performed in room air under general anesthesia and mechanical ventilation. All patients underwent a baseline hemodynamic study and balloon test occlusion of the Fontan fenestration before consideration of fenestration closure. The use of contrast was minimized prior to fenestration closure. Temporary occlusion of the Fontan fenestration was achieved by the use of balloon-tip catheters for 10–15 min. Adequate occlusion was confirmed by low-contrast angiography (Fig. 1a). The decision to close the fenestration was based on the baseline and test occlusion hemodynamics at the discretion of individual operators. The devices to close the fenestration included Amplatzer septal occluder (Abbott, Abbott Park, IL, USA; Fig. 1b), Amplatzer cribriform occluder (Abbott), CardioSEAL septal occluder (Nitinol Medical Technologies, Inc., Boston, MA, USA), and the Cheatham Platinum stent (B. Braun Medical Inc., Bethlehem, PA, USA). After device closure, aspirin was administered for at least 6 months. Systemic oxygen transport (SOT) was obtained as a marker of tissue oxygenation [6]. SOT (in mL of oxygen per minute per square meter) was calculated using the following formula: SOT = cardiac index × arterial blood oxygen concentration (1.34 × hemoglobin [Hb] × [SaO2 × 0.01]) × 10. The dissolved oxygen component was not included because its contribution was deemed negligible.
Review of literature
Regarding the hemodynamic criteria for the Fontan fenestration closure, the literature was searched in PubMed using the following keywords: “fenestration,” “fenestrated,” “interatrial communication,” “closure,” “occlusion,” “percutaneous,” “transcatheter,” and “Fontan.” Original articles describing hemodynamic criteria and having a sample size of ≥ 10 were included. Follow-up data were extracted with a particular focus on unfavorable outcomes after closure.
Statistical analyses
Data are expressed as median with range, mean with standard deviation, and number with frequency based on the type and distribution of data. Data were compared between the two groups (closure vs. non-closure) using the Chi-square test, independent t test, or Mann–Whitney U test. Data were compared between patients using a paired sample t test or Wilcoxon signed rank test. Factors showing significant univariate associations (p < 0.05) with non-closure were then included in multivariable logistic regression along with the backward selection method. The Kaplan–Meier product-limit method and Cox proportional hazards regression were used to analyze the freedom from the primary outcome after cardiac catheterization to examine the association of all potential factors with the primary outcome. Statistical analyses were performed using SPSS version 26 (IBM SPSS Inc., Chicago, IL, USA). A p value < 0.05 was considered statistically significant.
Results
Patient characteristics
The study cohort consisted of 38 patients who underwent cardiac catheterization for an indication of Fontan fenestration closure. The patient demographics were as follows: females (n = 23, 61%), African Americans (n = 11), Caucasians (n = 13), and others (n = 14); median age of 6.2 years (range, 2.8–40.9 years). Most patients had low oxygen saturation, with a mean of 87 ± 6%. The most frequent underlying cardiac diagnosis was hypoplastic left heart syndrome (37%). Single ventricular morphology was right-ventricle dominant (n = 19) and left ventricle dominant or bi-ventricle (n = 19). Heterotaxy was present in four patients. The most frequent first palliation was the Norwood/Daymus–Kaye–Stancel procedure (n = 13, 34%), followed by pulmonary artery banding (n = 8), systemic-pulmonary shunt (n = 11), and none (n = 6). A majority (n = 32, 84%) of patients underwent a bidirectional Glenn procedure or Hemi-Fontan procedure. The types of Fontan were lateral tunnel (n = 25), extracardiac Fontan (n = 11), and atriopulmonary connection (n = 2). The median age at the Fontan operation was 2.5 years (range, 1.4–9.9 years). Five patients had pacemaker implants. Most patients (92%) had normal or mildly reduced ventricular systolic function, whereas three patients had moderately or severely reduced function. Six patients (16%) had moderate or more atrioventricular valve regurgitation. The mean gradient across patent fenestration was 6.3 ± 2.0 mmHg. The most common indication for fenestration closure was cyanosis (n = 23, 61%), followed by exercise intolerance (n = 9, 24%). Two-thirds of the patients were on anti-platelet or anti-coagulation medications (aspirin [n = 22], warfarin [n = 2], and rivaroxaban [n = 1]). Other medications included angiotensin-converting enzyme inhibitor (ACEI)/angiotensin receptor blockers (ARBs) (n = 18), furosemide (n = 9), sildenafil (n = 4), digoxin (n = 3), spironolactone (n = 2), beta blockers (n = 2), and anti-arrhythmic agents (n = 1).
