Abstract
The vertebrate heart is regulated by excitatory adrenergic and inhibitory cholinergic innervations, as well as non-adrenergic non-cholinergic (NANC) factors that may be circulating in the blood or released from the autonomic nerves. As an example of NANC signaling, an increased histaminergic tone, acting through stimulation of H2 receptors, contributes markedly to the rise in heart rate during digestion in pythons. In addition to the direct effects of histamine, it is also known that histamine can reinforce the cholinergic and adrenergic signaling. Thus, to further our understanding of the histaminergic regulation of the cardiovascular response in pythons, we designed a series of in vivo experiments complemented by in vitro experiments on sinoatrial and vascular ring preparations. We demonstrate the tachycardic mechanism of histamine works partly through a direct binding of cardiac H2 receptors and in part through a myocardial histamine-induced catecholamine release, which strengthens the sympathetic adrenergic signaling pathway.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The heart of tetrapods and teleost fish is dually innervated by excitatory adrenergic sympathetic nerves and inhibitory cholinergic parasympathetic nerves (Burnstock 1969; Sandblom and Axelsson 2011; Wang 2012; Taylor et al. 2014). Resting reptiles typically exhibit a high cholinergic tone and a low adrenergic tone, and the characteristic tachycardia during exercise is normally mediated by withdrawal of the parasympathetic tone in combination with an increased sympathetic tone (Wang et al. 2001; Joyce et al. 2018; Joyce and Wang 2020). It is, however, also clear that non-adrenergic non-cholinergic (NANC) signals, such as histamine, secretin, insulin and oxyntomodulin, exert profound effects on heart rate (fH) in some vertebrates (Gunnes et al. 1983; Baron 1994; Sowden et al. 2007; Skovgaard et al. 2009). These NANC factors may be circulating hormones (Enok et al. 2012), neurotransmitters being released from the autonomic nerves innervating the heart [i.e., co-transmission with the classic neurotransmitters (Burnstock 1976; Li et al. 2006)], or released directly from the heart (Tota et al. 2010). The NANC regulation of fH is pronounced during digestion in snakes where more than half of the tachycardia supporting the metabolic responses to digestion (specific dynamic action, SDA) can be ascribed to NANC stimulation of the heart (Wang et al. 2001; Enok et al. 2012; Burggren et al. 2014).
In pythons, the initial NANC stimulation of fH during digestion is due to the appearance of a histaminergic tone with activation through H2 receptors (Skovgaard et al. 2009; Enok et al. 2012). Consequently, the postprandial tachycardia depends on both a withdrawal of vagal tone and a doubling of intrinsic fH (i.e., fH after the combination of atropine and propranolol), executed by histamine (Skovgaard et al. 2009). It has recently been reported that histamine also exerts a positive chronotropic effect in rattlesnakes, turtles and caimans (Skovgaard et al. 2018). Histamine additionally plays a major role in cardiovascular regulation during embryonic development of the red-footed tortoise (Crossley et al. 2013) where fH is partially governed by a histaminergic tone, which can be blocked by the H2 receptor antagonist ranitidine, and may serve to compensate for limited autonomic regulation.
While histamine acts on histaminergic receptors, some of the histaminergic response in mammals originates via adrenergic pathways (Flacke et al. 1967; Subramanian and Mulder 1977; Laher and McNeill 1980a; Li et al. 2006). Furthermore, Enok et al. (2012) noted that the H2-receptor antagonist ranitidine did not alter fH in digesting P. molurus after the administration of propranolol and atropine. These observations indicate that histamine does not work solely through a direct mechanism on histaminergic receptors. We were, therefore, compelled to investigate the potential histaminergic-adrenergic interaction in pythons by measuring maximal changes in fH upon histamine administration in combination with different pre- and postganglionic blockers, adrenergic, cholinergic, and histaminergic antagonists. First, we described the magnitude of the histaminergic change in fH in vivo using fully recovered snakes, and we then characterized the histaminergic change in fH in vitro using isolated heart preparations to avoid confounding effects of circulating catecholamines and other autonomic compensatory responses. We report that histamine is able to induce tachycardia partly through a direct binding of H2-receptors, and by inducing a myocardial catecholamine release with subsequent activation of β-adrenoceptors.
