Abstract
Purpose
Patients without evidence of disease at radical cystectomy (RC) following neoadjuvant chemotherapy (NAC) have the greatest potential for survival in muscle-invasive bladder cancer. Historically, 15 % of such patients will experience disease recurrence and cancer-specific mortality. We sought to evaluate the effect of pre-treatment clinical factors on the risk of recurrence in patients who were ypT0N0 at RC.
Methods
We performed a multi-institutional review of patients treated with NAC + RC for muscle-invasive bladder cancer (≥cT2) without pathologic evidence of disease at surgery (ypT0N0). The association of pre-treatment clinicopathologic features with recurrence was evaluated using Cox proportional hazards.
Results
A total of 78 patients were identified with ypT0 disease at RC after NAC. Median postoperative follow-up was 32.4 months (IQR 16.8, 60.0), during which time 17 patients recurred at a median of 6.4 months after RC. Estimated 3-year recurrence-free survival (RFS) of this cohort was 74.8 %. In univariate analysis, cT4 disease (HR 3.12; p = 0.04) and time to RC (HR 1.17 for each month increase; p < 0.01) were associated with inferior RFS.
Conclusion
Patients without evidence of disease at the time of RC are still at risk of recurrence and death from bladder cancer. Higher clinical stage and increased time to RC were associated with an increased risk of recurrence and subsequent death. These data highlight the importance of timely RC and the continued risk of recurrence in higher clinically staged patients—underscoring the need for close monitoring and patient counseling.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Muscle-invasive and locally advanced bladder cancer remains a lethal urologic malignancy, with an estimated 70 % 5-year survival rate even when localized to the bladder [1]. Neoadjuvant chemotherapy (NAC) followed by radical cystectomy (RC) is considered the standard of care for these patients [2, 3]. Patients with a pathologic complete response (ypT0N0) achieve the greatest survival benefit from NAC [4, 5]. To that end, there has been an increasing trend in the literature to utilize a complete pathologic response as a surrogate for survival outcomes when assessing neoadjuvant chemotherapy [6–8].
It is unknown whether complete pathologic response is an adequate marker of success for patients receiving NAC, as even those patients with the greatest potential for cure are still at risk of cancer-specific mortality. In the original neoadjuvant trial by Grossman, 15 % of patients who achieved a pathologic complete response died of their disease [2]. Similarly, 15–20 % of patients without evidence of disease in their pathologic specimen after RC alone suffer cancer-specific mortality [5]. Thus, while it is understood that patients who achieve a pathologic complete response have the potential for long-term survival following neoadjuvant chemotherapy, not all patients follow the same course. Given this gap in our knowledge, we sought to describe the survival of patients with a pathologic complete response following treatment with neoadjuvant chemotherapy along with the identification of risk factors for recurrence and death in a multi-institutional cohort.
Methods
We performed a retrospective review of patients with muscle-invasive and locally advanced bladder cancer (≥cT2N0-3) treated with NAC followed by RC between 1980 and 2012 as part of an institutional review board (IRB)-approved collaboration between Mayo Clinic (n = 37), the University of Texas MD Anderson Cancer Center (n = 25), and the University of Kansas Medical Center (n = 16). As per the review of the IRB, consent was waived. Pre-treatment clinical variables were collected including age, gender, race, clinical stage, concomitant carcinoma in situ, lymphovascular invasion, hydronephrosis, and the type of chemotherapy utilized. Clinical staging was defined according to the AJCC classification [9] and was based on the findings at the time of cystoscopic examination with a bimanual palpation of the abdomen, together with axial imaging prior to the receipt of neoadjuvant chemotherapy.
Following NAC, radical cystectomy and extended lymphadenectomy were performed as has been previously described [10] by fellowship-trained urologic oncologists at all institutions. Board-certified pathologists at each participating institution performed tumor staging according to the American Joint Committee on Cancer’s AJCC Cancer Staging Manual [9]. Patients were selected for analysis based on the presence of a pathologic complete response (ypT0N0) on final pathology specimen. Following radical cystectomy, patients returned for surveillance as per the NCCN guidelines with visits at 3- to 6-month intervals for the first 2 years followed by 6- to 12-month intervals, thereafter [11].
