Abstract
Purpose
Salvage Radical Prostatectomy is challenging and associated with high rates of incontinence. The novel Retzius-sparing RARP (RS-RARP) approach has shown impressive high immediate and 1-year continence rates (> 90%) when applied as primary treatment. The purpose of this study is to evaluate the impact of salvage Retzius-sparing RARP (sRS-RARP) on continence outcomes in the salvage scenario.
Materials and methods
Using PRISMA guidelines, a systematic review and meta-analysis of articles was conducted on Medline through PubMed and on Cochrane through Central Register of Controlled Trials databases. Inclusion and exclusion criteria were used to select 17 retrospective cohort studies published until April 2023 about sRS-RARP and continence. Data were extracted independently by at least two authors. The International Prospective Register of Systematic Reviews (PROSPERO) was registered. Retrospective studies were subjected to a domain-based risk of bias assessment in accordance with the Newcastle–Ottawa quality assessment scale cohort studies (NOS). Prostate cancer patients were chosen from prospective nonrandomized or randomized sRS-RARP or sS-RARP studies that examined continence outcomes.
Results
Seventeen studies were included: 14 were retrospectives only and 3 described retrospective comparison cohorts (sRS-RARP vs sS-RARP). All the retrospective studies were of “fair” quality using the NOS. sRS-RARP may increase recovery of urinary continence after surgery compared to sS-RARP [OR 4.36, 95% CI 1.7–11.17; I2 = 46.8%; studies = 4; participants = 87].
Conclusions
sRS-RARP approach has potential to improve continence outcomes in the salvage setting.
Patient summary
sRS-RARP approach has potential to positively impact continence function on patients who underwent salvage surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate cancer (PCa) prevalence has substantially increased over decades. Its treatment has evolved substantially recently and retropubic approach for robotic-assisted radical prostatectomy is well stablished with recognized perioperative, oncological and function outcomes [1]. It has been already adopted as a standard surgical procedure in many urological centers over the world [2].
However, several studies have evaluated the efficacy and effectiveness of the modern Retzius-sparing robot-assisted radical prostatectomy technique. This emerging approach seems to improve urinary function and quality of life in patients with prostate cancer and has been found to not increase the risk of positive surgical margins or complications. Retzius-sparing prostatectomy impacts in early continence recovery 3 to 6 months faster than those who undergo conventional prostatectomy. Immediate urinary continence was also higher in the Retzius-sparing group compared to the standard technique. On the other hand, Retzius sparing has shown to be much more technically challenging for surgeons than conventional retropubic access [3, 4]. In this sense, RS-RARP has been gradually applied in salvage scenario, raising as a potential tool for reducing the high complications and incontinence rates in this setting.
This systematic review and meta-analysis study aimed to assess the impact of the novel Retzius-sparing robotic-assisted radical prostatectomy (RS-RARP) on continence outcomes in patients who underwent salvage surgery after failure of primary treatment, a scenario poorly explored in the literature.
Methods
Evidence acquisition
Study selection criteria for this review
The databases PubMed, Embase, Medline and Cochrane Central Register of Controlled Trials were used to conduct our literature search. The database was searched up until April 2023. The terms “Salvage prostatectomy”, “Post radiation” “Retzius-sparing”, “robot-assisted radical prostatectomy”, and “Retzius preservation” were used to find relevant studies. Two impartial reviewers conducted the literature search. The International Prospective Register of Systematic Reviews (PROSPERO) has registered the protocol for this study that includes the inclusion criteria (PROSPERO ID 425688). Inclusion criteria were salvage RS-RARP or RARP studies that examined perioperative and functional outcomes. Studies with no previous radiation therapy or lack of continence outcome were utilized as exclusion criteria.
Study design and outcomes
Prostate cancer patients were chosen for prospective nonrandomized or randomized RS-RARP or RARP studies that examined perioperative and functional outcomes, or at least overall continence at the end of the follow-up. Surgery approach conducted in each study (RS-RARP and/or S-RARP), patient characteristics (age, body mass index [BMI], preoperative prostate-specific antigen [PSA], preoperative Gleason score, and pathological stage) were accessed; primary outcome is postoperative urine continence. It was defined in all included trials as either using no pads or 0–2 pads.
