Purpose
Abstract
To determine if treatment of non-obstructing urolithiasis is effective in management of recurrent UTI.
Materials and methods
A retrospective review was performed of patients undergoing elective management of non-struvite upper tract urinary calculi with recurrent UTI from 2009 to 2016. Recurrent UTI was defined at ≥ 3 UTI in 12 months, with symptoms and documented urine culture. Preoperative CT was performed in all patients to determine stone burden. All patients had postoperative imaging and ≥ 12 months of follow-up. Pre- and postoperative variables were between patients who had recurrent UTI after treatment versus those who did not.
Results
46 patients met inclusion criteria. 42 (91.3%) were female. Median age was 63.7 years (IQR 49.1, 73.4) and median total stone burden was 20 mm (IQR 14–35). Within the cohort, 20 (43.5%) underwent ureteroscopy only, 26 (56.5%) underwent PCNL ± URS, and none underwent ESWL. Median postoperative follow-up was 2.9 years (IQR 2.0, 4.3). Only five patients (10.9%) had recurrent UTI after treatment. 80% were with the preoperative pathogen. The presence of residual stone was an independent risk factor for recurrent UTI after treatment (p < 0.046). Diabetes, hypertension, immunosuppression and chronic kidney disease were not.
Conclusions
Stone removal for patients with recurrent UTIs was associated with a high rate of success (89.1%) in elimination of further recurrent UTIs. Residual fragments are independently associated with persistent recurrent UTIs and thus, complete stone removal is of paramount importance in treatment of this patient population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Urinary tract infections (UTI) are common conditions that are found in both men and women, with women having a higher incidence of UTIs. Nearly a third of all women report a UTI prior to 24 years of age [1]. Individuals that develop a UTI are more likely to develop subsequent UTIs and the risk of recurrence increases as the number of prior infections increase [2]. Not only is there significant morbidity in UTIs to the patient but a significant economic burden exists as well, with the cost of UTIs estimated to be $3.5 billion dollars in 2000 in total medical expenditures in the United States ($1.03 billion for men and $2.47 billion for women) [3, 4].
The role of kidney stones in the pathogenesis or resolution of UTIs is not clear. Kidney stones affect many people and up to 10% of all individuals will have a kidney stone in their lifetime [5]. It is known that infectious stones can harbor bacteria inside, making these specific bacteria resistant to antimicrobial therapy [6]. More recently, calcium stones have also been demonstrated to harbor bacteria in the same manner, making eradication of infection difficult, leading to recurrent UTI [5]. The benefit of having non-obstructing metabolic stones removed, in the setting of UTIs, is unknown.
Therefore the objective of this study is to determine if non-obstructing, non-infectious stone removal via ureteroscopy (URS) or percutaneous nephrolithotomy (PCNL) in patients with recurrent UTI decreases the incidence of future urinary tract infections.
Materials and methods
After Institutional Review Board approval, a retrospective review of patients with recurrent UTI and who underwent a procedure at Mayo Clinic (Rochester, MN) for non-obstructive urolithiasis from 2009 through 2016 was performed. Recurrent UTI were confirmed with a documented history and at least one preoperative culture confirmed through chart review. Preoperatively, UTIs in our study were considered if there was documentation of symptoms and a positive culture. Preoperative CT scans were performed to confirm stone size, location and non-obstructing nature. Patients either had negative preoperative cultures, or were treated with a multiday course of preoperative antibiotics before stone extraction. Patients undergoing PCNL all received 7 days of preoperative anti-biotics even with a negative culture with one of the following regimens based on allergies and renal function: nitrofurantoin 100 mg BID, trimethoprim–sulfamethoxazole 800/160 mg BID, ciprofloxacin 500 mg BID. URS was performed with an access sheath, pressurized irrigant and lithotripsy with basket retrieval of fragments larger than the 1.9 Fr basket. Postoperative recurrent UTI were all confirmed with urine cultures. Patients were excluded who did not have culture documented UTI and/or who did not have at least 12 months of follow-up. Patients with infection based stones (struvite and carbonate) were also excluded.
Patient demographics and comorbidities were obtained at baseline. Recurrent UTIs were defined as greater than equal to 3 infections in 12 months. The stone size, location, and preoperative organism were noted. Type of operation (URS and/or PCNL), stone type and stone cultures (when available) were also noted. Postoperative stone free rates were determined with either US and KUB or non-contrast CT, defined as no residual radiopaque renal or ureteral calculi. Postoperative UTI was determined by positive urine culture with or without symptoms. Those within 30 days of surgical intervention were considered secondary to instrumentation and not considered as contributing to recurrent UTI.
