Abstract
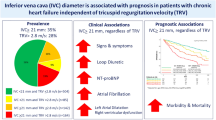
Inferior vena cava (IVC) diameter can be used to approximate right atrial pressure in patients admitted for acute decompensated heart failure (ADHF). Recent studies linked IVC dilation to an increased risk of early re-admission and short-term mortality. Moreover, renal insufficiency (RI) is an established risk factor for mortality in ADHF and is associated with congestion. We hypothesized that the IVC diameter is a marker of all-cause mortality but its prognostic impact may be influenced by kidney function. We analyzed data of 1101 patients admitted for ADHF with available echocardiography of the IVC by chart review and death registry linkage. Patients were dichotomized according to a cut-off value of 21 mm. Cox proportional hazards model was used to identify mortality predictors. A dilated IVC was detected in 474 (43.1%) patients. Overall, 400 (36.3%) patients died within 3 years. All-cause mortality was significantly higher in patients with dilated IVC [hazard ratio 1.45 (confidence interval 1.21–1.74); p < 0.001]. However, a dilated IVC was only associated with all-cause mortality in patients with RI function [hazard ratio 1.60 (confidence interval 1.26–2.03); p < 0.001] but not in patients with a preserved kidney function [hazard ratio 1.04 (confidence interval 0.72–1.50); P = 0.84]. IVC diameter was identified as an independent predictor for all-cause mortality in a Cox proportional hazards model with a significant interaction between IVC diameter and baseline kidney function. In conclusion, IVC dilation is a marker of high mortality risk in patients admitted for ADHF. However, this observation was confined to patients with RI.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Since 2006, heart failure is the most common reason for hospital admissions in Germany [1]. Around 25% of patients will be re-hospitalized within 30 days after discharge, and the risk of death is considerably increased over a prolonged period compared to heart failure patients who have never been hospitalized [2]. In patients admitted due to acute decompensated heart failure (ADHF), the degree of congestion is of prognostic relevance [3]. Since even subclinical congestion at discharge is a risk factor for early re-admission and mortality [4, 5], detailed assessment of congestion is crucial for optimal treatment. However, clinical signs and/or symptoms of heart failure-related congestion are insensitive and unspecific [6]. Congestion in the absence of clinical signs and symptoms is called hemodynamic congestion. According to a scientific statement of the European Society of Cardiology, the reference standard for evaluation of hemodynamic congestion is cardiac catheterization to measure right atrial pressure (RAP) and pulmonary capillary wedge pressure [7]. However, cardiac catheterization is invasive and may not be appropriate to routinely assess congestion during treatment. Published data support approximation of RAP using the inferior vena cava (IVC) diameter [8, 9]. Of note, data from small studies indicate that IVC dilation may be associated with early re-admission in patients hospitalized for ADHF [10, 11]. In addition, renal insufficiency (RI) is also associated with worse prognosis [12] and congestion itself is related to RI [13, 14]. Therefore, the aim of this study was to determine the prognostic impact of IVC dilation in regard to long-term mortality and its dependency on kidney function.
Methods
We identified cases with the primary discharge diagnosis of heart failure according to the ICD-10 (International Statistical Classification of Diseases and Related Health Problems, 10th revision, German Modification) code I50.* treated in our department for at least 3 days between April 1, 2008, and December 31, 2014. Only the first hospitalization, i.e., index hospitalization, was analyzed from patients hospitalized twice or more. ADHF due to left-sided heart failure as primary cause for hospital admission was evaluated by chart review and patients with primary right-heart failure were omitted. The study was approved by the ethical review committee of the University of Lübeck.