Materials and methods
Experimental animals
54 Python regius with a body mass ranging from 60 to 568 g (294.8 ± 20.6 g) and 8 Python sebae (for microvascular myography experiments only) weighing between 125 and 237 g (172.5 ± 12.3 g) were purchased from a commercial supplier and kept at Aarhus University in vivaria with a local heat source providing a temperature gradient from 25 to 32 °C at a photoperiod of 12:12 h. These two species are closely related (Reynolds et al. 2014) and studies from our lab reveal very similar physiological responses to autonomic agonists and antagonists with the family of Pythonidae (T. Wang unpublished findings). Animals were fed weekly and had free access to water, but were fasted for 2 weeks before experimentation to ensure a post-absorptive state. All snakes grew during captivity and appeared healthy. The snakes were kept at 30 °C in climatic chambers during measurements, where they were shielded from visual and auditory disturbances. Experiments were performed according to Danish Federal Regulations.
Surgery and instrumentation
Anesthesia was induced by enclosing the snakes in an inflated zip-lock bag containing swabs saturated with isoflurane (IsoFlo® vet 100%, Abbott Laboratories) for 5–10 min (Eatwell 2010). The trachea was intubated with soft polyethylene tube for mechanical ventilation (Harvard Apparatus mechanical ventilator; Cambridge, MA, USA) with 1–5% isoflurane (Fluotec three vaporizer; Simonsen and Weel; Vallensbæk, Denmark) at five breaths min−1 and a tidal volume of 30 ml kg−1. After subcutaneous application of lidocaine, a ventrolateral incision posterior to the kidney allowed access for occlusive cannulation of the vertebral artery with a polyethylene (PE)-50 catheter containing heparinized saline (50 IU/ml) to measure mean arterial blood pressure (MAP). The catheter was exteriorized through a small incision in the skin and fastened with three sutures. Snakes were allowed to recover for 18–36 h at 30 °C within a climatic chamber; Olesen et al. (2008) previously showed that fH and MAP return to resting values within 24 h. MAP was measured by connecting the arterial catheter to a pressure transducer (PX600; Baxter Edwards, Irvine, CA, USA), calibrated daily against a static water column and connected to an in-house built preamplifier, and fH was derived from the pulsatile pressure. Signals were recorded at 100 Hz using Biopac MP100 data acquisition system (Biopac Systems; Goleta, CA, USA).
Experimental protocols
We investigated the effect of histamine prior to and after administration of pre- and postganglionic blockers, adrenergic, cholinergic and histaminergic antagonists. All drugs were given in aliquots of 1 ml kg−1 through the arterial catheter, except for reserpine (used for sinoatrial preparation study only), which was administered intraperitoneally at 24 and 48 h prior to harvesting the hearts for in vitro studies. Infusion of similar volumes of saline (sham injections) caused negligible and short lasting changes in blood pressure. MAP and fH were measured 20–30 min after administration of each drug, except for histamine, where we recorded the maximal cardiac and vascular responses. Hemodynamic variables were allowed to return to baseline after each histamine injection before continuing the experimental protocol.
Does the indirect effect of histamine originate from an increased adrenergic tone or a release of cholinergic tone?
To investigate whether histamine exerts indirect actions, i.e., whether the histaminergic change in fH depends on adrenergic or cholinergic stimulation, we tested whether the histaminergic response in fH changed after an autonomic blockade. We measured MAP and fH in six snakes at rest, followed by a bolus injection of histamine (100 nmol kg−1) prior to and after the muscarinic acetylcholine-receptor antagonist atropine (3 mg kg−1) and the β-adrenergic receptor antagonist propranolol (3 mg kg−1). A final bolus of histamine was given after the histamine H2-receptor antagonist ranitidine (40 mg kg−1). Antagonists were administered sequentially and histamine boluses repeated in the same individual snakes.
To test any indirect effects of atropine and propranolol non-collectively, ten fasting snakes in two groups were used to study the adrenergic and cholinergic tones after histamine. Five snakes received a bolus of histamine (100 nmol kg−1) before and after atropine (3 mg kg−1) and propranolol (3 mg kg−1), whereas the order of atropine and propranolol was reversed in the other five snakes.
Does histamine affect tonus in the vasculature?
