Abstract
The study aimed to assess the long-term outcomes after fenestration closure in patients at risk for Fontan failure. Of 119 patients who underwent Fontan operation between 1995 and 2004, fenestration was not created in 89 patients (NF group) and created in 30 patients with hypoplastic left heart syndrome, heterotaxy syndrome, high pulmonary arterial pressure, high systemic ventricular end-diastolic pressure, low ventricular ejection fraction, or atrioventricular valve regurgitation. All fenestrations were closed spontaneously or by catheter/surgical interventions, excepting two patients, and therefore, they were excluded. In fenestration group, patients with pre-Fontan mean pulmonary arterial pressure ≥ 15 mmHg or systemic atrioventricular valve regurgitation ≥ moderate were classified as high-risk Fontan candidates (F-HR group, n = 16), and the remaining patients were as standard-risk (F-SR group, n = 12). Protein-losing enteropathy-free survival rates did not differ among the three groups (p = 0.72). Serial follow-up catheter examinations after Fontan operation were completed in 69 patients in NF group and 11 patients in both F-SR and F-HR groups. Cardiac index and pulmonary vascular resistance significantly and similarly decreased over time in all groups, though the F-HR group showed lowest arterial oxygen saturation, lowest cardiac index, and highest pulmonary vascular resistance. The F-HR group also showed much veno-venous collaterals (p = 0.049), low peak oxygen consumption (p = 0.019), and low anaerobic threshold (p = 0.023) as compared to those in the F-SR group. In F-HR group, cyanosis remained after fenestration closure due to transformation from fenestration to veno-venous collaterals, which resulted in elevation of pulmonary vascular resistance, low cardiac index, and deterioration of exercise tolerance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fenestration between the Fontan pathway and the atrium facilitates a smooth initiation to Fontan circulation, as initially reported by Bridges et al. [1]. This simple surgical modification has been proven to allow patients at risk for early Fontan failure to undergo Fontan operation successfully [2]. Nowadays, some institutions create fenestration routinely at Fontan operation [3], while others recommend that it should be limited to selected patients to avoid the risk of paradoxical cerebral embolism, persistent hypoxemia, and subsequent increase of ventricular preload derived from development of aorto-pulmonary collateral arteries [4].
Is permanent fenestration beneficial? Some reports revealed that permanent fenestration was advantageous to maintain cardiac output, reduce late-onset atrial tachyarrhythmia, and finally improve late mortality rate [5, 6]. On the contrary, the others showed that fenestration closure preserved exercise capacity by increasing systemic oxygen saturation in exchange for decreasing cardiac output; in addition, anticoagulation therapy is no longer needed after that [7,8,9,10].
As our institutional policy, volume overload to systemic ventricle is intended to be minimized in Fontan circulation. At first, concrete coil embolization for aorto-pulmonary collaterals is routinely performed just before Fontan operation. Then fenestration is created at Fontan operation only in patients at risk for Fontan failure based on fundamental diagnosis and pre-Fontan cardiopulmonary condition. Fenestration is, however, closed once after Fontan circulation was established, so that it is designed to be closed spontaneously. If it is patent beyond one year after Fontan operation, surgical or catheter-based fenestration closure is planned. The objective of this study is herein to access the long-term outcomes after fenestration closure in patients at risk for Fontan failure, especially for high-risk Fontan candidates.
Materials and Methods
Ethical Statement
The National Cerebral and Cardiovascular Center Institutional Review Board approved this retrospective study (R19092) and opt-out consent was obtained instead of individual written informed consent.
Patient Selection
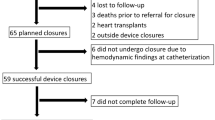
From 1995 to 2004, 119 patients underwent the Fontan operation (Fig. 1). Of those, fenestration was created in 30 patients at risk for Fontan failure and not created in 89 patients without any risks (NF group). Two patients whose fenestrations were unable to be closed to date were excluded from the study.
There were no specific preoperative criteria for creating fenestration, diagnosis such as hypoplastic left heart syndrome and heterotaxy syndrome with extra-cardiac total anomalous pulmonary venous connection or pre- and peri-operative hemodynamics such as pulmonary artery pressure, systemic ventricular end-diastolic pressure, systemic ventricular ejection fraction, and systemic atrioventricular valve regurgitation were considered and the indication was decided individually.
For further investigation (Fig. 1), patients with fenestration were divided into two groups according to previous reports concerned about risks for Fontan failure [11,12,13,14,15,16,17,18]. Sixteen patients with mean pulmonary arterial pressure ≥ 15 mmHg and/or preoperative systemic atrioventricular valve regurgitation ≥ moderate at pre-Fontan evaluation were classified as high-risk Fontan candidates (F-HR group), and the remaining 12 patients were as standard-risk candidates (F-SR group).