Baseline characteristics like age, gender, date of admission, date of discharge, and lab values were extracted from the hospital information system. Comorbidities and discharge medications were obtained by reviewing digital discharge letters. Echocardiography was performed 1 (0–3) days after admission. The maximum and minimum IVC diameter (IVCmax and IVCmin, respectively) was retrospectively determined by one investigator (KB). For this purpose, stored echocardiography images were loaded and analyzed using Xcelera software (version 1.2.4 until 2013-02-18, thereafter version 4.1.1; Philips, Best, The Netherlands). The investigator was blinded to all other available data, especially clinical endpoints. Other echocardiography parameters were obtained by reviewing individual echocardiography reports. An IVCmax of more than 21 mm together with an inspiratory collapse of less than 50% indicates high RAP according to current guidelines (Table 1) [9]. The inspiratory collapse is expressed as IVC collapsibility index (IVCCI), which was calculated as (IVCmax − IVCmin)/IVCmax. The IVC was termed “dilated”, when IVCmax was above 21 mm. As in previous studies, 20 mg of torasemide was defined as being equivalent to 40 mg of furosemide. Patients were considered to have heart failure with reduced ejection fraction (HFrEF) when the echocardiography report stated that the ejection fraction was moderately or severely reduced. According to the 2005 recommendations for chamber quantification [15], this translates to an ejection fraction of <45% which is close to ≤40% stated in the current ACCF/AHA Heart Failure guidelines for the HFrEF definition [16]. An estimated glomerular filtration rate below 60 ml/min/1.73 m2 according to Modification of Diet in Renal Disease Study equation (eGFR) [17] was defined as RI. Worsening renal function (WRF) was defined as increase in creatinine concentration of ≥1.5-times from baseline or ≥26.5 µmol/l within 48 h as recently suggested [18].
The primary endpoint of all-cause mortality was assessed via the death registry of the state Schleswig–Holstein. For patients who did not die, the end of follow-up was defined as the latest documented event, i.e., either discharge from index hospitalization, discharge from the last local hospitalization in the University Hospital of Lübeck, or date of the successful death registry query.
The study population was dichotomized in patients with an IVCmax of ≤21 and >21 mm. Categorical patient characteristics were summarized as frequencies and compared using Fisher’s exact test. Continuous variables were summarized as median with interquartile range (IQR) and compared using Wilcoxon rank-sum test. Stepwise multivariable logistic regression analysis was performed to identify predictors for IVC dilation. Analogously, predictors for all-cause mortality were identified by means of stepwise multivariable Cox regression analysis. Before each stepwise regression analysis, univariable pre-selection of candidate predictors was performed considering all baseline and echocardiography parameters listed in Table 2 with less than 15% missing values. The inclusion criterion for multivariable analysis was a p < 0.05 in univariable analysis. The cumulative mortality rate was visualized by means of a Kaplan–Meier plot and compared using log-rank test. Previous studies observed an association between different congestion surrogates with kidney function [19]; therefore, we tested the statistical interaction between IVCmax and eGFR in the final Cox proportional hazard model. Predicted hazard ratios (HR) were plotted against the linearly coded IVCmax for different eGFR offsets to visualize the interaction between IVCmax and baseline kidney function. All statistical tests were two-sided and considered significant if p < 0.05. All statistical analyses were done using the software statistical language R (http://www.r-project.org; version 3.1.3).
Results
In total, 3373 cases with the primary diagnosis of heart failure were identified. Of these, 2598 were index hospitalizations of unique patients. The final study population consisted of 1101 patients with ADHF due to left-sided heart failure and available echocardiography of the IVC. An IVCmax > 21 mm was found in 474 (43.1%) patients. Median IVCmax was 20 (IQR 16–24) mm in the total population. Patients with an IVCmax > 21 mm and IVCmax ≤ 21 had a median IVC diameter of 25 (IQR 23–27) and 17 (IQR 14–19) mm, respectively. In 628 (56%) patients, echocardiography loops of the IVC, facilitating distinction between IVCmax and IVCmin, were available. IVCmin was 15 (IQR 10–20) mm in the total population with 10 (IQR 6–14) mm and 20 (IQR 16–23) mm in patients with an IVCmax ≤ 21 mm and >21 mm, respectively. The IVCCI was less in patients with an IVCmax > 21 mm than in IVCmax ≤ 21 mm (22% (IQR 13–36) versus 34% (IQR 22–56), respectively; p < 0.001). According to the current echocardiography guidelines (IVCmax > 21 mm plus IVCCI < 50%) [9], 87% of patients with an IVCmax > 21 mm and available IVCmin value were defined as having high RAP.
Baseline characteristics are presented in Table 2. With regard to IVC diameter, patient groups had a similar age and, with the exception of the presence of atrial fibrillation, comorbidity profile. However, patients with a dilated IVC seem to be sicker with regard to several echocardiography and laboratory characteristics. Moreover, in-hospital treatment was longer in these patients and they were discharged with a higher loop diuretic dose. Baseline RI was associated with higher incidence of coronary artery disease-related comorbidities.
