Abstract
Purpose
To explore the usability and diagnostic accuracy for prostate cancer of three multiparametric magnetic resonance imaging (mpMRI)/transrectal ultrasound (TRUS)-guided fusion biopsy systems operated by the same urologists.
Methods
We performed a prospective, observational study including patients that underwent prostate biopsy due to a visible lesion in mpMRI (PI-RADS ≥ 3). We consecutively assessed two platforms with a rigid image registration (BioJet, D&K Technologies and UroNav, Invivo Corporation) and one with an elastic registration (Trinity, KOELIS). Four urologists evaluated each fusion system in terms of usability based on the System Usability Scale and diagnostic accuracy based on the detection of prostate cancer.
Results
We enrolled 60 consecutive patients that received mpMRI/TRUS-guided prostate biopsy with the BioJet (n = 20), UroNav (n = 20) or Trinity (n = 20) fusion system. Comparing the rigid with the elastic registration systems, the rigid registration systems were more user-friendly compared to the elastic registration systems (p = 0.012). Similarly, the prostate biopsy with the rigid registration systems had a shorter duration compared to the elastic registration system (p < 0.001). Overall, 40 cases of prostate cancer were detected. Of them, both the BioJet and UroNav fusion systems detected 13 prostate cancer cases, while the Trinity detected 14. No significant differences were demonstrated among the three fusion biopsy systems in terms of highest ISUP Grade Group (p > 0.99).
Conclusions
Rigid fusion biopsy systems are easier to use and provide shorter operative time compared to elastic systems, while both types of platforms display similar detection rates for prostate cancer. Still, further high-quality, long-term results are mandatory.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Prostate biopsy (PB) is considered the cornerstone of prostate cancer (PCa) diagnosis and it is listed among the most common urological interventions [1]. Even though PB was traditionally performed through a systematic transrectal ultrasound (TRUS)-guided approach [2], multiparametric magnetic resonance imaging (mpMRI) has recently altered the diagnostic algorithm of PCa, as it increases the detection rate of clinically significant PCa both in biopsy-naïve patients and in patients with prior negative PB [3, 4]. MpMRI-targeted PB may be performed either through a cognitive or an image-fusion approach [5]. Both techniques provide similar detection rates, although it seems that fusion-targeted PB may slightly improve the detection rate of clinically significant PCa in experienced hands [6, 7].
Multiple mpMRI/TRUS-guided fusion systems are currently approved for PB, with each system presenting its own advantages and disadvantages [8]. The commercially available platforms can fuse the mpMRI with the TRUS data through an elastic or a rigid registration [9]. Despite the indirect evidence supporting that there is no significant difference in the detection rate of PCa between both registration systems, to date, no study has directly compared elastic versus rigid registration systems regarding their usability and diagnostic accuracy for clinically significant and insignificant PCa [10]. The latter is predominantly attributed to the fact that urology departments performing mpMRI/TRUS-guided fusion PB opt for one biopsy system and, thus, direct comparisons of different biopsy systems in terms of user-friendliness and intra- or interobserver agreement were, so far, not possible.
Within this framework, we aimed to explore the usability and diagnostic accuracy of three different MRI/TRUS-guided fusion PB systems operated by the same urologists.
Materials and methods
Study design
We performed a prospective, observational study at the Department of Urology and Pediatric Urology, Julius-Maximilians-University of Würzburg, Würzburg, Germany and report its findings based on the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement for cohort studies [11]. All patients undergoing PB due to a visible lesion in mpMRI (PI-RADS ≥ 3) were considered eligible and were enrolled after providing written informed consent. On the contrary, we excluded patients undergoing PB without identified lesions in mpMRI, as well as patients on active surveillance due to prior PCa diagnosis.
We intended to obtain a new MRI/TRUS-targeted fusion biopsy system in our department. Therefore, we consecutively evaluated the BioJet (D&K Technologies GmbH, Barum, Germany), UroNav (Invivo Corporation, Gainesville, Florida, USA) and Trinity (KOELIS, Grenoble, France) fusion biopsy systems from April to August 2017. Both, the BioJet and UroNav platforms fuse the mpMRI with the TRUS data through a rigid registration, while the Trinity platform performs this fusion through a non-rigid (elastic) approach.
