Abstract
Purpose
To determine whether the immunohistochemical markers survivin and E-cadherin can predict progress at initially diagnosed Ta bladder cancer.
Methods
We retrospectively searched for every initially diagnosed pTa urothelial bladder carcinoma having been treated at our single-center hospital in Germany from January 1992 up to December 2004. Follow-up was recorded up to June 2010, with recurrence or progress being the endpoints. Immunohistochemical staining and analysis of survivin and E-cadherin of the TURB specimens were performed. Outcome dependency of progression and no progression with immunohistochemical staining was analyzed using uni- and multivariate regression analysis, Kaplan–Meier analysis and uni- and multivariate Cox regression analysis.
Results
Overall, 233 patients were included. Forty-two percent of those were tumor free in their follow-up TURBs, 46 % had at least one pTa recurrence and 12 % even showed progress to at least pT1 bladder cancer. Aberrant staining of E-cadherin was found within 71 % of patients with progression in contrast to only 40 % in cases without progression (p = 0.004). Of all progressed patients, 92 % showed overexpression of survivin in their initial pTa specimen compared to 61 % without progression (p = 0.001). Kaplan–Meier analysis revealed aberrant E-cadherin staining to be associated with worse progression-free survival (PFS) (p = 0.005) as well as overexpression of survivin (p = 0.003). In multivariate Cox regression analysis, strong E-cadherin staining was an independent prognosticator for better PFS (p = 0.033) and multifocality (p = 0.046) and tumor size over 3 cm (p = 0.042) were prognosticators for worse PFS.
Conclusion
Adding the immunohistochemical markers survivin and E-cadherin could help to identify patients at risk of developing a progressive disease in initial stage pTa bladder cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Urothelial carcinoma of the bladder (UCB) is the second most common cancer of the genitourinary tract and is responsible for the death of 150,000 people annually [1, 2]. Compared to other malignancies, overall survival rates of patients with non-muscle-invasive bladder cancer (NMIBC) are distinguished. Nevertheless, recurrence rate after primary transurethral resection is about 70 % with 10–20 % of those patients having tumor progression toward muscle-invasive bladder cancer (MIBC). Despite radical cystectomy and other treatment regimen, almost half of the patients have occult distant metastases at that time, being responsible for most of UCB-specific deaths [3].
Epithelial-to-mesenchymal transformation (EMT) is a process involving cell conversion from an epithelial-to-mesenchymal phenotype by means of upregulation of mesenchymal markers and downregulation of epithelial markers with nuclear transcription factors, hence gaining mesenchymal characteristics such as motility and invasive properties [4, 5]. Besides UCB, cell lines displaying EMT phenotype have increased invasiveness and are associated with poor patient outcome regarding various tumors like breast, gastrointestinal and prostate cancer [6–8].
E-cadherin is one of the most important mediators of cell-to-cell adhesion in epithelial tissues and has important barrier functions. Besides, it maintains the phenotype and apical-base polarity of epithelial cells [9, 10]. Loss of E-cadherin and novel expression of N-cadherin/P-cadherin (cadherin switch) are among the defining features of EMT and have been reported in bladder tumorigenesis [11, 12]. Beyond that, in current literature E-cadherin expression was significantly correlated with stage and histologic grade of urothelial cancer [13].
As recently shown, survivin is another probably effective biomarker concerning the prediction of disease recurrence, progression and mortality in UCB. Survivin is a member of the inhibitor of apoptosis (IAP) family and is involved in the regulation of cell division. Its expression is correlated with aggressiveness of tumor cells, whereas its prognostic potential is additionally based on the capability to inhibit apoptosis and improving angiogenesis [14].
The lack of definite biomarkers with predictive capacity beyond grade and stage in UCB and the absence of data concerning pTa tumors in particular, lead us to investigate the prognostic significance of immunohistochemical expression of E-cadherin and survivin in stage pTa UCB—underlining its clinical importance in the process. As disease progression causes a change in the therapeutic regimen, we solely focused on progressed patients.