Regression analysis was performed to assess predictors for IVC dilation. Candidates with significant effect in univariable analyses were included in stepwise backward selections. The final model is shown in Table 3.
Overall, 400 (36.3%) patients died within 3 years after admission to the index hospitalization. The median follow-up was 14 (IQR 6–33) months. In the total population, mortality was 5.5, 18.1, and 25.4% after 30, 180, and 365 days, respectively. An IVCmax > 21 mm and eGFR < 60 ml/min/1.73 m2 were associated with increased all-cause mortality (HR 1.45, 95% CI 1.21–1.74 and HR 2.03, 95% CI 1.67–2.48, respectively; p < 0.001 for both; Fig. 1). After univariable pre-selection and stepwise backward selection, IVCmax remained significantly associated in a multivariable Cox regression model for all-cause mortality (HR per mm IVCmax increase 1.03, 95% CI 1.01–1.05; p = 0.001; Table 4). The addition of an interaction term for linearly coded IVCmax and eGFR revealed that this interaction is statistically significant (p = 0.03 for interaction) and improved the predictive information of the model (p = 0.03 by log likelihood ratio test). Moreover, the predicted HR progressively increased when eGFR declined (Fig. 2). Considering IVC diameter dichotomized (IVCmax > 21 mm versus IVCmax ≤ 21 mm), IVC dilation was only significantly associated with all-cause mortality in patients with an eGFR < 60 ml/min/1.73m² (HR 1.60, 95% CI 1.26–2.03; p < 0.001) but not in patients with an eGFR ≥ 60 ml/min/1.73m² (HR 1.04, 95% CI 0.72–1.50; p = 0.84; p = 0.047 for interaction between IVC dilation and RI). A four-strata Kaplan–Meier curve visualizes this finding (Fig. 3).
Predicted hazard ratios from a multivariable model over the 10–90% interquartile range for different baseline eGFRs. The hazard ratio of 1 was arbitrarily set to maximal inferior vena cava diameter (IVCmax) of 20 mm and an estimated glomerular filtration rate (eGFR) of 60 ml/min/1.73m². Covariates considered in the multivariable model are listed in Table 4
Discussion
Our study demonstrates that IVCmax-assessed congestion is associated with all-cause mortality. However, this association is influenced by baseline kidney function.
ADHF is a sentinel event with a detrimental impact on prognosis. In patients with chronic heart failure, the mortality risk is considerably increased after hospitalization compared to patients never hospitalized [2]. Large registries reported mortality rates of approximately 12 and 30% after 30 days and 1 year, respectively [20]. However, in the RELAX-AHF placebo group, mortality rate was only 3.3 and 11.3% after 30 and 180 days, respectively [21]. In our cohort, mortality rates were in between, i.e., 5.5, 18.1, and 25.4% after 30, 180, and 365 days, respectively (Fig. 1).
According to the baseline characteristics, patients with dilated IVC had more advanced heart failure. Regression modeling identified male sex, atrial fibrillation, tricuspid regurgitation, heart failure with reduced ejection fraction, and a low hemoglobin level at baseline as predictors for IVC dilation. From a pathophysiological point of view, atrial fibrillation and HFrEF may facilitate congestion, whereas the severity of tricuspid regurgitation and the hemoglobin level may also indicate the grade of congestion. The statistical association of male sex is more puzzling. In general, males are taller than females and it would be intuitive that their IVC is wider. However, height did not correlate with IVC diameter in a large study [22], nor is normalization to height recommended by current guidelines for the interpretation of IVC diameter because it did not improve prediction of IVC consistently in studies building the foundation for these guidelines [9]. Since moderate to severe tricuspid regurgitation was more common in patients with dilated IVC, we suggest that, in principle, both can be used for assessment of prognosis in patients with left-sided heart failure. Both are a read-out for the level of advanced left-sided heart failure-related congestion [23], and secondary right-sided heart failure is known to be marker of worse prognosis in left-sided heart failure [24].
