Abstract
To evaluate predictors of early and long-term outcomes of surgical repair of acute Type A aortic dissection. Retrospective single-centre study evaluating patients surgically treated between 1998 and 2013. Clinical follow-up was performed. Complications were classified according to the International Aortic Arch Surgery Study Group recommendations. Statistical analysis included univariate and multivariate analysis of preoperative and operative data. One hundred eighty-five patients were evaluated. The follow-up was complete for 180 patients (97 %). Mean age was 63 years, 82 % had a DeBakey type I aortic dissection, 18 % a type II. Eleven patients (6 %) died intraoperatively, 119 of the remaining (68 %) had postoperative complications. Thirty-day mortality was 21 % (38 patients). Average ICU and hospital stay were 6 and 14 days, respectively. During a mean follow-up time of 6 ± 4 years we observed 44 deaths (31 %). Twenty patients (14 %) needed late thoracic aorta reoperation. Results from the multivariate analysis are as follows. Thirty-day mortality was associated with abdominal pain at presentation (p < 0.01). The incidence of postoperative complications was related to older age at intervention (p < 0.01) and longer cross-clamp time (p < 0.01). Mortality at follow-up was significantly increased by older age at intervention (p < 0.01), with a logarithmic growth after 60 years, female sex (p < 0.01), preoperative limb ischemia (p = 0.02) and DHCA (p < 0.01). The surgical results of type A aortic dissection are affected by age at intervention with a logarithmic increase of late mortality in patients older than 60 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Type A aortic dissection is a severe condition, requiring emergent surgical treatment. Despite increased understanding of the pathophysiology and improved surgical techniques and perioperative care, surgical mortality has remained high through years ranging from 15 to 30 % [1–3]. Several studies report the influence of pre- and perioperative variables on outcome [4–10], but findings are often controversial and there is still debate on optimal management [11–13].
We reviewed our institutional experience with acute type A aortic dissection, aiming to identify determinants of early and long-term results.
Materials and methods
Definitions
All patients were diagnosed with an acute “type A” aortic dissection, according to the Stanford University definition [14]. We further classified cases in DeBakey type I or II [15].
Obesity was considered as a body mass index >30. Systemic arterial hypertension was defined as history of systolic pressure >140 mmHg or diastolic pressure >90 mmHg. Diabetes was a history of diabetes mellitus regardless of duration of disease or need for antidiabetic agents. Dyslipidemia was any lipid disorder. Chronic lung disease was defined according to “EuroSCORE II”, as well as peripheral vascular disease and renal impairment. Coronary artery disease was a left main stenosis >50 % or major branches stenosis >70 %. The neurological status on admission was considered undefined when the patient was already on sedation. Cardiogenic shock was identified as persistent hypotension (systolic pressure <80 mmHg or mean pressure 30 mmHg lower than baseline) with adequate of elevated filling pressures. Postoperative complications were classified according to the latest consensus statement from the International Aortic Arch Surgery Study Group [16].
Operative technique
Intraoperative transoesophageal echocardiogram was used for confirmation of diagnosis and evaluation of aortic valve. All patients underwent a median sternotomy. Arterial cannulation for cardiopulmonary bypass (CPBP) was carried out through the femoral or subclavian artery (using an interposition graft) or, when appropriate, the ascending aorta; most patients received right atrium or bicaval venous cannulation, some cases required initial connection to the femoral vein. The left ventricle was vented through the right superior pulmonary vein or the main pulmonary artery. Temperature was continuously measured in the nasopharynx, oesophagus, and rectum. During cooling the extent of aortic dissection was explored. After distal cross-clamping and aortotomy, cold blood cardioplegia was administered directly into the coronary ostia. Subsequently proximal ascending aorta was inspected for intimal tears; aortic valve and coronary arteries were accurately evaluated. When needed, procedures on the aortic root were performed at this time. In few cases the ascending aorta was replaced by means of a clamped distal anastomosis; all other patients received a period of circulatory arrest, allowing for cross-clamp removal, evaluation of aortic arch and open distal anastomosis. In the early experience a deep hypothermic circulatory arrest (DHCA) was carried out, cooling down the patient to 18–20 °C of rectal temperature. Later on we used retrograde cerebral perfusion (RCP) as neuroprotection strategy, with 150–450 ml/min via the superior vena cava maintaining a central venous pressure of 20–30 mmHg, at a rectal temperature of 18–20 °C. In the last years, we routinely used the antegrade selective cerebral perfusion (ASCP) according to Kazui [17] with a perfusion flow of 10–15 ml/kg/min, maintaining a right radial artery pressure of 40–70 mmHg, at a rectal temperature of 25–30 °C. After completion of the distal anastomosis, CPBP was re-instituted through the prosthesis. Re-warming was achieved at 1 °C per 3 min, not exceeding a 10 °C gradient between blood temperature and nasopharyngeal or rectal temperature. The proximal anastomosis was performed during re-warming.
