Abstract
Purpose
To evaluate the prognostic value of positive surgical margins (PSM) focality for the prediction of biochemical recurrence (BCR) in patients undergoing robotic-assisted radical prostatectomy (RARP) for prostate cancer.
Methods
All men with clinically localized prostate cancer undergoing RARP in our tertiary referral centre between May 2005 and August 2016 were retrospectively identified. Patients with neoadjuvant therapy were excluded. Comparisons were made between cases with negative surgical margins (NSM), unifocal PSM (uPSM), and multifocal PSM (mPSM).
Results
From a total of 973 patients available for analysis, 315 (32%) had a PSM. In these patients, 190 had uPSM and 125 had mPSM. Focality of PSM was significantly associated with tumour stage and grade, preoperative PSA, and postoperative PSA persistence (all p < 0.001), but not with nerve sparing (NS) (p = 0.15). PSA persistence was found in 120 (12%) patients, resulting in 853 patients available for survival analyses with a median follow-up of 52 months. Both uPSM and mPSM were found to be independent predictors of BCR, conferring a hazard ratio of 1.9 (95% CI 1.3–3.0; p = 0.002) and 3.4 (95% CI 2.1–5.6; p < 0.001), respectively, when compared to NSM. In subgroup analyses, PSM was particularly predictive for BCR when patients underwent unilateral or bilateral NS (p ≤ 0.003).
Conclusions
Based on a large case series of RARP, we found PSM focality to be an independent predictor of BCR, with a 1.9- and 3.4-fold risk increase for BCR in case of uPSM and mPSM, respectively. PSM seems to be of particular prognostic relevance when NS has been performed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical prostatectomy (RP) is a common treatment method for clinically localized prostate cancer (PCa) [1]. Surgical approaches to RP have steadily evolved over the last decades [2]. Sufficient benign tissue should separate the tumour from the resection plane to ensure a complete removal of malignant cells, while urethral sphincter muscle and adjacent neurovascular should be spared for sustained continence and erectile function [3, 4]. Achieving this dual oncological and functional aim remains a challenge and entails the risk of leaving tumour tissue behind. In such case, tumour cells would outline the superficial layer of the prostatectomy specimen, reported as a positive surgical margin (PSM). The probability for PSM occurrence mostly depends on tumour characteristics, accuracy of preoperative disease burden assessment, surgeons skills, and strategy with respect to nerve-sparing (NS) technique, as well as on the pathological assessment [5, 6].
PSM are reported in 6.5–32% of patients in contemporary series of RP [7] and represent an established independent risk factor for biochemical recurrence (BCR), defined as a prostate-specific antigen (PSA) relapse after surgery [6, 8, 9]. Ultimately, a PSM may lead to clinical progression and premature cancer-related death [10,11,12,13]. Nevertheless, the prognostic value of detailed characterization of PSM in the era of robot-assisted RP (RARP) remains less investigated [6, 14, 15].
In the present study, we aimed to evaluate the association between PSM focality, clinicopathological characteristics, and the risk for BCR in a large contemporary series of men undergoing RARP.
Patients and methods
Study population and design
All men with clinically localized prostate cancer undergoing RARP in our tertiary referral centre between May 2005 and August 2016 were identified. Data were retrieved from electronic medical records and, if necessary, from referring urologist or patient’s general practitioner. From 2008, a part of the identified men were included in our prospective single-centre cohort study (prostate cancer outcomes cohort study: proCOC [16, 17]). The study was approved by the local ethics committee (StV KEK-ZH-Nr. 25-2008 & StV KEK-ZH-Nr. 06/08).
Patients who received a neoadjuvant therapy before surgery were excluded from analysis. A PSA value of 0.1 ng/ml or higher was defined as BCR. Men with a PSA persistence after RARP were excluded from analysis of BCR. Patients were censored from the analysis of BCR whenever any secondary therapy was performed before evidence of BCR. Patients with BCR and possible local recurrence were offered early salvage radiotherapy when the PSA raised over 0.1 ng/ml.