Congestion has also been identified as an important prognostic factor. Clinical congestion at discharge as well as commonly used markers of decongestion during diuretic treatment (i.e., weight loss and fluid loss) have additionally been linked to prognosis [4, 25]. Unfortunately, clinical congestion markers are rather unspecific for heart failure [6, 7]; weight and fluid loss are difficult to assess and often inconsistent [26]. Measuring RAP and pulmonary capillary wedge pressure by means of right heart catheterization is considered the reference standard for assessment of hemodynamic congestion [7]. But right heart catheterization is invasive, cost-intensive and not suitable for repetitive measurements during decongestion. Instead, IVCmax and IVCCI can appropriately be used to estimate RAP semi-quantitatively (i.e., high, intermediate, or normal) rather than to estimate a precise numeric pressure value [8, 9]. Patients with an IVCmax > 21 mm, assumed to have a high RAP, had an increased mortality risk compared to patients with an IVCmax ≤ 21 mm. Our finding is in line with two smaller prospective studies demonstrating that the IVC diameter was larger at admission and at discharge in ADHF patients who were re-hospitalized within 30 days [10] and that patients with an IVCmax > 21 mm had less event-free survival (i.e., death or ADHF re-hospitalization) compared to patients with an IVC ≤ 21 mm [27]. In addition, two studies found an association of IVC dilation with long-term prognosis in patients with chronic heart failure [22, 28]. Very recently, two small prospective studies also linked IVC dilation in ADHF patients to an increased mortality risk [29, 30]. All these data are conclusive and point out that the IVC diameter is a marker of prognosis in heart failure patients and this holds true not only for IVC diameters measured after diuretic decongestion but also for admission diameters [10]. A randomized controlled trial is warranted to assess whether the IVC diameter can be used in addition to clinical congestion assessment to improve decongestion or whether the IVC diameter serves solely as marker to identify patients with advanced disease and, hence, worse prognosis.
As reviewed recently, several studies considering different congestion surrogates (i.e., RAP, central venous pressure, or abdominal pressure) found an association between congestion and renal impairment [19]. In line with these data, patients with IVC dilation had also RI in our study. In a multivariable Cox regression model, we found a significant interaction between eGFR and IVCmax. This interaction led to progressively higher predicted hazard ratios with increasing IVCmax while eGFR attenuates. After dichotomization of IVCmax and eGFR at clinically meaningful cut-offs, IVC dilation was only significantly associated with all-cause mortality in patients with an impaired but not in patients with preserved kidney function. This finding was also supported by the finding that in a three covariate Cox model containing IVC dilation, RI, and their interaction term, only the latter two were significantly associated with mortality. Although this does not verify a biological interaction or provide mechanistic insight, our observation fits well in the evolving picture. For example, this finding is supported by the results of a recent study which found a similar interaction between persistent clinical congestion and worsening renal function [31]. Pathophysiologically, systemic congestion may increase renal venous pressure and thereby reduce renal arteriovenous pressure gradient which, in turn, may reduce renal blood flow. This is supported by the finding of a recent study that intrarenal venous flow assessed by means of intrarenal Doppler ultrasonography was dependent on RAP rather than resistance index [32]. Viewed from the other site, RI may lead to systemic congestion itself and impede diuretic decongestion substantially. One can speculate that patients with pronounced congestion can quite well be decongested as long as kidney function is preserved. However, when kidney function is impaired, sufficient decongestion is difficult and even may not be possible by conventional diuretic treatment [33, 34]. In line with this, Matsue et al. observed that high-dose furosemide was associated with an increase in in-hospital mortality risk in patients with RI but not in patients with preserved kidney function [35]. Either way, prognosis worsens with increasing congestion and decreasing eGFR. With regard to eGFR, chronic kidney disease is defined as eGFR < 60 ml/min/1.73m² present for more than 3 months and is highly prevalent in the elderly [36]. However, a baseline eGFR < 60 ml/min/1.73m² in our study might not reflect chronic kidney disease for which reason we chose to call it RI.