Patients
Study approval was granted by the Ethics Committee of the University of Padova, individual patient consent was waived. Between 1998 and 2013, 185 patients underwent surgery at our Institution for an acute type A aortic dissection: 105 male (57 %), mean age 63 ± 13 years (range 19–85 years). Among these, 152 patients were diagnosed with a DeBakey type I dissection (82 %), 33 with a DeBakey type II (18 %).
Available baseline patient characteristics, risk factors, basic diagnosis and clinical presentation are summarized in Table 1.
Follow-up data were derived from outpatient clinic records, telephone contact and municipal civil registries, and was complete in 180 patients (97 %).
Statistical analysis
Continuous variables were expressed as average, with standard deviation as a measure of variability. The individual effect of clinical data on outcomes was evaluated by Cox proportional hazards regression analysis. Proportional hazard assumption was checked for each model (both univariate and multivariable) using the Grambsh and Therneau test and diagnostic plots based on Shoenfeld residual. Nonlinear effect of covariates was modelled using a restrictive cubic spline function, and its significance was assessed by the χ 2 Wald test. The model strategy was determined following a backward selection strategy among variables reaching at least level 0.25 at univariable analysis. Model fit was considered significantly improved on the basis of the Akaike Information Criterion applied backward for each model at a significance level of 0.05. To account for possible overfitting in the Cox model secondary to a high ratio between events and covariates, cross-validation and bootstrap (1000 runs) techniques were applied. Somer’s Concordance Index Dxy was obtained for goodness of fit evaluation and adjusted for optimism. Cumulative survival curves were generated with the Kaplan–Meier method and compared by the log-rank test. The statistical significance was set at p < 0.05. The R-System statistical package and the Harrell’s rms libraries were used for analysis.
Results
Surgical management
In 10 patients (5 %) the distal anastomosis was performed by cross-clamping the aorta; all other cases received a period of circulatory arrest. Seven patients (5 %), early in our experience, received DHCA, lasting a mean time of 30 ± 15 min. Later on we used RCP in 101 patients (58 %), mean time of perfusion was 29 ± 16 min. Finally we introduced ASCP and managed 67 patients (38 %) with a mean perfusion time of 57 ± 41 min. Fifty-nine cases (32 %) required aortic valve replacement (AVR), while 41 patients (22 %) needed a full aortic root replacement. Valve sparing procedure was performed only in 3 cases (2 %). The extent of the aortic replacement was confined to the ascending aorta in 145 patients (78 %) and to the hemiarch in 14 (8 %), while the total arch replacement was performed in 26 patients (14 %). Additional coronary artery bypass grafting (CABG) was required in 10 cases (6 %).
Early outcomes
Intraoperative mortality was 6 % (11 patients). Among the remaining patients, the mean intensive care unit (ICU) stay was 6 ± 9 days and the mean hospital stay 14 ± 12 days. Overall 30-day mortality was 21 % (38 patients). Postoperative complications occurred in 119 cases (68 %). Most common complications included global or focal neurological deficit (20 % and 12 %, respectively), arrhythmia (28 %, mainly atrial fibrillation), respiratory parenchymal complications (20 %), postoperative bleeding (20 %) and renal dysfunction (16 %). Detailed postoperative data are presented in Table 2.
