Abstract
Previous studies have reported the prognostic value of objective nutritional indices such as the Controlling Nutritional Status (CONUT) score, Geriatric Nutritional Risk Index (GNRI) and Prognostic Nutritional Index (PNI). However, the effects of these indices in patients with coronary artery disease (CAD) who have undergone percutaneous coronary intervention (PCI) remain unclear. Furthermore, there are insufficient data to combine these indices. A total of 1984 patients who underwent elective PCI were enrolled. The Combined Objective Nutritional Score was determined by assigning 1 point each for high CONUT score (3–12), low GNRI (< 98) or low PNI (< 45). Patients were grouped into normal nutritional status (0 points), mild-to-moderate malnutrition (1–2 points) and severe malnutrition (3 points). Incidences of all-cause death and cardiac death were evaluated. Among the 1984 patients, 514 (25.9%) and 244 (12.3%) had mild-to-moderate and severe malnutrition, respectively. During follow-up (median 7.4 years), 293 all-cause deaths were identified, including 92 cardiac deaths. Kaplan–Meier curves showed ongoing divergence in rates of death among nutritional statuses determined by the novel score (log rank test, p < 0.0001). Multivariate Cox hazard analysis showed that patients with a Combined Objective Nutritional Score of 3 showed 2.91-fold (95% confidence interval (CI) 2.10–4.00; p < 0.0001) and 2.16-fold (95% CI 1.15–3.92; p = 0.02) increases in risk of mortality and cardiac mortality compared with patients with a Combined Objective Nutritional Score of 0. In conclusion, malnutrition as evaluated by the Combined Objective Nutritional Score was significantly associated with worse long-term cardiovascular outcomes among CAD patients who underwent PCI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Malnutrition has been recognized as an independent risk factor for unfavorable events in patients with heart failure [1, 2]. Weight loss with development of cardiac cachexia is commonly associated with declines in physical function and worse prognosis. Evaluation of nutritional status is, therefore, recommended in guidelines for heart failure [3, 4] and early nutritional intervention can reduce the risk of adverse cardiac events in these patients [5]. Some objective nutritional indices such as the Controlling Nutritional Status (CONUT) score [6], Geriatric Nutritional Risk Index (GNRI) [7] and Prognostic Nutritional Index (PNI) [8, 9], have been reported as useful clinical predictors of mortality or morbidity in patients with heart failure [10,11,12,13,14].
Some recent studies have evaluated nutritional status using these objective nutritional indices and have demonstrated associations between clinical outcomes and malnutrition in patients with coronary artery disease (CAD) [15,16,17]. Although CONUT score, GNRI and PNI might offer useful predictive markers, these indices were calculated using different methods that show various advantages and disadvantages. The aim of our study was to evaluate the prognostic values of these three objective nutritional indices among CAD patients who have undergone elective percutaneous coronary intervention (PCI). Furthermore, we combined data from these indices and evaluated the effects of a novel combined score (Combined Objective Nutritional Score) on long-term outcomes.
Materials and methods
Study population and data collection
The present study was a single-center, observational, retrospective cohort study. Among consecutive patients with CAD who underwent elective PCI for the first time at Juntendo University Hospital, Tokyo, Japan, between January 2000 and December 2011, only patients for whom pre-procedural CONUT score, GNRI and PNI were available were investigated. Patients with known malignancy or active inflammatory disease were excluded from the study.
Demographic data and information about coronary risk factors, medications, revascularization procedure-related factors, and co-morbidities were prospectively collected and analyzed. Blood samples were collected in the early morning after overnight fasting, and blood pressure (BP) was measured on admission. Patients with BP > 140/90 mmHg or those receiving antihypertensive drugs were regarded as hypertensive. Dyslipidemia was defined as low-density lipoprotein cholesterol (LDL-C) ≥ 140 mg/dl, high-density lipoprotein cholesterol (HDL-C) ≤ 40 mg/dl, triglycerides ≥ 150 mg/dl, or current treatment with statins and/or lipid-lowering agents [18]. Diabetes mellitus was defined as either hemoglobin A1c ≥ 6.5% or medication with insulin or oral hypoglycemic drugs. Chronic kidney disease (CKD) was defined as an estimated glomerular filtration rate < 60 ml/min/1.73 m2 as calculated using the Modification of Diet in Renal Disease equation modified with a Japanese coefficient using baseline serum creatinine [19]. A current smoker was defined as a person who was smoking at the time of PCI or who had stopped smoking within 1 year before PCI. Left ventricular ejection fraction (LVEF) was assessed using left ventricular angiography or echocardiography before PCI. All patients had symptoms of effort angina, documented myocardial ischemia, or both.