Those with recurrent UTI postoperatively were compared to those without. Fisher’s exact test was used to compare categorical variables and Wilcoxon rank sum was used for continuous variables. JMP (SAS Institute, Minneapolis, MN) was used for statistical analysis.
Results
A total of 46 patients were included in the cohort. Preoperative patient demographics, comorbidities, class of UTI pathogens, and stone characteristics are listed in Table 1. Escherichia coli, Enterococcus species and Klebsiella pneumoniae were common causative organisms in 17 (37%), 8 (17%) and 6 (13%) of patients. Only one patient was non-Caucasian in our cohort. The patients were primary older, Caucasian females. 17% of patients were on prophylactic antibiotics preoperatively. Most preoperative infections were with gram negative rods. On preoperative imaging, median total stone burden of 20 mm (IQR 14–35) with a range of 5–100 mm. Fourteen patients had total stone burden less than 15 mm.
Of the procedures performed, 43% of patients underwent ureteroscopy only and 57% had PCNL ± URS. Median preoperative stone burden of those undergoing URS was 14 mm (IQR 11–20) and those undergoing PCNL was 26 mm (IQR 20–40). Stone cultures were obtained in 76% of patients at primary procedure, and 54% were positive. The most common organisms on stone culture were Enterococcus sp. (32%), Pseudomonas aeruginosa (16%), Escherichia coli (11%) and Klebsiella pneumoniae (11%). However, only 67% of positive stone cultures were concordant with preoperative UTI pathogens. There were three complications (two Clavien grade 2 and one Clavien 4b). This included two cases of SIRS/sepsis leading to one unplanned readmission. After surgery, 22% required a second stage stone operation due to residual stone.
The stone free rate after last treatment was 64% at the time of first postoperative imaging studies. Stone free was defined as the absence of any radiopaque calculi at the time of postoperative imaging. Imaging modalities for postoperative follow-up were 46% non-contrast CT, 41% KUB and renal US, 11% KUB only, 2% renal US only. Postoperative imaging was obtained on postoperative day 1 in 31% of patients (who all underwent PCNL), and 69% underwent imaging at a median of 64 days postoperatively (IQR 44–105). The stone free rate for ureteroscopy only was 63% compared to 65% for PCNL with or without ureteroscopy.
Median residual fragment size was 3 mm (IQR 2–6), and there were no findings of nephrocalcinosis or medullary sponge kidney that contributed to residual fragment. Median time of most recent follow-up is 2.9 years (IQR 2.0–4.3). Patients were placed on postoperative antibiotics for a median time of 1 week (range 0–12). Of patients that were on prophylaxis prior to surgery, 68% of patients were able to discontinue postoperatively and no patients were started on long-term prophylaxis after surgery. 52% had a single UTI > 30 days after the stone procedure at a median time of 12.3 months (IQR 5.2–27.8), and no factors were significantly different between those with and without sporadic UTIs. 89% of the cohort was free of recurrent UTIs postoperatively. In the group of five patients with recurrent UTIs, four occurred within 12 months and one occurred > 12 months. Four of the five had recurrent UTIs with the same pathogen identified preoperatively. On average, patients experienced on average 3.1 UTIs in the year prior to surgical intervention and only 0.5 UTI in the following year, with a statistically significant difference on paired t test analysis of p < 0.001.
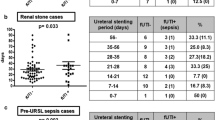
Differences between those with postoperative recurrent UTI compared to those who did not are listed on Table 2. Presence of residual stone was the only statistically significant factor in recurrent UTI after stone procedure (p = 0.046), but size of residual stone was not. Preoperative patient risk factors such as diabetes mellitus, hypertension, preoperative creatinine, BMI, and age were not associated with postoperative recurrent UTI. There was no significant association with stone composition. The type of procedure and positive stone culture were also not associated with postoperative recurrent UTI.
Discussion
In our cohort, 89% of patients with recurrent UTIs and a non-obstructive, non-infectious renal stone were cured after stone extraction. There was no difference in cure rates with regards to age, BMI, diabetes mellitus, hypertension or immunosuppression. Additionally, there was no difference in stone size or method of extraction between URS and PCNL. Patients typically received at least 1 week of antibiotics pre- and postoperatively based on preoperative urine culture. Postoperative SIRS/sepsis rate was 4%. Just under half of patients did not have a documented UTI after stone extraction, and there was a statistically significant difference in the number of UTIs in the year before and after stone intervention (p < 0.001). A sporadic UTI should not be considered a treatment failure. Notably, only residual stone was demonstrated as a risk factor for postoperative recurrent UTI.