Long-term outcomes
After a mean follow-up time of 6 ± 4 years, we registered a mortality of 31 % (44 patients). Among hospital-discharged patients, overall survival was 91 % at 1 year, 77 % at 5 years and 66 % at 10 years. Twenty patients (14 %) required reintervention on the thoracic aorta: 15 patients due to residual type B aortic dissection and 5 patients for residual aortic arch dissection and consequent enlargement. Freedom from reintervention was 96 % at 1 year, 84 % at 5 years and 81 % at 10 years. The vast majority of patients showed good clinical status, with only 3 % of them presenting in NYHA class III or IV (Table 2).
Outcome predictors
We performed univariate analysis of all available preoperative, operative and postoperative data to determine their correlation with incidence of postoperative complications, 30-day mortality, follow-up mortality and reintervention on thoracic aorta at follow-up. All statistically significant variables were further studied with a multivariate model. Results are shown in Tables 3 and 4.
Several factors were associated to the outcomes considered. From the multivariate model 30-day mortality was correlated to abdominal pain as presenting symptom (p < 0.01); postoperative complications occurred more frequently with older age (p < 0.01) and longer cross-clamp time (p < 0.01); follow-up mortality was associated to older age (p = 0.02), female sex (p < 0.01), limb ischemia (p = 0.02) and use of DHCA (p = 0.02). As far as reintervention on thoracic aorta at follow-up is concerned, the multivariate model showed no independent risk factors.
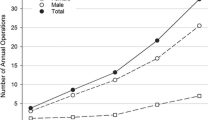
By plotting the mortality hazard with age at intervention, we revealed a logarithmic growth in patients older than 60 years. On this basis we stratified survival rates according to age, with a cutoff of 60 years and the results showed a significant divergence (p < 0.01) of the two curves (Fig. 1).
Discussion
Despite advances in surgical techniques, anaesthetic management, neuroprotection strategy and perioperative care, acute type A aortic dissection still presents high mortality rates (15–30 %) [1–3], pointing out the need for further investigations and possible technical refinements. This study is a retrospective, single-centre analysis of a large series of cases over a twelve-year period.
We reported a 30-day mortality of 21 %, comparable to the most recent reports from the literature [5, 8, 16, 18–21]. As far as postoperative complications is concerned, we applied the latest consensus statement from the International Aortic Arch Surgery Study Group [16] (structured in 16 items, each divided into four progressive grades of severity), with the belief that this classification will allow for a more detailed and reliable comparison between studies. To the best of our knowledge, this is the first study applying this classification; nevertheless our findings can still be compared to the present literature. Most common complication resulted to be a grade II (i.e. “non-life-threatening”) arrhythmia, other frequent and more concerning adverse events were renal dysfunction requiring haemodialysis (i.e. grade III) and bleeding requiring surgery (i.e. grade IV). Focusing on neurological outcome, the overall incidence of a permanent impairment (i.e. grade III or IV of global, focal or spinal deficit) was 20 % (35 patients), confirming results from other authors [7, 8].
In 2007, the IRAD investigators proposed a risk model for early mortality, in which age >70 years, prior AVR, preoperative hypotension, shock or tamponade, migrating chest pain, any pulse deficit, intraoperative hypotension, right ventricular dysfunction and CABG were risk factors for mortality, while partial arch replacement was associated to lower mortality [22]. In other reports pre-existing cardiac disease, cardiopulmonary resuscitation and longer CPB time were independent risk factors for 30-day mortality, while the use of circulatory arrest and biological glue were associated with reduced risk [5, 7, 23]. Our analysis identified several factors correlated to 30-day mortality (Table 3), surprisingly the multivariate model showed abdominal pain on presentation (p < 0.01) as the only independent predictor of outcome. This result can be explained by a possible correlation between abdominal pain on presentation and visceral malperfusion, a known important risk factor for early mortality [24]. On this basis, in patients presenting with this symptom, particular care should be taken to preoperatively evaluate the blood flow through the visceral vessels, to plan the proper surgical strategy. Restoration of flow into the true lumen in these cases is of paramount importance to avoid bowel ischemia. Unfortunately even extended aortic arch reconstructions can result ineffective, due to the presence of re-entry tears in the descending aorta. From this point of view, recent reports of combined (single-stage) proximal and distal aortic repair with the use of antegrade TEVAR are extremely interesting and could overcome this problem [25]. Another technical strategy that can be used is subintimal flap fenestration [26]. The rationale for subintimal flap fenestration is to achieve reperfusion of malperfused aortic branches by means of decompression of the true lumen. However, high postprocedural complications (11–20 %) and mortality rates (17–34 %) have been reported with this technique [27–30].