Surgical and Catheter-Based Intervention Procedures
An extra-cardiac total cavopulmonary connection was performed using an expanded polytetrafluoroethylene graft (n = 91, F-SR: 11, F-HR: 15, NF: 65) or a roll made from autologous pericardium (n = 23, F-SR: 1, F-HR: 1, NF: 21) [19]. For three patients in the NF group, a direct anastomosis between the pulmonary artery and the inferior vena cava was made without an extra-cardiac conduit [20]. To create a fenestration, an expanded polytetrafluoroethylene tube was interposed between the extra-cardiac conduit and the atria with a median tube diameter of 5.0 mm [inter-quartile range (IQR) 4.0–5.5], because it was easy to close spontaneously or by catheter-based coil embolization. Fenestration was closed spontaneously in 13 patients, by catheter-based coil embolization with MReye Flipper detachable embolization coils (Cook Medical Inc, Bloomington, IN, USA) in 11 patients, or by surgical ligation in two patients. The median duration from the Fontan operation to fenestration closure was 1.46 years [IQR 0.8–4.4]. For catheter-based fenestration closure, changes in central venous pressure and cardiac mixed venous oxygen saturation were evaluated by temporary balloon occlusion test. The indications for closure were a central venous pressure less than 12 mmHg before temporary occlusion and an increase in central venous pressure of less than 4 mmHg or a decrease in mixed venous oxygen saturation of less than 10% during temporary fenestration occlusion [21].
Patients
Patient characteristics are summarized in Table 1. Patient age at Fontan operation was older in the F-SR and F-HR group than in the NF group (p = 0.001). On the other hand, statistical analysis showed no significant difference between the F-SR group and the F-HR group (p = 0.79). Single-ventricular ejection fraction (p = 0.007) was lower in the F-SR group than in the NF group. Preoperative single-ventricular end-diastolic pressure (p = 0.007) were higher in the F-HR group than in NF group. Mean pulmonary arterial pressure (p = 0.0007) were higher in the F-HR group than in F-SR and NF group. Pulmonary vascular resistance did not differ among the three groups. The duration of patent fenestration did not differ between the F-SR and F-HR groups.
Study Methods
The present study was a retrospective, single-center comparative study. The evaluated variables were as follows: (1) Overall outcomes: Protein-losing enteropathy-free survival rate, (2) Serial changes in cardiopulmonary function assessed by cardiac catheter examination at five, 10 and 15 years after Fontan completion: single-ventricular ejection fraction, mean pulmonary arterial pressure, single-ventricular end-diastolic pressure, pulmonary vascular resistance, arterial oxygen saturation and cardiac index, (3) Exercise capacity testing at 15 years after Fontan completion: Peak oxygen uptake (peak VO2) and anaerobic threshold (AT) as assessed by symptom-limited treadmill exercise with expired gas analysis [22], (4) Development of veno-venous collaterals at 15 years after Fontan completion, and (5) Liver function at 15 years after Fontan completion: Aspartate aminotransferase, alanine transaminase, total bilirubin, platelet count, total protein, albumin, collagen IV, and hyaluronic acid. Serial follow-up cardiac catheter examinations after Fontan completion were routinely scheduled every five years after the operation and were completed in 63 of 89 patients in the NF group (70.8%), in 11 of 12 patients in F-SR group (91.7%), and 11 of 16 patients in F-HR group (68.8%). The characteristics of these patients are listed in Table 2. Arterial oxygen saturation was measured in all patients under room air conditions. Because no optimal method of evaluating veno-venous collateral development has been established, the method of evaluating aorto-pulmonary collaterals reported by Spicer et al. [23] was applied, with some modifications (Table 3).
Statistical Analysis
When appropriate, data are expressed as the mean ± standard deviation. Numerical data were analyzed using the Wilcoxon or Kruskal–Wallis test. Pearson's chi-square test was used for comparisons between groups. Changes in hemodynamic parameters over time were compared among the three groups by repeated-measures analysis of variance, with the main effects of groups and time, as well as interaction effects between group and time. The Tukey–Kramer test and Steel–Dwass test was used for post hoc multiple comparisons. Estimated overall protein-losing enteropathy-free survival rate was determined using the Kaplan–Meier method and were analyzed using the log-rank test. Statistical analyses were performed using JMP pro 15.1.0 (SAS Institute, Cary, NC, USA). Differences were considered statistically significant at p-values of less than 0.05.
