Abstract
The effects of prehospital epinephrine administration on post-arrest neurological outcome in out-of-hospital cardiac arrest (OHCA) patients with non-shockable rhythm remain unclear. To examine the time-dependent effectiveness of prehospital epinephrine administration, we analyzed 118,396 bystander-witnessed OHCA patients with non-shockable rhythm from the prospectively recorded all-Japan OHCA registry between 2011 and 2014. Patients who achieved prehospital return of spontaneous circulation without prehospital epinephrine administration were excluded. Patients with prehospital epinephrine administration were stratified according to the time from the initiation of cardiopulmonary resuscitation (CPR) by emergency medical service (EMS) providers to the first epinephrine administration (≤ 10, 11–19, and ≥ 20 min). Patients without prehospital epinephrine administration were stratified according to the time from CPR initiation by EMS providers to hospital arrival (≤ 10, 11–19, and ≥ 20 min). The primary outcome was 1-month neurologically intact survival (cerebral performance category 1 or 2; CPC 1–2). Multivariate logistic regression analysis demonstrated that there was no significant difference in the chance of 1-month CPC 1–2 between patients who arrived at hospital in ≤ 10 min without prehospital epinephrine administration and patients with time to epinephrine administration ≤ 19 min. However, compared to patients who arrived at hospital in ≤ 10 min without prehospital epinephrine administration, patients with time to epinephrine administration ≥ 20 min and patients who arrived at hospital in 11–19, and ≥ 20 min without prehospital epinephrine administration were significantly associated with decreased chance of 1-month CPC 1–2 (p < 0.05, < 0.05, and < 0.001, respectively). In conclusion, when prehospital CPR duration from CPR initiation by EMS providers to hospital arrival estimated to be ≥ 11 min, prehospital epinephrine administered ≤ 19 min from CPR initiation by EMS providers could improve neurologically intact survival in bystander-witnessed OHCA patients with non-shockable rhythm.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Epinephrine is the first drug administered during cardiopulmonary resuscitation (CPR) and is recommended in the 2015 CPR guidelines for use in adult cardiac arrest [1, 2]. Previous studies including randomized controlled trials, observational studies, meta-analyses and systematic reviews have suggested that prehospital epinephrine administration in patients with out-of-hospital cardiac arrest (OHCA) increased prehospital return of spontaneous circulation (ROSC) and survival to hospital admission, however, had no benefit on or reduced long-term survival and neurologically intact survival [3,4,5,6,7,8,9,10,11,12,13,14]. Studies examining the association between prehospital epinephrine administration and survival or neurologically intact survival stratifying patients by initial rhythm (shockable or non-shockable) demonstrated conflicting results, partially due to a lack of detailed analysis regarding the timing of epinephrine administration, the inclusion of patients with OHCA achieving prehospital ROSC without prehospital epinephrine administration, and in particular, the use of patients without prehospital epinephrine administration as a reference, regardless of the prehospital CPR duration required to hospital arrival [3,4,5,6,7,8,9,10, 14,15,16,17,18,19]. Although the 2015 CPR guidelines recommend prehospital epinephrine administration as soon as feasible after onset of cardiac arrest due to non-shockable rhythm, the effects and optimal timing of prehospital epinephrine administration on neurologically intact survival in patients with OHCA with non-shockable rhythm still remain controversial [1, 2, 17, 19, 20].
This study aimed to test our hypothesis that the effects of prehospital epinephrine administration differ in patients with OHCA with non-shockable rhythm according to the time from the initiation of CPR by emergency medical service (EMS) providers to the first epinephrine administration in association with prehospital CPR duration required to hospital arrival.
Materials and methods
Study design and data source
In January 2005, the Fire and Disaster Management Agency (FDMA) of Japan launched a prospective, nationwide, population-based registry based on the Utstein-style data collection including all patients with OHCA [21, 22]. Using this registry, this observational study enrolled adults (age ≥ 18 years) for whom resuscitation was attempted after OHCA between January 2011 and December 2014. Cardiac arrest was confirmed by victim with unresponsiveness and the absence of normal breathing [23, 24]. The cause of the arrest was determined by the physicians in charge and EMS providers.