The burden of UTI to the patient is quite high and very common, with a lifetime incidence in females exceeding 50% [1, 3, 4]. There is evidence associating urologic stones and UTI. Comorbidities likely also have a role in UTI pathogenesis with patients diagnosed with CKD having higher rates of UTI with stones present [7]. In addition, those with inflammatory bowel disease (IBD) and a stone have higher rates of UTI compared to the general population, suggesting an increased role in early interventions for stone extraction [8].
There has been minimal investigation into the role of non-obstructing, non-infectious stones in recurrent UTIs. However, a recent study also investigated the role of treating stones in the setting of recurrent UTI [10]. This was a retrospective review of 120 patients at a tertiary care facility and included patients with recurrent UTI undergoing ESWL, URS and PCNL. The rates of postoperative recurrent UTI clearance were notably different in this study than the prior (89 vs 48%). Of note, the prior study did not note how they confirmed preoperative recurrent UTI in the patient population. Our findings were similar in not finding associations with age, gender, diabetes mellitus, or immunosuppression. Additionally, stone factors of size, burden and composition were not significant in either analysis. We did not find hypertension as a significant factor associated with recurrent UTI. Importantly, our cohort differed as no patients in our cohort underwent ESWL due to the significant stone burden within the cohort (median stone size of 1.4 cm) and low stone free rates with ESWL in patients with stone burdens > 1 cm [11, 12]. A notable difference in between studies is the inclusion of patients with residual stone fragments in the statistical analysis and their role in postoperative recurrent UTI.
One hypothesis is that bacteria are harbored in the stone itself. There have been multiple studies done demonstrating the ability for bacteria to grow and interact in a calculus despite appropriate antibiotic therapy [5, 6]. However, recent studies have shown significant rates of negative stone cultures, as well as discordant rates corresponding urine and stone cultures. A rate of 22% positive stone culture in patients with non-struvite stones has been reported [13]. A large single center review of 776 PCNL stone cultures demonstrated a 38.7% rate of positive stone cultures with a 45.8% discordance of those cultures [14]. This is in comparison to our cohort with a 54% positive stone culture rate and 67% concordance. The higher rate of stone culture positivity can be explained due to a selected cohort with history of recurrent UTI.
It remains unclear of the role regarding positive stone cultures and their role in pathogenesis of recurrent UTI due to the high discordance rate. Regardless of the pathogenesis of recurrent UTIs with stone disease, there appears to be a role in stone extraction with a high rate of success in our cohort. Further supporting the hypothesis, we demonstrated a significant difference in postoperative recurrent UTI in those with residual stone. In a recent study of stone removal and recurrent UTI, patients undergoing ESWL were also included in the analysis and had a higher rate of recurrent UTI after procedure (37 vs 28%) [10]. Although those with recurrent stone were excluded, there may have been residual dust collections harboring stone in this non-extraction procedure.
Patients in our cohort only proceeded to surgery after a negative culture or receiving a course of culture specific antibiotics before stone removal. PCNL patients typically receive antibiotics for at least 1 week pre- and postoperatively. Although patients with recurrent UTI receive multiple courses of antibiotics, the effect of antibiotics given at the time of stone removal cannot be ignored in its role of eradication of UTI. The antibiotic courses were relatively brief and well within the typical course of antibiotics this patient population receives on a regular basis [9]. It is the combination of antibiotics and stone removal that contributes to the high rate of cure.
There are limitations to our analysis. This was a retrospective analysis and subject to sampling bias due to criteria and requirements for UTI documentation and reporting bias due to some patient records not being available to us. Our population was mainly Caucasian as a result of the demographics of our patient population. Patients did receive counseling post-procedurally for stone prevention, including hydration, which may have led to reduction in UTI. However, none were diagnosed with or receive specific treatments for other potential causes of recurrent UTI, including vaginal atrophy or constipation (besides periprocedural constipation). We did not identify newly diagnosed patients with vaginal atrophy or constipation in our cohort, however we only captured care in our health system. Also, our patients in general had larger stones with median size > 1 cm. Not all patients had same imaging follow-up (CT, KUB and/or US) or time to follow-up, which may impact the true stone free rate. Due to the high rate of cure, our group of patients with postoperative recurrent UTI was small. This was a single center study, however a single surgeon performed all ureteroscopies and PCNL in similar fashion. There was not a control group to compare continued conservative, symptomatic based treatment of recurrent UTI, however given the stone parameters in the patient population a matched control group of observation would be difficult given stone sizes. We did attempt to control for this by comparing number preoperative versus postoperative UTIs in paired fashion as a surrogate for a control group, which demonstrated significant UTI reduction postoperatively.