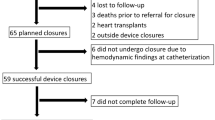
Transcatheter fenestration device closure
The median age at catheterization was 6.0 years (range, 2.8–40.9 years), with a weight of 22.0 kg (range, 14.0–71.5 kg). The duration between the Fontan operation and cardiac catheterization was 3.6 years (range, 7–33 years). Fontan fenestration was closed in 33 patients, whereas it was left remained open in five patients. The devices to close the fenestration included an Amplatzer septal occluder (n = 25), Amplatzer Cribriform occluder (n = 4), CardioSEAL septal occluder (n = 2), and the Cheatham Platinum stent (n = 2). Device closure was successful for all patients without any significant adverse events. Systemic oxygen saturation increased by 7.2 ± 5.7% (p < 0.001) after closure. All patients were discharged the next day after satisfactory device position was documented on transthoracic echocardiography. After closure, additional diuretic medications were needed in three patients due to peripheral edema but were shortly discontinued.
Fenestration closure versus non-closure
The non-closure group was more likely to have NYHA class III symptoms, be on sildenafil, ACEI/ARBs, and furosemide, and had significant atrioventricular valve regurgitation (Table 1). All patients underwent baseline hemodynamic studies and balloon occlusion tests of the fenestration during catheterization. At baseline, the non-closure group had a higher mean left atrial pressure, lower systemic oxygen saturation, and lower SOT (Table 2). With the balloon occlusion test, all patients showed an increase in systemic oxygen saturation by 5.9 ± 4.7% (p < 0.001), an increase in mean Fontan pressure by 1.4 ± 1.4 mmHg (p < 0.001), a decrease in cardiac index by 0.5 ± 1.2 L/min/m2 (p = 0.01), and a decrease in SOT by 55 ± 185 mL/min/m2 (p = 0.005), whereas systemic venous oxygen saturation did not change. Balloon occlusion test caused a higher increase in the mean Fontan pressure in the non-closure group (2.6 mmHg vs. 1.3 mmHg, p = 0.042). In the final multivariable logistic regression model (Table 3), the hemodynamic variables that were significantly associated with non-closure were higher left atrial pressure at baseline (odds ratio, 1.74; 95% confidence interval [CI] 1.04–2.92; p = 0.032) and increase in Fontan pressure in the balloon occlusion test (odds ratio, 2.16; 95% CI 1.03–4.55; p = 0.043). In the non-closure group, closure was deferred because of either high Fontan pressure with balloon occlusion test ≥ 20 mmHg, a rise in Fontan pressure by ≥ 4 mmHg, a decrease in cardiac output by ≥ 50%, or a decrease in SOT by ≥ 46% (Supplementary Table).
Follow-up and primary outcome
During a median follow-up period of 3.4 years (range, 1 month–12.6 years), the incidence of primary adverse outcomes was 13% (5/38), with a mortality rate of 5% (2/38). The incidence of primary adverse outcomes was significantly higher in the non-closure group (60% vs. 6%, p = 0.01, Fig. 2). From the baseline patient characteristics, the factors significantly associated with the development of primary adverse outcomes by univariate analysis were non-closure of fenestration, use of sildenafil, longer hospital stay after the Fontan operation, and abnormal ventricular systolic function (Table 4). In the cardiac catheterization data, the significant factors were higher mean left atrial pressure, higher ventricular end-diastolic pressure, higher Fontan pressure, cardiac index, and SOT at baseline, and lower systemic oxygen saturation and higher Fontan pressure after the balloon occlusion test. Multivariable analysis did not show statistical significance in any hemodynamic variables after accounting for fenestration closure, likely due to the small sample size in the non-closure group.
Detailed hemodynamic data for each patient are detailed in the Supplemental Table. In the fenestration closure group, two patients had a primary adverse outcome during the follow-up period. In these two patients, balloon occlusion testing increased the Fontan pressure by 7 mmHg and 3 mmHg, (resulting in final Fontan pressures of 16 mmHg and 17 mmHg), decreased cardiac index by 41% and 55%, and decreased SOT by 27% and 52%, respectively.