Patients with a complete response were stratified by recurrence status at the time of final follow-up. Descriptive statistics were utilized to summarize the pre-treatment characteristics, and differences between groups were assessed utilizing 2-sided t tests (continuous data) and Chi-squared analyses (categorical) with significance defined as p < 0.05. Pre-treatment variables demonstrating a significant difference between patients who recurred and those who did not were further analyzed using Kaplan–Meier and Cox proportional hazard methods for recurrence-free and cancer-specific survival. All analyses were performed utilizing SAS 9.3 (Cary, NC, USA).
Results
In total, 359 patients were treated with NAC followed by RC during the study period. Of these patients, 78 (21.2 %) had a pathologic complete response, with characteristics summarized in Table 1. At a median of 32.4 months (IQR 16.8, 60.0) of follow-up, 17 (21.8 %) patients suffered recurrence, 16 of whom died of disease. Estimated 3-year recurrence-free and cancer-specific survival was 74.8 and 81.1 %, respectively. Table 2 demonstrates the sites of recurrence. All recurrences occurred within 3 years of the time of surgery, at a median of 6.4 months (IQR 4.44, 14.4) from RC. Ten patients recurred at multiple sites, with pulmonary metastases representing the predominant recurrence site. Characteristics between patients stratified by recurrence did not differ, with the exception of pre-treatment clinical stage and time to RC from pre-chemotherapy transurethral resection (TUR). Specifically, a greater proportion of patients with recurrence presented with cT4 disease (29.4 %) versus cT2/3 (6.6 %, p = 0.009) and at a greater interval from pre-chemotherapy TUR to RC (median 5.8 vs. 5.1 months, p = 0.02).
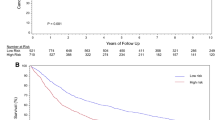
In univariate Cox proportional hazards regression of pre-surgical variables on the risk of recurrence, only cT4 disease (HR 3.12; 95 % CI 1.10–8.87; p = 0.03) and time to RC from TUR (HR 1.17 for each month increase; 95 % CI 1.07–1.28; p < 0.01) were associated with recurrence (Table 3). Indeed, on multivariable analysis, time to RC from TUR and cT4 remained associated with risk of recurrence (HR 1.17 [p < 0.01] and 3.19 [p = 0.048], respectively). Estimated 3-yr recurrence-free survival for cT4 versus cT2/cT3 was 41.7 and 80.1 %, respectively (p = 0.02, Fig. 1). Similarly, cancer-specific mortality was significantly increased in patients with cT4 disease (HR 3.05: 95 % CI: 1.06–8.78, p = 0.04) with an estimated 3-year CSS of 64.8 versus 83.6 %, p = 0.03 (see Fig. 2). Patients were stratified by clinical stage in order to identify differences in clinical features which may explain stage-specific differences in survival. Chemotherapy regimen and decade of treatment (Supplemental Table 1) differed by clinical stage at presentation; however, after adjusting for their effect, cT4 disease remained associated with recurrence risk (data not shown).
Discussion
To our knowledge, the present data represent the first focused description of survival in patients with a pathologic complete response after treatment with NAC and RC. Our results demonstrate that approximately 21 % of patients with a complete response suffer recurrence at a median of 6 months. Patterns of recurrence were typical of urothelial cell carcinoma, with a predominance of pulmonary metastatic disease. Finally, we identified clinical stage T4 and increased time to RC as significant predictors of the risk of subsequent recurrence and death after treatment.
As previously noted, NAC and consolidative surgery are the standard of care for muscle-invasive bladder cancer. However, research has shown that in the non-neoadjuvant setting approximately 15 % of patients will ultimately recur despite pT0N0 disease [2, 5] which is corroborated in the present series. Given the paucity of literature on these patients who are pathologically free of disease, the question remains as to why these patients recur?
Our finding of an association of advanced clinical stage with risk of recurrence during follow-up may be explained by the effect of TUR in patients managed with NAC and RC. Specifically, the adequacy of the pre-chemotherapy TUR has been shown to increase pathologic complete response rate after NAC and RC [12]. However, in patients managed with bladder preservation in whom a complete response is noted, distant recurrence during follow-up is not uncommon [13]. While it is intuitive that transurethral resection may drive the outcomes for the primary tumor, these distant recurrences are likely explained by our inability to accurately detect and stage occult metastatic disease in patients with advanced clinical stage. Certainly, the short interval from therapy to recurrence—6 months in the present series—would argue toward preexisting metastatic disease.