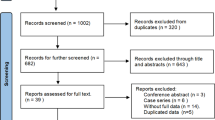
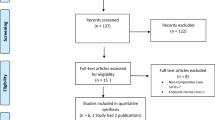
Assessment of study selection and validity
A data extraction form was created, relevant reports were collected, and two independent reviewers looked over the titles and abstracts of the pertinent literature (Fig. 1). The complete text was examined if the title and abstract were unclear. After carefully examining the chosen publications, a final judgment was made regarding the studies’ eligibility requirements. When two independent reviewers differed on the same document, consensus or contact with a third reviewer was required before the document could be included. According to the Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guideline, the current systematic review was carried out [5]. Retrospective studies were subjected to a domain-based risk of bias assessment in accordance with the Newcastle–Ottawa quality assessment scale cohort studies (NOS) [6]. Both the risk of bias and the caliber of the evidence were evaluated independently by two reviewers. From the included studies, study and participant characteristics were taken.
Data synthesis and statistical analysis
Descriptive statistics that used weighted averages and weighted standard deviations with individual cohort size as the weight were used to summarize patient characteristics and outcomes. The odds ratio (OR) was the effect measurements applied to dichotomous data. In the post hoc meta-analysis, available data and numbers were examined to determine standardized mean differences (SMDs), combined ORs, and 95% confidence intervals (CIs). The random-effect model of the studies’ variance and the heterogeneity parameter uses the inverse of the studies’ weight. In pooled analyses, the percentage of overall variation among studies’ heterogeneity was assessed using the P value and the I2 statistic [7, 8]. We conducted random-effect analysis to compare each parameter between RS-RARP and RARP. SMDs for continuous outcomes and ORs for dichotomous variables are used to represent the results. P < 0.05 suggested publication bias.
Surgical technique
The step-by-step modern Retzius-sparing robot-assisted radical prostatectomy technique consists of a 7 cm peritoneum opening at Douglas pouch; recto-prostatic space development; seminal vesicles and vas deferens isolation and section; extra-fascial dissection through peri-prostatic fat; neurovascular bundle control; bladder neck total preservation and opening; anterior dissection at Santorini plexus plane; apex dissection with urethra preservation and section; prostate release; vesicouretral modified Van Velthoven anastomosis; Rocco Stitch [9].
Results
The PRISMA flowchart (Fig. 1) describes the search technique shows the outcomes of the systematic literature review for the systematic review. Seventeen studies in total met the criteria for inclusion: 14 were retrospectives only and 3 described retrospective comparison cohorts (sRS-RARP vs sS-RARP) [10,11,12]. Table 1 and Fig. 1 provide more information on the study’s design, search method, data abstraction, and excluded studies (along with justifications).
Overall, it was determined that retrospective studies had a “fair” risk of bias (Table 2). Table 2 displays an overview of the cohort studies' risk of bias. Aiming to detect publication bias for urinary continence revealing asymmetry, NOS were recommended. It was determined that all the retrospective studies were of “fair” quality.
Overall continence
sRS-RARP may increase recovery of urinary continence after surgery compared to standard RARP [OR 4.36, 95% CI 1.7–11.17; I2 = 46.8%; studies = 4; participants = 87] (Fig. 2).
Nunes-Silva et al. have described the first Brazilian experience applying the RS-RARP approach in the post-radiation salvage scenario demonstrating continence rates of 25%, 75% and 91.6% at 1-, 3- and 12-month follow-ups, respectively [9]. Madi et al. reported significative better continence outcomes in sRS-RARP presenting immediate (25.0% vs 0.0%, P < 0.001), 3-month (80.0% vs 0%, P < 0.001), and 12-month continence rates (100% vs 44%, P = 0.0384) compared to S-RARP group. Median time to continence was also significantly shorter for the sRS-RARP patients (90.0 vs 270.0 days, P = 0.0095) [10].
Schuetz et al. reported immediate continence rates after catheter removal of 3 (14.3%) versus 0 (0%) in the sRS-RARP and S-RARP groups, respectively. At 12 months, overall continence rates were 4 (19%) versus 0 (0%); Incontinence grades 1, 2 and 3 were 7 (33%) versus 3 (43%), 3 (14%) versus 2 (29%), 4 (19%) versus 2 (29%) for sRS-RARP versus s-RARP, respectively, however, no statistical differences were observed between groups in this analysis [11]. On the other hand, Kowalczyk et al. reported continence criteria as 0–1 pads per day (PPD) and 0 PPD. Statistically significant differences in continence rates favored sRS-RARP, presenting Zero-PPD use rates of 54.1% vs. 6.3%, P < 0.001 and 0–1 PPD use rates of 78.4% vs. 43.8%, P = 0.003; overall continence rates were 29 (73%) vs 14 (44%) in the sRS-RARP and S-RARP, respectively [12].
At the time of the last follow-up, 286 patients (58.7%) in the pooled sample of S-RARP patients from the 17 studies examined in this analysis had excellent urine continence [9,10,11,12,13,14,15,16,17,18].
