Abstract
This study provides early results of re-operations after the prior surgical treatment of acute type A aortic dissection (AAD) and identifies risk factors for mortality. Between May 2003 and January 2014, 117 aortic re-operations after an initial operation for AAD (a mean time from the first procedure was 3.98 years, with a range of 0.1–20.87 years) were performed in 110 patients (a mean age of 59.8 ± 12.6 years) in seven European institutions. The re-operation was indicated due to a proximal aortic pathology in ninety cases: twenty aortic root aneurysms, seventeen root re-dissections, twenty-seven aortic valve insufficiencies and twenty-six proximal anastomotic pseudoaneurysms. In fifty-eight cases, repetitive surgical treatment was subscripted because of distal aortic pathology: eighteen arch re-dissections, fifteen arch dilation and twenty-five anastomotic pseudoaneurysms. Surgical procedures comprised a total of seventy-one isolated proximals, thirty-one isolated distals and fifteen combined interventions. In-hospital mortality was 19.6 % (twenty-three patients); 11.1 % in patients with elective/urgent indication and 66.6 % in emergency cases. Mortality rates for isolated proximal, distal and combined operations regardless of the emergency setting were 14.1 % (10 pts.), 25.8 % (8 pts.) and 33.3 % (5 pts.), respectively. The causes of death were cardiac in eight, neurological in three, MOF in five, sepsis in two, bleeding in three and lung failure in two patients. A multivariate logistic regression analysis revealed that risk factors for mortality included previous distal procedure (p = 0.04), new distal procedure (p = 0.018) and emergency operation (p < 0.001). New proximal procedures were not found to be risk factors for early mortality (p = 0.15). This multicenter experience shows that the outcome of REAAD is highly dependent on the localization and extension of aortic pathology and the need for emergency treatment. Surgery in an emergency setting and distal re-do operations after previous AAD remain a surgical challenge, while proximal aortic re-operations show a lower mortality rate. Foresighted decision-making is needed in cases of AAD repair, as the results are essential preconditions for further surgical interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Despite improved health care, including more expeditious referral to surgery, more fitting surgical techniques and better ICU treatment and surgery for acute type A dissection (AAD) continue to remain challenging [1–4]. During emergency surgery for acute type A aortic dissection (AAD), goals for successful treatment include restoration of the aortic valve function, treatment of malperfusion and resection of the proximal intimal tear. Moreover, in this context, of crucial importance is the extent of aortic resection to be performed to prevent future re-operations. In fact, un-removed tissue might predispose the patient to false lumen enlargement and, therefore, aneurysms, anastomotic pseudoaneurysm, re-dissection and aortic valve incompetence as a consequence of root dilatation. On the other hand, a more radical procedure including root and arch replacement may increase the technical complexity of this emergency operation with possible additional operative risk. In this context, a number of studies on the risk factors of re-operation have identified subgroups of patients in whom an aggressive approach can be justified and, therefore, preferred [5–7]. However, the literature lacks prospective studies proving a favorable outcome after a more aggressive approach in this subset of patients rather than a conservative approach. In this setting, re-operation after AAD will still continue to be a concern and a burden for patients who survive the first operation and a surgical challenge for surgeons who must deal with the re-do. Until now, a small number of single-center studies [8, 9] has focused on re-operations after AAD, and no multicenter investigation has reported on a stratification of the operative risk for mortality after re-operation. Therefore, the aim of this study is to report outcomes and risk factors for mortality in redo surgical procedures after a prior operation for AAD from a multicenter European database, including a reasonable number of patients with different surgical approaches.
Patients and methods
This is an analysis of 110 consecutive patients who were operated on between May 2003 and December 2013, in seven sites of real-word practice in Europe (Italy: five centers and Germany: two centers). Data regarding demographic variables, type of first operation, indication for re-operation, type of re-do and postoperative outcomes were retrospectively retrieved from individual institutional databases and entered in the REAAD database (re-do after acute type A aortic dissection) at the University Hospital of Muenster. The ethical committee of the University of Muenster approved the study, and patient consent was waived. The study population consisted of ninety-one males and nineteen females with a mean age of 59.8 ± 12.6 years (range 25–88 years). The baseline patient characteristics are shown in Table 1. All patients who survived the first operation and underwent a second surgical aortic procedure or aortic valve surgery were included. Patients who underwent endovascular procedures without second surgery as well as patients who underwent heart surgery for causes not related to the first operation, like isolated CABG, mitral valve surgery, VAD implantation etc., were excluded. Moreover, patients primarily operated on for chronic aortic dissection were also excluded. The main end-point of this study was in-hospital mortality. Other endpoints included major complications, length of hospital stay (LOS) and length of intensive care unit stay (ICU stay).