It is well established that preoperative staging is inaccurate in approximately 50 % of patients undergoing RC [14–16]. The NCCN guidelines recommend imaging with either contrast-enhanced CT scanning or MR Urography [11]; however, the sensitivity of these studies ranges from 60.0 to 76.4 % [17, 18]. In order to improve staging—and by corollary assessment of response to chemotherapy—alternative modalities are needed. Other such approaches include C11-choline and 18FDG PET/CT, which have been extensively studied in urothelial cell carcinoma with mixed results when compared to conventional CT scanning [19–22].
Furthermore, NAC is not a binary event; rather, it is affected by treatment regimen, dosing, number of cycles, and tolerance. Certainly, our finding of an association with increased time from pre-chemotherapy TUR to RC and risk of recurrence suggests that timely chemotherapy and RC are important in this population—a conclusion that is well established in the immediate cystectomy literature [23]. Additionally, the use of NAC is based on trials which utilized MVAC [2, 3], and we noted considerable variability in treatment regimen, a finding corroborated by a recent “real-world” analysis of NAC use [8]. Finally, response to NAC may represent selection of chemosensitive and less aggressive tumors as opposed to a marker of optimal delivery of chemotherapy [6]. Thus, while pathologic complete response has been suggested as a surrogate for success in management of this patient population, the method by which a complete response is garnered is multifactorial and may not adequately reflect patient outcome.
Our results are not without limitations. The subset of patients with a complete response after NAC is small which limited our statistical analyses. Thus, while we were able to demonstrate that clinical T4 was associated with RFS and CSS after adjusting for single variables per model, our inability to control for all variables raises the potential for unmeasured confounders. Furthermore, our inability to control time to RC for chemotherapy regimen and number of cycles limits the interpretation of these specific time-dependent findings. Furthermore, we acknowledge that our inability to evaluate the effect of cT4a as compared to cT4b may obscure a potentially meaningful difference in survival. While this does limit the ability to compare our cohort and data to the large RCTs of NAC, these data represent a real-world analysis of outcomes in patients with a complete pathologic response to NAC.
Another limitation is the pattern and timing of recurrence. Our series is limited by a median follow-up of 32.4 months, which may prevent adequate capture of all recurrences given that patients with a complete response may have a delayed recurrence pattern. However, prior literature has shown that approximately 90 % of recurrences occur within 36 months of surgery [24]. As mentioned previously, the pattern of recurrence raises the potential concern for inaccurate pre-surgical clinical staging in this cohort despite the receipt of standard of care evaluation. Despite these limitations, our data demonstrate that patients with a complete pathologic response following NAC and RC are still subject to recurrence and that patients with advanced clinical stage and longer intervals to RC appear to have the greatest risk of recurrence during follow-up.
Conclusion
Muscle-invasive bladder cancer remains a lethal disease even in the pathologic absence of disease at cystectomy. Despite a recent focus on equating pathologic response to survival, our data corroborate prior experiences with recurrence in patients without disease at cystectomy [5] and underscore the gap between pathology and durable survival. Finally, our results highlight the group of patients at greatest risk of recurrence and indicate that clinical stage should be taken into consideration to individualize follow-up after radical cystectomy.