Surgical technique
RARP were performed with the four-arm daVinci® Surgical System (Intuitive Surgical Inc., Sunnyvale, CA, USA). Bilateral extended pelvic lymph-node dissection was performed as described earlier in patients with either PSA ≥ 10 ng/ml at diagnosis or Gleason score (GS) ≥ 7 at biopsy [18]. A unilateral or bilateral nerve-sparing (uNS or bNS) technique was discussed with patients and, if appropriate, offered to patients with clinically organ-confined GS ≤ 7 tumour at biopsy. A uNS was offered to cases with GS 8 and low contralateral tumour burden at biopsy. No nerve sparing (nNS) was performed in all the other patients. Grade of nerve sparing referring to fascial layers was not documented and was not specifically standardized among the surgeons. However, nerve sparing was always performed by an experienced surgeon (> 80 radical prostatectomy performed).
Pathological analysis
All surgical specimens were analysed by specialized uro-pathologists in our institution using standardized whole-mount sections. Tumour characteristics were obtained from pathology reports. Tumour grading was reported according to the current Prognostic Grade Groups (PGG) and GS from pathology reports were matched accordingly [19, 20]. Surgical margins were deemed positive whenever cancer cells touched the surface of the RP specimen on light microscopy (tumour on ink) [17]. For this study, location of the PSM was systematically reviewed from the original pathology report and classified according to Fontenot et al.: posterior, posterolateral, lateral, and anterior at the apex, apical, and mid portions of the prostate or bladder neck [15]. PSM of one of these locations was defined as a unifocal PSM (uPSM), irrespective of PSM length. Whenever two of these locations were positive or bilateral PSMs were present, the PSM was deemed as multifocal (mPSM).
Statistical analysis
Continuous variables are presented as median and interquartile ranges (IQR) and analysed using the Kruskal–Wallis test. The results for categorical variables are presented as percentage and were analysed using Fisher’s exact test or Chi-square test whenever appropriate. Estimates of BCR-free survival (RFS) were calculated with the Kaplan–Meier method and compared with the log-rank test. A stepwise reverse multivariable Cox regression analysis (entry level at p ≤ 0.05 and removal cut-off at p ≥ 0.1) was modelled to evaluate PSM focality as a predictor of BCR, including established predictors of BCR as covariates. Proportional hazard assumption was assessed for each variable with the plot of a log-negative–log-survival distribution and by the plot of Schoenfeld’s residuals over time. Predictive accuracy of the Cox regression model was estimated using the Harrell’s concordance index (c index). All analyses were performed with IBM SPSS Statistics Release 24.0.0.1 (IBM Corp., Armonk, NY, USA). All p values were two-sided with p values < 0.05 considered statistically significant.
Results
A total of 982 patients undergoing RARP were identified. Nine patients were excluded because of neoadjuvant androgen deprivation therapy. Table 1 summarizes patients’ characteristics of the remaining 973 cases available for the final analysis. Median age was 64 years and median preoperative PSA was 7.3 ng/ml. A majority of patients had organ-confined disease (684/973 = 70%) without lymph-node invasion (898/973 = 92%) and a PGG ≤ 3 (785/973 = 81%). Postoperatively, 120/973 (12%) patients had a PSA persistence and were excluded from survival analyses regarding RFS. Median follow-up time for the remaining 853 patients was 52 months (IQR 15–72). During follow-up, BCR occurred in 117/853 (14%) patients after a median follow-up of 24 months (IQR 12–44).
From 973 patients, 315 (32%) had a PSM. Of these, 190 (60%) were reported to have uPSM, whereas 125 (40%) were reported to have mPSM (Table 1). Patients with mPSM had significantly higher preoperative PSA, higher tumour stage, higher PGG, and higher rate of postoperative PSA persistence than patients with uPSM or negative surgical margins (NSM) (all p < 0.001).
Around two-thirds of all patients underwent surgery with NS technique (627/973 = 64%), of which 319 (51%) had uNS and 308 (49%) had bNS (Table 1). No significant association was found between NS and surgical margins status (p = 0.15).