Statistical analysis
Continuous variables are presented as mean ± SD and categorical variables are expressed as frequencies. Potential risk factors for in-hospital mortality, including the preoperative risk factors of patients such as age, hypertension, diabetes mellitus, peripheral vascular disease, chronic obstructive pulmonary disease, congestive heart failure, renal insufficiency coronary artery disease and Marfan’s syndrome were entered in the univariate and multivariate logistic regression. The dependent variable of the logistic model was the in-hospital mortality. This included any death that occurred during the initial hospitalization until discharge. Variables entered in the model included the following surgical variables: ischemic time, cardiopulmonary bypass time, surgical technique and the type of first procedure. The indication for the re-operation and the time interval between the two procedures were also analyzed. A univariate analysis was first performed. Variables with p < 0.2 were included in a multivariable logistic model regression analysis using stepwise selection to determine the independent predictors of in-hospital mortality. The discrimination achieved was assessed with the C statistic, which is equivalent to the area under the receiver operating characteristic curve. C statistical values of 1.0 indicate perfect discrimination between survivors and deaths, whereas values of 0.5 indicate random discrimination. Moreover, the performance of the model was verified with a Hosmer–Lemeshow test. A p value <0.05 was considered statistically significant. Data analysis was performed using Excel 2010 (Microsoft, Redmond, WA, USA) and commercially available statistical software packages (SPSS for Windows, Version 15.0, SPSS, Inc., Chicago, IL, USA).
Results
Operative procedures for initial repair and indication for re-operation
The most frequent initial procedure was replacement of the ascending aorta with aortic valve resuspension in more than the half of the entire cohort—sixty-seven (57.26 %, 67 pts.). A more aggressive approach regarding the proximal aorta was performed in twenty-two patients consisting in root replacement either with a valve-sparing procedure (two patients) or with the Bentall operation (twenty patients). Distal procedures were conducted in less than one-third of the patients (twenty-seven patients—23.08 %), including partial arch replacement in ten patients and total arch replacement with and without elephant trunk procedure in six and ten patients, respectively. Data are shown in Table 1.
After a mean time from the first procedure for AAD of 3.98 years (range 0.1–20.87), a total of 117 aortic re-operations were performed in 110 patients (with a mean age of 59.8 ± 12.6 years), four patients had a second re-operation and one patient even a fourth re-operation. In two patients, AAD presented the first time after a previous cardiac operation not related to aortic procedures. Proximal re-operation was required due to the following causes: an aortic root aneurysm in twenty patients, a root re-dissection in seventeen, an aortic valve insufficiency in twenty-seven and a proximal anastomotic pseudoaneurysm in twenty-six. Two cases of proximal pseudoaneurysms were due to a prosthesis infection.
Distal causes for re-operation were arch re-dissection in eighteen patients, arch dilatation in fifteen and anastomotic pseudoaneurysm in twenty-five. A total of fifteen patients (10.82 %) were referred to surgery due to late complications proximally involving the aortic root or immediately above the sinotubular junction, and distally to the prosthesis material. A total of eighteen patients (15.38 %) were operated on in an emergency setting, whereas thirty-two patients were urgently referred to surgery.
Procedures performed at the time of redo, in-hospital mortality, major complications and risk factors for mortality
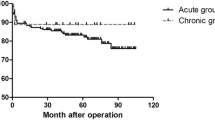
There were twenty-three (19.6 %) in-hospital deaths, of which eleven had undergone emergency and two urgent operations. The overall mortality rate among elective or urgent operations was 11.1 %, whereas it was 66.6 % in the emergency setting. Mortality rates for isolated proximal, distal and combined operations regardless of the emergency setting were 14.1 % (10 pts.), 25.8 % (8 pts.) and 33.3 % (5 pts.). Figures 1 and 2 schematize the mortality rates according to the setting (emergency vs. elective) and to the performed procedure. The causes of death were cardiac in eight, neurological in three, MOF in five, sepsis in two, bleeding in three and lung failure in two patients. Univariate and multivariate logistic regression analyses revealed that risk factors for mortality were emergency operations (p < 0.001, odd 15.4), previous distal procedures including total arch replacements with or without elephant trunk (p = 0.04, odd 5.3) and new distal procedures (p = 0.018, odd 4.4). Neither new proximal procedures nor initial ascending aortic replacements with partial hemi-arch replacements were found to be risk factors for early mortality (p = 0.15, and p = 0.84, respectively). The p value of the Hosmer–Lemeshow test was 0.17, and C statistic for the fitted logistical regression model was 0.88 (p < 0.001), indicating that the model fit was excellent.