Results
Overall Outcomes
Protein-losing enteropathy-free survival rates at 15 years were 83.3% in the F-SR group, 75.0% in the F-HR group, and 82.9% in the NF group (log-rank: p = 0.72) (Fig. 2). During study period, no patients developed stroke.
Serial Changes in Hemodynamic Indices Assessed by Cardiac Catheter Examination
Regarding single-ventricular ejection fraction, single-ventricular end-diastolic pressure, and mean pulmonary arterial pressure, no significant group effect, time effect, or interaction effect were observed (Fig. 3a–c).
Serial changes in a single-ventricular ejection fraction (SVEF), b single-ventricular end-diastolic pressure (SVEDP), c mean pulmonary artery pressure (PAP), d pulmonary vascular resistance (PVR), e arterial oxygen saturation (SaO2), and f cardiac index (CI) after Fontan completion assessed by cardiac catheter examination. NF non-fenestration group, F-SR fenestration-standard-risk group, F-HR fenestration-high-risk group. GE group effect, TE time effect, IE interaction effect. *p < 0.05 between F-HR versus F-SR and F-HR versus NF by the Tukey–Kramer test for post hoc multiple comparisons. #p < 0.05 between five years post-operative findings versus 10- or 15-year post-operative findings by Tukey–Kramer test for post hoc multiple comparisons
Pulmonary vascular resistance decreased significantly over time in all groups (time effect: p = 0.022) and was significantly higher in the F-HR group than in the other two groups (group effect: p = 0.006), yet the interaction effect was not significant (Fig. 3d).
Arterial oxygen saturation was significantly lower in the F-HR group than in the other two groups (group effect: p < 0.001), yet it did not change over time in any of the three groups (time effect: p = 0.50) and the interaction effect was not significant (p = 0.79) (Fig. 3e).
Cardiac index decreased significantly over time in all three groups (time effect: p = 0.037) and was significantly lower in the F-HR group than in the other two groups (group effect: p = 0.006). The interaction effect, however, was not significant (p = 0.74) (Fig. 3f).
Veno-Venous Collaterals at 15 Years After Fontan Completion
Of 22 patients in the F group who underwent follow-up cardiac catheter examination at 15 years after Fontan operation, 15 (68.2%) patients developed significant veno-venous collaterals. The grade of veno-venous collaterals was significantly higher in the F-HR group than in the F-SR group (p = 0.049) (Fig. 4a). No significant difference in the grade of veno-venous collaterals was associated with fenestration closure method (spontaneous or intervention, p = 0.99).
Exercise Capacity at 15 Years After Fontan Completion
Peak VO2 [median; F-SR 32.4 (IQR 26.4–35.5) vs F-HR 26.5 (21.3–27.1), mean; 31.4 ± 6.6 vs 24.4 ± 4.2 ml/min/kg, p = 0.019] and AT [18.0 (16.0–20.2) vs 15.8 (12.6–17.1), 18.3 ± 2.9 vs 15.2 ± 2.7 ml/min/kg, p = 0.023] were significantly deteriorated in F-HR group than in F-SR group at 15 years after Fontan completion (Fig. 4a, b).
Liver Function at 15 Years After Fontan Completion
Aspartate aminotransferase, alanine transaminase, total bilirubin, platelet count, total protein, collagen IV, and hyaluronic acid did not differ among the three groups, although total bilirubin and collagen IV were high and platelet count was low in all three groups as compared to standard values at 15 years after Fontan completion. The serum albumin levels were normal in all three groups; however, it was significantly lower in F-HR group than in NF group (4.4 ± 0.2 vs 4.6 ± 0.3 mg/dl, p = 0.023) (Table 4).
Discussion
The retrospective comparative study presented here identified no significant differences of protein-losing enteropathy-free survival rate among the three groups. Such a favorable outcome was thought to be resulted from maintained low Fontan pathway pressure, systemic ventricle ejection fraction, and systemic ventricular end-diastolic pressure in F-HR group during the entire follow-up period, nevertheless high pulmonary artery pressure, high end-diastolic pressure, and atrioventricular valve dysfunction were coexisted before Fontan operation. The prevention of systemic ventricular volume overload by thorough management of aorto-pulmonary collaterals therefore should be justified, at least until 15 years scheduled follow-up.
On the other hands, relative but significantly lower arterial oxygen saturation continued in the F-HR group during the entire follow-up period because fenestration was transformed to veno-venous collaterals consequently. Such a persistent desaturation caused significantly high pulmonary vascular resistance (hypoxia induced vasoconstriction) and low cardiac index in F-HR group later [24]. As the result, F-HR group showed significantly reduced peak VO2 and AT 15 years after the Fontan operation, as compared to those in F-SR group.