Due to the registry design aspects, our study has several limitations. First, neither the time point of the IVC evaluation nor the evaluation itself was standardized. However, the IVC diameter was determined retrospectively from prospectively collected data by a single investigator according to guideline recommendations. Second, several interesting characteristics were not recorded at all or had many missing values and, therefore, cannot be considered as covariate in our regression model (for example, blood pressure, heart rate, IVCCI, urea, NT-proBNP, clinical signs/symptoms of heart failure, and ejection fraction as continuous variable). Serial measurements of IVC diameter are not available; therefore, it is not possible to make a statement regarding the ability for decongestion of patients with preserved and impaired kidney function. Finally, all presented analyses have to be interpreted as exploratory and hypothesis-generating.
In conclusion, the IVC diameter is a marker of all-cause mortality in patients admitted for ADHF. However, this finding was confined to patients with RI since IVC dilation was not associated with an increased mortality risk in patients with preserved kidney function.
Abbreviations
- ADHF:
-
Acute decompensated heart failure
- CI:
-
Confidence interval
- eGFR:
-
Estimated glomerular filtration rate
- HFrEF:
-
Heart failure with reduced ejection fraction
- HR:
-
Hazard ratio
- IVC:
-
Inferior vena cava
- IVCCI:
-
IVC collapsibility index
- IVCmax:
-
Maximum IVC diameter
- IVCmin:
-
Minimum IVC diameter
- RI:
-
Renal insufficiency
- WRF:
-
Worsening renal function
References
Neumann T, Biermann J, Erbel R, Neumann A, Wasem J, Ertl G, Dietz R (2009) Heart failure: the commonest reason for hospital admission in Germany: medical and economic perspectives. Dtsch Arztebl Int 106(16):269–275
Solomon SD, Dobson J, Pocock S, Skali H, McMurray JJ, Granger CB, Yusuf S, Swedberg K, Young JB, Michelson EL, Pfeffer MA, Candesartan in Heart failure: Assessment of Reduction in M, morbidity I (2007) Influence of nonfatal hospitalization for heart failure on subsequent mortality in patients with chronic heart failure. Circulation 116 (13):1482–1487
Drazner MH, Rame JE, Stevenson LW, Dries DL (2001) Prognostic importance of elevated jugular venous pressure and a third heart sound in patients with heart failure. N Engl J Med 345(8):574–581
Ambrosy AP, Pang PS, Khan S, Konstam MA, Fonarow GC, Traver B, Maggioni AP, Cook T, Swedberg K, Burnett JC Jr, Grinfeld L, Udelson JE, Zannad F, Gheorghiade M, Investigators ET (2013) Clinical course and predictive value of congestion during hospitalization in patients admitted for worsening signs and symptoms of heart failure with reduced ejection fraction: findings from the EVEREST trial. Eur Heart J 34(11):835–843
Lala A, McNulty SE, Mentz RJ, Dunlay SM, Vader JM, AbouEzzeddine OF, DeVore AD, Khazanie P, Redfield MM, Goldsmith SR, Bart BA, Anstrom KJ, Felker GM, Hernandez AF, Stevenson LW (2015) Relief and recurrence of congestion during and after hospitalization for acute heart failure: insights from Diuretic Optimization Strategy Evaluation in Acute Decompensated Heart Failure (DOSE-AHF) and Cardiorenal Rescue Study in Acute Decompensated Heart Failure (CARESS-HF). Circ Heart Fail 8(4):741–748
Wang CS, FitzGerald JM, Schulzer M, Mak E, Ayas NT (2005) Does this dyspneic patient in the emergency department have congestive heart failure? JAMA 294(15):1944–1956
Gheorghiade M, Follath F, Ponikowski P, Barsuk JH, Blair JE, Cleland JG, Dickstein K, Drazner MH, Fonarow GC, Jaarsma T, Jondeau G, Sendon JL, Mebazaa A, Metra M, Nieminen M, Pang PS, Seferovic P, Stevenson LW, van Veldhuisen DJ, Zannad F, Anker SD, Rhodes A, McMurray JJ, Filippatos G, European Society of C, European Society of Intensive Care M (2010) Assessing and grading congestion in acute heart failure: a scientific statement from the acute heart failure committee of the heart failure association of the European Society of Cardiology and endorsed by the European Society of Intensive Care Medicine. Eur J Heart Fail 12 (5):423–433