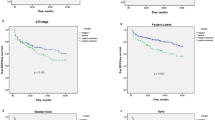
The estimated RFS at 5 years was 86% (95% confidence interval (CI) 83–90%) for NSM, 70% (95% CI 62–79%) for uPSM, and 60% (95% CI 47–74%) for mPSM, respectively (p < 0.001) (Fig. 1).
In a multivariable analysis, both uPSM and mPSM remained significant predictors for BCR, independently of tumour stage, nodal stage, PGG, and application of NS (Table 2). There was a 1.9-fold risk increase for BCR between NSM and uPSM (95% CI 1.3–3.0; p = 0.002), and a 3.4-fold risk increase for BCR between NSM and mPSM (95% CI 2.1–5.6; p < 0.001). Of note, bNS remained an independent predictor for BCR, with a 2.1-fold risk increase for BCR compared to nNS (95% CI 1.3–3.4; p = 0.003). The preoperative PSA reached the removal level cut-off (p ≥ 0.1) and was thus not included in the multivariable Cox regression model.
The predictive accuracy of the Cox regression model was 0.781 for the conventional NSM versus PSM stratification versus 0.783 for NSM, uPSM, and mPSM stratification. When surgical margin status was removed from the model, the c-index was 0.734.
The Cox regression model was tested for interaction between above-mentioned covariates. A significant interaction was found between surgical margin status and PGG, as well as between surgical margin status and NS technique (data not shown). This prompted us to conduct a subgroup analysis stratifying for PGG and NS technique (Fig. 2a–e). To further complete the subgroup analysis, a stratification for tumour stage was also performed (Fig. 2f, g).
In patients with PGG ≤ 3, both uPSM and mPSM showed lower RFS estimates than NSM (Fig. 2a), whereas only mPSM had denotatively lower RFS estimates in patients with PGG ≥ 4 (Fig. 2b). This observation was verified by a multivariable Cox regression analysis (Table S1; all p < 0.001). Neither uPSM nor mPSM was predictive for BCR when patients did not receive any NS (Fig. 2c, Table S2, all p > 0.05). Contrarily, both uPSM and mPSM were predictive for BCR in patients who had undergone nerve sparing (Fig. 2d, e, Table S2; all p ≤ 0.003).
In the subgroup analysis for tumour stage, both uPSM and mPSM remained independent predictors for BCR in both ≤ pT2 and ≥ pT3 tumours (Fig. 2f, g and Table S3, all p ≤ 0.04).
Patients with BCR were treated by the early salvage radiotherapy in 19 of 25 (76%) cases when mPSM was present, in 19 of 31 cases (61%) when uPSM was noted and in 29 of 51 (57%) cases with NS. Data on therapy decision after BCR were missing in ten patients (0, 4, and 6 cases in the mPSM, uPSM, and NSM groups, respectively). Adjuvant radiotherapy was performed before evidence of BCR in three patients, which were censored from the RFS analysis at the time of secondary therapy.
Discussion
The present study consists of a large contemporary consecutive series of RARP performed over more than a decade. Of all cases, 32% were deemed positive for surgical margins and differentiation for PSM focality was significantly associated with worse clinicopathological parameters. Most importantly, focality of PSM was found as an independent predictor of BCR, with an HR of 1.9 and 3.4 for uPSM and mPSM, respectively, when compared to NSM.
In a systematic review on RARP series, Novara et al. found a mean PSM rate of 15% (range 6.5–32) and reported tumour stage and grade to be strong predictors of PSM [7]. Comparatively, the PSM rate in the present study was at the upper range limit (32%), despite a relatively low rate of extracapsular tumour extension (≥ pT3: 30%) and that of high-grade disease (PGG ≥ 4: 19%). This discrepancy may come from interobserver variability concerning PSM evaluation, which has been reported by several studies and was particularly high between non-academic pathologists and dedicated academic uro-pathologists [21,22,23]. The relatively high PSM rate in our series may thus be attributable to the meticulous evaluation of all prostatectomy samples by specialized uro-pathologists, who reported a uPSM even when only one tumour cell touched the ink surface.