The incidence of low output syndrome, neurological events, renal failure, respiratory failure and bleeding requiring re-operation, was 11.9 % (14 pts.), 11.1 % (13 pts.), 9.4 % (11 pts.), 12.7 % (15 pts.) and 17.9 % (20 pts.), respectively. The mean ICU stay and mean hospital stay were 9.79 ± 13.71 and 17.68 ± 15.14 days.
Proximal procedures
The rate of proximal procedures at the time of re-do was higher than distal and combined procedures with 60.6 % (71 procedures) vs. 26.4 % (31), vs. 12.8 % (15), respectively. Ascending aortic replacement with aortic valve resuspension was the most frequently used procedure at the time of the first surgery (59.1 %). Eleven patients (15.4 %), who underwent more aggressive procedures the first time, including an aortic valve replacement, a valve-sparing operation and the Bentall procedure, underwent new proximal procedures.
The most frequent proximal procedure during re-do was the composite aortic root replacement (the Bentall procedure) (56.3 %, 40 operations), followed by an isolated aortic valve replacement (13 pts. 18.3 %) and an ascending aortic replacement (12.6 %). Table 2 shows in detail the operative procedures at the time of re-operation as well as the time of the initial repair for AAD.
The mortality rates for the isolated proximal operations regardless of the emergency setting were 14.1 % (10 pts.). Seven out of ten deaths were reported after emergency operations. The mortality rate for isolated proximal procedures in elective or urgent settings was 6 % (3 pts. out 60).
Distal procedures
A total of thirty-one patients underwent isolated distal procedures. The most frequent distal procedure at the time of re-operation was total arch replacement (19 pts. 61.2 %), followed by frozen elephant trunk in seven patients (22.5 %), (Table 3). Ascending aortic replacement with an aortic valve resuspension was the most frequently used procedure at the time of the first surgery—64.5 %—and distal repair. Of note, none of the patients that underwent late distal repair received initial arch procedures (Table 3). Mortality rates for distal regardless of the emergency setting was 25.8 % (8 pts.). The mortality rate for isolated distal procedures in elective or urgent settings was 14.8 %. All patients (4 pts.) that underwent emergency distal repair died.
Combined procedures
A total of fifteen patients underwent combined procedures, consisting of concomitant proximal and distal repair. The most frequent combined procedures at the time of re-operation were the Bentall procedure with total arch replacement (3 pts.) and a more conservative approach including proximal and distal patch reconstruction (3 pts.). Ascending aortic replacement with aortic valve resuspension was, as reported for proximal and distal late procedures, the most frequently used procedure at the time of the first surgery—64.5 %. The mortality rate was 33.33 % in both elective and emergency settings. Table 4 shows in detail the operative procedures at the time of re-operation as well as the time of the initial repair for AAD.
Discussion
The aim of this multicenter study was to report on outcomes and stratification of mortality risk of re-do after prior AAD repair. To our best knowledge, this is the first multi-institutional report with a reasonable number of patients and procedures.
When performing AAD repair, a solution that satisfies two main goals has to be achieved. The first and most important one is to save the patient’s life by performing a safe operation; the secondary aim is to guarantee long-term freedom from re-operations. It is certainly more difficult to achieve both goals in an emergency setting than in an elective one. Supracoronary replacement of the ascending aorta with root reconstruction is one of the most commonly adopted conservative approaches used during surgery for AAD. The drawback of this conservative technique is that the remaining aortic wall might predispose the patient to proximal or distal aneurysm formation as well as re-dissection, requiring re-operation on the aortic root or arch during the late postoperative period. On the other hand, a more time-consuming and surgically demanding operation with a more aggressive approach (including composite root replacement or/and arch replacement with or without elephant trunk) must be weighed against potential long-term failure of the conservative technique. In this setting, whether or not to be aggressive is a subject of debate. In this context, many authors have advocated a more systematic aggressive approach in view of risk of late operations [10]; some others, instead, suggest a more aggressive approach only in some subsets of patients that present risk factors for re-operations [5, 6, 8, 11, 12]. In this setting, an extensive report on re-operations after first repair for AAD can help surgeons to tailor the better strategy during the initial operation not only on the basis of the long-term outcome after first repair, but also in view of outcomes of a further eventual re-operation.