Materials and methods
Patient assessment
We retrospectively searched for every initially diagnosed pTa urothelial bladder carcinoma having been treated at our single-center hospital in Germany from January 1992 up to December 2004 and followed up their further clinical course up until June 2010. Only patients with either no further tumor or recurrence or progressive disease by histopathological evaluation were included in the study. This meant in detail:
-
disease free: patients with at least one further suspect lesion during follow-up that was biopsied or transurethral resected and proven to be non-malignant, e.g., cystitis, by histopathological means,
-
recurrent: patients with at least one recurrent tumor that was proven to be a stage pTa urothelial bladder carcinoma by histopathological means,
-
progredient: patients with at least one recurrent tumor that was proven to be at least a stage pT1 urothelial bladder carcinoma by histopathological means.
Patients, who probably underwent transurethral resection during follow-up regime, but not at our hospital, could not be included into the study, as well as patients without any clinical occurrence of disease if not histopathologically proven. Patients with incomplete follow-up until June 2010 were also excluded from the study.
Clinical and histopathological patient data included in the study were collected, and histopathological slides and paraffin-embedded blocks were evaluated.
Clinical treatment of patients
After transurethral resection of the bladder and histopathological diagnosis of stage pTa urothelial carcinoma, patients underwent a re-resection in cases of high-grade tumor according to the WHO classification 1973, multifocal tumors, tumors with diameter >3 cm or lack of bladder muscle in the specimen [15]. The resection technique was the same throughout the entire cohort: a transurethral resection with a cutting electrode by monopolar device. There was no immediate instillation of chemotherapy in this era, but various instillation treatment schemes were being performed in cases of high-graded (in most cases Bacillus Calmette–Guérin instillations) or multifocal tumors (e.g., instillation of Mitomycin C). After that patients were being followed up for at least 5 years with two to four urethrocystoscopies in the first year, one to four in the second, one to three in the third and one or two routine endoscopies in the fourth and fifth year, in some cases once a year thereafter depending on initial tumor grade and number of tumors as well as the follow-up course.
Immunohistochemistry: assessment and evaluation
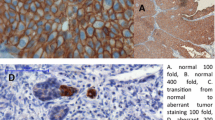
Sections of 4 µm were cut and mounted on poly-l-lysine-coated glass slides from formalin-fixed and paraffin-embedded tissue blocks. IHC analysis was carried out in a BenchMark IHC Full System immunostainer (Roche Diagnostics, Mannheim, Germany) using the avidin–biotin peroxidase method with diaminobenzidine as a chromatogen according to the manufacturer’s instructions. The primary antibodies of E-cadherin and survivin were used as shown in Fig. 1.
Expression of the markers was visualized with a Primo Star microscope (Carl Zeiss Microimaging, Jena, Germany) under 40-fold magnification. Evaluation of UCB immunostaining was performed independently by urologist and pathologist (C.G., W.O., S.S.), without knowledge of clinical and follow-up data. For both markers, E-cadherin and survivin, staining intensity was assessed as lost (0), weak (+), moderate (++) and strong (+++) in the entire slide. Aberrant E-cadherin staining was defined as any expression other than strong, and overexpression of survivin was moderate and strong straining. E-cadherin staining pattern was solely membranous, whereas survivin staining pattern was cytoplasmatic.
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics, version 21.0 (SPSS Inc, Chicago, IL, USA). Descriptive analysis was executed using SPSS Statistics to specify patient and tumor characteristics. Multivariate linear regression analysis was performed to study the association of clinicopathological parameters and expression of the IHC markers. Dependency of outcome of progression and the absence of progression with immunohistochemical staining were analyzed using uni- and multivariate analysis. Kaplan–Meier analysis and Cox regression analysis were performed to prove clinicopathological and immunohistochemical parameters regarding progression-free survival.