Discussion
Our meta-analysis data suggest that sRS-RARP approach has potential to provide significant higher chances for achieving continence compared to the S-RARP approach in the PCa salvage scenario.
Currently, minimally invasive radical prostatectomy performed by robotic platform is the gold standard technique for treating localized PCa minimizing the potential side effects of surgical treatment, especially regarding functional outcomes [13]. However, radical prostatectomy surgery has passed through a long evolution since Walsh et al. have described the technique details of the anatomical radical prostatectomy performed by open approach by that time [14, 15]. Over time, the laparoscopic and robotic developments overcome the open radical prostatectomy limitations and became the standard approach of care in the primary setting.
Since 2010, Galfano et al. then brought up the first technique description of the revolutionary Retzius-sparing surgery which has been applied exclusively by robotic approach and it has changed the current history of PCa surgical treatment. Theoretically, the advantages of Retzius-sparing approach over the standard retropubic anterior approach is the fact it promotes direct visualization of the rectum along dissection possibly minimizing risks of injury, as well as it allows total preservation of the key continence ligaments that sustains the bladder and urethra anteriorly. This novel RS-RARP approach has shown outstanding continence outcomes presenting immediate continence rates around 90% when applied in the primary setting [3, 4].
In parallel, this evolution ranging from open to conventional RARP and then to RS-RARP has also been gradually applied to the salvage setting overtime, although in a slower pace over last year’s due to the much higher challenging technical aspects involving this surgery in the salvage scenario. After local energy application for primary treatment, especially post-radiation energy application, peri-prostatic anatomy is corrupted due to tissues adhesions, inflammation, dense fibrosis, and scars. Therefore, the preservation of functional outcomes without compromising oncological results become the main challenging aspects during a salvage surgery. It demands a high level of expertise by surgeons due to the higher risk of morbidity and side effects such as high-grade incontinence and serious operative complications such as rectal injuries [1].
Traditionally, historical series of salvage open radical prostatectomy for radio-recurrent PCa reported incontinence rates ranging from 22 to 73%, rectal injury as high as 19–28% and overall complication rates of up to 67% [16]. Due to these disappointing results, only few patients used to be driven to local salvage treatment and the open approach was a domain in this scenario by that time. Inevitably, technology evolution towards robotic surgery made it to be applied in the salvage setting. Currently, recent series evaluating salvage RARP performed by the standard retropubic approach showed improvements in overall complications rates of 39–47% compared to the open approach, although continence rates have remained low 33–40% [17, 18].
In this context, Retzius-sparing RARP has raised as an inflexion point in the natural history of the salvage surgery along the decades demonstrating potential to change the curve of continence outcomes in these patients formerly condemned to a long-term risk of incontinence. sRS-RARP has shown improvements in continence recovery rates not only in the primary setting, but it also has shown outstanding results when applied in the salvage scenario.
Nunes-Silva et al. have described the first Brazilian experience applying the RS-RARP approach in the post-radiation salvage scenario demonstrating continence rates of 25%, 75% and 91.6% at 1-, 3- and 12-month follow-ups, respectively [18]. Madi et al. reported significative better continence outcomes in sRS-RARP presenting immediate (25.0% vs 0.0%, P < 0.001), 3-month (80.0% vs 0%, P < 0.001), and 12-month continence rates (100% vs 44%, P = 0.0384) compared to S-RARP group. Median time to continence was also significantly shorter for the sRS-RARP patients (90.0 vs 270.0 days, P = 0.0095) [10].
Schuetz et al. reported immediate continence rates after catheter removal of 3 (14.3%) versus 0 (0%) in the sRS-RARP and S-RARP groups, respectively. At 12 months, overall continence rates were 4 (19%) versus 0 (0%); incontinence grades 1, 2 and 3 were 7 (33%) versus 3 (43%), 3 (14%) versus 2 (29%), and 4 (19%) versus 2 (29%) for sRS-RARP versus s-RARP, respectively, however, no statistical differences were observed between groups in this analysis [11]. On the other hand, Kowalczyk et al. reported continence criteria as 0–1 pads per day (PPD) and 0 PPD. Statistically significant differences in continence rates favored sRS-RARP, presenting Zero-PPD use rates of 54.1% vs. 6.3%, P < 0.001 and 0–1 PPD use rates of 78.4% vs. 43.8%, P = 0.003; overall continence rates were 29 (73%) vs 14 (44%) in the sRS-RARP and S-RARP, respectively [12].