To the best of our knowledge, this is the first study based on a case series including only RARP and reporting both uPSM and mPSM as independent predictors of BCR. Multiple prior studies have investigated the role of PSM in RP and showed results that were in line with our findings. In a case series of 1712 open RP, Mauermann et al. found an adjusted HR for BCR of 1.2 and 1.6 for uPSM and mPSM (p = 0.001 and p < 0.001), respectively, when compared to NSM [24]. Sammon et al. reported an adjusted HR for BCR of 3.6 for mPSM (p < 0.001), but the authors did not specify the risk entailed by patients with uPSM [25]. When directly comparing mPSM with uPSM, an adjusted HR for BCR of 1.4 (p = 0.002) and 2.3 (p < 0.001) has been reported by Stephenson et al. and Lee et al., respectively [26, 27]. A few studies found mPSM, but not uPSM as an independent predictor of BCR in patients after RP [28,29,30,31]. The other reports showed that PSM focality was not an independent predictor for BCR [15, 32,33,34,35,36,37]. However, these reports had either low patient sample size (< 500), low overall PSM rate (< 10%), and short follow-up period (median ≤ 12 months), or did not include a comparison with NSM cases. In summary, the current literature–including our study—suggests that PSM stratified by focality is of prognostic value in patients after RP for prostate cancer.
Of interest, subgroup analyses included in the present study revealed a denotative role for PSM focality in patients with PGG ≤ 3 as well as in patients who had undergone NS. Because the area of nerve sparing is particularly prone to PSM [38], it appears conceivable that a relevant amount of tumour tissue may have been left behind, even when seemingly minimal uPSM was reported. In contrast, we were not able to show any significant association between uPSM and BCR in patients with PGG ≥ 4 as well as in patients who had not undergone NS. Besides lack of analytical power, a potential explanation may be that the two later subgroups are characterized by a selection of high-risk patients, for whom other tumour characteristics (e.g., micrometastases) may have outweighed the risk entailed by uPSM.
Whether the application of NS bears a higher risk for PSM and would, therefore, impact on prognosis is debated [38, 39]. In the present study, no association was found between NS technique and surgical margins status. Although not significant in univariable analysis, bNS was found as an independent predictor for BCR in multivariable analysis, which may be the consequence of interaction between NS and surgical margin status [40]. Such association has not been reported previously in the literature and, thus, deserves further assessment in the other large cohorts. One explanation may be that the disease burden was underestimated in this patient group, leading to an inadequate selection of patients who were offered a bNS technique. Underestimation of disease burden prior RP has been shown to be relevant in a previous study from our centre [41]. In that study, tumour undergrading at biopsy frequently occurred in a group of community pathologists and was found as an independent predictor for both PSM and BCR. In light of these results, implementation of preoperative tumour delineation by multiparametric MRI as well as strategies of intraoperative fresh-frozen tissue analysis are promising tools to overcome the potential oncological risk of NS [42,43,44,45].
The present study has limitations. PSM length and GS at PSM were not consistently documented in pathological reports available for this study and could, therefore, not be analysed. Due to an insufficient number of cases accounting for disease progression or death events, these oncological outcomes were not evaluated in this study.
Conclusions
PSM focality is significantly associated with worse clinicopathological features and remains a significant independent predictor for BCR in patients after RARP. PSM seems to be of particular prognostic relevance when NS has been performed. Clinicians should be aware of the prognostic impact of PSM focality for further patient counselling.