Discussion
The decision to close or leave the fenestration open at the catheterization appeared appropriate in our patients’ group because the closure group had a very low incidence of Fontan-associated disease, heart transplant, or death, while the non-closure group had a high incidence of these outcomes. Fenestration closure was likely to be deferred in patients with significant atrioventricular valve regurgitation, NYHA class III symptoms, and those on medications for heart failure. At the time of cardiac catheterization, the significant hemodynamic variables associated with the decision of non-closure were higher left atrial pressure at baseline and higher Fontan pressure on balloon occlusion testing. Elevated left atrial pressure indicates the presence of ventricular diastolic dysfunction, and a high Fontan pressure would not bode a favorable long-term outcome.
In the univariate analysis, several clinical and hemodynamic variables were found to be significant predictors of primary adverse outcomes. These variables are the use of sildenafil, abnormal ventricular systolic function, elevated left atrial pressure, elevated end-diastolic pressure, and elevated Fontan pressure. This shows that abnormal ventricular systolic function with elevated Fontan pressure is an important factor for poor outcomes. Interestingly, a high cardiac index was also a significant predictor of the primary outcome. This may imply that the existence of a right-to-left shunt at the fenestration increases cardiac output and can be a risk factor for a worse outcome. Even years after the Fontan operation, fenestration may be necessary to augment cardiac output and decompress systemic venous pressure in some patients. Because fenestration closure potentially leads to adverse outcomes, clinical judgment to close or leave the fenestration open is important.
The hemodynamic criteria for safe and effective Fontan fenestration closure remain unclear. The 2011 scientific statement from the American Heart Association delivered recommendations for transcatheter closure of Fontan fenestrations (Class IIa; Level of Evidence, C) as follows: “It is reasonable to consider transcatheter closure of a chronic (outside of the immediate postoperative period) Fontan fenestration if the patient has favorable hemodynamics and tolerates test occlusion” [8]. Acceptable hemodynamics with temporary fenestration occlusion were defined as improved systemic oxygen saturation associated with only a modest rise in Fontan pressure or fall in cardiac output. As shown in our cohort, balloon occlusion testing increased the Fontan pressure and decreased the cardiac output. However, the question remains as to what extent of change is acceptable in each of these cases.
A review of the literature (Table 5) was performed regarding the transcatheter closure of Fontan fenestration [7, 9,10,11,12,13,14,15,16,17,18]. Hemodynamic criteria were defined arbitrarily and differed between institutions. Fenestration closure was undertaken without subsequent adverse outcomes in the majority of the patients during the follow-up period, whereas the incidence of developed protein-losing enteropathy, plastic bronchitis, worsening heart failure, pleural effusion, or ascites after fenestration closure ranged between 0 and 17% in the different institutions, with an overall incidence rate of 6% (n = 35/585). The overall outcome was the same percentage of adverse outcomes found in our fenestration closure group. In these reports, Pihkala et al. [12] reported 152 cases who attempted to close the fenestration with the lowest incidence of poor outcome (1.3%) and the longest follow-up period (median 4.5 years). Their criteria for closure were as follows: ≤ 4 mmHg of rise in Fontan pressure and ≤ 10% decrease in mixed venous saturation.
Most studies focused only on hemodynamic data during cardiac catheterization to judge the candidacy of fenestration closure. However, the baseline clinical factors are important and should be taken into consideration for decision making. In a study of 47 patients undergoing Fontan fenestration closure, 8 patients developed heart failure symptoms [17]. These patients were more likely to be on digoxin, sildenafil, or ACEI/ARB, and had systolic ventricular dysfunction on echocardiography prior to the closure. Similarly, our study showed that the use of sildenafil, furosemide, and moderate to severe atrioventricular valve regurgitation were more frequent in the non-closure group. Additionally, the use of sildenafil and abnormal systolic ventricular function were associated with the development of the primary adverse outcomes. Fenestration closure may not be wise in the presence of these clinical risk factors, even if the hemodynamic data are marginally acceptable at catheterization.