Written, informed consent was obtained from all patients before undergoing PCI. This study was performed in accordance with the Declaration of Helsinki and with the approval of our institutional review board.
Primary endpoints
Both all-cause death and cardiac death during the follow-up period were evaluated. Cardiac death was defined as death from CAD, cardiogenic shock, or sudden death. Clinical follow-up comprised analyses of clinical charts and responses to questionnaires sent to patients or their families, and telephone contact. Mortality data were collected from the medical records of patients who died or who were treated at our institution, and details and causes of death were obtained from other hospitals to which patients had been admitted.
Evaluation of nutritional indices
Baseline CONUT score was calculated from serum albumin levels, total cholesterol levels and total lymphocyte counts as follows: serum albumin ≥ 3.5 g/dl, 0 points; 3.0–3.4 g/dl, 2 points; 2.5–2.9 g/dl, 4 points; and < 2.5 g/dl, 6 points; total cholesterol ≥ 180 mg/dl, 0 points; 140–179 mg/dl, 1 point; 100–139 mg/dl, 2 points; and < 100 mg/dl, 3 points; and total lymphocyte count ≥ 1600/ml, 0 points; 1200–1599/ml, 1 point; 800–1199/ml, 2 points; and < 800/ml, 3 points [6]. CONUT scores range from 0 to 12. An individual with normal nutritional status would have a CONUT score of 0, with higher scores indicating worse nutritional status.
GNRI was calculated from serum albumin and body weight and height obtained on hospital admission, as previously described: GNRI = 14.89 × serum albumin (g/dl) + 41.7 × (actual body weight/ideal body weight). Actual body weight/ideal body weight was set to 1 when the body weight of the patient exceeded the ideal body weight. Ideal body weight in the present study was calculated using a body mass index (BMI) of 22 kg/m2, because of its validity [20], instead of the value calculated using the Lorentz formula in the original GNRI equation [7].
Baseline PNI was calculated as 10 × serum albumin (g/dl) + 0.005 × total lymphocyte count (per mm3) [9]. Data for these components were collected in the morning on the day of PCI.
Risk of malnutrition was defined as present when the patient showed CONUT score ≥ 3, GNRI < 98 or PNI < 45 [7, 9, 21]. We gave these patients 1 point for each criterion met, and this total was considered the Combined Objective Nutritional Score (e.g., a patient with a CONUT score of 2, a GNRI of 97 and a PNI of 43 would have a Combined Objective Nutritional Score of 2 points). Patients were divided into three groups according to this combined assessment score as: Group 1, normal nutritional status (0 points); Group 2, mild-to-moderate malnutrition (1–2 points); and Group 3, severe malnutrition (3 points).
Statistical analysis
Quantitative data are presented as mean ± standard deviation or median and interquartile range (IQR). Categorical variables are presented as frequencies. Continuous variables across groups were compared using one-way analysis of variance or the Kruskal–Wallis test. Categorical variables (presented as frequencies) were compared using the Chi-squared test. Unadjusted cumulative event rates were estimated using Kaplan–Meier curves and compared across groups. Cox proportional hazards models were used to assess uni- and multivariate covariates. Hazard ratios (HRs) and confidence intervals (CIs) were calculated for each factor by Cox proportional hazards analysis. Three Cox multivariate models were used: Model 1, unadjusted; Model 2, adjusted for age and sex; and Model 3, adjusted for the variables in Model 2 plus CKD, current smoker status, diabetes mellitus, family history of CAD, hypertension, LVEF and statin use. Differences were considered significant at the level of p < 0.05. Statistical analyses were performed using JMP version 12.0 software (SAS Institute, Cary, NC, USA).
Results
Prevalence of malnutrition in patients with stable CAD
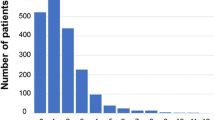
Of the 2092 patients who underwent elective PCI, pre-procedural CONUT score, GNRI and PNI data were available for 1984 patients (94.8%). For these patients, median CONUT score was 1 (IQR 0, 2), median GNRI was 101.3 (IQR 96.8, 105.7) and median PNI was 48.9 (IQR 45.4, 48.9). Figure 1a, c, e shows the distribution of each Objective Nutritional Index. Using these indices as a screening tool for malnutrition, 21–28% of patients were at risk of malnutrition [CONUT score ≥ 3, 421 patients (21.2%); GNRI < 98, 562 patients (28.3%); and PNI < 45, 459 patients (23.1%)]. Using these data, the Combined Objective Nutritional Score was calculated and patients were divided into 3 groups: Group 1, 1226 patients (61.8%); Group 2, 514 patients (25.9%); and Group 3, 244 patients (12.3%) (Table 1).