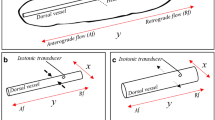
To investigate the effects of histamine on the vasculature and the underlying mechanism, a series of microvascular myograph studies were conducted. In these studies, the direct effects of histamine were investigated without the confounding effects of autonomic reflexes or circulating catecholamines. Snakes were anaesthetised with isoflurane, decapitated and opened up so the stomach and intestine could be removed en bloc and placed in ice-cold physiological salt solution (PSS): (mM) 119 NaCl, 25 NaHCO3, 1.18 KH2PO4, 4.7 KCl, 1.17 MgSO4, 1.6 CaCl2, 5.5 glucose and 0.026 EDTA. We isolated 1.5–2 mm long segments of gastric and mesenteric arteries with diameters of approximately 300–400 μm that were mounted on 40 μm stainless steel wires on a wire-myograph (Model 410A, Danish Myo Technology, Aarhus, Denmark) for recording of isometric tension (Mulvany and Halpern 1977) using a PowerLab data acquisition system (ADInstruments, Oxfordshire, England). The vessels were kept in PSS at 30 °C bubbled with 5% CO2/room air (pH = 7.4) delivered by a gas mixing pump (Wösthoff, Bochum, Germany). Vessels were left for 30 min to stabilize and resting tension was normalized by adjusting the diameter of the vessel with a micrometer screw to a transmural pressure of 6.27 kPa (Enok et al. 2012). Contractility of all vessels was evaluated in a high K+ solution (KPSS 123.7 mM), which is PSS with NaCl substituted by KCl on an equimolar basis. To investigate the effects of histamine on isolated stomach and intestine arteries, histamine concentration–response curves (histamine 10–8–10–4 M) were constructed in vessels incubated for 30 min with vehicle (control), the histamine H2-receptor antagonist ranitidine (10–6 M), histamine H1-receptor antagonist diphenhydramine (10–6 M) or α-adrenoceptor antagonist phentolamine (10–5 M). Following the series of histamine dilutions, the effects of histamine (10–4 M) and acetylcholine (10–3 M) were evaluated before and after incubation (30 min) with atropine (10–5 M).
Does the increase in adrenergic tone arise from a postganglionic mechanism?
To obtain a measure of the maximal fH and to manipulate the postganglionic release of noradrenaline we measured resting MAP, fH, and changes in these upon injection of histamine (100 nmol kg−1) in six snakes. Finally, the maximal responses were measured after enforced activity by provoking the snakes to strike or hiss at least three times within 1 min. The same procedure was carried out 24 h after the postganglionic adrenergic neuron-blocker bretylium tosylate (10 mg kg−1).
Does the increased adrenergic tone stem from myocardial histamine-induced catecholamine release?
To investigate whether histamine elicits a myocardial release of catecholamines, we determined the chronotropic effects of histamine on heart strip preparations in vitro. In these preparations, there are no confounding effects of autonomic compensatory regulation or circulating catecholamines. 16 fasting snakes were anesthetized with isofluorane before the hearts were removed and dissected to provide a pacemaker-containing sinoatrial preparation. Each cardiac preparation mounted vertically with the upper end attached to a force transducer (model UC 2; Statham, Oxnard, CA, USA) and the lower to a fixed hook, to measure intrinsic fH. All preparations were suspended in water-jacketed (30 °C) organ baths with 50 ml Ringer’s solution typical for reptiles (Joyce et al. 2014): (mM) 95 NaCl, 2.5 KCl, 1 MgSO4, 1 NaH2PO4, 5 glucose, 1.5 CaCl2, 25 NaHCO3 and a pH of 7.7), bubbled with 48% O2, 2% CO2 and 50% N2 by a Wösthoff mixing pump (Wösthoff, Bochum, Germany). The preparations were given 30 min recovery after mounting, before they were stretched using a micrometer screw to reach maximum force of contraction, again followed by 30 min recovery time before initiating measurements. Each preparation was treated with cumulative administrations of histamine (10–8, 10–7, 10–6, 10–5 and 10–4 M). Propranolol-treated heart strips were incubated with propranolol (10–4 M) until they stabilized before the cumulative histamine administration. In a separate group of snakes, the catecholamine-depleting agent reserpine was injected intraperitoneally (5 mg kg−1) 48 and 24 h prior to measurements. All drug concentrations were based on previously published protocols (Laher and McNeill 1980a; Temma et al. 1989; Skovgaard et al. 2009) and preliminary experiments.
Is histamine of mast cell origin in Python regius?
To reveal whether the histamine acting on the heart stems from mast cells or from another source, as shown in P. molurus (Enok et al. 2012), MAP and fH were measured in 10 digesting snakes fed a rodent meal corresponding to 25% of body mass, five untreated snakes and five snakes injected every sixth hour with the mast cell stabilizer cromolyn (25 mg kg−1). Injections were started 1 h prior to the fasting measurement. Cardiovascular parameters were recorded in fasted snakes, before all snakes were fed. MAP and fH were then recorded 24 h into the postprandial period and after atropine (4 mg kg−1), propranolol (4 mg kg−1) and ranitidine (40 mg kg−1).