References
Bill-Axelson A, Holmberg L, Garmo H, Rider JR, Taari K, Busch C, Nordling S, Häggman M, Andersson S-O, Spångberg A, Andrén O, Palmgren J, Steineck G, Adami H-O, Johansson J-E (2014) Radical prostatectomy or watchful waiting in early prostate cancer. N Engl J Med 370:932–942. https://doi.org/10.1056/NEJMoa1311593
Ficarra V, Novara G, Artibani W, Cestari A, Galfano A, Graefen M, Guazzoni G, Guillonneau B, Menon M, Montorsi F, Patel V, Rassweiler J, Van Poppel H (2009) Retropubic, laparoscopic, and robot-assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. Eur Urol 55:1037–1063. https://doi.org/10.1016/j.eururo.2009.01.036
Sooriakumaran P, Dev HS, Skarecky D, Ahlering TE, Wiklund P (2016) Oncologic outcomes of robotic-assisted radical prostatectomy: the “balancing act” of achieving cancer control and minimizing collateral damage. In: Razdan S (ed) Urinary continence and sexual function after robotic radical prostatectomy. Springer International Publishing, Cham, pp 101–113
Walsh PC, Donker PJ (1982) Impotence following radical prostatectomy: insight into etiology and prevention. J Urol 128:492–497
Vickers A, Bianco F, Cronin A, Eastham J, Klein E, Kattan M, Scardino P (2010) The learning curve for surgical margins after open radical prostatectomy: implications for margin status as an oncological end point. J Urol 183:1360–1365. https://doi.org/10.1016/j.juro.2009.12.015
Yossepowitch O, Briganti A, Eastham JA, Epstein J, Graefen M, Montironi R, Touijer K (2014) Positive surgical margins after radical prostatectomy: a systematic review and contemporary update. Eur Urol 65:303–313. https://doi.org/10.1016/j.eururo.2013.07.039
Novara G, Ficarra V, Mocellin S, Ahlering TE, Carroll PR, Graefen M, Guazzoni G, Menon M, Patel VR, Shariat SF, Tewari AK, Van Poppel H, Zattoni F, Montorsi F, Mottrie A, Rosen RC, Wilson TG (2012) Systematic review and meta-analysis of studies reporting oncologic outcome after robot-assisted radical prostatectomy. Eur Urol 62:382–404. https://doi.org/10.1016/j.eururo.2012.05.047
Karakiewicz PI, Eastham JA, Graefen M, Cagiannos I, Stricker PD, Klein E, Cangiano T, Schröder FH, Scardino PT, Kattan MW (2005) Prognostic impact of positive surgical margins in surgically treated prostate cancer: multi-institutional assessment of 5831 patients. Urology 66:1245–1250. https://doi.org/10.1016/j.urology.2005.06.108
Meeks JJ, Eastham JA (2013) Radical prostatectomy: positive surgical margins matter. Urol Oncol 31:974–979. https://doi.org/10.1016/j.urolonc.2011.12.011
Boorjian SA, Karnes RJ, Crispen PL, Carlson RE, Rangel LJ, Bergstralh EJ, Blute ML (2010) The impact of positive surgical margins on mortality following radical prostatectomy during the prostate specific antigen era. J Urol 183:1003–1009. https://doi.org/10.1016/j.juro.2009.11.039
Chalfin HJ, Dinizo M, Trock BJ, Feng Z, Partin AW, Walsh PC, Humphreys E, Han M (2012) Impact of surgical margin status on prostate cancer-specific mortality. BJU Int 110:1684–1689. https://doi.org/10.1111/j.1464-410X.2012.11371.x
Stephenson AJ, Eggener SE, Hernandez AV, Klein EA, Kattan MW, Wood DP, Rabah DM, Eastham JA, Scardino PT (2014) Do margins matter? The influence of positive surgical margins on prostate cancer-specific mortality. Eur Urol 65:675–680. https://doi.org/10.1016/j.eururo.2013.08.036
Wright JL, Dalkin BL, True LD, Ellis WJ, Stanford JL, Lange PH, Lin DW (2010) Positive surgical margins at radical prostatectomy predict prostate cancer specific mortality. J Urol 183:2213–2218. https://doi.org/10.1016/j.juro.2010.02.017
Lee S, Kim KB, Jo JK, Ho JN, Oh JJ, Jeong SJ, Hong SK, Byun SS, Choe G, Lee SE (2016) Prognostic value of focal positive surgical margins after radical prostatectomy. Clin Genitourin Cancer 14(4):e313–e319. https://doi.org/10.1016/j.clgc.2015.12.013