Distribution of objective nutritional indices and Kaplan–Meier curves for all-cause death. a Distribution of CONUT score. b Kaplan–Meier curves stratified by CONUT score (0–2 vs. 3–12). c Distribution of GNRI. d Kaplan–Meier curves stratified by GNRI levels (≥ 98 vs. < 98). e Distribution of PNI. f Kaplan–Meier curves for all-cause death stratified by PNI levels (≥ 45 vs. < 45). Median CONUT score, GNRI and PNI were 1 (IQR 0, 2), 101.3 (IQR 96.8, 105.7) and 48.9 (IQR 45.5, 48.9), respectively. Kaplan–Meier curves showed that the incidence of death was significantly higher in malnourished patients assessed using each Objective Nutritional Index than in those who were not (log rank test, all p < 0.0001). CONUT controlling nutritional status, GNRI Geriatric Nutritional Risk Index, PNI Prognostic Nutritional Index
Baseline and procedural characteristics
Clinical and procedural characteristics of the patients are shown in Table 2. Patients with worse nutritional status were significantly older and showed a higher prevalence of diabetes mellitus, multivessel coronary disease and CKD, as well as lower LDL-C, HDL-C, triglycerides and LVEF. Patients in this group were also less likely to be current smokers or to have been receiving treatment using statins on admission.
Clinical outcomes
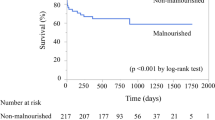
Median duration of follow-up was 7.4 years (IQR 4.6–10.1 years). In total, 293 (frequency, 14.8%) all-cause deaths were identified during follow-up, including 92 (4.6%) cases of cardiac death. All-cause deaths among patients stratified by nutritional status using CONUT score, GNRI and PNI are presented in Fig. 1b, d, f. Kaplan–Meier curves showed that the incidence of death was significantly higher in malnourished patients assessed using each Objective Nutritional Index than in those who were not (log rank test, p < 0.0001 each). Furthermore, Kaplan–Meier analysis also showed that cumulative incidences of all-cause death and cardiac death increased clearly and significantly with worse nutritional status among patients stratified by Combined Objective Nutritional Score (log rank test, both p < 0.0001; Fig. 2).
Kaplan–Meier curves for cardiovascular events stratified using the Combined Objective Nutritional Index. a Kaplan–Meier curves for all-cause death. b Kaplan–Meier curves for cardiac death. Kaplan–Meier analysis showed that cumulative incidences of all-cause death and cardiac death increased clearly and significantly with worse nutritional status among patients stratified by Combined Objective Nutritional Score (log-rank test, both p < 0.0001)
Table 3 shows Cox proportional hazard analyses for all-cause death and cardiac death. In unadjusted Cox modeling (Model 1), rate of all-cause death and cardiac death rose progressively with groups of worse nutritional status (both p < 0.0001 for trend). After adjustment for age and sex, Model 2 yielded similar results. Patients in Group 2 and Group 3 were significantly associated with all-cause death and cardiac death compared with patients in Group 1. Even after adjusting for age, sex and other risk factors (Model 3), patients with a Combined Objective Nutritional Score of 3 (Group 3) displayed a 2.91-fold (95% CI 2.10–4.00; p < 0.0001) and 2.16-fold (95% 1.15–3.92; p = 0.02) increase in risk of mortality and cardiac mortality compared with those with a Combined Objective Nutritional Score of 0 (Group 1).
Discussion
The major findings of the present study were as follows: (1) patients with worse nutritional status tended to show worse clinical characteristics, such as advanced age or higher prevalences of diabetes mellitus or CKD; (2) malnourished patients assessed by each Objective Nutritional Index (CONUT score, GNRI and PNI) displayed higher mortality than those without malnutrition; (3) the Combined Objective Nutritional Score effectively stratified CAD patients, and patients with worse malnutrition had significantly higher risks of all-cause death and cardiac death than those without malnutrition, even after adjusting for other risk factors.