Data analysis and statistics
For in vivo studies, fH and MAP were compared within treatments prior to histamine injections and as histaminergic changes in fH and MAP with two-way ANOVAs for repeated measures and Tukey’s multiple comparison tests. Levels of fHs, and MAPs before and after histamine injections and histaminergic changes in fHs and MAP were compared between treatments. Adrenergic and cholinergic tones on the heart were calculated as Skovgaard et al. (2009) using equations from Altimiras et al. (1997), on the basis of the R-R interval (fH−1), and the histaminergic tone was calculated as changes in R-R interval upon administration of the H2-receptor antagonist ranitidine relative to the triple block (after a complete blockade).
For in vitro heart strips studies, histaminergic changes in fH and the inotropic change exerted by histamine were compared at different histamine concentrations, between different treatments or between different cardiac tissues, and evaluated by a two-way ANOVA for repeated measures and Tukey’s multiple comparisons tests.
Wire-myograph data recordings were analysed using Chart5™ software (ADInstruments, Oxfordshire, England). The mechanical response of the vessel segments was measured as active wall tension, which is the change in force divided by twice the segment length (Mulvany and Halpern 1977). Data were evaluated with a two-way ANOVA or a one-way ANOVA for repeated measures followed by a Holm-Sidak post hoc test.
Differences were considered statistically significant at a 95% level of confidence (p < 0.05). All data are presented as mean S.E.M.
Results
In vivo test using specific H2-receptor antagonist ranitidine
Resting snakes were characterized by a large inhibitory cholinergic tone (50 ± 19%), and absent excitatory adrenergic (− 21 ± 16%) and histaminergic tones (− 3 ± 5%). Histamine caused a marked tachycardia in fasting undisturbed snakes, more than doubling the fH from 19.5 ± 2.6 to 51.3 ± 3.7 min−1 (Fig. 1a). Autonomic double blockade increased fH to 29.3 ± 1.9 min−1 and reduced the histaminergic change in fH from 31.8 ± 2.3 to 14.6 ± 3.3 min−1 (p < 0.001), the same as the reduction induced solely by propranolol; 16.2 ± 2.6 min−1 (p = 0.985; change in fH after propranolol vs. change in fH after atropine; Fig. 1a). Ranitidine completely abolished the remaining effect of histamine (p = 0.998). The histaminergic hypertension was abolished after double autonomic blockade (p = 0.022; Fig. 1b).
In vivo effects of a histamine bolus (100 nmol kg−1) on fH a and MAP b during rest, after propranolol (3 mg kg−1), a double block; addition of atropine (3 mg kg−1), and a triple block; addition of ranitidine (40 mg kg−1). The antagonists were administered sequentially between repeat histamine injections. Black bars are before histamine, white bars are maximal responses to histamine, and gray bars are the histaminergic changes in fH and MAP. Broken line in A at 65.0 min−1 is the maximal fH. An asterisk represents significant differences upon administration of histamine, and letters represent significant differences between treatments within one group (p < 0.05) evaluated by a two-way ANOVA. Values are means ± S.E.M., n = 6 (except for measurements after propranolol, which were only carried out on four animals)
In vivo and in vitro tests using muscarinic antagonist atropine, β-adrenoceptor antagonist propranolol and α-adrenoceptor antagonist phentolamine
As described earlier, histamine doubled fH in fasting snakes with a rise from 18.2 ± 1.1 and 22.2 ± 2.5 min−1 to 45.2 ± 1.4 min−1 and 45.7 ± 2.2 min−1 (Fig. 2a, c). Atropine induced a significant tachycardia (p < 0.001), and the histaminergic change in fH was reduced (p = 0.016; Fig. 2c). Propranolol significantly dampened the effects of histamine (p < 0.001). When propranolol was given before atropine, propranolol reduced the histaminergic change in fH profoundly, from 27.0 ± 1.7 to 13.6 ± 2.0 min−1 (Fig. 2a). Regardless of the double blockade order, the histaminergic change in fH decreased and was less than half of the effect in resting animals (Fig. 2a, c). Atropine completely abolished the hypertensive effect of histamine (Fig. 2d).
In vivo effects of histamine (100 nmol kg−1) on fH (a, c) and MAP (b, d) during rest, after propranolol (3 mg kg−1) or atropine (3 mg kg−1) and after a double blockade in vivo. Black bars are before histamine, white bars are maximal responses to histamine, and gray bars are the histaminergic changes in fH and MAP. Broken line in A at 65.0 min−1 is the maximal fH. An asterisk represents significant difference after histamine, and letters represent significant differences between treatments within one group (p < 0.05) evaluated by a two-way ANOVA. Values are means ± S.E.M., n = 5
Histamine induced a contraction in isolated stomach and intestine arteries, which was completely blocked by the histamine H1-receptor antagonist diphenhydramine (Fig. 3a, b). There were no effects of the α-adrenoceptor antagonist phentolamine. However, when the same vessels were incubated with atropine the effects of histamine were abolished (Fig. 3c).