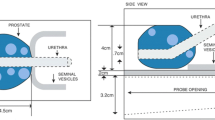
Four urologists with no prior experience on mpMRI/TRUS fusion PB assessed the usability, user-friendliness and diagnostic accuracy of each fusion system for the detection of PCa. In particular, two trainees, who had previously accomplished approximately 40 TRUS-guided biopsies, and two senior urologists, who had already accomplished more than 250 TRUS-guided biopsies, performed five consecutive mpMRI/TRUS-guided fusion PBs with each system. Overall, twenty biopsies were carried out with each fusion PB system. Apart from a trained nurse, during the procedure, all operators were alone in the operating room and performed the biopsy without any surveillance. The step-by-step study protocol is illustrated in Fig. 1.
After successfully performing the corresponding biopsies, all operators completed the System Usability Scale (SUS). The SUS is a 100-point scale consisting of ten questions that evaluate the learnability and user-friendliness of a given technology [12]. The SUS score for each technology is converted to a grading scale, with scores 90–100 ranking this technology as A-class, 80–89 as B, 70–79 as C, 60–69 as D and 0–59 as F [13].
Prostate biopsy procedure
All included patients underwent mpMRI at our institution with a 3 Tesla scanner using an external phased-array coil. The mpMRI protocol included T2-weighted imaging, diffusion-weighted imaging and, when indicated, a dynamic contrast-enhanced sequence based on the PI-RADS v2 [14]. All mpMRI-targeted biopsies were performed with the corresponding fusion PB system via a transrectal approach under local anesthesia. A specialized radiologist on prostate mpMRI identified and marked all targets intraoperatively. From each identified target, two or three cores were taken based on the size of the lesion. Subsequently, all patients underwent systematic 12-core PB. All cores were evaluated by specialized uropathologists and were classified according to the International Society of Urological Pathology (ISUP) Grade Group [15]. After undergoing PB, all patients were hospitalized and were evaluated clinically for any postoperative complications. The following day, post-void residual was determined, and all patients were discharged.
Outcomes
The primary outcome of our study was the usability based on the SUS and the operative time between elastic and rigid registration platforms. Secondary outcomes included: (i) the usability based on the SUS and the operative time of each mpMRI/TRUS-guided fusion system; (ii) the detection rate of clinically significant and insignificant PCa between elastic and rigid registration platforms; (iii) the overall detection rate of clinically significant and insignificant PCa of each fusion system combined with the systematic 12-core PB; (iv) the perioperative and postoperative safety of each mpMRI/TRUS-guided fusion system.
Statistical analysis
We summarized all baseline characteristics with descriptive statistics in the form of median with interquartile range (IQR) or frequencies with proportions. For continuous variables, we applied the Mann–Whitney test to compare between elastic and rigid platforms and the Kruskal–Wallis test to compare among the three fusion systems. For the latter, Dunn’s pairwise comparisons were performed using the method of Bonferroni to calculate adjusted p values. On the contrary, for categorical variables, we applied the Fisher’s exact test. All analyses were undertaken using the R statistical software (version 3.6.3) and two-sided p values lower than 0.05 were considered statistically significant.
Results
Baseline characteristics
We enrolled 60 consecutive patients with a median age of 64 (IQR: 61–70) years that received mpMRI/TRUS-guided PB with the BioJet (n = 20), UroNav (n = 20) or Trinity (n = 20) fusion system. Overall, 16 (27%) patients had a highest PI-RADS score of 3, 28 (46%) of PI-RADS 4 and 16 (27%) of PI-RADS 5. No statistically significant differences were detected in the baseline characteristics among the three groups. The baseline characteristics of all included patients are depicted in Table 1.
System usability scale
The four urologists evaluated the user-friendliness of the three fusion systems after performing the corresponding biopsies. The UroNav presented user-friendliness of class C (median 72.5, IQR 63.8, 80.6), the BioJet of class D (median 65, IQR 63.8, 68.1) and the Trinity of class F (median 38.8, IQR 37.5, 45). Based on the SUS score, the rigid registration systems (BioJet and UroNav) were more user-friendly compared to the elastic registration platform (Trinity), p = 0.012. Similarly, when comparing among the three systems, a statistically significant difference was also demonstrated, p = 0.031. Of note, compared to the junior urologists, the two senior urologists rated all fusion systems with a higher user-friendliness score based on the SUS scale.