Proximal procedures
In the current report, the rate of proximal procedures was higher than distal and combined procedures 60.67 % (71 procedures) vs. 26.49 % (31) vs. 12.81 % (15). Mortality rate for proximal operations was 14.08 % (10 pts.); of them, 7 deaths were reported after emergency operation. Those results regarding the proximal aorta resemble the outcome obtained by Estrera et al. [9]. In his report including 63 proximal re-operations after first repair for AAD, mortality rate was 11 %. The little difference with our results can be explained by the higher emergency referral of our patients (15.49 % for proximal procedures vs. 8 % in the group of Estrera). In another study, including 58 patients who underwent root or ascending after prior aortic valve or ascending aortic replacement, Silva et al. [13] reported comparable results to our data (mortality rate by 12 %). To remark the theory that a first conservative approach on the aortic root should be preferred, Moon et al. [14] found that a more aggressive strategy neither eliminated the risk of proximal operations nor reduced the rate of potential valve-related complications. Additionally, in our last report [5] including 319 consecutive patients who underwent replacement of the ascending aorta with preservation of the aortic root after AAD, we found, after 23-year follow-up, freedom from re-operation of 97, 92, and 82 % patients at 5, 10, and 23 years, respectively. Thus, a conservative approach regarding the root seems to be the preferable solution in light of the lower perioperative mortality, the long freedom from proximal re-operation and an acceptable mortality rate in case of re-operation.
Distal procedures
Multivariate logistic regression analysis revealed that risk factor for mortality beside emergency operation (p < 0.001, odd 15.4) was new aggressive distal procedure (including total arch with or without elephant trunk procedure), whereas hemi-arch replacement was not found to be a risk factor for early mortality. None of the patients who underwent late isolated distal repair received initial arch procedures (including hemi-arch, total arch with or without elephant trunk). Thus, one can speculate that the first repair was too minimalist and that the possibility of a re-operation would have been better avoided in light of a higher mortality (25.81 %—8 pts.) compared to the proximal procedures. All emergency cases (4 pts.) that required a distal procedure died. On the other hand, distal mortality rate in elective setting was of 14.80 %. Our results are consistent with those reported by Rylski et al. In his study [15], six patients (4 were emergency cases) out of twenty-eight (mortality 21.42 %) did not survive the surgery or the early postoperative period. In his study, twenty-four patients underwent distal open aortic repair and four patients underwent the endovascular approach. In another report by the same author [12], all emergency cases died, whereas all elective cases survived surgery. Of note, in this study, six patients (50 %) underwent thoracic endovascular aortic repair (TEVAR), three patients (25 %) a hybrid approach by means of debranching and only three patients underwent complete surgical repair. Those two studies, in conjunction with our report, highlight the potential advantages of the endovascular repair. Furthermore, in another study, Rylski et al. [16] compared the outcomes of endovascular re-intervention (n. 54 pts.) versus re-do (distal open repair n. 84 pts.) in patients after surgery for AAD. They found an in-hospital mortality rate for the open group and the endovascular group of 23 % vs 0 % (p = 0.01), respectively. Of note, we reported similar results concerning the distal re-dos (21.42 %).
Another important issue emerging from this study and from the above-mentioned reports regards the poor outcome in emergency situations. In this setting, a strict CT follow-up is of utmost importance to plan elective surgery and reduce mortality. Moreover, a stricter follow-up is even more necessary in patients with known risk factors for re-operations [5, 6, 17].
Another interesting finding of our study after the multivariate regression adjustment concerned the previous distal procedure. Previous total arch replacement with or without elephant trunk was found to be a risk factor for mortality, whereas previous hemi-arch replacement was not found to be a risk factor for early mortality. A possible explanation might reside in a more complex operative field. Thus, the more complex the initial operation was, the more complex the re-operation is. Our analysis, however, does not take into account the last advancements in the arch surgery since no patient of our cohort initially underwent FET. In this setting, it is out of debate that frozen elephant trunk allows the adaptation of the false lumen to the true one. Shrestha et al. [10] reported a freedom of distal re-operation of 100 % after a mean follow-up of forty months—those results are promising. However, as specified by the authors, such a strategy is not appropriate in all AADA cases; it should be implemented only in experienced centers and only if absolutely necessary. Moreover, they recommended this procedure for experienced surgeons with at least twenty elective FET implantations before he/she starts with such an operation in an acute dissection patient.