We also considered predictors of postoperative complications (Table 3) and identified older age (p < 0.01) and longer cross-clamp time (p < 0.01) to be independent risk factors. Interestingly, in our study, age at operation was associated to higher early morbidity but seemed not to affect significantly the 30-day mortality.
Overall all-cause mortality at follow-up was 31 % (44 patients). Numerous factors were associated to late death in our study (Table 4). Bekkers et al. reported older age, prior myocardial infarction, higher preoperative creatinine, preoperative COPD and impaired left ventricular function as independent risk factors for late mortality [5]. Our findings confirmed older age (p < 0.01) to be independently associated to late mortality. We also revealed female sex (p < 0.01), limb ischemia on presentation (p = 0.02) and use of DHCA (p < 0.01) as independent predictors of late death.
As far as reoperation is regarded, we considered for the statistical analysis only reintervention on the thoracic aorta, aiming to recognise cases in which progression of a residual dissection required a further surgical procedure. The incidence of this late adverse outcome was 14 %. On the univariate analysis, younger age (p < 0.01) and aortic disease familiarity (p < 0.01) had the strongest correlation with this outcome (Table 4). The effect of younger age on reoperation was probably due to a longer survival probability, leading to a higher likelihood of residual dissection progression. On the other hand is not of any surprise the impact of aortic disease familiarity that implies congenital connective disorders predisposing to aortic enlargement. Interestingly, the extension of distal repair of the aortic dissection resulted not to influence the incidence of reoperation. Unfortunately, the multivariate analysis failed to identify independent risk factors, probably due to the small number of events.
The rule of age on outcome of type A aortic dissection was addressed by many authors but results are controversial. In one of the earlier papers on the topic, Neri et al. analysed surgical results in octogenarians and concluded that a 30-day mortality of 83 %, with intraoperative mortality of 33 % were too high to justify a surgical repair [31]. In 2002, Mehta et al. analysed data from the IRAD stratifying patients by age with a cutoff of 70 years: postoperative complications were similar in the two groups; among patients treated surgically, in-hospital mortality was higher in the elderly cohort (37.5 vs. 23 %) but still lower than medically managed patients of corresponding age [32]. In 2010, Trimarchi et al. reviewed the IRAD and, analysing in-hospital mortality of medically versus surgically managed patients, concluded that surgery was recommended for patients aged 70–80 years and beneficial for octogenarians [33]. Similar results were reported by Rylski et al. using the GERAADA (German Registry for Acute Aortic Dissection Type A) [34]. All these studies did not investigate the effect of age on long-term mortality. A more recent report from Kilic et al. compared surgical results in patients aged <70 years versus older patients and showed no significant difference in mortality after 1 year [18]. Comparing octogenarians versus younger patients, Tang et al. found similar results after a mean follow-up of 1.5 years [35].
Our cohort had a mean age of 63 ± 13 years, ranging from 19 to 85 years; patients aged >70 years accounted for 32 % of the entire population (60 patients) and octogenarians represented 8 % of cases (15 patients). The policy of our Institution is to offer surgical repair regardless of patient age or comorbidities; therefore, a possible selection bias is minimized in our series. Contrary to the aforementioned reports, according to our data, age at intervention resulted not to influence significantly the 30-day mortality, although it determined a higher incidence of postoperative complications. On the other hand, after a mean follow-up time of 6 ± 4 years, older age turned out to be independent risk factor of late mortality, with 60 years as cutoff for higher risk of death at follow-up (Fig. 1).
The long follow-up time reported in our analysis could explain these findings. Although a shorter life expectancy can justify a higher long-term mortality in octogenarians, it cannot be generalized to all patients older than 60 years. Further investigations need to be performed on this subset of patients, to identify possible differences with a younger population that could clarify our results.
As age did not show any impact on early mortality, we believe that it should not be considered as sole criteria to exclude patients from undergoing repair. Nevertheless, the long-term outcome must be taken into account for an appropriate preoperative risk stratification and adequate patient and relative information.