Moreover, the operative time was significantly shorter with the rigid registration systems compared to the elastic registration system, p < 0.001. Interestingly, the two senior urologists performed faster the biopsies with all fusion systems compared to the junior urologists. The comparisons between rigid and elastic registration systems are presented in Table 2, while the comparisons among the three fusion biopsy platforms can be seen in Table 3.
Detection rate and safety
Overall, 40 cases of PCa were detected. Of them, both the BioJet and UroNav fusion systems detected 13 PCa cases, while the Trinity detected 14. Eight patients presented with clinically insignificant and 32 with clinically significant PCa. No significant differences were demonstrated between rigid (BioJet and UroNav) and elastic (Trinity) registration systems in terms of highest ISUP Grade Group, p = 0.98. Similarly, when comparing among the three fusion biopsy systems, no statistically significant differences were detected, p > 0.99. All relevant measures and comparisons are available in Tables 2 and 3.
During the course of the study, no severe perioperative and postoperative adverse events were observed. In particular, no cases of excessive bleeding were reported, and no urinary catheter was placed after PB. Accordingly, none of the included participants developed postoperative fever or acute urinary retention. Overall, only transient hematospermia, hematuria or hematochezia were reported among most participants.
Discussion
Our findings demonstrate that rigid registration platforms may be easier to use compared to elastic registration platforms among urologists with no prior experience with a mpMRI/TRUS-guided fusion biopsy system. In an attempt to classify the evaluated biopsy systems, UroNav was graded with the highest score followed by BioJet and Trinity. Of note, the operative time was significantly shorted with the rigid registration platforms compared to the elastic platforms. Still, it should be highlighted that all three evaluated MRI/TRUS-guided fusion biopsy systems presented similar detection rates for both clinically significant and insignificant PCa diagnosis. Importantly, the senior urologists performed faster the biopsies with all fusion systems and attributed to all fusion systems higher SUS scores compared to the junior urologists. Hence, no definite conclusions on the long-term use of each individual fusion biopsy system can be drawn from the evaluation of only five early applications per investigator.
The predominant difference between the three included fusion systems is the type of image registration [16,17,18]. Rigid fusion systems combine the mpMRI and TRUS images before PB and do not adjust for potential deformations of the prostate gland during the procedure, such as patient movement or pressure of the gland with the probe [19]. On the other hand, elastic fusion systems compensate for such deformations by scanning the prostate gland before the acquisition of each core [19]. However, this scanning increases the operative time and, based on our analysis, negatively affects the usability of the system.
It should be highlighted that our findings are in line with both experimental and clinical studies comparing the two image registration techniques. Even though initial experimental studies have tended to slightly favor elastic registration systems, novel ex vivo data demonstrate that rigid and elastic registration display similar results [20, 21]. In particular, based on a high-quality, multi-operator phantom study, the authors concluded that elastic and rigid registration display similar registration errors and that elastic registration does not improve the diagnostic accuracy of the PB [19].
To date, only one clinical study has compared the two image registration techniques for the detection of PCa. More specifically, Delongchamps et al. included, in a single cohort study, 131 patients that underwent rigid mpMRI/TRUS image registration and 133 that underwent elastic registration. The rigid mpMRI-targeted fusion PB detected 46 of the 60 total PCa cases, whereas the elastic mpMRI-targeted fusion PB detected 35 of the 44 total cases. All undetected cases in both groups by systematic PB were histologically classified as clinically insignificant PCa. Overall, no significant differences were observed between the rigid and the elastic mpMRI-targeted fusion PB for the detection of clinically significant PCa [22].
Similarly, a meta-analysis indirectly compared rigid and elastic image registration for the detection of clinically significant and any PCa, demonstrating that the two registration techniques display similar detection rates. In particular, the authors compared rigid mpMRI-targeted fusion PB versus systematic PB and elastic mpMRI-targeted fusion PB versus systematic PB. The detection rate of clinically significant PCa of rigid mpMRI-targeted fusion PB versus systematic PB was 1.40 (95% CI 1.13–1.75, p = 0.002), while the detection rate of elastic mpMRI-targeted fusion PB versus systematic PB was 1.45 (95% CI 1.21–1.73, p < 0.0001). Therefore, the authors indirectly concluded, based on the similar detection rates of the two fusion techniques versus systematic PB (p = 0.83), that rigid and elastic image registration techniques display similar diagnostic accuracy for PCa [10]. Still, this comparison should have been preferably addressed in the form of a network meta-analysis.