Classical Fontan indication, so called “10 commandments” has been already modified in almost all over the world, as represented by “2 commandments” reported in 2007 [14]. Nowadays, pre-Fontan stratification of patients was not reported to influence post-Fontan outcomes [25], so that Kotani et al. pointed out the unpredictable nature of fenestration requirement then recommended that the indication of fenestration creation should not be decided by the preoperative diagnosis, ventricular function, pulmonary artery pressure, and pulmonary vascular resistance [26]. However, this study showed more than 15 mmHg of pre-Fontan pulmonary arterial pressure and/or significant atrioventricular valve regurgitation as the result of ventricular dysfunction well predicted post-Fontan status. Fenestration closure in high-risk Fontan candidates seems not to be hemodynamically beneficial, on the other hand, it has no disadvantages because fenestration was replaced by collaterals, as described above. Because fenestration was closed by percutaneous coil embolization or surgery in nine of 14 patients (64.3%) in F-HR group, which was more than that in F-SR group (4/12 = 33.3%, p < 0.01), the results presented here indicates that interventional closure of fenestration was not necessary, but not harmful.
On the contrary, fenestration closure seems to be beneficial for F-SR group. Decreased cardiac output and increased arterial oxygen saturation are well-known phenomena just after fenestration closure [7, 8], then this study confirmed immediate recovery of cardiac output without recurrence of hypoxia in F-SR group. Such favorable outcomes would not be achieved if fenestration is persisted. Given the fact that fenestration closure was neither poison nor medicine for F-HR group, our strategy for fenestration creation and closure would be justified.
Whereas comparable life prognosis and late Fontan complication-free rates 15 years after the Fontan operation would justify the indication of Fontan operation for F-HR groups, special attention should be paid to their ultra-long-term clinical features, because exercise intolerance had already significantly progressed, and the serum albumin level was within normal but lower. It is needless to say that coil embolization of veno-venous collaterals cannot resolve this situation. Home oxygen therapy or administration of pulmonary vasodilator may be helpful to delay the timing of Fontan failure. As shown in several previous reports, again we concluded that fenestration was beneficial for initiation to Fontan circulation in selected patients, but no longer helpful after that [2]. In other words, fenestration itself can not extend the indication of Fontan operation.
Study Limitations
Due to the non-randomized retrospective nature of the present study and the small number of patients who underwent fenestrated extra-cardiac total cavopulmonary connection, this study’s statistical power may be too limited to support its conclusions. It should also be noted that the long-term follow-up data presented here were mainly collected from patients for whom Fontan operation was indicated, in whom fenestration could be closed, and who had survived for 15 years subsequently.
Conclusion
Fenestration closure after the establishment of Fontan circulation could improve systemic oxygen delivery in standard-risk patients. However, cyanosis remained due to natural transformation from fenestration to veno-venous collaterals in high-risk patients, which resulted in elevation of pulmonary vascular resistance, low cardiac index, and deterioration of exercise tolerance.
Data Availability
The data that support the findings of this study are available from the corresponding author, Takaya Hoashi, upon reasonable request.
References
Bridges ND, Lock JE, Castaneda AR (1990) Baffle fenestration with subsequent transcatheter closure. Modification of the Fontan operation for patients at increased risk. Circulation 82:1681–1689
Lemler MS, Scott WA, Leonard SR, Stromberg D, Ramaciotti C (2002) Fenestration improves clinical outcome of the fontan procedure: a prospective, randomized study. Circulation 105:207–212
Toncu A, Radulescu CR, Dorobantu D, Stoica S (2020) Does routine fenestration improve early and late postoperative outcomes in patients undergoing Fontan palliation? Interact CardioVasc Thorac Surg 30:773–779
Kaulitz R, Ziemer G, Paul T, Peuster M, Bertram H, Hausdorf G (2002) Fontan-type procedures: residual lesions and late interventions. Ann Thorac Surg 74:778–785
Atz AM, Travison TG, McCrindle BW et al (2011) Late status of Fontan patients with persistent surgical fenestration. J Am Coll Cardiol 57:2437–2443