This study was approved by the ethics committee of Kanazawa University, and informed consent was waived because of the anonymous nature of the data used.
The Japanese EMS system
Japan has approximately 127 million residents occupying an area of 378,000 km2. Details of the Japanese EMS system have been described previously [21]. Briefly, the FDMA of Japan supervises the nationwide EMS system, and local fire stations operate the local EMS systems. Emergency lifesaving technicians are allowed to use automated external defibrillators (AED), insert of an airway adjunct or a peripheral intravenous line, and administer Ringer’s Lactate solution. Only specifically trained emergency lifesaving technicians are permitted to insert a tracheal tube and administer intravenous epinephrine, following physician instructions conveyed over phone. All EMS providers perform CPR according to the Japanese CPR guideline [23]. As EMS providers in Japan are legally prohibited from terminating resuscitation in the field, most OHCA patients who receive CPR by EMS providers are transported to hospital, except in cases where fatality is certain.
Data collection and quality control
Data were collected prospectively for variables such as age, sex, cause of arrest, bystander-witness status, bystander CPR with or without AED, initial cardiac rhythm, bystander category. Other variables included whether (a) epinephrine was administered, (b) advanced airway management techniques were used, (c) ROSC was achieved before hospital arrival, combined with the time of (a) the emergency call, (b) ambulance arrival at the scene, (c) CPR initiation by the EMS providers, (d) ROSC, (e) ambulance arrival at the hospital, (f) epinephrine administration, (g) shock delivery by the EMS providers; 1-month survival, and neurological outcome at 1 month after cardiac arrest. The response time was calculated as the time from the emergency call to the arrival of an ambulance at the scene. The time to epinephrine administration was defined as the time from CPR initiation by EMS providers to the first epinephrine administration. Prehospital CPR duration was defined as the time from CPR initiation by EMS providers to ROSC in cases where prehospital ROSC was achieved or to hospital arrival when prehospital ROSC was not achieved. Neurological outcome was defined using the Cerebral Performance Category (CPC) scale: category 1, good cerebral performance; category 2, moderate cerebral disability; category 3, severe cerebral disability; category 4, coma or vegetative state; and category 5, death [22]. CPC categorization was performed by the physician in charge.
Outcome
The primary study outcome was 1-month neurologically intact survival, defined as a CPC score of 1 or 2 (CPC 1–2).
Statistical analysis
Continuous variables were expressed as medians (interquartile range) or means and standard deviations and compared using the Wilcoxon and Kruskal–Wallis tests. Categorical variables were expressed as counts and percentages, and differences between groups were compared using the χ2 test. We classified age into two categories: < 75 and ≥ 75 years according to the latest definition of elderly by the Japan Gerontological Society and the Japan Geriatrics Society [25, 26]. We categorized response time (≤ 6, 7–8, and ≥ 9 min), and in patients with prehospital epinephrine administration, time to epinephrine administration (≤ 10, 11–19, and ≥ 20 min) according to their first and third quartiles (Table 1) and previous reports [17, 19]. Patients without prehospital epinephrine administration or prehospital ROSC may have received epinephrine after hospital arrival. Therefore, the prehospital CPR duration to hospital arrival which is almost equivalent to the time from CPR initiation by EMS providers to the first in-hospital epinephrine administration was divided into 3 categories (≤ 10, 11–19, and ≥ 20 min), consistent with the categorization of time to epinephrine administration. In bystander-witnessed OHCA patients with non-shockable rhythm (Cohort 1) and those except for patients who achieved prehospital ROSC without prehospital epinephrine administration (Cohort 2), multivariate logistic regression analysis using 8 prehospital variables, including potential confounders derived based on biological plausibility and from previous studies, was performed. We identified factors associated with 1-month CPC 1–2 and calculated the adjusted odds ratio (OR) and 95% confidence interval (CI). Eight prehospital variables were used for analysis: age, sex, presumed cardiac etiology, initial rhythm (pulseless electrical activity (PEA) or asystole), bystander CPR, use of advanced airway management, response time, the presence or absence of prehospital epinephrine administration, and the time to epinephrine administration or the prehospital CPR duration to hospital arrival. In Cohort 2, several models with different references were constructed to evaluate the time-dependent effectiveness of prehospital epinephrine administration. Statistical analyses were performed using JMP Pro software, version 12.2.0 (SAS Institute, Cary, NC, USA). All tests were 2-tailed, and p values < 0.05 were considered statistically significant.