Somford DM, van Oort IM, Cosyns JP, Witjes JA, Kiemeney LA, Tombal B (2012) Prognostic relevance of number and bilaterality of positive surgical margins after radical prostatectomy. World J Urol 30(1):105–110. https://doi.org/10.1007/s00345-010-0641-4
Umbehr M, Kessler TM, Sulser T, Kristiansen G, Probst N, Steurer J, Bachmann LM (2008) ProCOC: the prostate cancer outcomes cohort study. BMC Urol 8:9. https://doi.org/10.1186/1471-2490-8-9
Wettstein MS, Saba K, Umbehr MH, Murtola TJ, Fankhauser CD, Adank JP, Hofmann M, Sulser T, Hermanns T, Moch H, Wild P, Poyet C (2017) Prognostic role of preoperative serum lipid levels in patients undergoing radical prostatectomy for clinically localized prostate cancer. Prostate 77(5):549–556. https://doi.org/10.1002/pros.23296
Feicke A, Baumgartner M, Talimi S, Schmid DM, Seifert H-H, Müntener M, Fatzer M, Sulser T, Strebel RT (2009) Robotic-assisted laparoscopic extended pelvic lymph-node dissection for prostate cancer: surgical technique and experience with the first 99 cases. Eur Urol 55:876–883. https://doi.org/10.1016/j.eururo.2008.12.006
Epstein JI, Egevad L, Amin MB, Delahunt B, Srigley JR, Humphrey PA, Grading C (2016) The 2014 International Society of Urological Pathology (ISUP) consensus conference on Gleason grading of prostatic carcinoma: definition of grading patterns and proposal for a new grading system. Am J Surg Pathol 40(2):244–252. https://doi.org/10.1097/pas.0000000000000530
Epstein JI, Zelefsky MJ, Sjoberg DD, Nelson JB, Egevad L, Magi-Galluzzi C, Vickers AJ, Parwani AV, Reuter VE, Fine SW, Eastham JA, Wiklund P, Han M, Reddy CA, Ciezki JP, Nyberg T, Klein EA (2016) A contemporary prostate cancer grading system: a validated alternative to the Gleason score. Eur Urol 69(3):428–435. https://doi.org/10.1016/j.eururo.2015.06.046
Ekici S, Ayhan A, Erkan L, Bakkaloğlu M, Özen H (2003) The role of the pathologist in the evaluation of radical prostatectomy specimens. Scand J Urol Nephrol 37:387–391. https://doi.org/10.1080/00365590310014535
van der Kwast TH, Collette L, Van Poppel H, Van Cangh P, Vekemans K, DaPozzo L, Bosset JF, Kurth KH, Schroder FH, Bolla M, European Organisation for R, Treatment of Cancer R, Genito-Urinary Cancer G (2006) Impact of pathology review of stage and margin status of radical prostatectomy specimens (EORTC trial 22911). Virchows Arch 449(4):428–434. https://doi.org/10.1007/s00428-006-0254-x
Evans AJ, Henry PC, Van der Kwast TH, Tkachuk DC, Watson K, Lockwood GA, Fleshner NE, Cheung C, Belanger EC, Amin MB, Boccon-Gibod L, Bostwick DG, Egevad L, Epstein JI, Grignon DJ, Jones EC, Montironi R, Moussa M, Sweet JM, Trpkov K, Wheeler TM, Srigley JR (2008) Interobserver variability between expert urologic pathologists for extraprostatic extension and surgical margin status in radical prostatectomy specimens. Am J Surg Pathol 32:1503–1512. https://doi.org/10.1097/PAS.0b013e31817fb3a0
Mauermann J, Fradet V, Lacombe L, Dujardin T, Tiguert R, Tetu B, Fradet Y (2013) The impact of solitary and multiple positive surgical margins on hard clinical end points in 1712 adjuvant treatment-naive pT2–4 N0 radical prostatectomy patients. Eur Urol 64:19–25. https://doi.org/10.1016/j.eururo.2012.08.002
Sammon JD, Trinh Q-D, Sukumar S, Ravi P, Friedman A, Sun M, Schmitges J, Jeldres C, Jeong W, Mander N, Peabody JO, Karakiewicz PI, Harris M (2013) Risk factors for biochemical recurrence following radical perineal prostatectomy in a large contemporary series: a detailed assessment of margin extent and location. Urol Oncol 31:1470–1476. https://doi.org/10.1016/j.urolonc.2012.03.013