Beigel R, Cercek B, Luo H, Siegel RJ (2013) Noninvasive evaluation of right atrial pressure. J Am Soc Echocardiogr 26(9):1033–1042
Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB (2010) Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr 23(7):685–713 (quiz 786–788)
Goonewardena SN, Gemignani A, Ronan A, Vasaiwala S, Blair J, Brennan JM, Shah DP, Spencer KT (2008) Comparison of hand-carried ultrasound assessment of the inferior vena cava and N-terminal pro-brain natriuretic peptide for predicting readmission after hospitalization for acute decompensated heart failure. JACC Cardiovasc Imaging 1(5):595–601
Carbone F, Bovio M, Rosa GM, Ferrando F, Scarrone A, Murialdo G, Quercioli A, Vuilleumier N, Mach F, Viazzi F, Montecucco F (2014) Inferior vena cava parameters predict re-admission in ischaemic heart failure. Eur J Clin Invest 44(4):341–349
Damman K, Valente MA, Voors AA, O’Connor CM, van Veldhuisen DJ, Hillege HL (2014) Renal impairment, worsening renal function, and outcome in patients with heart failure: an updated meta-analysis. Eur Heart J 35(7):455–469
Damman K, van Deursen VM, Navis G, Voors AA, van Veldhuisen DJ, Hillege HL (2009) Increased central venous pressure is associated with impaired renal function and mortality in a broad spectrum of patients with cardiovascular disease. J Am Coll Cardiol 53(7):582–588
Mullens W, Abrahams Z, Francis GS, Sokos G, Taylor DO, Starling RC, Young JB, Tang WH (2009) Importance of venous congestion for worsening of renal function in advanced decompensated heart failure. J Am Coll Cardiol 53(7):589–596
Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ, Chamber Quantification Writing G, American Society of Echocardiography’s G, Standards C, European Association of E (2005) Recommendations for chamber quantification: a report from the American Society of Echocardiography’s Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr 18 (12):1440–1463
Writing Committee M, Yancy CW, Jessup M, Bozkurt B, Butler J, Casey DE, Jr., Drazner MH, Fonarow GC, Geraci SA, Horwich T, Januzzi JL, Johnson MR, Kasper EK, Levy WC, Masoudi FA, McBride PE, McMurray JJ, Mitchell JE, Peterson PN, Riegel B, Sam F, Stevenson LW, Tang WH, Tsai EJ, Wilkoff BL, American College of Cardiology Foundation/American Heart Association Task Force on Practice G (2013) 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 128 (16):e240–327
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J, Ckd EPI (2009) A new equation to estimate glomerular filtration rate. Ann Intern Med 150(9):604–612
Damman K, Tang WH, Testani JM, McMurray JJ (2014) Terminology and definition of changes renal function in heart failure. Eur Heart J 35(48):3413–3416
Verbrugge FH, Dupont M, Steels P, Grieten L, Malbrain M, Tang WH, Mullens W (2013) Abdominal contributions to cardiorenal dysfunction in congestive heart failure. J Am Coll Cardiol 62(6):485–495
Kociol RD, Hammill BG, Fonarow GC, Klaskala W, Mills RM, Hernandez AF, Curtis LH (2010) Generalizability and longitudinal outcomes of a national heart failure clinical registry: Comparison of Acute Decompensated Heart Failure National Registry (ADHERE) and non-ADHERE Medicare beneficiaries. Am Heart J 160(5):885–892
Teerlink JR, Cotter G, Davison BA, Felker GM, Filippatos G, Greenberg BH, Ponikowski P, Unemori E, Voors AA, Adams KF Jr, Dorobantu MI, Grinfeld LR, Jondeau G, Marmor A, Masip J, Pang PS, Werdan K, Teichman SL, Trapani A, Bush CA, Saini R, Schumacher C, Severin TM, Metra M, Investigators REiAHF (2013) Serelaxin, recombinant human relaxin-2, for treatment of acute heart failure (RELAX-AHF): a randomised, placebo-controlled trial. The Lancet 381(9860):29–39