Results
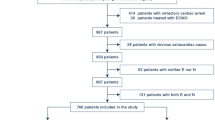
During the 4-year study period, 506,050 OHCA events were documented. Out of 496,560 patients with OHCA with attempted resuscitation by EMS providers, there were 124,856 bystander-witnessed patients with OHCA with non-shockable rhythm aged ≥ 18 years (24.7%; Cohort 1). Following the exclusion of 6460 patients from Cohort 1 who achieved prehospital ROSC without prehospital epinephrine administration, 118,396 patients with OHCA were eligible for analysis (23.4%; Cohort 2) (Fig. 1). Baseline patient characteristics and post-arrest outcomes of all patients and subgroups of Cohort 1 are shown in Table 1. The rate of 1-month CPC 1–2 in all patients was 1.13% (1416/124,856) in Cohort 1. Patients who achieved prehospital ROSC without prehospital epinephrine administration were younger, with a lower incidence of presumed cardiac etiology and use of advanced airway management, a higher proportion of PEA, a shorter response time and prehospital CPR duration, and a considerably higher 1-month survival rate and CPC 1–2 rate than other groups. In Cohort 1, multivariate logistic regression analysis revealed that older age, use of advanced airway management, and prehospital epinephrine administration were negatively associated with 1-month CPC 1–2. PEA and shorter response time were positively associated with 1-month CPC 1–2 (Table 2).
In Cohort 2, the rates of 1-month CPC 1–2 were 0.90% (71/7895) in patients with prehospital epinephrine administration with time to epinephrine administration ≤ 10 min, 0.66% (85/12,886) for 11–19 min, 0.30% (19/6383) for ≥20 min, and 0.65% (29/4465) in patients without prehospital epinephrine administration with prehospital CPR duration to hospital arrival ≤ 10 min, 0.37% (124/33,506) for 11–19 min, 0.15% (82/53,261) for ≥20 min (p < 0.001). Multivariate logistic regression analysis revealed that there was no significant difference in 1-month CPC 1–2 rates between patients who arrived at hospital in ≤ 10 min without prehospital epinephrine administration and patients with time to epinephrine administration ≤ 19 min. Furthermore, compared to patients who arrived at hospital in ≤ 10 min without prehospital epinephrine administration, patients with time to epinephrine administration ≥ 20 min, patients who arrived at hospital in 11–19, and ≥ 20 min without prehospital epinephrine administration were significantly associated with decreased chance of 1-month CPC 1–2 (p < 0.05, < 0.05, and < 0.001, respectively) (Fig. 2; Table 3, model 1). Compared to patients who arrived at hospital in 11–19 min without prehospital epinephrine administration, patients with time to epinephrine administration ≤ 19 min were significantly associated with increased chance of 1-month CPC 1–2 (Table 3, model 2). Compared to patients who arrived at hospital in ≥ 20 min without prehospital epinephrine administration, patients with prehospital epinephrine administration, irrespective of the timing, were significantly associated with increased chance of 1-month CPC 1–2 (Table 3, model 3). Time to epinephrine administration ≤ 10 and 11–19 min increased the chance of 1-month CPC 1–2 compared with time to epinephrine administration ≥ 20 min (Table 3, model 6).
Adjusted odds ratios (OR) and 95% confidence intervals (CI) of the presence or absence of prehospital epinephrine administration for 1-month neurologically intact survival in association with time to epinephrine administration and cardiopulmonary resuscitation (CPR) duration to hospital arrival in Cohort 2 (Table 3, model 1). Neurologically intact survival was defined as a Cerebral Performance Category (CPC) 1 or 2. Patients with prehospital epinephrine administration were categorized according to the time from CPR initiation by emergency medical service (EMS) providers to the first epinephrine administration (time to epinephrine administration ≤ 10, 11–19, and ≥ 20 min), and patients without prehospital epinephrine administration were categorized according to the time from CPR initiation by EMS providers to hospital arrival (CPR duration to hospital arrival ≤ 10, 11–19, and ≥ 20 min). Adjusted ORs were calculated using a predefined set of seven potential confounders: age, sex, cardiac etiology, initial rhythm, bystander CPR, use of advanced airway management, response time
Discussion
In this nationwide, population-based observational study of OHCA in Japan, when prehospital CPR duration from CPR initiation by EMS providers to hospital arrival was ≥ 11 min, prehospital epinephrine administered ≤ 19 min from CPR initiation by EMS providers improved neurologically intact survival in bystander-witnessed OHCA patients with non-shockable rhythm.