Study limitations
Our study was a retrospective analysis; therefore, subject to incomplete events reporting. CT-angio or echocardiographic aortic assessment at follow-up was not available in many cases, thus further analysis on residual dissection was not possible.
Conclusions
Despite advances in perioperative management, surgical results of acute type A aortic dissection are still characterized by high rates of early and long-term mortality. Older age at intervention significantly increased the incidence of postoperative complications and late deaths, with a logarithmic growth of long-term mortality in patients older than 60 years. On the other hand, it seemed not to affect early mortality, suggesting that age should not be considered as the absolute criteria to exclude patients from surgery.
Eventually we underlined the role of clinical presentation of patients on outcome, being abdominal pain the worst prognostic factor.
References
Golledge J, Eagle KA (2008) Acute aortic dissection. Lancet 372:55–66
Braverman AC (2010) Acute aortic dissection: clinician update. Circulation 122:184–188
Hagan PG, Nienaber CA, Isselbacher EM, Bruckman D, Karavite DJ, Russman PL, Evangelista A, Fattori R, Suzuki T, Oh JK, Moore AG, Malouf JF, Pape LA, Gaca C, Sechtem U, Lenferink S, Deutsch HJ, Diedrichs H, Marcos y Robles J, Llovet A, Gilon D, Das SK, Armstrong WF, Deeb GM, Eagle KA (2000) The international registry of acute aortic dissection (IRAD): new insights into an old disease. JAMA 283:897–903
Trimarchi S, Nienaber CA, Rampoldi V, Myrmel T, Suzuki T, Mehta RH, Bossone E, Cooper JV, Smith DE, Menicanti L, Frigiola A, Oh JK, Deeb MG, Isselbacher EM, Eagle KA, International Registry of Acute Aortic Dissection Investigators (2005) Contemporary results of surgery in acute type A aortic dissection: the international registry of acute aortic dissection experience. J Thorac Cardiovasc Surg 129:112–122
Bekkers JA, Raap GB, Takkenberg JJ, Bogers AJ (2013) Acute type A aortic dissection: long-term results and reoperations. Eur J Cardiothorac Surg 43:389–396
Haldenwang PL, Wahlers T, Himmels A, Wippermann J, Zeriouh M, Kroner A, Kuhr K, Strauch JT (2012) Evaluation of risk factors for transient neurological dysfunction and adverse outcome after repair of acute type A aortic dissection in 122 consecutive patients. Eur J Cardiothorac Surg 42:e115–e120
Chiappini B, Schepens M, Tan E, Dell’Amore A, Morshuis W, Dossche K, Bergonzini M, Camurri N, Reggiani LB, Marinelli G, Di Bartolomeo R (2005) Early and late outcomes of acute type A aortic dissection: analysis of risk factors in 487 consecutive patients. Eur Heart J 26:180–186
Mehta RH, Suzuki T, Hagan PG, Bossone E, Gilon D, Llovet A, Maroto LC, Cooper JV, Smith DE, Armstrong WF, Nienaber CA, Eagle KA, International Registry of Acute Aortic Dissection (IRAD) Investigators (2002) Predicting death in patients with acute type A aortic dissection. Circulation 105:200–206
Ehrlich M, Fang WC, Grabenwoger M, Cartes-Zumelzu F, Wolner E, Havel M (1998) Perioperative risk factors for mortality in patients with acute type A aortic dissection. Circulation 98:294–298
Pansini S, Gagliardotto PV, Pompei E, Parisi F, Bardi G, Castenetto E, Orzan F, di Summa M (1998) Early and late risk factors in surgical treatment of acute type A aortic dissection. Ann Thorac Surg 66:779–784
Bonser RS, Ranasinghe AM, Loubani M, Evans JD, Thalji NM, Bachet JE, Carrel TP, Czerny M, Di Bartolomeo R, Grabenwoger M, Lonn L, Mestres CA, Schepens MA, Weigang E (2011) Evidence, lack of evidence, controversy, and debate in the provision and performance of the surgery of acute type A aortic dissection. J Am Coll Cardiol 58:2455–2474