Malnutrition is not rare, but represents a crucial issue for aged or hospitalized patients. Malnutrition has been reported to be related to worse clinical outcomes in patients with end-stage renal failure, cancer, heart failure and myocardial infarction (MI) [14, 22,23,24]. To date, several nutritional markers have been reported, including lymphocyte count, serum albumin levels, total cholesterol, the Mini-Nutritional Assessment (MNA) [25], the Subjective Global Assessment (SGA) [26], CONUT score, GNRI or PNI. Underweight status has also been reported as related to worse nutritional status and a greater risk of cardiovascular events [27]. The MNA or SGA require subjective assessment, which might be affected by medical staff and their experience. In addition, obtaining these data is not easy in daily clinical situations. Single blood parameters or bodyweight are easy to use and assess, but assessments using only one indicator may be affected by various factors. CONUT score, GNRI and PNI each use two or three objective parameters to evaluate different aspects of nutritional conditions. Calculating these indices using inexpensive markers is simple and easy. However, these indices are calculated using different methods and components, and each has specific advantages and disadvantages. First, GNRI is usually calculated by serum albumin and BMI, but may underestimate malnutrition in patients with a normal or larger BMI. PNI is calculated by serum albumin and lymphocyte count. Basta et al. assessed the prognostic value of CONUT score and PNI in patients with ST-elevation MI, but PNI was not associated with increased risk of cardiovascular events [22]. CONUT score is calculated from three blood parameters (serum albumin, total cholesterol and lymphocyte count), offering an advantage over other objective indices using two parameters. However, patients with CAD are recommended to be treated with statin therapy, so total cholesterol level may not be an appropriate nutritional marker for CAD patients. The present study assessed nutritional status using these three objective nutritional indices, finding that those patients assessed as showing poor nutrition experienced a higher incidence of all-cause death. Furthermore, patients with worse nutritional status evaluated using the Combined Objective Nutritional Score were at significantly higher risk of not only all-cause death, but also cardiac death. To the best of our knowledge, this is first study to evaluate the association between malnutrition and long-term cardiac mortality. Our findings indicate that nutritional assessment using this novel combined score should be taken into consideration in patients who have undergone PCI.
Malnutrition is a complex state comprising reductions in protein reserves, caloric collapse, and weakening of the immune defenses. In patients with chronic diseases such as heart failure, malnutrition affects the natural evolution of the disease and the disease in turn affects the nutritional status. This relationship in heart failure has been explained as part of the “vicious circle” of chronic heart failure [10]. A previous study reported that malnutrition was significantly associated with higher concentrations of inflammatory markers and carotid atherosclerosis in patients with chronic heart failure [28]. A relationship between malnutrition and atherosclerosis was also reported in CAD patients. Ko et al. showed that relative muscle mass was negatively associated with prevalence of coronary calcification [29]. Furthermore, serum albumin is one of the components of CONUT score, GNRI and PNI. Although serum albumin is usually used as a nutritional marker, albumin levels are influenced by factors such as synthesis, clearance, and dilution. Under inflammatory conditions, serum albumin concentration is affected by decreased hepatic synthesis, increased leakage into the interstitial space, and catabolism [30]. In addition to the inflammatory factor, antioxidant properties of serum albumin have been reported [31]. Increased oxidative stress represents an important pathogenic factor in cardiovascular disease. These mechanisms might influence the association between malnutrition and cardiovascular outcomes in the present study. CONUT score, GNRI and PNI are calculated by serum albumin level as one of the components. Thus, the combined score might be mainly influenced by serum albumin level. However, other components such as total lymphocyte counts, total cholesterol level and BMI, also affected clinical outcomes among patients in the present study. Univariate Cox hazard analysis for mortality showed that each component was associated with clinical outcomes (not shown in the result).
Our results suggest that evaluation of nutritional status might be useful for risk stratification of stable CAD patients. However, few nutritional intervention studies have investigated CAD patients with poor nutritional status. A future task is thus to clarify what medical treatments or nutritional interventions can improve the prognosis of such patients.
This study has several limitations. First, as a single-center, observational study of a small patient cohort, unknown confounding factors might have affected the outcomes, regardless of analytical adjustments. Second, the nutritional status of patients was evaluated only once in the present study; changes over time during the follow-up period were not assessed.
In conclusion, nutritional status evaluated by three objective nutritional indices; CONUT score, GNRI and PNI, was associated with long-term outcomes in stable CAD patients treated with PCI. In addition, the Combined Objective Nutritional Score effectively stratified these populations and patients evaluated as showing a poorer nutritional condition exhibited a higher risk of cardiovascular events.