Interestingly, neither previous hemi-arch replacements nor new hemi-arch replacements were a risk factor for mortality after re-operation. In conjunction with this finding, other studies [14–16] have found high freedom from distal re-operation when a hemi-arch surgery is performed. The partial resection of the lesser curvature of the arch in conjunction with the resection of the clamp site can stabilize the entire aortic wall and confer an advantage, preventing distal re-operation. Moon et al. [14] found that none of the thirty-four patients who survived hemi-arch replacement required an anterior re-operation. Moreover, hemi-arch replacement showed a trend towards better freedom from re-operation, but the difference did not reach statistical significance. Rylski et al. [15] showed that aggressive arch replacement in 534 patients was associated with a low in-hospital mortality after AAD repair (12 %) and high freedom from distal aortic re-intervention (over 85 % at ten years). Kim et al. [18] found a significantly better survival rate and freedom from neurological injury in patients receiving hemi-arch replacement when compared with patients who underwent total arch replacement for repair of DeBakey AAD. As reported in our study, arch replacement performed the first time or at the time of re-operation was, after multivariate adjustment, an independent risk factor for mortality, whereas both a previous hemi-arch replacement and a new hemi-arch replacement were not. These findings and the previously mentioned studies underline the importance of the hemi-arch technique.
The hemi-arch technique seems to be a compromise solution resulting in a lower incidence of distal procedures and an acceptable mortality regarding initial and late operation. Put briefly, a minimalist approach concerning not only the proximal aorta but also the arch by means of a hemi-arch replacement at the time of the first repair neither constitutes a risk factor for mortality the first time [14], nor at the time of the re-do.
Limitations of this study
The main limitation of the current report lies in its retrospective design. Moreover, re-operation rates have not been calculated since not all patients underwent prior AAD repair in the same center. This increases the diversity and variety of procedures that were performed. Although we attempted to account for factors that changed during this period (the year of operation and center), some issues may not be reflected in the multivariate analysis. However, this variety can also be considered an advantage, giving a meaningful overview of outcome in re-do after AAD. Further studies are required to confirm these results.
Abbreviations
- AAD:
-
Acute type A aortic dissection
- AVR:
-
Aortic valve replacement
- BMI:
-
Body mass index
- BSA:
-
Body surface area
- CABG:
-
Coronary artery bypass grafting
- COPD:
-
Chronic obstructive pulmonary disease
- EF:
-
Ejection fraction
- FET:
-
Frozen elephant trunk
- ET:
-
Elephant trunk
- ICU:
-
Intensive care unit
- LOS:
-
Length of stay
- MOF:
-
Multiorgan failure
- REAAD:
-
Re-do operation after acute type A aortic dissection
- TEVAR:
-
Thoracic endovascular aortic repair
- VAD:
-
Ventricular assist device
References
Colli A, Carrozzini M, Galuppo M, Comisso M, Toto F, Gregori D, Gerosa G (2015) Analysis of early and long-term outcomes of acute type A aortic dissection according to the new international aortic arch surgery study group recommendations. Heart Vessels. doi:10.1007/s00380-015-0770-1
Schneider SR, Dell’Aquila AM, Akil A, Schlarb D, Panuccio G, Martens S, Rukosujew A (2016) Results of “elephant trunk” total aortic arch replacement using a multi-branched, collared graft prosthesis. Heart Vessels 31(3):390–396
Okina N, Ohuchida M, Takeuchi T, Fujiyama T, Satoh A, Sakamoto T, Adachi H, Imaizumi T (2013) Utility of measuring C-reactive protein for prediction of in-hospital events in patients with acute aortic dissection. Heart Vessels 28(3):330–335