One of the important long-term complications associated with Fontan circulation is lymphatic system issue (i.e., protein-losing enteropathy and plastic bronchitis). Recent studies have shown the etiology of Fontan associated lymphatic disorders being the combination of the congenital lymphatic anatomical variant and elevated central venous pressure [19, 20]. Fenestration closure certainly increases central venous pressure and possibly facilitates the development of this devastating complications in patients with unfavorable lymphatic variants. Magnetic resonance lymphatic imaging may play an important role on identifying the patients who would be at risk for the lymphatic disorders and be used as a tool for judging the candidacy of fenestration closure.
To discuss the criteria for Fontan fenestration closure, an increase in Fontan pressure at balloon occlusion test was adopted because it was significantly smaller in the closure group. Hemodynamic data of the participants of the closure group with primary outcome (in the present study) and Pihkala’s criteria were also referred. Furthermore, clinical variables were added based on our results and previous reports [17]. Thus, the following are taken at our institution as criteria for acceptable hemodynamics and clinical factors for Fontan fenestration closure:
-
1.
Balloon occlusion test:
-
i.
Fontan pressure ≤ 17 mmHg.
-
ii.
≤ 2 mmHg increase in Fontan pressure.
-
iii.
≤ 40% decrease in cardiac output.
-
iv.
≤ 30% decrease in systemic oxygen transport.
-
v.
≤ 10% decrease in mixed venous saturation.
-
i.
-
2.
Fenestration closure should be considered with caution in patients with NYHA class III or IV, concurrent need of heart failure medications (sildenafil, furosemide and digoxin), moderate to severe atrioventricular valve regurgitation, or moderate to severe ventricular systolic dysfunction on echocardiography.
Limitations
This was a retrospective study with an inherent limitation of generalizability. The data on follow-up outcomes were limited in some patients because our center is a referring hospital. The sample size was small, which led to a lower statistical power of the study. In addition, the incidence of the primary adverse outcomes was low at 6% (2/33) in the fenestration closure group. As a result, multivariable analysis was not feasible to evaluate the significant hemodynamic variables associated with the development of the primary adverse outcomes after accounting for fenestration closure. The decision to close or leave the fenestration open was at the discretion of the operators, and two patients with Fontan pressure of 19 mmHg at the test occlusion still went on to undergo fenestration closure. A prospective and multi-center study with a large sample size is warranted to evaluate the optimal timing for and to test these hemodynamic recommendations for fenestration closure.
Conclusion
The decision to close or leave the fenestration in Fontan patients appeared appropriate in our cohort. Fontan fenestration may not be wise in patients with a high baseline left atrial pressure or a significant increase in Fontan pressure on the balloon occlusion test.
The optimal criteria for safe fenestration closure were discussed, based on our results and those of previous studies. Further accumulation of these cases is needed to clarify the safer eligibility criteria for Fontan fenestration closure.
References
Lemler MS, Scott WA, Leonard SR, Stromberg D, Ramaciotti C (2002) Fenestration improves clinical outcome of the fontan procedure: a prospective, randomized study. Circulation 105:207–212
Meadows J, Lang P, Marx G, Rhodes J (2008) Fontan fenestration closure has no acute effect on exercise capacity but improves ventilatory response to exercise. J Am Coll Cardiol 52:108–113
Momenah TS, Eltayb H, Oakley RE, Qethamy HA, Faraidi YA (2008) Effects of transcatheter closure of Fontan fenestration on exercise tolerance. Pediatr Cardiol 29:585–588
Kotani Y, Chetan D, Saedi A, Saedi A, Zhu J, Grosse-Wortmann L, Coles JG, Caldarone CA, Arsdell GSV, Honjo O (2014) Persistent fenestration may be a marker for physiologic intolerance after Fontan completion. J Thorac Cardiovasc Surg 148:2532–2538