To our knowledge, this is the first and largest study demonstrating that prehospital epinephrine administered ≤ 19 min from CPR initiation by EMS providers improved or at least had no harmful effects on neurologically intact survival, defined as a CPC score of 1 or 2, in patients with OHCA with non-shockable rhythm (Table 3). Nakahara et al. reported that prehospital epinephrine administration improved overall survival but not neurologically intact survival in patients with OHCA with non-shockable rhythm [16]. However, the timing of prehospital epinephrine administration was not considered. In a further study, the authors reported that early epinephrine administration, defined as within 10 min from CPR initiation by EMS providers, improved survival but not neurologically intact survival in patients with OHCA with non-shockable rhythm [19]. Recently, Hansen et al. reported that early epinephrine administration (time in minutes as continuous variable) improved neurologically intact survival in patients with OHCA with non-shockable rhythm [20]. However, the study analyzed only patients with epinephrine administration. Goto et al. demonstrated that in patients with OHCA with non-shockable rhythm, prehospital epinephrine administration < 20 min from CPR initiation by EMS providers was significantly associated with a higher ratio of 1-month survival than that of patients without epinephrine administration. However, 1-month neurologically intact survival rate in OHCA patients with epinephrine administration ≥ 10 min was significantly lower than that in patients without epinephrine administration [17]. In the present study, early prehospital epinephrine administration (time to epinephrine administration ≤ 10 and 11–19 min) increased the chance of 1-month CPC 1–2 compared to late epinephrine administration (time to epinephrine administration ≥ 20 min) in bystander-witnessed OHCA patients with non-shockable rhythm (Table 3, model 6). Furthermore, compared to patients who arrived at hospital in 11–19 or ≥ 20 min without prehospital epinephrine administration, patients with time to epinephrine administration ≤ 19 min were significantly associated with increased chance of 1-month CPC 1–2 (Table 3, models 2 and 3). These conflicting results were attributable to differences in the inclusion and exclusion criteria between the present study and previous studies. Goto et al. and other studies [3,4,5,6,7,8,9,10, 14, 16,17,18] investigated the association between prehospital epinephrine administration and post-arrest outcome without excluding patients with OHCA who achieved prehospital ROSC without prehospital epinephrine administration. In the present study, prehospital epinephrine administration was negatively associated with neurologically intact survival on including these patients (Table 2). However, these patients had more favorable factors associated with achieving neurologically intact survival and considerably higher neurologically intact survival rate as previously reported [19] (15.6% in the present study, Fig. 1; Tables 1, 2). Therefore, patients achieving prehospital ROSC without prehospital epinephrine administration should be excluded when examining the effects of prehospital epinephrine administration. In these patients with a low incidence of cardiac etiology and high proportion of PEA (Table 1), elimination of reversible causes may be more effective than epinephrine administration. Tomio et al. reported that prehospital epinephrine administration is favorably associated with neurologically intact survival in patients with OHCA with asystole but not in those with PEA [18]. After excluding patients achieving prehospital ROSC without prehospital epinephrine administration, we examined the time-dependent effectiveness of prehospital epinephrine administration in patients in whom epinephrine was assumed to be necessary to reverse cardiac arrest. Furthermore, previous studies used “patients without prehospital epinephrine administration” as a reference, regardless of the prehospital CPR duration required to hospital arrival [3,4,5,6,7,8,9,10, 14, 16,17,18]. Patients who did not receive prehospital epinephrine in the prehospital setting may have received epinephrine later at the hospital. Therefore, there was a lack of information regarding