Pellicori P, Carubelli V, Zhang J, Castiello T, Sherwi N, Clark AL, Cleland JG (2013) IVC diameter in patients with chronic heart failure: relationships and prognostic significance. JACC Cardiovasc Imaging 6(1):16–28
Drazner MH, Hamilton MA, Fonarow G, Creaser J, Flavell C, Stevenson LW (1999) Relationship between right and left-sided filling pressures in 1000 patients with advanced heart failure. J Heart Lung Transplant 18(11):1126–1132
Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiery JL (2016) Left ventricular heart failure and pulmonary hypertension. Eur Heart J 37(12):942–954
Kociol RD, McNulty SE, Hernandez AF, Lee KL, Redfield MM, Tracy RP, Braunwald E, O’Connor CM, Felker GM, Committee NHFNS, Investigators (2013) Markers of decongestion, dyspnea relief, and clinical outcomes among patients hospitalized with acute heart failure. Circ Heart Fail 6(2):240–245
Testani JM, Brisco MA, Kociol RD, Jacoby D, Bellumkonda L, Parikh CR, Coca SG, Tang WH (2015) Substantial discrepancy between fluid and weight loss during acute decompensated heart failure treatment. Am J Med 128 (7):776–783 e4
Lee HF, Hsu LA, Chang CJ, Chan YH, Wang CL, Ho WJ, Chu PH (2014) Prognostic significance of dilated inferior vena cava in advanced decompensated heart failure. Int J Cardiovasc Imaging 30(7):1289–1295
Nath J, Vacek JL, Heidenreich PA (2006) A dilated inferior vena cava is a marker of poor survival. Am Heart J 151(3):730–735
Cubo-Romano P, Torres-Macho J, Soni NJ, Reyes LF, Rodriguez-Almodovar A, Fernandez-Alonso JM, Gonzalez-Davia R, Casas-Rojo JM, Restrepo MI, de Casasola GG (2016) Admission inferior vena cava measurements are associated with mortality after hospitalization for acute decompensated heart failure. J Hosp Med. doi:10.1002/jhm.2620
Torres D, Cuttitta F, Paterna S, Garofano A, Conti G, Pinto A, Parrinello G (2016) Bed-side inferior vena cava diameter and mean arterial pressure predict long-term mortality in hospitalized patients with heart failure: 36 months of follow-up. Eur J Intern Med 28:80–84
Wattad M, Darawsha W, Solomonica A, Hijazi M, Kaplan M, Makhoul BF, Abassi ZA, Azzam ZS, Aronson D (2015) Interaction between worsening renal function and persistent congestion in acute decompensated heart failure. Am J Cardiol 115(7):932–937
Iida N, Seo Y, Sai S, Machino-Ohtsuka T, Yamamoto M, Ishizu T, Kawakami Y, Aonuma K (2016) Clinical implications of intrarenal hemodynamic evaluation by doppler ultrasonography in heart failure. JACC Heart Fail 4(8):674–682
Hanatani A, Shibata A, Kitada R, Iwata S, Matsumura Y, Doi A, Sugioka K, Takagi M, Yoshiyama M (2016) Administration of tolvaptan with reduction of loop diuretics ameliorates congestion with improving renal dysfunction in patients with congestive heart failure and renal dysfunction. Heart Vessels. doi:10.1007/s00380-016-0872-4
Uemura Y, Shibata R, Takemoto K, Uchikawa T, Koyasu M, Ishikawa S, Mitsuda T, Miura A, Imai R, Iwamiya S, Ozaki Y, Kato T, Miura T, Watarai M, Murohara T (2016) Clinical benefit of tolvaptan in patients with acute decompensated heart failure and chronic kidney disease. Heart Vessels 31(10):1643–1649
Matsue Y, Shiraishi A, Kagiyama N, Yoshida K, Kume T, Okura H, Suzuki M, Matsumura A, Yoshida K, Hashimoto Y (2016) Renal function on admission modifies prognostic impact of diuretics in acute heart failure: a propensity score matched and interaction analysis. Heart Vessels. doi:10.1007/s00380-016-0817-y
Summary of Recommendation Statements (2013) Kidney international supplements. J Diabetes Res 3(1):5–14. doi:10.1038/kisup.2012.77
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to disclose.
Rights and permissions
About this article
Cite this article
Jobs, A., Brünjes, K., Katalinic, A. et al. Inferior vena cava diameter in acute decompensated heart failure as predictor of all-cause mortality. Heart Vessels 32, 856–864 (2017). https://doi.org/10.1007/s00380-017-0944-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-017-0944-0