Accumulating evidence indicates that the mpMRI/TRUS-guided fusion PB may not be superior to a cognitive fusion in terms of PCa diagnosis [23, 24] Given that the cognitive approach does not require any additional training from the operator, the relatively low grade of user-friendliness of all evaluated fusion biopsy platforms demonstrated by our study may discourage some clinicians from preferring these platforms compared to the cognitive approach. Another limitation of the mpMRI-targeted PB is that it requires high level of expertise and training for accurate interpretation of the prostate mpMRI findings [25]. Even specialized radiologists and experienced urologists on prostate mpMRI display limited inter-reader and intraoperator reproducibility [26]. Therefore, the interest has turned to novel diagnostic modalities [27]. Recently, micro-US-guided PB emerged as a promising alternative to mpMRI-targeted PB, as it seems more user-friendly than mpMRI-targeted PB and, interestingly, provides similar detection rates to mpMRI-targeted PB [28].
Strengths and limitations
It should be highlighted that the available literature is inconclusive about the superiority of one image registration technique over the other. In this scope, we provide, to our knowledge, the first study that aims to compare three different mpMRI/TRUS-guided fusion biopsy systems regarding usability and significant or insignificant PCa detection. Our findings suggest that both rigid and elastic image registration techniques display similar detection rates for PCa diagnosis. Additionally, by demonstrating that the PB with an elastic image registration platform is time-consuming and may be inconvenient for the operator, we pointed out another potential limitation of elastic image registration platforms compared to rigid platforms.
Nevertheless, our study presents some limitations, relevant to its non-randomized and single-center design, as well as to its relatively small sample size in terms of participating urologists and patients. Given that we consecutively assessed three fusion biopsy systems and that we evaluated the usability and diagnostic accuracy of each system for approximately 1 month, the absence of randomization could not be avoided. It should be also highlighted that, at baseline, all investigators had no prior experience with fusion PB. However, by the third device, each of the investigators had prior experience of ten fusion biopsies, which may have affected operative time and comfort assessment of the devices. As a surrogate, in an attempt to provide comparable outcomes, the number of biopsies, the involved operators and the biopsy protocol remained identical for all biopsy systems. Similarly, due to the short duration of our study, the small size of participants and operators may limit the generalizability of our findings. Thus, our study may be underpowered in detecting any differences among the included mpMRI/TRUS-guided fusion biopsy systems, if they exist. Based on the previous notion, we did not evaluate the positivity rate of each fusion system concerning only the targeted biopsy cores. Moreover, considering the established role of mpMRI in PCa diagnosis, it was beyond the scope of the present study to compare mpMRI/TRUS-guided PB with the systematic PB.
Future perspectives
It should be stressed that, although mpMRI is an integral part of PCa diagnostic algorithm, given the scarcity of available data regarding the detection rate of clinically significant and insignificant PCa between rigid and elastic fusion biopsy systems, further well-designed, large-scale studies are needed to elucidate this field of research. Ideally, randomized or multicenter trials with both experienced and novice operators are necessary to validate and strengthen the robustness of our findings. Similarly, because of the sequential test orders of the fusion devices, a randomization was not methodologically feasible. In an ideal future study, each of the investigators should start with a different device so that the usability and diagnostic accuracy of each fusion system may be adequately tested. Accordingly, fusion mpMRI may increase costs for every health care system and, therefore, future comparative studies should aim to explore whether the fusion approach is superior to the cognitive approach in terms of PCa diagnosis. It should be also noted that studies comparing the detection rates of mpMRI-targeted PB with other novel diagnostic modalities such as micro-US-guided PB are expected with great interest.
Conclusion
Our results indicate that rigid fusion biopsy systems are easier to use and provide shorter operative time compared to elastic systems. Prior experience with TRUS-guided transrectal prostate biopsy seems to positively affect usability and operating time of the mpMRI/TRUS-guided fusion PB systems. Through direct comparisons, we demonstrated that elastic and rigid image registration platforms display similar detection rates for clinically significant and insignificant PCa. Still, the non-randomized design and the small sample size of our study limits its external validity and, therefore, further high-quality, long-term trials are warranted to corroborate our findings.