the timing of in-hospital epinephrine administration upon arrival to the emergency department. To address this methodological limitation, we stratified the “patients without prehospital epinephrine administration” group according to prehospital CPR duration to hospital arrival, which is almost equivalent to the time from CPR initiation by EMS providers to the first in-hospital epinephrine administration. Using these novel stratification methods, we found that epinephrine administration ≤ 19 min from CPR initiation by EMS providers had beneficial effects or at least had no harmful effects on neurologically intact survival in bystander-witnessed OHCA patients with non-shockable rhythm. Conceivably, the decision to administer epinephrine to patients with OHCA in the prehospital setting or to transport these patients to a hospital without prehospital epinephrine administration depends on prehospital CPR duration required to hospital arrival. Prehospital epinephrine administration requires intravascular access and interruption of high-quality CPR. Therefore, we suggest that if EMS providers are able to transport patients to a hospital within 10 min providing high-quality CPR, transport might be given priority. However, median or mean CPR duration to hospital arrival was > 20 min among patients with OHCA with non-shockable rhythm without prehospital ROSC (Table 1). Accordingly, prehospital epinephrine administration ≤ 19 min, if possible ≤ 10 min, should be attempted to achieve neurologically intact survival for most patients with OHCA with non-shockable rhythm.
The major limitation to this study is that patients with prehospital epinephrine administration were not assigned based on randomized selection. Second, excluding OHCA patients achieving prehospital ROSC without prehospital epinephrine administration results in a bias favoring the group with epinephrine administration because some patients may have achieved ROSC without epinephrine administration in this group. Third, we did not evaluate the association between total doses of epinephrine and post-arrest outcome because we did not have detailed cumulative doses of epinephrine, including in-hospital dosages. Fourth, we investigated only patients with non-shockable rhythm because defibrillation is recommended as a first-line treatment for shockable rhythm; optimal timing of epinephrine administration in relation to the timing of defibrillation may vary according to patient factors and resuscitation conditions and is difficult to determine [1]. Fifth, patients with rhythm conversion from initial non-shockable to shockable rhythm and subsequent shock delivery in prehospital setting were also excluded to eliminate the effects of prehospital defibrillation [27]. Finally, high-quality CPR performed by EMS providers may extend the effective time window for epinephrine administration. Unfortunately, we did not have sufficient data to allow us to perform further risk adjustment (e.g., quality of EMS providers, comorbid disease, location of cardiac arrest, and in-hospital medication). These limitations are attributable to the retrospective study design. To validate the results of this study and to establish the target population for the administration of prehospital epinephrine to improve neurologically intact survival, a well-designed, placebo controlled, double-blind, randomized control trial with a large sample evaluating the efficacy of epinephrine administration and optimal administration timing is required. An ongoing randomized trial in the United Kingdom comparing epinephrine and placebo for patients with OHCA may provide further insight into epinephrine administration (PARAMEDIC 2: ISRCTN73485024) [28].
Conclusions
When prehospital CPR duration from CPR initiation by EMS providers to hospital arrival estimated to be ≥ 11 min, prehospital epinephrine administration ≤ 19 min from CPR initiation by EMS providers could improve neurologically intact survival in bystander-witnessed OHCA patients with non-shockable rhythm. The decision to administer epinephrine to OHCA patients with non-shockable rhythm in the prehospital setting or to transport these patients to a hospital without prehospital epinephrine administration depends on the prehospital CPR duration required to hospital arrival.