Effects of histamine in isolated small intestine arteries a and isolated small stomach arteries b incubated with vehicle (control), the histamine H1-receptor antagonist, diphenhydramine (10–6 M), the histamine H2-receptor antagonist, ranitidine (10–6 M) or the α-adrenergic antagonist phentolamine (10–5 M). Data are presented as mean ± S.E.M., n = 6–8. An asterisk represents a significant difference from control curve and crosses in circles represent a significant difference from initial histamine concentration (10–8 M) (p < 0.05) evaluated by a two-way ANOVA followed by a Holm-Sidak post hoc test. c Effects of histamine (10–4 M) before and after incubation with the cholinergic antagonist atropine (10–5 M) in small intestine arteries (black bars) and small stomach arteries (open bars). Data are presented as mean ± S.E.M., n = 3. An asterisk represents significant difference from pre-incubation values of histamine (p < 0.05) evaluated by a one-way ANOVA for repeated measures followed by a Holm-Sidak post hoc test
In vivo test using adrenergic neuron-blocker bretylium tosylate
Bretylium tosylate did not affect fH at rest or during enforced activity (p = 0.119; 0.906, respectively), but the effect of histamine was exacerbated (p = 0.016; Fig. 4a). The fH of 65.0 ± 1.6 min−1 at enforced activity after bretylium tosylate (marked with a broken line in all figures depicting fH) was considered the maximal fH throughout the in vivo measurements. Histamine caused a significant elevation of MAP in both untreated and bretylium tosylate-treated snakes (p < 0.001; p = 0.017, respectively; Fig. 4b), while enforced activity had no significant effect (p = 0.483). Bretylium tosylate caused small reductions in MAP after histamine and during activity compared to untreated snakes (p = 0.001 and 0.039, respectively).
In vivo effects of the postganglionic adrenergic neuron-blocker bretylium tosylate (BT; 10 mg kg−1) on fH a and MAP b during rest, after histamine (His.; 100 nmol kg−1) and to enforced activity. Black bars are before bretylium tosylate, white bars are after. Broken line in A at 65.0 min−1 is the maximal fH. An asterisk represents significant difference after bretylium tosylate, and letters represent significant differences between treatments within one group (p < 0.05) evaluated by two-way ANOVA. Values are means ± S.E.M., n = 6
In vitro heart preparations
We did not observe any difference in base fH between control and reserpine pre-treated sinoatrial strips (p = 0.820), both were significantly higher than fH of propranolol-treated strips (p = 0.014; p = 0.001, respectively; Fig. 5a), and both were significantly higher than fH of propranolol-treated strips at every histamine concentration. Control sinoatrial strips were sensitive to a histamine concentration of 10–6 M, where the histaminergic change in fH increased by 12.5 ± 5.6 min−1 (p = 0.001; Fig. 5a). The histaminergic changes in fH in both propranolol-treated and reserpine pre-treated sinoatrial strips were insensitive at this histamine concentration (p = 0.906), but responded to 10–5 M histamine (p < 0.001 for both). The histaminergic change in fH of controls was significantly higher than the histaminergic change in fH of reserpine pre-treated at 10–6, 10–5 and 10–4 M histamine (p = 0.004) and higher than that of propranolol-treated strips at 10–4 (p = 0.012).
Effects of cumulative administration of histamine on intrinsic fH a and the histaminergic change in fH, ΔfH b, in sinoatrial preparations treated with vehicle (control, black), propranolol (10–4 M, orange) and reserpine (5 mg kg−1, pre-treated intraperitoneally 48 and 24 h prior to experimentation, green). An asterisk represents a significant difference from control preparations and crosses in circles represent a significant difference from initial histamine concentration (0 M) (p < 0.05) evaluated by two-way ANOVA). Values are means ± S.E.M., n = 5–6
In vivo test using mast cell stabilizer cromolyn
Fasting fH of control and mast cell-stabilized snakes did not differ (p = 0.999). In both groups, fH doubled after 24 h of digestion (Fig. 6a), atropine induced tachycardia, propranolol elicited bradycardia, and ranitidine lowered fH to fasting levels (p = 0.217 compared to controls; p = 0.054 compared to cromolyn-treated snakes). After 24 h of digestion the cholinergic tone decreased (to 11 ± 8%) and the histaminergic tone increased (to 31 ± 11%; Fig. 6). There were no significant differences in fH or MAP between control and cromolyn-treated snakes at any measurement (p = 0.361 for fH; p = 0.093 for MAP).