References
Siegel R et al (2014) Cancer statistics, 2014. CA Cancer J Clin 64(1):9–29
Grossman HB et al (2003) Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N Engl J Med 349(9):859–866
Advanced Bladder Cancer Meta-analysis Collaboration (2005) Neoadjuvant chemotherapy in invasive bladder cancer: update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta-analysis collaboration. Eur Urol 48(2):202–205 (discussion 205–206)
Rosenblatt R et al (2012) Pathologic downstaging is a surrogate marker for efficacy and increased survival following neoadjuvant chemotherapy and radical cystectomy for muscle-invasive urothelial bladder cancer. Eur Urol 61(6):1229–1238
Kassouf W et al (2007) P0 stage at radical cystectomy for bladder cancer is associated with improved outcome independent of traditional clinical risk factors. Eur Urol 52(3):769–774
Lavery HJ et al (2014) Pathological T0 following radical cystectomy with or without neoadjuvant chemotherapy: a useful surrogate. J Urol 191(4):898–906
Petrelli F et al (2014) Correlation of pathologic complete response with survival after neoadjuvant chemotherapy in bladder cancer treated with cystectomy: a meta-analysis. Eur Urol 65(2):350–357
Zargar H et al (2015) Multicenter assessment of neoadjuvant chemotherapy for muscle-invasive bladder cancer. Eur Urol 67(2):241–249
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474
Zehnder P et al (2011) Super extended versus extended pelvic lymph node dissection in patients undergoing radical cystectomy for bladder cancer: a comparative study. J Urol 186(4):1261–1268
Clark PE et al (2013) Bladder cancer. J Natl Compr Canc Netw 11(4):446–475
James AC et al (2014) Role of maximal endoscopic resection before cystectomy for invasive urothelial bladder cancer. Clin Genitourin Cancer 12(4):287–291
Meyer A et al (2014) The natural history of clinically complete responders to neoadjuvant chemotherapy for urothelial carcinoma of the bladder. J Urol 192(3):696–701
Svatek RS et al (2011) Discrepancy between clinical and pathological stage: external validation of the impact on prognosis in an international radical cystectomy cohort. BJU Int 107(6):898–904
Ploeg M et al (2012) Discrepancy between clinical staging through bimanual palpation and pathological staging after cystectomy. Urol Oncol 30(3):247–251
Gray PJ et al (2014) Clinical-pathologic stage discrepancy in bladder cancer patients treated with radical cystectomy: results from the national cancer data base. Int J Radiat Oncol Biol Phys 88(5):1048–1056
Tritschler S et al (2012) Staging of muscle-invasive bladder cancer: can computerized tomography help us to decide on local treatment? World J Urol 30(6):827–831
Papalia R et al (2012) Diffusion-weighted magnetic resonance imaging in patients selected for radical cystectomy: detection rate of pelvic lymph node metastases. BJU Int 109(7):1031–1036
Rouanne M et al (2014) Potential impact of 18F-FDG PET/CT on patients selection for neoadjuvant chemotherapy before radical cystectomy. Eur J Surg Oncol 40(12):1724–1730
Ozturk H (2015) Detecting metastatic bladder cancer using 18F-fluorodeoxyglucose positron-emission tomography/computed tomography. Cancer Res Treat 47(4):834–843
Maurer T et al (2012) Diagnostic efficacy of [11C] choline positron emission tomography/computed tomography compared with conventional computed tomography in lymph node staging of patients with bladder cancer prior to radical cystectomy. Eur Urol 61(5):1031–1038
Graziani T et al (2015) 11C-choline PET/CT for restaging of bladder cancer. Clin Nucl Med 40(1):e1–e5
Gore JL et al (2009) Mortality increases when radical cystectomy is delayed more than 12 weeks: results from a surveillance, epidemiology, and end results-medicare analysis. Cancer 115(5):988–996
Sonpavde G et al (2011) Disease-free survival at 2 or 3 years correlates with 5-year overall survival of patients undergoing radical cystectomy for muscle invasive bladder cancer. J Urol 185(2):456–461
Author contribution
Parker WP was involved in protocol development, data collection, data analysis and wrote the manuscript. Ho PL was involved in data collection and edited the manuscript. Boorjian SA, Holzbeierlein JM, Kamat AM and Lee EK were involved in protocol development and edited the manuscript. Melquist JJ was involved in data collection and edited the manuscript. Thapa P was involved in data collection, data analysis and edited the manuscript. Frank I edited the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Ashish M Kamat, MD has the following disclosures: Research Funding—FKD, Heat Biologics, Photocure, Telesta Therapeutics, Merk Abott Molecular, and Pacific Edge. Consulting—Sanofi, Taris, Telesta Therapeutics, Spectrum Pharmaceuticals, Theralase, MDX Health, Merck, Abbott Molecular, Heat Biologics, and Photocure. Advisory Board—Sanofi and Theralase. The authors declare that no other potential conflicts of interest exist.
Ethical statements
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Parker, W.P., Ho, P.L., Boorjian, S.A. et al. The importance of clinical stage among patients with a complete pathologic response at radical cystectomy after neoadjuvant chemotherapy. World J Urol 34, 1561–1566 (2016). https://doi.org/10.1007/s00345-016-1801-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-016-1801-y