References
Link MS, Berkow LC, Kudenchuk PJ, Halperin HR, Hess EP, Moitra VK, Neumar RW, O’Neil BJ, Paxton JH, Silvers SM, White RD, Yannopoulos D, Donnino MW (2015) Part 7: adult advanced cardiovascular life support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 132(18 Suppl 2):S444–S464
Soar J, Nolan JP, Böttiger BW, Perkins GD, Lott C, Carli P, Pellis T, Sandroni C, Skrifvars MB, Smith GB, Sunde K, Deakin CD, Adult advanced life support section Collaborators (2015) European Resuscitation Council Guidelines for Resuscitation 2015: section 3. Adult advanced life support. Resuscitation 95:100–147
Olasveengen TM, Sunde K, Brunborg C, Thowsen J, Steen PA, Wik L (2009) Intravenous drug administration during out-of-hospital cardiac arrest: a randomized trial. JAMA 302:2222–2229
Jacobs IG, Finn JC, Jelinek GA, Oxer HF, Thompson PL (2011) Effect of adrenaline on survival in out-of-hospital cardiac arrest: a randomised double-blind placebo-controlled trial. Resuscitation 82:1138–1143
Hagihara A, Hasegawa M, Abe T, Nagata T, Wakata Y, Miyazaki S (2012) Prehospital epinephrine use and survival among patients with out-of-hospital cardiac arrest. JAMA 307:1161–1168
Machida M, Miura S, Matsuo K, Ishikura H, Saku K (2012) Effect of intravenous adrenaline before arrival at the hospital in out-of-hospital cardiac arrest. J Cardiol 60:503–507
Dumas F, Bougouin W, Geri G, Lamhaut L, Bougle A, Daviaud F, Morichau-Beauchant T, Rosencher J, Marijon E, Carli P, Jouven X, Rea TD, Cariou A (2014) Is epinephrine during cardiac arrest associated with worse outcomes in resuscitated patients? J Am Coll Cardiol 64:2360–2367
Fukuda T, Ohashi-Fukuda N, Matsubara T, Gunshin M, Kondo Y, Yahagi N (2016) Effect of prehospital epinephrine on out-of-hospital cardiac arrest: a report from the national out-of-hospital cardiac arrest data registry in Japan, 2011–2012. Eur J Clin Pharmacol 72:1255–1264
Hayashi Y, Iwami T, Kitamura T, Nishiuchi T, Kajino K, Sakai T, Nishiyama C, Nitta M, Hiraide A, Kai T (2012) Impact of early intravenous epinephrine administration on outcomes following out-of-hospital cardiac arrest. Circ J 76:1639–1645
Tanaka H, Takyu H, Sagisaka R, Ueta H, Shirakawa T, Kinoshi T, Takahashi H, Nakagawa T, Shimazaki S, Ong Eng Hock M (2016) Favorable neurological outcomes by early epinephrine administration within 19 minutes after EMS call for out-of-hospital cardiac arrest patients. Am J Emerg Med 34:2284–2290
Loomba RS, Nijhawan K, Aggarwal S, Arora RR (2015) Increased return of spontaneous circulation at the expense of neurologic outcomes: is prehospital epinephrine for out-of-hospital cardiac arrest really worth it? J Crit Care 30:1376–1381
Atiksawedparit P, Rattanasiri S, McEvoy M, Graham CA, Sittichanbuncha Y, Thakkinstian A (2014) Effects of prehospital adrenaline administration on out-of-hospital cardiac arrest outcomes: a systematic review and meta-analysis. Crit Care 18:463
Lin S, Callaway CW, Shah PS, Wagner JD, Beyene J, Ziegler CP, Morrison LJ (2014) Adrenaline for out-of-hospital cardiac arrest resuscitation: a systematic review and meta-analysis of randomized controlled trials. Resuscitation 85:732–740
Olasveengen TM, Wik L, Sunde K, Steen PA (2012) Outcome when adrenaline (epinephrine) was actually given vs. not given—post hoc analysis of a randomized clinical trial. Resuscitation 83:327–332
Ewy GA, Bobrow BJ, Chikani V, Sanders AB, Otto CW, Spaite DW, Kern KB (2015) The time dependent association of adrenaline administration and survival from out-of-hospital cardiac arrest. Resuscitation 96:180–185
Nakahara S, Tomio J, Takahashi H, Ichikawa M, Nishida M, Morimura N, Sakamoto T (2013) Evaluation of pre-hospital administration of adrenaline (epinephrine) by emergency medical services for patients with out of hospital cardiac arrest in Japan: controlled propensity matched retrospective cohort study. BMJ 347:f6829
Goto Y, Maeda T, Goto Y (2013) Effects of prehospital epinephrine during out-of-hospital cardiac arrest with initial non-shockable rhythm: an observational cohort study. Crit Care 17:R188