Stephenson AJ, Wood DP, Kattan MW, Klein EA, Scardino PT, Eastham JA, Carver BS (2009) Location, extent and number of positive surgical margins do not improve accuracy of predicting prostate cancer recurrence after radical prostatectomy. J Urol 182:1357–1363. https://doi.org/10.1016/j.juro.2009.06.046
Lee JW, Ryu JH, Kim YB, Yang SO, Lee JK, Jung TY (2013) Do positive surgical margins predict biochemical recurrence in all patients without adjuvant therapy after radical prostatectomy? Korean J Urol 54(8):510–515. https://doi.org/10.4111/kju.2013.54.8.510
Maxeiner A, Magheli A, Jöhrens K, Kilic E, Braun TL, Kempkensteffen C, Hinz S, Stephan C, Miller K, Busch J (2016) Significant reduction in positive surgical margin rate after laparoscopic radical prostatectomy by application of the modified surgical margin recommendations of the 2009 International Society of Urological Pathology consensus. BJU Int 118:750–757. https://doi.org/10.1111/bju.13451
Dev HS, Wiklund P, Patel V, Parashar D, Palmer K, Nyberg T, Skarecky D, Neal DE, Ahlering T, Sooriakumaran P (2015) Surgical margin length and location affect recurrence rates after robotic prostatectomy. Urol Oncol 33:109.e107–109.e113. https://doi.org/10.1016/j.urolonc.2014.11.005
Sooriakumaran P, Ploumidis A, Nyberg T, Olsson M, Akre O, Haendler L, Egevad L, Nilsson A, Carlsson S, Jonsson M, Adding C, Hosseini A, Steineck G, Wiklund P (2015) The impact of length and location of positive margins in predicting biochemical recurrence after robot-assisted radical prostatectomy with a minimum follow-up of 5 years. BJU Int 115(1):106–113. https://doi.org/10.1111/bju.12483
Kordan Y, Salem S, Chang SS, Clark PE, Cookson MS, Davis R, Herrell SD, Baumgartner R, Phillips S, Smith JA Jr, Barocas DA (2009) Impact of positive apical surgical margins on likelihood of biochemical recurrence after radical prostatectomy. J Urol 182(6):2695–2701. https://doi.org/10.1016/j.juro.2009.08.054
Pfitzenmaier J, Pahernik S, Tremmel T, Haferkamp A, Buse S, Hohenfellner M (2008) Positive surgical margins after radical prostatectomy: do they have an impact on biochemical or clinical progression? BJU Int 102(10):1413–1418. https://doi.org/10.1111/j.1464-410X.2008.07791.x
Godoy G, Tareen BU, Lepor H (2009) Site of positive surgical margins influences biochemical recurrence after radical prostatectomy. BJU Int 104(11):1610–1614. https://doi.org/10.1111/j.1464-410X.2009.08688.x
Shikanov S, Song J, Royce C, Al-Ahmadie H, Zorn K, Steinberg G, Zagaja G, Shalhav A, Eggener S (2009) Length of positive surgical margin after radical prostatectomy as a predictor of biochemical recurrence. J Urol 182(1):139–144. https://doi.org/10.1016/j.juro.2009.02.139
Psutka SP, Feldman AS, Rodin D, Olumi AF, Wu C-L, McDougal WS (2011) Men with organ-confined prostate cancer and positive surgical margins develop biochemical failure at a similar rate to men with extracapsular extension. Urology 78:121–125. https://doi.org/10.1016/j.urology.2010.10.036
Hsu M, Chang SL, Ferrari M, Nolley R, Presti JC Jr, Brooks JD (2011) Length of site-specific positive surgical margins as a risk factor for biochemical recurrence following radical prostatectomy. Int J Urol 18(4):272–279. https://doi.org/10.1111/j.1442-2042.2011.02729.x
O’Neil LM, Walsh S, Cohen RJ, Lee S (2015) Prostate carcinoma with positive margins at radical prostatectomy: role of tumour zonal origin in biochemical recurrence. BJU Int 116(Suppl 3):42–48. https://doi.org/10.1111/bju.13173
Preston MA, Breau RH, Lantz AG, Morash C, Gerridzen RG, Doucette S, Mallick R, Eastham JA, Cagiannos I (2015) The association between nerve sparing and a positive surgical margin during radical prostatectomy. Urol Oncol 33:18.e11–18.e16. https://doi.org/10.1016/j.urolonc.2014.09.006