Our meta-analysis data have shown statistically significant increase in chances for achieving continence for patients in the sRS-RARP group [OR 4.36, 95% CI 1.7–11.17]. This represents an increment chance of 336% higher for achieving continence in patients underwent sRS-RARP. These findings corroborate most of current sRS-RARP literature signalizing an improvement in early return to continence in patients underwent salvation by this novel approach. However, the fact that the current literature available is only composed of retrospective studies, added to the fact that randomized controlled trials comparing both robotic approaches are not yet available, it leads us to alert that further studies are still needed to corroborate our findings.
In this sense, it suggests that the improved continence mechanisms previously seen in Retzius-sparing applied to the primary setting, may be possible translated to the salvage scenario after radiotherapy and other initial energy treatment modalities. It is possible to infer that the preservation of the Retzius anterior space and consequently its supporting ligaments to the bladder and anterior urethra maintaining sphincteric integrity may play a remarkable role in continence recovery when sRS-RARP approach is applied providing better immediate and long-term continence verified in the current available literature. In addition, although nerve-sparing has not been routinely performed in salvage setting due to risk of compromise on oncological outcomes, it is known that the Retzius space also shelter an expressive amount of prostatic nerve fibers that runs on the anterior aspect of the prostate surface. It is possible that the preservation of these anterior nerve fibers in sRS-RARP may also contribute somehow to improve continence outcomes.
Our review and meta-analysis corroborate the findings in current literature regarding the fact sRS-RARP has potential to provide a significant improvement on continence recovery rates. However, this study carries limitations regarding the fact of paucity amount of literature already published about sRS-RARP and the retrospective nature of these available literature. Further randomized controlled trials are still needed comparing both robotic approaches in this salvage scenario.
Conclusions
sRS-RARP approach has potential to improve continence outcomes in the salvage setting.
Data availability
Not applicable.
Abbreviations
- RS-RARP:
-
Retzius-sparing robotic-assisted radical prostatectomy
- sRS-RARP:
-
Salvage Retzius-sparing RARP
- PROSPERO:
-
International prospective register of systematic reviews
- NOS:
-
Newcastle–Ottawa quality assessment scale cohort studies
- PCa:
-
Prostate cancer
- BMI:
-
Body mass index
- PSA:
-
Prostate-specific antigen
- PRISMA:
-
Preferred reporting items for systematic reviews and meta-analyses
- OR:
-
Odds ratio
- SMD:
-
Standardized mean difference
- CI:
-
Confidence interval
References
Nunes-Silva I, Barret E, Srougi V, Baghdadi M, Capogrosso P, Garcia-Barreras S, Kanso S, Tourinho-Barbosa R, Carneiro A, Sanchez-Salas R, Rozet F, Galiano M, Cathelineau X (2017) Effect of prior focal therapy on perioperative, oncologic and functional outcomes of salvage robotic assisted radical prostatectomy. J Urol 198(5):1069–1076. https://doi.org/10.1016/j.juro.2017.05.071
Ficarra V, Novara G, Artibani W, Cestari A, Galfano A, Graefen M, Guazzoni G, Guillonneau B, Menon M, Montorsi F, Patel V, Rassweiler J, Van Poppel H (2009) Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol 55(5):1037–1063. https://doi.org/10.1016/j.eururo.2009.01.036
Galfano A, Di Trapani D, Sozzi F, Strada E, Petralia G, Bramerio M, Ascione A, Gambacorta M, Bocciardi AM (2013) Beyond the learning curve of the Retzius-sparing approach for robot-assisted laparoscopic radical prostatectomy: oncologic and functional results of the first 200 patients with ≥ 1 year of follow-up. Eur Urol 64(6):974–980. https://doi.org/10.1016/j.eururo.2013.06.046
Galfano A, Ascione A, Grimaldi S, Petralia G, Strada E, Bocciardi AM (2010) A new anatomic approach for robot-assisted laparoscopic prostatectomy: a feasibility study for completely intrafascial surgery. Eur Urol 58(3):457–461. https://doi.org/10.1016/j.eururo.2010.06.008
Knobloch K, Yoon U, Vogt PM (2011) Preferred reporting items for systematic reviews and meta-analyses (PRISMA) statement and publication bias. J Craniomaxillofac Surg 39(2):91–92. https://doi.org/10.1016/j.jcms.2010.11.001
Wells GA, Shea B, O’Connell D, Peterson J, Welch V, Losos M et al (2023) The Newcastle–Ottawa scale (NOS) for assessing the quality if nonrandomized studies in meta-analyses. Ottawa Hospital Research Institute. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp. Accessed 22 May 2023.
Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analyses. BMJ 327(7414):557–560. https://doi.org/10.1136/bmj.327.7414.557
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21(11):1539–1558. https://doi.org/10.1002/sim
Nunes-Silva I, Hidaka AK, Monti CR, Tobias-Machado M, Zampolli HC (2021) Salvage Retzius sparing robotic assisted radical prostatectomy: the first brazilian experience. Int Braz J Urol. 47(6):1279–1280. https://doi.org/10.1590/S1677-5538.IBJU.2021.0260
Madi R, Sayyid RK, Hiffa A, Thomas E, Terris MK, Klaassen Z (2021) Early experience with salvage retzius-sparing robotic-assisted radical prostatectomy: oncologic and functional outcomes. Urology 149:117–121. https://doi.org/10.1016/j.urology.2020.12.029
Schuetz V, Reimold P, Goertz M, Hofer L, Dieffenbacher S, Nyarangi-Dix J, Duensing S, Hohenfellner M, Hatiboglu G (2021) Evolution of salvage radical prostatectomy from open to robotic and further to retzius sparing surgery. J Clin Med 11(1):202. https://doi.org/10.3390/jcm11010202
Kowalczyk KJ, Madi RH, Eden CG, Sooriakumaran P, Fransis K, Raskin Y, Joniau S, Johnson S, Jacobsohn K, Galfano A, Bocciardi AM, Hwang J, Kim IY, Hu JC (2021) Comparative outcomes of salvage retzius-sparing versus standard robotic prostatectomy: an international, multi-surgeon series. J Urol 206(5):1184–1191. https://doi.org/10.1097/JU.0000000000001939
Coelho RF, Rocco B, Patel MB, Orvieto MA, Chauhan S, Ficarra V, Melegari S, Palmer KJ, Patel VR (2010) Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a critical review of outcomes reported by high-volume centers. J Endourol 24(12):2003–2015. https://doi.org/10.1089/end.2010.0295
Walsh PC (1998) Anatomic radical prostatectomy: evolution of the surgical technique. J Urol 160(6 Pt 2):2418–2424. https://doi.org/10.1097/00005392-199812020-00010
Walsh PC, Lepor H, Eggleston JC (1983) Radical prostatectomy with preservation of sexual function: anatomical and pathological considerations. Prostate 4(5):473–485. https://doi.org/10.1002/pros.2990040506
Mason JB, Hatch L, Dall C, Kowalczyk KJ (2022) Salvage Retzius-sparing radical prostatectomy: a review of complications, functional outcomes, and oncologic outcomes. Curr Oncol 29(12):9733–9743. https://doi.org/10.3390/curroncol29120764
Eandi JA, Link BA, Nelson RA, Josephson DY, Lau C, Kawachi MH, Wilson TG (2010) Robotic assisted laparoscopic salvage prostatectomy for radiation resistant prostate cancer. J Urol 183(1):133–137. https://doi.org/10.1016/j.juro.2009.08.134
Kaffenberger SD, Keegan KA, Bansal NK, Morgan TM, Tang DH, Barocas DA, Penson DF, Davis R, Clark PE, Chang SS, Cookson MS, Herrell SD, Smith JA Jr (2013) Salvage robotic-assisted laparoscopic radical prostatectomy: a single institution, 5-year experience. J Urol 189(2):507–513. https://doi.org/10.1016/j.juro.2012.09.057
Acknowledgements
We thank Prof. Marcos Tobias-Machado, Urology Division, Centro Universitário FMABC, Santo André, São Paulo, Brazil.
Author information
Authors and Affiliations
Contributions
IN-S: project development, data management, data analysis, manuscript writing/editing. AKH: project development, data management, data analysis, manuscript writing/editing. FPAG: project development, data management, data analysis, manuscript writing/editing. RMH: data management, manuscript writing/editing. SG: project development, data management, data analysis, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
All the authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Research involving human participants, their data or biological material
None. This is a systematic review and meta-analysis study. The International Prospective Register of Systematic Reviews (PROSPERO) has registered the protocol for this study that includes the inclusion criteria (PROSPERO ID 425688).
Informed consent
None. This is a systematic review and meta-analysis study. The International Prospective Register of Systematic Reviews (PROSPERO) has registered the protocol for this study that includes the inclusion criteria (PROSPERO ID 425688).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nunes-Silva, I., Hidaka, A.K., Glina, F.P.A. et al. Can salvage Retzius-sparing robotic-assisted radical prostatectomy improve continence outcomes? A systematic review and meta-analysis study. World J Urol 41, 2311–2317 (2023). https://doi.org/10.1007/s00345-023-04505-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-023-04505-w