Tomio J, Nakahara S, Takahashi H, Ichikawa M, Nishida M, Morimura N, Sakamoto T (2017) Effectiveness of prehospital epinephrine administration in improving long-term outcomes of witnessed out-of-hospital cardiac arrest patients with initial non-shockable rhythms. Prehosp Emerg Care 21:432–441
Nakahara S, Tomio J, Nishida M, Morimura N, Ichikawa M, Sakamoto T (2012) Association between timing of epinephrine administration and intact neurologic survival following out-of-hospital cardiac arrest in Japan: a population-based prospective observational study. Acad Emerg Med 19:782–792
Hansen M, Schmicker RH, Newgard CD, Grunau B, Scheuermeyer F, Cheskes S, Vithalani V, Alnaji F, Rea T, Idris AH, Herren H, Hutchison J, Austin M, Egan D, Daya M, Resuscitation Outcomes Consortium Investigators (2018) Time to epinephrine administration and survival from non-shockable out-of-hospital cardiac arrest among children and adults. Circulation 137:2032–2040
Kitamura T, Iwami T, Kawamura T, Nitta M, Nagao K, Nonogi H, Yonemoto N, Kimura T, Japanese Circulation Society Resuscitation Science Study Group (2012) Nationwide improvements in survival from out-of-hospital cardiac arrest in Japan. Circulation 126:2834–2843
Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D, International Liaison Committee on Resuscitation; American Heart Association; European Resuscitation Council; Australian Resuscitation Council; New Zealand Resuscitation Council; Heart and Stroke Foundation of Canada; InterAmerican Heart Foundation; Resuscitation Councils of Southern Africa; ILCOR Task Force on Cardiac Arrest and Cardiopulmonary Resuscitation Outcomes (2004) Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation 110:3385–3397
Japan Resuscitation Council (2011) 2010 Japanese guidelines for emergency care and cardiopulmonary resuscitation. Tokyo, Health Shuppansha (in Japanese)
American Heart Association (2010) 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 122:S639–S946
Ouchi Y, Rakugi H, Arai H, Akishita M, Ito H, Toba K, Kai I, Joint Committee of Japan Gerontological Society (JGLS) and Japan Geriatrics Society (JGS) on the definition and classification of the elderly (2017) Redefining the elderly as aged 75 years and older: Proposal from the Joint Committee of Japan Gerontological Society and the Japan Geriatrics Society. Geriatr Gerontol Int 17:1045–1047
Funada A, Goto Y, Maeda T, Teramoto R, Hayashi K, Yamagishi M (2016) Improved survival with favorable neurological outcome in elderly individuals with out-of-hospital cardiac arrest in Japan—a nationwide observational cohort study. Circ J 80:1153–1162
Funada A, Goto Y, Tada H, Teramoto R, Shimojima M, Hayashi K, Yamagishi M (2016) Age-specific differences in prognostic significance of rhythm conversion from initial non-shockable to shockable rhythm and subsequent shock delivery in out-of-hospital cardiac arrest. Resuscitation 108:61–67
Perkins GD, Quinn T, Deakin CD, Nolan JP, Lall R, Slowther AM, Cooke M, Lamb SE, Petrou S, Achana F, Finn J, Jacobs IG, Carson A, Smyth M, Han K, Byers S, Rees N, Whitfield R, Moore F, Fothergill R, Stallard N, Long J, Hennings S, Horton J, Kaye C, Gates S (2016) Pre-hospital assessment of the role of adrenaline: measuring the effectiveness of drug administration in cardiac arrest (PARAMEDIC-2): trial protocol. Resuscitation 108:75–81
Acknowledgements
We thank all of the EMS providers and participating physicians in Japan and the FDMA for their generous cooperation in establishing and maintaining the database.
Funding
This work was supported by JSPS KAKENHI Grant Number JP16K19171.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Funada, A., Goto, Y., Tada, H. et al. Effects of prehospital epinephrine administration on neurologically intact survival in bystander-witnessed out-of-hospital cardiac arrest patients with non-shockable rhythm depend on prehospital cardiopulmonary resuscitation duration required to hospital arrival. Heart Vessels 33, 1525–1533 (2018). https://doi.org/10.1007/s00380-018-1205-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1205-6