Availability of data and material
The raw data of the study are available after request from the authors.
References
Borghesi M, Ahmed H, Nam R et al (2017) Complications after systematic, random, and image-guided prostate biopsy. Eur Urol 71:353–365. https://doi.org/10.1016/j.eururo.2016.08.004
Shoag JE, Nyame YA, Gulati R et al (2020) Reconsidering the trade-offs of prostate cancer screening. N Engl J Med 382:2465–2468. https://doi.org/10.1056/NEJMsb2000250
Kasivisvanathan V, Stabile A, Neves JB et al (2019) Magnetic resonance imaging-targeted biopsy versus systematic biopsy in the detection of prostate cancer: a systematic review and meta-analysis. Eur Urol 76:284–303. https://doi.org/10.1016/j.eururo.2019.04.043
Drost F-JH, Osses DF, Nieboer D et al (2019) Prostate MRI, with or without MRI-targeted biopsy, and systematic biopsy for detecting prostate cancer. Cochrane Database Syst Rev 4:CD012663. https://doi.org/10.1002/14651858.CD012663.pub2
Gayet M, van der Aa A, Beerlage HP et al (2016) The value of magnetic resonance imaging and ultrasonography (MRI/US)-fusion biopsy platforms in prostate cancer detection: a systematic review. BJU Int 117:392–400. https://doi.org/10.1111/bju.13247
Watts KL, Frechette L, Muller B et al (2020) Systematic review and meta-analysis comparing cognitive vs. image-guided fusion prostate biopsy for the detection of prostate cancer. Urol Oncol 38:734.e19-734.e25. https://doi.org/10.1016/j.urolonc.2020.03.020
Khoo CC, Eldred-Evans D, Peters M et al (2020) A comparison of prostate cancer detection between visual-estimation (cognitive registration) and image-fusion (software registration) targeted transperineal prostate biopsy. J Urol. https://doi.org/10.1097/JU.0000000000001476
Franz T, von Hardenberg J, Blana A et al (2017) MRT/TRUS-fusionierte biopsiesysteme. Urol 56:208–216. https://doi.org/10.1007/s00120-016-0268-1
Mozer P, Rouprêt M, Le Cossec C et al (2015) First round of targeted biopsies using magnetic resonance imaging/ultrasonography fusion compared with conventional transrectal ultrasonography-guided biopsies for the diagnosis of localised prostate cancer. BJU Int 115:50–57. https://doi.org/10.1111/bju.12690
Venderink W, de Rooij M, Sedelaar JPM et al (2018) Elastic versus rigid image registration in magnetic resonance imaging-transrectal ultrasound fusion prostate biopsy: a systematic review and meta-analysis. Eur Urol Focus 4:219–227. https://doi.org/10.1016/j.euf.2016.07.003
von Elm E, Altman DG, Egger M et al (2007) The Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet Lond Engl 370:1453–1457. https://doi.org/10.1016/S0140-6736(07)61602-X
Brooke J (1996) SUS: a ‘quick and dirty’ usability scale. In: Jordan P, Thomas B, Weerdmeester B, McClelland I (eds) Usability evaluation in industry. Taylor & Francis Ltd, London, p 189–194
Brooke J (2013) SUS: a retrospective. J Usability Stud 8:29–40
Weinreb JC, Barentsz JO, Choyke PL et al (2016) PI-RADS prostate imaging—reporting and data system: 2015, version 2. Eur Urol 69:16–40. https://doi.org/10.1016/j.eururo.2015.08.052
Epstein JI, Egevad L, Amin MB et al (2016) The 2014 international society of urological pathology (ISUP) consensus conference on gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40:244–252. https://doi.org/10.1097/PAS.0000000000000530
Dickinson L, Hu Y, Ahmed HU et al (2013) Image-directed, tissue-preserving focal therapy of prostate cancer: a feasibility study of a novel deformable magnetic resonance-ultrasound (MR-US) registration system. BJU Int 112:594–601. https://doi.org/10.1111/bju.12223
Ukimura O, Desai MM, Palmer S et al (2012) 3-Dimensional elastic registration system of prostate biopsy location by real-time 3-dimensional transrectal ultrasound guidance with magnetic resonance/transrectal ultrasound image fusion. J Urol 187:1080–1086. https://doi.org/10.1016/j.juro.2011.10.124