In vivo effects of the mast cell stabilizer cromolyn (25 mg kg−1) on fH a and MAP b. Black bars are control snakes, n = 5, and white bars are cromolyn-treated snakes, n = 5. Measurements were carried out in resting, fasting snakes, 24 h into digestion, after atropine (4 mg kg−1), propranolol (Propran.; 4 mg kg−1) and ranitidine (40 mg kg−1). Broken line in A at 65.0 min−1 is the maximal fH. Letters represent significant differences between treatments within one group (p < 0.05) evaluated by two-way ANOVA. Values are means ± S.E.M
Discussion
Our findings indicate that there is a more complex mechanism for the action of histamine than previously appreciated in reptiles (Skovgaard et al. 2009, 2018), and demonstrate that histamine acts both directly on histaminergic receptors and through adrenergic and cholinergic mechanisms.
Chronotropic responses to histamine
Our in vivo studies confirm a pronounced tachycardia in response to histamine injections in fully recovered pythons (Skovgaard et al. 2009), and we demonstrate that the β-adrenergic antagonist propranolol greatly diminished this tachycardia. This indicates an adrenergic component of the histamine fH response, in addition to the direct effect of histamine on H2-receptors (Skovgaard et al. 2009). Histamine could either bind directly to β-adrenoceptors on the cardiac pacemaker, as suggested in carp ventricle (Temma et al. 1989), or histamine could induce a release of catecholamines from postganglionic sympathetic cardiac neurons (Li et al. 2006).
To investigate whether the adrenergic component arose from catecholamines in postganglionic sympathetic nerves, we used the sympathetic neuron blocker bretylium tosylate. Bretylium tosylate did not affect the histaminergic tachycardia and did not attenuate the tachycardia in response to stress (enforced activity), which seems primarily mediated through circulating catecholamines released from chromaffin tissue (Stinner and Ely 1993). Thus, it is likely that the adrenergic component of the histamine response is not a consequence of noradrenaline released from sympathetic cardiac neurons. The tachycardia during enforced activity was similar to that previously reported in P. molurus (Secor et al. 2000) and Boa constrictor (Wang et al. 2001).
The in vivo experiments do not allow for dissociation of autonomic compensatory cardiovascular responses and a histamine-induced release of catecholamines from sympathetic neurons or the adrenal medulla. We therefore studied the indirect effects of histamine on the intrinsic fH of isolated in vitro sinoatrial preparations harboring the pacemaker (Skovgaard et al. 2009). Reserpine, which depletes presynaptic catecholamines in neurons (Li et al. 2007) and blocks catecholamine release from the adrenal medulla (Hillarp 1960) and the myocardium (Temma et al. 1989a), reduced the responses of the sinoatrial preparations to histamine. Similarly, to the in vivo findings, β-adrenoceptor blockade with propranolol also reduced the sinoatrial responses to histamine, indicating that histamine, in addition to the direct stimulation of H2-receptors, induces tachycardia indirectly by inducing catecholamine release, further stimulating β-adrenoceptors. This histamine-induced catecholamine release is likely to be elicited through H2-receptor stimulation since the in vivo chronotropic effects of histamine were abolished by the combination of propranolol and ranitidine. The existence of a histamine-induced catecholamine release has been previously suggested in feline (Laher and McNeill 1980a), canine (Flacke et al. 1967) and rodent cardiac tissues (Laher and McNeill 1980b), but this is the first description in an ectothermic vertebrate.
Effects of histamine on MAP in vivo and contractility of isolated blood vessels in vitro
Our in vivo experiments showed that the hypertensive effects of histamine were abolished by atropine, and our in vitro studies on the isolated blood vessels confirm that atropine could greatly attenuate the constriction otherwise elicited by histamine. These are surprising findings given the general absence of parasympathetic innervation of the vascular system. It is likely, however, that atropine can exert a competitive antagonist effect on the histaminergic receptors (Arunlakshana and Schild 1997). Thus, the histamine-mediated vasoconstriction was abolished by an H1-receptor blockade as well as a cholinergic block by atropine.
Chronotropic effects of mast cells
Finally, our in vivo studies showed that cromolyn did not affect the postprandial cardiovascular response, which supports the view that the regulating histamine is of non-mast cell origin in pythons (Enok et al. 2012). The source of histamine release during digestion remains enigmatic.