Ono M, Boethig D, Goerler H, Lange M, Westhoff-Bleck M, Breymann T (2006) Clinical outcome of patients 20 years after Fontan operation–effect of fenestration on late morbidity. Eur J Cardiothorac Surg 30:923–929
Loomba RS, Danduran ME, Dixon JE, Rao RP (2014) Effect of Fontan fenestration on regional venous oxygen saturation during exercise: further insights into Fontan fenestration closure. Pediatr Cardiol 35:514–520
Meadows J, Lang P, Marx G, Rhodes J (2008) Fontan fenestration closure has no acute effect on exercise capacity but improves ventilatory response to exercise. J Am Coll Cardiol 52:108–113
Heal ME, Jackson LB, Atz AM, Butts RJ (2017) Effects of persistent Fontan fenestration patency on cardiopulmonary exercise testing variables. Congenit Heart Dis 2:399–402
Goff DA, Blume ED, Gauvreau K, Mayer JE, Lock JE, Jenkins KJ (2000) Clinical outcome of fenestrated Fontan patients after closure: the first 10 years. Circulation 102:2094–2099
Yurlov IA, Podzolkov VP, Zelenikin MM et al (2011) Experience with bidirectional cavopulmonary anastomosis and modified Fontan operation in patients with single ventricle and concomitant visceral heterotaxy. Interact Cardiovasc Thorac Surg 12:563–568
Burkhart HM, Dearani JA, Mair DD et al (2003) The modified Fontan procedure: early and late results in 132 adult patients. J Thorac Cardiovasc Surg 125:1252–1259
Alsaied T, Bokma JP, Engel ME et al (2017) Predicting long-term mortality after Fontan procedures: a risk score based on 6707 patients from 28 studies. Congenit Heart Dis 12:393–398
Hosein RB, Clarke AJ, McGuirk SP et al (2007) Factors influencing early and late outcome following the Fontan procedure in the current era. The “Two Commandments”? Eur J Cardiothorac Surg 31:344–352
Kim SJ, Kim WH, Lim HG, Lee JY (2008) Outcome of 200 patients after an extracardiac Fontan procedure. J Thorac Cardiovasc Surg 136:108–116
d’Udekem Y, Xu MY, Galati JC et al (2012) Predictors of survival after single-ventricle palliation: the impact of right ventricular dominance. J Am Coll Cardiol 59:1178–1185
Tseng SY, Siddiqui S, Di Maria MV et al (2020) Atrioventricular valve regurgitation in single heart disease: a common problem associated with progressive deterioration and mortality. J Am Heart Assoc 9:e015737
Alsaied T, Bokma JP, Engel ME et al (2017) Factors associated with long-term mortality after Fontan procedures: a systematic review. Heart 103:104–110
Adachi I, Yagihara T, Kagisaki K et al (2005) Fontan operation with a viable and growing conduit using pedicled autologous pericardial roll: serial changes in conduit geometry. J Thorac Cardiovasc Surg 130:1517–1522
McKay R, Dearani JA (2008) Extracardiac Fontan with direct cavopulmonary connections. Ann Thorac Surg 85:669–671
Pihkala JI, Järvelä M, Boldt T et al (2016) Fate of fenestration in children treated with Fontan operation. Catheter Cardiovasc Interv 87:E233–E239
Ohuchi H, Negishi J, Noritake K et al (2015) Prognostic value of exercise variables in 335 patients after the Fontan operation: a 23-year single-center experience of cardiopulmonary exercise testing. Congenit Heart Dis 10:105–116
Spicer RL, Uzark KC, Moore JW, Mainwaring RD, Lamberti JJ (1996) Aortopulmonary collateral vessels and prolonged pleural effusions after modified Fontan procedures. Am Heart J 131:1164–1168
Cai J, Su Z, Shi Z et al (2008) Nitric oxide and milrinone: combined effect on pulmonary circulation after Fontan-type procedure: a prospective, randomized study. Ann Thorac Surg 86:882–888
Vigano G, McMahon CJ, Walsh K, Oslizlok P, Franklin O, Nolke L et al (2019) High-risk Fontan completion patients achieve low perioperative risk and benefit from cavopulmonary connection 7 years out. Eur J Cardiothorac Surg 56:664–670
Kotani Y, Chetan D, Saedi A et al (2014) Persistent fenestration may be a marker for physiologic intolerance after Fontan completion. J Thorac Cardiovasc Surg 148:2532–2538
Funding
None declared.
Author information
Authors and Affiliations
Contributions
HO and TH conceived the presented idea. HO developed the theory and performed the computations. HO, KK, and HI encouraged HO to investigate long-term effect of temporary fenestration and supervised the findings of this work. All authors discussed the results and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All the authors declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ozawa, H., Hoashi, T., Ohuchi, H. et al. Long-Term Outcomes After Fenestration Closure in High-Risk Fontan Candidates. Pediatr Cardiol 42, 1356–1364 (2021). https://doi.org/10.1007/s00246-021-02619-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-021-02619-9