Conclusion
Stone extraction is associated with significant reduction in postoperative recurrent UTI. A single UTI is common in the immediate post-operative period and is not indicative of treatment failure. Residual stone will predispose patients to continued recurrent UTI postprocedurally and complete stone clearance should be pursued.
References
Foxman B, Barlow R, D’Arcy H, Gillespie B, Sobel JD (2000) Urinary tract infection: self-reported incidence and associated costs. Ann Epidemiol 10:509–515
Mabeck CE (1972) Treatment of uncomplicated urinary tract infection in non-pregnant women. Postgrad Med J 48:69–75
Griebling TL (2005) Urologic diseases in America project: trends in resource use for urinary tract infections in women. J Urol 173:1281–1287
Griebling TL (2005) Urologic diseases in America project: trends in resource use for urinary tract infections in men. J Urol 173:1288–1294
Barr-Beare E, Saxena V, Hilt EE et al (2015) The Interaction between Enterobacteriaceae and calcium oxalate deposits. PLoS One 10:e0139575
Rocha H, Santos LC (1969) Relapse of urinary tract infection in the presence of urinary tract calculi: the role of bacteria within the calculi. J Med Microbiol 2:372–376
Chih-Yen H, Hsing-Lin LIN, Yen-Ko LIN et al (2014) Urinary tract infection in patients with chronic kidney disease. Turk J Med Sci 44:145–149
Varda BK, McNabb-Baltar J, Sood A et al (2015) Urolithiasis and urinary tract infection among patients with inflammatory bowel disease: a review of US emergency department visits between 2006 and 2009. Urology. 85:764–770
Abbo LM, Hooton TM (2014) Antimicrobial stewardship and urinary tract infections. Antibiotics (Basel, Switzerland) 05(3):174–192
Omar M, Abdulwahab-Ahmed A, Chaparala H, Monga M (2015) Does stone removal help patients with recurrent urinary tract infections? J Urol 194:997–1001
Cui X, Ji F, Yan H et al (2015) Comparison between extracorporeal shock wave lithotripsy and ureteroscopic lithotripsy for treating large proximal ureteral stones: a meta-analysis. Urology 85:748–756
Fankhauser CD, Hermanns T, Lieger L et al (2018) Extracorporeal shock wave lithotripsy versus flexible ureterorenoscopy in the treatment of untreated renal calculi. Clin Kidney J 11(3):364–369
de Cógáin MR, Lieske JC, Vrtiska TJ, Tosh PK, Krambeck AE (2014) Secondarily infected nonstruvite urolithiasis: a prospective evaluation. Urology 84:1295–1300
Paonessa JE, Gnessin E, Bhojani N, Williams JC Jr, Lingeman JE (2016) Preoperative bladder urine culture as a predictor of intraoperative stone culture results: clinical implications and relationship to stone composition. J Urol 196:769–774
Author information
Authors and Affiliations
Contributions
DKA: Protocol/project development, Data collection, data analysis, manuscript writing and editing; AEK: Protocol/project development, Data collection, manuscript writing and editing; VS: Data analysis, manuscript writing and editing; FJM: Data collection, manuscript writing and editing; MEW: Data analysis; JJK: Manuscript editing; MER: Protocol/project development, Data collection, data analysis, manuscript writing and editing.
Corresponding author
Ethics declarations
Conflict of interest
AEK—Paid consultant for Lumenis and Boston Scientific. Non-paid consultant for Thermadex. No other authors have disclosures.
Research involving human participants
Appropriate Institutional Review Board approval was obtained for this retrospective review.
Informed consent
An informed consent waiver was approved due to the retrospective nature of this research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Agarwal, D.K., Krambeck, A.E., Sharma, V. et al. Treatment of non-obstructive, non-struvite urolithiasis is effective in treatment of recurrent urinary tract infections. World J Urol 38, 2029–2033 (2020). https://doi.org/10.1007/s00345-019-02977-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-019-02977-3