Conclusions
In addition to the direct action through stimulation of H2-receptors, histamine acts indirectly by stimulating a release of catecholamines, probably via H2-receptors, activating β-adrenoceptors in the python heart. Histamine is an important regulator of the cardiovascular system in other reptiles (Crossley et al. 2013; Skovgaard et al. 2018), so our results are likely broadly relevant across the reptile phylogeny. The finding of this indirect mechanism reveals multiple roles of histamine, both in postprandial and pathological processes, e.g., during anaphylactic shock, where circulating and myocardial released histamine might have even more profound effects through release of catecholamines (Genovese and Spadaro 1997). Finally, we confirm that histamine is not released from mast cells in digesting P. regius, which has also been shown in P. molurus (Enok et al. 2012).
The hormone-induced catecholamine release might not be a histamine-specific property. Observations of propranolol abolishing a neurotensin-induced tachycardia in pythons (Skovgaard et al. 2007) might be, as hypothesized previously, due to a neurotensin-mediated presynaptic release of catecholamines from sympathetic nerves innervating the heart. This could also indicate a more prevalent phenomenon of hormones’ ability to release local pools of catecholamines.
References
Altimiras J, Aissaoui A, Tort L, Axelsson M (1997) Cholinergic and adrenergic tones in the control of heart rate in teleosts. How should they be calculated? Comp Biochem Physiol 118A:131–139. https://doi.org/10.1016/S0300-9629(96)00402-1
Arunlakshana O, Schild HO (1997) Some quantitative uses of drug antagonists. Br J Pharmacol 120:151–161. https://doi.org/10.1111/j.1476-5381.1997.tb06793.x
Baron AD (1994) Hemodynamic actions of insulin. Am J Physiol 267:E187-202. https://doi.org/10.1152/ajpendo.1994.267.2.E187
Burggren WW, Christoffels VM, Crossley DA, Enok S, Farrell AP, Hedrick MS, Hicks JW, Jensen B, Moorman AFM, Mueller CA, Skovgaard N, Taylor EW, Wang T (2014) Comparative cardiovascular physiology: future trends, opportunities and challenges. Acta Physiol (Oxf) 210:257–276. https://doi.org/10.1111/apha.12170
Burnstock G (1969) Evolution of the autonomic innervation of visceral and cardiovascular systems in vertebrates. Pharmacol Rev 21:247–324
Burnstock G (1976) Do some nerve cells release more than one transmitter? Neuroscience 1:239–248
Crossley DA, Sartori MR, Abe AS, Taylor EW (2013) A role for histamine in cardiovascular regulation in late stage embryos of the red-footed tortoise, Chelonoidis carbonaria Spix, 1824. J Comp Physiol 183:811–820. https://doi.org/10.1007/s00360-013-0746-3
Eatwell K (2010) Options for analgesia and anaesthesia in reptiles. Practice 32:306–311. https://doi.org/10.1136/inp.c3917
Enok S, Simonsen LS, Pedersen SV, Wang T, Skovgaard N (2012) Humoral regulation of heart rate during digestion in pythons (Python molurus and Python regius). Am J Physiol 302:R1176-1183. https://doi.org/10.1152/ajpregu.00661.2011
Flacke W, AtanackoviĆ D, Gillis RA, Alper MH (1967) The Actions of Histamine on the Mammalian Heart. J Pharmacol Exp Ther 155:271–278
Genovese A, Spadaro G (1997) Highlights in cardiovascular effects of histamine and H1-receptor antagonists. Allergy 52:67–78
Gunnes P, Waldum HL, Rasmussen K et al (1983) Cardiovascular effects of secretin infusion in man. Scand J Clin Lab Invest 43:637–642
Hillarp NA (1960) Effect of reserpine on the nucleotide and catecholamine content of the denervated adrenal medulla of the rat. Nature 187:1032
Joyce W, Wang T (2020) What determines systemic blood flow in vertebrates? J. Exp. Biol. 223:215335
Joyce W, Gesser H, Wang T (2014) Purinoceptors exert negative inotropic effects on the heart in all major groups of reptiles. Comp Biochem Physiol 171A:16–22. https://doi.org/10.1016/j.cbpa.2014.02.005
Joyce W, Miller TE, Elsey RM, Wang T, Crossley DA (2018) The effects of embryonic hypoxic programming on cardiovascular function and autonomic regulation in the American alligator (Alligator mississippiensis) at rest and during swimming. J Comp Physiol B. https://doi.org/10.1007/s00360-018-1181-2
Laher I, McNeill JH (1980a) Effects of histamine in the isolated kitten heart. Can J Physiol Pharmacol 58:1256–1261
Laher I, McNeill JH (1980b) Effects of histamine on rat isolated atria. Can J Physiol Pharmacol 58:1114–1116