Boehm K, Graefen M (2015) Prostate cancer: nerve-sparing surgery and risk of positive surgical margins. Nat Rev Urol 12:131–132. https://doi.org/10.1038/nrurol.2014.359
Lo SK, Li IT, Tsou TS, See L (1995) Non-significant in univariate but significant in multivariate analysis: a discussion with examples. Changgeng Yi Xue Za Zhi 18(2):95–101
Mortezavi A, Keller EX, Poyet C, Hermanns T, Saba K, Randazzo M, Fankhauser CD, Wild PJ, Moch H, Sulser T, Eberli D (2016) Clinical impact of prostate biopsy undergrading in an academic and community setting. World J Urol. https://doi.org/10.1007/s00345-016-1788-4
von Bodman C, Brock M, Roghmann F, Byers A, Löppenberg B, Braun K, Pastor J, Sommerer F, Noldus J, Palisaar RJ (2013) Intraoperative frozen section of the prostate decreases positive margin rate while ensuring nerve sparing procedure during radical prostatectomy. J Urol 190:515–520. https://doi.org/10.1016/j.juro.2013.02.011
Beyer B, Schlomm T, Tennstedt P, Boehm K, Adam M, Schiffmann J, Sauter G, Wittmer C, Steuber T, Graefen M, Huland H, Haese A (2014) A feasible and time-efficient adaptation of NeuroSAFE for da Vinci robot-assisted radical prostatectomy. Eur Urol 66:138–144. https://doi.org/10.1016/j.eururo.2013.12.014
Bianchi R, Cozzi G, Petralia G, Alessi S, Renne G, Bottero D, Brescia A, Cioffi A, Cordima G, Ferro M, Matei DV, Mazzoleni F, Musi G, Mistretta FA, Serino A, Tringali VML, Coman I, De Cobelli O (2016) Multiparametric magnetic resonance imaging and frozen-section analysis efficiently predict upgrading, upstaging, and extraprostatic extension in patients undergoing nerve-sparing robotic-assisted radical prostatectomy. Medicine (Baltimore) 95:e4519. https://doi.org/10.1097/md.0000000000004519
Petralia G, Musi G, Padhani AR, Summers P, Renne G, Alessi S, Raimondi S, Matei DV, Renne SL, Jereczek-Fossa BA, De Cobelli O, Bellomi M (2015) Robot-assisted radical prostatectomy: multiparametric MR imaging-directed intraoperative frozen-section analysis to reduce the rate of positive surgical margins. Radiology 274:434–444. https://doi.org/10.1148/radiol.14140044
Funding
None.
Author information
Authors and Affiliations
Contributions
EXK protocol/project development, data collection or management, data analysis, and manuscript writing/editing. JB data collection or management, and manuscript writing/editing. AJB data collection or management, and manuscript writing/editing. KS data collection or management, data analysis, and manuscript writing/editing. AM data collection or management, data analysis, and manuscript writing/editing. BK data collection or management, and manuscript writing/editing. CDF data collection or management, data analysis, and manuscript writing/editing. PW protocol/project development, data analysis, and manuscript writing/editing. TS protocol/project development, data analysis, and manuscript writing/editing. TH protocol/project development, data analysis, and manuscript writing/editing. DE protocol/project development, data analysis, and manuscript writing/editing. CP protocol/project development, data collection or management, data analysis, and manuscript writing/editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors disclose no potential conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Keller, E.X., Bachofner, J., Britschgi, A.J. et al. Prognostic value of unifocal and multifocal positive surgical margins in a large series of robot-assisted radical prostatectomy for prostate cancer. World J Urol 37, 1837–1844 (2019). https://doi.org/10.1007/s00345-018-2578-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-018-2578-y