Daily PO, Trueblood HW, Stinson EB, Wuerflein RD, Shumway NE (1970) Management of acute aortic dissections. Ann Thorac Surg 10:237–247
DeBakey ME, Cooley DA, Creech O Jr (1955) Surgical considerations of dissecting aneurysm of the aorta. Ann Surg 142:586–610
Tsai TT, Nienaber CA, Eagle KA (2005) Acute aortic syndromes. Circulation 112:3802–3813
Erbel R, Aboyans V, Boileau C, Bossone E, Di Bartolomeo R, Eggebrecht H, Evangelista A, Falk V, Frank H, Gaemperli O, Grabenwoger M, Haverich A, Iung B, Manolis AJ, Meijboom F, Nienaber CA, Roffi M, Rousseau H, Sechtem U, Sirnes PA, von Allmen RS, Vrints CJ, Authors/Task Force members (2014) 2014 ESC guidelines on the diagnosis and treatment of aortic diseases: document covering acute and chronic aortic diseases of the thoracic and abdominal aorta of the adult. The task force for the diagnosis and treatment of aortic diseases of the european society of cardiology (ESC). Eur Heart J 35(41):2873–2926
Yan TD, Tian DH, Lemaire SA, Hughes GC, Chen EP, Misfeld M, Griepp RB, Kazui T, Bannon PG, Coselli JS, Elefteriades JA, Kouchoukos NT, Underwood MJ, Mathew JP, Mohr FW, Oo A, Sundt TM, Bavaria JE, Di Bartolomeo R, Di Eusanio M, Trimarchi S, International Aortic Arch Surgery Study Group (2014) Standardizing clinical end points in aortic arch surgery: a consensus statement from the international aortic arch surgery study group. Circulation 129:1610–1626
Kazui T, Inoue N, Yamada O, Komatsu S (1992) Selective cerebral perfusion during operation for aneurysms of the aortic arch: a reassessment. Ann Thorac Surg 53:109–114
Kilic A, Tang R, Whitson BA, Sirak JH, Sai-Sudhakar CB, Crestanello J, Higgins RS (2013) Outcomes in the current surgical era following operative repair of acute type A aortic dissection in the elderly: a single-institutional experience. Interact CardioVasc Thorac Surg 17:104–109
Russo CF, Mariscalco G, Colli A, Santè P, Nicolini F, Miceli A, De Chiara B, Beghi C, Gerosa G, Glauber M, Gherli T, Nappi G, Murzi M, Molardi A, Merlanti B, Vizzardi E, Banadei I, Coletti G, Carrozzini M, Gelsomino S, Caiazzo A, Lorusso R (2015) Italian multicentre study on type A acute aortic dissection: a 33-year follow-up. Eur J Cardiothorac Surg. doi:10.1093/ejcts/ezv048
Ohnuma T, Kimura N, Sasabuchi Y, Asaka K, ShiotsukaJ Komuro T, Mouri H, Lefor AT, Adachi H, Sanui M (2015) Lower heart rate in the early postoperative period does not correlate with long-term outcomes after repair of type A acute aortic dissection. Heart Vessels 30(3):355–361
Schneider SRB, Dell’Aquila AM, Akil A, Schlarb D, Panuccio G, Martens S, Rukosujew A (2014) Results of “elephant trunk” total aortic arch replacement using a multi-branched, collared graft prosthesis. Heart vessels. doi:10.1007/s00380-014-0612-6
Rampoldi V, Trimarchi S, Eagle KA, Nienaber CA, Oh JK, Bossone E, Myrmel T, Sangiorgi GM, De Vincentiis C, Cooper JV, Fang J, Smith D, Tsai T, Raghupathy A, Fattori R, Sechtem U, Deeb MG, Sundt TM 3rd, Isselbacher EM, International Registry of Acute Aortic Dissection (IRAD) Investigators (2007) Simple risk models to predict surgical mortality in acute type A aortic dissection: The international registry of acute aortic dissection score. Ann Thorac Surg 83:55–61
Tan ME, Dossche KM, Morshuis WJ, Knaepen PJ, Defauw JJ, van Swieten HA, van Boven WJ, Kelder JC, Waanders FG, Schepens MA (2003) Operative risk factors of type A aortic dissection: analysis of 252 consecutive patients. Cardiovasc Surg 11:277–285