Li M, Hu J, Chen Z et al (2006) Evidence for histamine as a neurotransmitter in the cardiac sympathetic nervous system. Am J Physiol 291:H45-51. https://doi.org/10.1152/ajpheart.00939.2005
Li M, Hu J, Chen T et al (2007) Histamine in Macaca mulatto monkey cardiac sympathetic nerve system: a morphological and functional assessment. Auton Neurosci 137:37–43. https://doi.org/10.1016/j.autneu.2007.06.285
Mulvany MJ, Halpern W (1977) Contractile properties of small arterial resistance vessels in spontaneously hypertensive and normotensive rats. Circ Res 41:19–26
Olesen MG, Bertelsen MF, Perry SF, Wang T (2008) Effects of preoperative administration of butorphanol or meloxicam on physiologic responses to surgery in ball pythons. J Am Vet Med Assoc 233:1883–1888. https://doi.org/10.2460/javma.233.12.1883
Reynolds RG, Niemiller ML, Revell LJ (2014) Toward a tree-of-life for the boas and pythons: multilocus species-level phylogeny with unprecendented taxon sampling. Mol Phylogenet Evol 71:201–213. https://doi.org/10.1016/j.ympev.2013.11.011
Sandblom E, Axelsson M (2011) Autonomic control of circulation in fish: A comparative view. Autonom Neurosci 165:127–139. https://doi.org/10.1016/j.autneu.2011.08.006
Secor SM, Hicks JW, Bennett AF (2000) Ventilatory and cardiovascular responses of a python (Python molurus) to exercise and digestion. J Exp Biol 203:2447–2454
Skovgaard N, Conlon JM, Wang T (2007) Evidence that neurotensin mediates postprandial intestinal hyperemia in the python, Python regius. Am J Physiol 293:R1393-1399. https://doi.org/10.1152/ajpregu.00256.2007
Skovgaard N, Møller K, Gesser H, Wang T (2009) Histamine induces postprandial tachycardia through a direct effect on cardiac H2-receptors in pythons. Am J Physiol 296:R774-785. https://doi.org/10.1152/ajpregu.90466.2008
Skovgaard N, Abe AS, Taylor EW, Wang T (2018) Cardiovascular effects of histamine in three widely diverse species of reptiles. J Comp Physiol B 188:153–162. https://doi.org/10.1007/s00360-017-1108-3
Sowden GL, Drucker DJ, Weinshenker D, Swoap SJ (2007) Oxyntomodulin increases intrinsic heart rate in mice independent of the glucagon-like peptide-1 receptor. Am J Physiol 292:R962-970. https://doi.org/10.1152/ajpregu.00405.2006
Stinner JN, Ely DL (1993) Blood pressure during routine activity, stress, and feeding in black racer snakes (Coluber constrictor). Am J Physiol 264:R79-84. https://doi.org/10.1152/ajpregu.1993.264.1.R79
Subramanian N, Mulder AH (1977) Modulation by histamine of the efflux of radiolabeled catecholamines from rat brain slices. Eur J Pharmacol 43:143–152
Taylor EW, Leite CAC, Sartori MR et al (2014) The phylogeny and ontogeny of autonomic control of the heart and cardiorespiratory interactions in vertebrates. J Exp Biol 217:690–703. https://doi.org/10.1242/jeb.086199
Temma K, Akamine M, Shimizu T et al (1989) Histamine directly acts on beta-adrenoceptors as well as H1-histaminergic receptors, and causes positive inotropic effects in isolated ventricular muscles of carp heart (Cyprinus carpio). Comp Biochem Physiol 92C:143–148
Tota B, Cerra MC, Gattuso A (2010) Catecholamines, cardiac natriuretic peptides and chromogranin A: evolution and physiopathology of a “whip-brake” system of the endocrine heart. J Exp Biol 213:3081–3103. https://doi.org/10.1242/jeb.027391
Wang T, Taylor EW, Andrade D, Abe AS (2001) Autonomic control of heart rate during forced activity and digestion in the snake Boa constrictor. J Exp Biol 204:3553–3560
Wang T (2012) Chapter 141 - Evolution of the cardiovascular autonomic nervous system in vertebrates. In: Robertson D, Biaggioni I, Burnstock G et al (eds) Primer on the autonomic nervous system, 3rd edn. Academic Press, San Diego, pp 669–673
Acknowledgements
This study was supported by the A.P. Møller Foundation and the Danish Independent Research
Council (Natur og Univers, Det Frie Forskningsråd).
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by Bernd Pelster.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nørgaard, S., Joyce, W., Jensen, M.F. et al. Histamine exerts both direct H2-mediated and indirect catecholaminergic effects on heart rate in pythons. J Comp Physiol B 191, 347–355 (2021). https://doi.org/10.1007/s00360-020-01338-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00360-020-01338-6