Garekar S, Walters HL, Delius RE, Thomas RL, Ross RD (2006) Intermediate outcomes of fenestrated Fontan procedures. J Thorac Cardiovasc Surg 131:247–249
John AS, Johnson JA, Khan M, Driscoll DJ, Warnes CA, Cetta F (2014) Clinical outcomes and improved survival in patients with protein-losing enteropathy after the Fontan operation. J Am Coll Cardiol 64:54–62
Hijazi ZM, Fahey JT, Kleinman CS, Kopf GS, Hellenbrand WE (1992) Hemodynamic evaluation before and after closure of fenestrated Fontan. An acute study of changes in oxygen delivery. Circulation 86:196–202
Feltes TF, Bacha E, Beekman RH III, Cheatham JP, Feinstein JA, Gomes AS, Hijazi ZM, Ing FF, Moor M, Morrow WR, Mullins CE, Taubert KA, Zahn EM, American Heart Association Congenital Cardiac Defects Committee of the Council on Cardiovascular Disease in the YoungCouncil on Clinical Cardiology, Council on Cardiovascular Radiology and Intervention, American Heart Association (2011) Indications for cardiac catheterization and intervention in pediatric cardiac disease: a scientific statement from the American Heart Association. Circulation 123:2607–2652
Bridges ND, Lock JE, Mayer JE Jr, Burnett J, Castaneda AR (1995) Cardiac catheterization and test occlusion of the interatrial communication after the fenestrated Fontan operation. J Am Coll Cardiol 25:1712–1717
Goff DA, Blume ED, Gauvreau K, Mayer JE, Lock JE, Jenkins KJ (2000) Clinical outcome of fenestrated Fontan patients after closure: the first 10 years. Circulation 102:2094–2099
Moore JW, Murdison KA, Baffa GM, Kashow K, Murphy JD (2000) Transcatheter closure of fenestrations and excluded hepatic veins after fontan: versatility of the Amplatzer device. Am Heart J 140:534–540
Pihkala J, Yazaki S, Mehta R, Lee KJ, Chaturvedi R, McCrindle BW, Arsdell GV, Benson LN (2007) Feasibility and clinical impact of transcatheter closure of interatrial communications after a fenestrated Fontan procedure: medium-term outcomes. Catheter Cardiovasc Interv 69:1007–1014
Masura J, Bordacova L, Tittel P, Berden P, Podnar T (2008) Percutaneous management of cyanosis in Fontan patients using Amplatzer occluders. Catheter Cardiovasc Interv 71:843–849
Al-Hay AA, Abushaban L, Al-Qbandi MA, Alanbaei M (2011) Occlusion of Fontan fenestrations using Amplatzer septal occluder. Int J Cardiovasc Imaging 27:483–490
Malekzadeh-Milani S, Ladouceur M, Bajolle F, Bonnet D, Boudjemline Y (2015) Closure of Fontan fenestration with the use of covered stents: short- and mid-term results in a cohort of 50 patients. Cardiol Young 25:868–873
Pihkala JI, Järvelä M, Boldt T, Jokinen E, Liikanen I, Mattila I, Eerola A (2016) Fate of fenestration in children treated with fontan operation. Catheter Cardiovasc Interv 87:E233–E239
Góreczny S, Dryżek P, Morgan GJ, Kula AM, Moll JJ, Moll JA, Qureshi S, Moszura T (2017) Fenestration closure with Amplatzer Duct Occluder II in patients after total cavo-pulmonary connection. Arch Med Sci 13:337–345
Webb MK, Hunter LE, Kremer TR, Huddleston CB, Fiore AC, Danon S (2020) Extracardiac Fontan fenestration device closure with Amplatzer Vascular Plug II and Septal Occluder: procedure results and medium-term follow-up. Pediatr Cardiol 41:703–708
Itkin M, Piccoli DA, Nadolski G, Rychik J, DeWitt A, Pinto E, Rome J, Dori Y (2017) Protein-losing enteropathy in patients with congenital heart disease. J Am Coll Cardiol 69:2929–2937
Dori Y, Keller MS, Rome JJ, Gillespie MJ, Glatz AC, Dodds K, Goldberg DJ, Goldfarb S, Rychik J, Itkin M (2016) Percutaneous lymphatic embolization of abnormal pulmonary lymphatic flow as treatment of plastic bronchitis in patients with congenital heart disease. Circulation 133:1160–1170
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there are no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kawasaki, Y., Sasaki, T., Forbes, T.J. et al. Optimal criteria for transcatheter closure of Fontan fenestration: a single-center experience with a review of literature. Heart Vessels 36, 1246–1255 (2021). https://doi.org/10.1007/s00380-021-01798-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-021-01798-y