Geirsson A, Szeto WY, Pochettivo A, McGarvey ML, Keane MG, Woo YJ, Augoustides JG, Bavaria JE (2007) Significance of malperfusion syndromes prior to contemporary surgical repair for acute type A dissection: outcomes and need for additional revascularizations. Eur J Cardiothorac Surg 32(2):255–262
Chou HT, Lo JP, Chua CH, Lu MJ, Lin CH (2015) Initial Experience of modified four-branched graft technique and antegrade TEVAR in acute type A aortic dissection. Ann Thorac Cardiovasc Surg. doi:10.5761/atcs.oa.15-00015
Sacks D, McClenny TE, Cardella JF, Lewis CA (2003) Society of Interventional Radiology clinical practice guidelines. J Vasc Interv Radiol 14(9):S199–S202
Midulla M, Renaud A, Martinelli T, Koussa M, Mounier-Vehier C, Prat A, Beregi JP (2011) Endovascular fenestration in aortic dissection with acute malperfusion syndrome: immediate and late follow-up. J Thorac Cardiovasc Surg 142:66–72
Beregi JP, Haulon S, Otal P, Thony F, Bartoli JM, Crochet D, Lacombe P, Bonneville JF, Besse F, Douek P, Heautot JF, Rousseau H, Societé Fraçaise d’Imagerie Cardio-Vasculaire (SFICV) Research Group on Aortic Dissection (2003) Endovascular treatment of acute complications associated with aortic dissection: midterm results from a multicenter study. J Endovasc Ther 10:486–493
Patel HJ, Williams DM, Meerkov M, Dasika NL, Upchurch GR, Deeb GM (2009) long-term results of percutaneous management of malperfusion in acute type B aortic dissection: implications for thoracic aortic endovascular repair. J Thorac Cardiovasc Surg 138:300–308
Slonim SM, Miller DC, Mitchell RS, Semba CP, Razavi MK, Dake MD (1999) percutaneous balloon fenestration and stenting for life-threatening ischemic complications in patients with acute aortic dissection. J Thorac Cardiovasc Surg 117:1118–1126
Neri E, Toscano T, Massetti M, Capannini G, Carone E, Tucci E, Diciolla F, Scolletta S, Morello R, Sassi C (2001) Operation for acute type A aortic dissection in octogenarians: is it justified? J Thorac Cardiovasc Surg 121:259–267
Mehta RH, O’Gara PT, Bossone E, Nienaber CA, Myrmel T, Cooper JV, Smith DE, Armstrong WF, Isselbacher EM, Pape LA, Eagle KA, Gilon D, International Registry of Acute Aortic Dissection (IRAD) Investigators (2002) Acute type A aortic dissection in the elderly: clinical characteristics, management, and outcomes in the current era. J Am Coll Cardiol 40:685–692
Trimarchi S, Eagle KA, Nienaber CA, Rampoldi V, Jonker FH, De Vincentiis C, Frigiola A, Menicanti L, Tsai T, Froehlich J, Evangelista A, Montgomery D, Bossone E, Cooper JV, Li J, Deeb MG, Meinhardt G, Sundt TM, Isselbacher EM, International Registry of Acute Aortic Dissection Investigators (2010) Role of age in acute type A aortic dissection outcome: report from the international registry of acute aortic dissection (IRAD). J Thorac Cardiovasc Surg 140:784–789
Rylski B, Suedkamp M, Beyersdorf F, Nitsch B, Hoffmann I, Blettner M, Weigang E (2011) Outcome after surgery for acute aortic dissection type A in patients over 70 years: data analysis from the german registry for acute aortic dissection type A (GERAADA). Eur J Cardiothorac Surg 40:435–440
Tang GH, Malekan R, Yu CJ, Kai M, Lansman SL, Spielvogel D (2013) Surgery for acute type A aortic dissection in octogenarians is justified. J Thorac Cardiovasc Surg 145:S186–S190
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Rights and permissions
About this article
Cite this article
Colli, A., Carrozzini, M., Galuppo, M. et al. Analysis of early and long-term outcomes of acute type A aortic dissection according to the new international aortic arch surgery study group recommendations. Heart Vessels 31, 1616–1624 (2016). https://doi.org/10.1007/s00380-015-0770-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00380-015-0770-1