Borkowetz A, Platzek I, Toma M et al (2015) Comparison of systematic transrectal biopsy to transperineal magnetic resonance imaging/ultrasound-fusion biopsy for the diagnosis of prostate cancer. BJU Int 116:873–879. https://doi.org/10.1111/bju.13023
Hale GR, Czarniecki M, Cheng A et al (2018) Comparison of elastic and rigid registration during magnetic resonance imaging/ultrasound fusion-guided prostate biopsy: a multi-operator phantom study. J Urol 200:1114–1121. https://doi.org/10.1016/j.juro.2018.06.028
Westhoff N, Siegel FP, Hausmann D et al (2017) Precision of MRI/ultrasound-fusion biopsy in prostate cancer diagnosis: an ex vivo comparison of alternative biopsy techniques on prostate phantoms. World J Urol 35:1015–1022. https://doi.org/10.1007/s00345-016-1967-3
Costa DN, Pedrosa I, Donato F et al (2015) MR imaging-transrectal US fusion for targeted prostate biopsies: implications for diagnosis and clinical management. Radiogr Rev Publ Radiol Soc N Am Inc 35:696–708. https://doi.org/10.1148/rg.2015140058
Delongchamps NB, Peyromaure M, Schull A et al (2013) Prebiopsy magnetic resonance imaging and prostate cancer detection: comparison of random and targeted biopsies. J Urol 189:493–499. https://doi.org/10.1016/j.juro.2012.08.195
Hamid S, Donaldson IA, Hu Y et al (2019) The SmartTarget biopsy trial: a prospective, within-person randomised, blinded trial comparing the accuracy of visual-registration and magnetic resonance imaging/ultrasound image-fusion targeted biopsies for prostate cancer risk stratification. Eur Urol 75:733–740. https://doi.org/10.1016/j.eururo.2018.08.007
Simmons LAM, Kanthabalan A, Arya M et al (2018) Accuracy of transperineal targeted prostate biopsies, visual estimation and image fusion in men needing repeat biopsy in the PICTURE trial. J Urol 200:1227–1234. https://doi.org/10.1016/j.juro.2018.07.001
Moldovan PC, Van den Broeck T, Sylvester R et al (2017) what is the negative predictive value of multiparametric magnetic resonance imaging in excluding prostate cancer at biopsy? A systematic review and meta-analysis from the european association of urology prostate cancer guidelines panel. Eur Urol 72:250–266. https://doi.org/10.1016/j.eururo.2017.02.026
Muller BG, Shih JH, Sankineni S et al (2015) Prostate cancer: interobserver agreement and accuracy with the revised prostate imaging reporting and data system at multiparametric MR imaging. Radiology 277:741–750. https://doi.org/10.1148/radiol.2015142818
Laurence Klotz CM (2020) Can high resolution micro-ultrasound replace MRI in the diagnosis of prostate cancer? Eur Urol Focus 6:419–423. https://doi.org/10.1016/j.euf.2019.11.006
Sountoulides P, Pyrgidis N, Polyzos SA et al (2021) Micro-ultrasound-guided versus multiparametric magnetic resonance imaging-targeted biopsy in the detection of prostate cancer: a systematic review and meta-analysis. J Urol. https://doi.org/10.1097/JU.0000000000001639
Funding
No funding was received for conducting this study.
Author information
Authors and Affiliations
Contributions
IS: Protocol/project development, data collection or management, data analysis, manuscript writing/editing. NP: Data analysis, manuscript writing/editing. LK: Data collection or management, manuscript editing. MK: Data collection or management, Manuscript editing. AT: Data collection or management, data analysis. HK: Protocol/project development, manuscript editing. GH: Protocol/project development, manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This is an observational study and no ethical approval was required.
Consent to participate and for publication
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Sokolakis, I., Pyrgidis, N., Koneval, L. et al. Usability and diagnostic accuracy of different MRI/ultrasound-guided fusion biopsy systems for the detection of clinically significant and insignificant prostate cancer: a prospective cohort study. World J Urol 39, 4101–4108 (2021). https://doi.org/10.1007/s00345-021-03761-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-021-03761-y