References
Lin H, Zhang H, Lin Z, Li X, Kong X, Sun G (2016) Review of nutritional screening and assessment tools and clinical outcomes in heart failure. Heart Fail Rev 21:549–565
Kalantar-Zadeh K, Anker SD, Horwich TB, Fonarow GC (2008) Nutritional and anti-inflammatory interventions in chronic heart failure. Am J Cardiol 101:89E–103E
Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, Gonzalez-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P (2016) 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J 37:2129–2200
Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE Jr, Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 62:e147–e239
Bonilla-Palomas JL, Gamez-Lopez AL, Castillo-Dominguez JC, Moreno-Conde M, Lopez Ibanez MC, Alhambra Exposito R, Ramiro Ortega E, Anguita-Sanchez MP, Villar-Raez A (2016) Nutritional intervention in malnourished hospitalized patients with heart failure. Arch Med Res 47:535–540
Ignacio de Ulibarri J, Gonzalez-Madrono A, de Villar NG, Gonzalez P, Gonzalez B, Mancha A, Rodriguez F, Fernandez G (2005) CONUT: a tool for controlling nutritional status. First validation in a hospital population. Nutr Hosp 20:38–45
Bouillanne O, Morineau G, Dupont C, Coulombel I, Vincent JP, Nicolis I, Benazeth S, Cynober L, Aussel C (2005) Geriatric Nutritional Risk Index: a new index for evaluating at-risk elderly medical patients. Am J Clin Nutr 82:777–783
Buzby GP, Mullen JL, Matthews DC, Hobbs CL, Rosato EF (1980) Prognostic nutritional index in gastrointestinal surgery. Am J Surg 139:160–167
Onodera T, Goseki N, Kosaki G (1984) Prognostic nutritional index in gastrointestinal surgery of malnourished cancer patients. Nihon Geka Gakkai Zasshi 85:1001–1005
Agra Bermejo RM, Gonzalez Ferreiro R, Varela Roman A, Gomez Otero I, Kreidieh O, Conde Sabaris P, Rodriguez-Manero M, Moure Gonzalez M, Seoane Blanco A, Virgos Lamela A, Garcia Castelo A, Gonzalez Juanatey JR (2017) Nutritional status is related to heart failure severity and hospital readmissions in acute heart failure. Int J Cardiol 230:108–114
Nishi I, Seo Y, Hamada-Harimura Y, Sato K, Sai S, Yamamoto M, Ishizu T, Sugano A, Obara K, Wu L, Suzuki S, Koike A, Aonuma K (2017) Nutritional screening based on the controlling nutritional status (CONUT) score at the time of admission is useful for long-term prognostic prediction in patients with heart failure requiring hospitalization. Heart Vessels 32:1337–1349
Shirakabe A, Hata N, Kobayashi N, Okazaki H, Matsushita M, Shibata Y, Nishigoori S, Uchiyama S, Asai K, Shimizu W (2018) The prognostic impact of malnutrition in patients with severely decompensated acute heart failure, as assessed using the Prognostic Nutritional Index (PNI) and Controlling Nutritional Status (CONUT) score. Heart Vessels 33:134–144
Cheng YL, Sung SH, Cheng HM, Hsu PF, Guo CY, Yu WC, Chen CH (2017) Prognostic nutritional index and the risk of mortality in patients with acute heart failure. J Am Heart Assoc 6:e004876
Honda Y, Nagai T, Iwakami N, Sugano Y, Honda S, Okada A, Asaumi Y, Aiba T, Noguchi T, Kusano K, Ogawa H, Yasuda S, Anzai T (2016) Usefulness of geriatric nutritional risk index for assessing nutritional status and its prognostic impact in patients aged ≥65 years with acute heart failure. Am J Cardiol 118:550–555
Chen QJ, Qu HJ, Li DZ, Li XM, Zhu JJ, Xiang Y, Li L, Ma YT, Yang YN (2017) Prognostic nutritional index predicts clinical outcome in patients with acute ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Sci Rep 7:3285
Wada H, Dohi T, Miyauchi K, Doi S, Konishi H, Naito R, Tsuboi S, Ogita M, Kasai T, Okazaki S, Isoda K, Suwa S, Daida H (2017) Prognostic impact of nutritional status assessed by the Controlling Nutritional Status score in patients with stable coronary artery disease undergoing percutaneous coronary intervention. Clin Res Cardiol 106:875–883