Jo Y, Anzai T, Sugano Y, Naito K, Ueno K, Kohno T, Yoshikawa T, Ogawa S (2008) Early use of beta-blockers attenuates systemic inflammatory response and lung oxygenation impairment after distal type acute aortic dissection. Heart Vessels 23(5):334–340
Dell’Aquila AM, Concistrè G, Gallo A, Pansini S, Piccardo A, Passerone G, Regesta T (2013) Fate of the preserved aortic root after treatment of acute type A aortic dissection: 23-year follow-up. J Thorac Cardiovasc Surg 146(6):1456–1460
Concistrè G, Casali G, Santaniello E, Montalto A, Fiorani B, Dell’Aquila A, Musumeci F (2012) Reoperation after surgical correction of acute type A aortic dissection: risk factor analysis. Ann Thorac Surg 93(2):450–455
Rylski B, Beyersdorf F, Blanke P, Boos A, Hoffmann I, Dashkevich A, Siepe M (2013) Supracoronary ascending aortic replacement in patients with acute aortic dissection type A: what happens to the aortic root in the long run? J Thorac Cardiovasc Surg 146(2):285–290
Kobuch R, Hilker M, Rupprecht L, Hirt S, Keyser A, Puehler T, Amman M, Zink W, Schmid C (2012) Late reoperations after repaired acute type A aortic dissection. J Thorac Cardiovasc Surg 144(2):300–307
Estrera AL, Miller CC 3rd, Villa MA, Lee TY, Meada R, Irani A, Azizzadeh A, Coogan S, Safi HJ (2007) Proximal reoperations after repaired acute type A aortic dissection. Ann Thorac Surg 83(5):1603–1609
Shrestha M, Fleissner F, Ius F, Koigeldiyev N, Kaufeld T, Beckmann E, Martens A, Haverich A (2015) Total aortic arch replacement with frozen elephant trunk in acute type A aortic dissections: are we pushing the limits too far? Eur J Cardiothorac Surg 47(2):361–366
Piccardo A, Regesta T, Pansini S, Dell’Aquila AM, Concistrè G, Martinelli L, Passerone G (2009) Fate of the aortic valve after root reconstruction in type A aortic dissection: a 20-year follow up. J Heart Valve Dis 18(5):507–513
Rylski B, Beyersdorf F, Kari FA, Schlosser J, Blanke P, Siepe M (2014) Acute type A aortic dissection extending beyond ascending aorta: limited or extensive distal repair. J Thorac Cardiovasc Surg 148(3):949–954
Silva J, Maroto LC, Carnero M, Vilacosta I, Cobiella J, Villagrán E, Rodríguez JE (2010) Ascending aorta and aortic root reoperations: are outcomes worse than first time surgery? Ann Thorac Surg 90(2):555–560
Moon MR, Sundt TM 3rd, Pasque MK, Barner HB, Huddleston CB, Damiano RJ Jr, Gay WA Jr (2001) Does the extent of proximal or distal resection influence outcome for type A dissections? Ann Thorac Surg 71(4):1244–1250
Rylski B, Milewski RK, Bavaria JE, Vallabhajosyula P, Moser W, Szeto WY, Desai ND (2014) Long-term results of aggressive hemiarch replacement in 534 patients with type A aortic dissection. J Thorac Cardiovasc Surg 148(6):2981–2985
Rylski B, Beyersdorf F, Desai ND, Euringer W, Siepe M, Kari FA, Vallabhajosyula P, Szeto WY, Milewski RK, Bavaria JE (2015) Distal aortic reintervention after surgery for acute DeBakey type I or II aortic dissection: open versus endovascular repair. Eur J Cardiothorac Surg 48(2):258–263
Fattouch K, Sampognaro R, Navarra E, Caruso M, Pisano C, Coppola G, Speziale G, Ruvolo G (2009) Long-term results after repair of type a acute aortic dissection according to false lumen patency. Ann Thorac Surg 88(4):1244–1250
Kim JB, Chung CH, Moon DH, Ha GJ, Lee TY, Jung SH, Choo SJ, Lee JW (2011) Total arch repair versus hemiarch repair in the management of acute DeBakey type I aortic dissection. Eur J Cardiothorac Surg 40(4):881–887
Funding
The authors do not have any funding support to declare.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
No author has a conflict of interest related to the material reported in this study.
Additional information
A. M. Dell’Aquila and F. Pollari contributed equally to this work and should both be considered as first authors.
Rights and permissions
About this article
Cite this article
Dell’Aquila, A.M., Pollari, F., Fattouch, K. et al. Early outcomes in re-do operation after acute type A aortic dissection: results from the multicenter REAAD database. Heart Vessels 32, 566–573 (2017). https://doi.org/10.1007/s00380-016-0907-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-016-0907-x