Wada H, Dohi T, Miyauchi K, Doi S, Naito R, Konishi H, Tsuboi S, Ogita M, Kasai T, Hassan A, Okazaki S, Isoda K, Suwa S, Daida H (2017) Prognostic impact of the geriatric nutritional risk index on long-term outcomes in patients who underwent percutaneous coronary intervention. Am J Cardiol 119:1740–1745
Teramoto T, Sasaki J, Ishibashi S, Birou S, Daida H, Dohi S, Egusa G, Hiro T, Hirobe K, Iida M, Kihara S, Kinoshita M, Maruyama C, Ohta T, Okamura T, Yamashita S, Yokode M, Yokote K (2013) Diagnostic criteria for dyslipidemia. J Atheroscler Thromb 20:655–660
Matsuo S, Imai E, Horio M, Yasuda Y, Tomita K, Nitta K, Yamagata K, Tomino Y, Yokoyama H, Hishida A, Collaborators developing the Japanese equation for estimated GFR (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53:982–992
Shah B, Sucher K, Hollenbeck CB (2006) Comparison of ideal body weight equations and published height-weight tables with body mass index tables for healthy adults in the United States. Nutr Clin Pract 21:312–319
Nochioka K, Sakata Y, Takahashi J, Miyata S, Miura M, Takada T, Fukumoto Y, Shiba N, Shimokawa H (2013) Prognostic impact of nutritional status in asymptomatic patients with cardiac diseases: a report from the CHART-2 Study. Circ J 77:2318–2326
Basta G, Chatzianagnostou K, Paradossi U, Botto N, Del Turco S, Taddei A, Berti S, Mazzone A (2016) The prognostic impact of objective nutritional indices in elderly patients with ST-elevation myocardial infarction undergoing primary coronary intervention. Int J Cardiol 221:987–992
Seo SH, Kim SE, Kang YK, Ryoo BY, Ryu MH, Jeong JH, Kang SS, Yang M, Lee JE, Sung MK (2016) Association of nutritional status-related indices and chemotherapy-induced adverse events in gastric cancer patients. BMC Cancer 16:900
Takahashi H, Ito Y, Ishii H, Aoyama T, Kamoi D, Kasuga H, Yasuda K, Maruyama S, Matsuo S, Murohara T, Yuzawa Y (2014) Geriatric nutritional risk index accurately predicts cardiovascular mortality in incident hemodialysis patients. J Cardiol 64:32–36
Guigoz Y, Vellas B, Garry PJ (1996) Assessing the nutritional status of the elderly: the Mini Nutritional Assessment as part of the geriatric evaluation. Nutr Rev 54:S59–S65
Detsky AS, McLaughlin JR, Baker JP, Johnston N, Whittaker S, Mendelson RA, Jeejeebhoy KN (1987) What is subjective global assessment of nutritional status? JPEN J Parenter Enteral Nutr 11:8–13
Kalantar-Zadeh K, Block G, Horwich T, Fonarow GC (2004) Reverse epidemiology of conventional cardiovascular risk factors in patients with chronic heart failure. J Am Coll Cardiol 43:1439–1444
Nakagomi A, Kohashi K, Morisawa T, Kosugi M, Endoh I, Kusama Y, Atarashi H, Shimizu W (2016) Nutritional status is associated with inflammation and predicts a poor outcome in patients with chronic heart failure. J Atheroscler Thromb 23:713–727
Ko BJ, Chang Y, Jung HS, Yun KE, Kim CW, Park HS, Chung EC, Shin H, Ryu S (2016) Relationship between low relative muscle mass and coronary artery calcification in healthy adults. Arterioscler Thromb Vasc Biol 36:1016–1021
von Haehling S, Doehner W, Anker SD (2007) Nutrition, metabolism, and the complex pathophysiology of cachexia in chronic heart failure. Cardiovasc Res 73:298–309
Roche M, Rondeau P, Singh NR, Tarnus E, Bourdon E (2008) The antioxidant properties of serum albumin. FEBS Lett 582:1783–1787
Acknowledgements
We are grateful to the staff of the Department of Cardiovascular Medicine at Juntendo University and the Department of Cardiology at Juntendo University Shizuoka Hospital. We also appreciate the secretarial assistance of Yumi Nozawa.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Wada, H., Dohi, T., Miyauchi, K. et al. Combined effect of nutritional status on long-term outcomes in patients with coronary artery disease undergoing percutaneous coronary intervention. Heart Vessels 33, 1445–1452 (2018). https://doi.org/10.1007/s00380-018-1201-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-018-1201-x