Results
Patient characteristics
Between January 1992 and December 2004, 1366 patients total had been diagnosed with stage pTa urothelial carcinoma of the bladder at our single-center hospital. Two hundred and twenty-three of those patients with suspect lesions of the bladder mucosa detected by endoscopy during follow-up underwent a further transurethral resection of the bladder at our institution at least once. The number of TURBs in the follow-up period until June 2010 varied between one and ten.
While 99 patients (42 %) never showed malignant findings in their follow-up TURBs, 107 patients (46 %) had at least one pTa urothelial carcinoma recurrence and 27 (12 %) patients even showed progress to at least pT1 bladder cancer.
For further data of the collective, please refer to Table 1.
Prognostic relevance of EMT markers E-cadherin and survivin for stage pTa UCB
For E-cadherin, tumor specimens of 210 patients (90 %) were suitable for immunohistochemical (IHC) evaluation and 215 tumor specimens (92 % of patients) for survivin. Aberrant or overexpressed, respectively, staining of both markers for EMT was statistically significantly associated in terms of predicting progression with (early) invasive urothelial bladder carcinoma. Seventy-one percent of patients with progression showed aberrant staining of E-cadherin in contrast to only 40 % without progression (p = 0.004). Overexpression of survivin was found in 92 % of all progressed patients in their initial pTa UCB specimen, whereas in patients without progression, survivin overexpression was found in only 61 % (p = 0.001). Please refer to Fig. 1.
Kaplan–Meier analysis revealed aberrant E-cadherin staining to be associated with statistically significant worse progression-free survival (PFS) (81 vs. 94 %, p = 0.005) as well as overexpression of survivin (81 vs. 97 %, p = 0.003). Please refer to Fig. 2.
Univariate and multivariate regression analysis for prognostic factors of progression in stage pTa UCB
Normal (strong) E-cadherin staining as a positive prognosticator (OR 0.278, CI 0.110–0.705, p = 0.007) and overexpressed survivin (OR 7.550, CI 1.733–32.90, p = 0.007) being associated with progression were the only predictive parameters in univariate regression analysis. There was also a tendency toward older age (OR 1.036, CI 0.995–1.077, p = 0.084), high-grade tumors (OR 3.083, CI 0.907–10.48, p = 0.071) and tumor size (OR 2.894, CI 0.959–8.730, p = 0.059) to predict progression, but this did not reach statistical significance. There was no independent predictive factor for progression of stage pTa bladder cancer in multivariate analysis. Please refer to Table 2.
Univariate and multivariate Cox regression analysis for prognostic factors of progression-free survival in stage pTa UCB
In multivariate Cox regression analysis, strong E-cadherin staining was an independent prognosticator for better PFS (HR 0.160, CI 0.030–0.859, p = 0.033) and multifocality (HR 4.004, CI 1.024–15.66, p = 0.046) and tumor size over 3 cm (HR 8.267, CI 1.078–63.37, p = 0.042) were prognosticators for worse PFS. Overexpression of survivin failed to be an independent prognosticator in multivariate analysis but was an independent prognosticator in univariate Cox regression analysis (HR 6.768, CI 1.599–28.64, p = 0.009). Normal (strong) staining of E-cadherin (HR 0.303, CI 0.126–0.731, p = 0.008) indicated also in this analysis for better PFS. Also poorly differentiated initial pTa UCB in WHO grading 1973 was an independent prognosticator for worse PFS in univariate Cox regression analysis. Please refer to Table 3.
Discussion
In the present study, we were able to demonstrate that overexpression of survivin is associated with progressive disease in pTa bladder cancer. This is the first study to describe survivin expression in IHC in TURB specimens of solely pTa bladder cancer. Compared to other studies, we have analyzed a major number of samples underlining the power of our data. Besides, we identified E-cadherin as a second immunohistochemical marker that predicts progressive disease in pTa bladder cancer.
In our cohort, we were able to demonstrate that overexpression of survivin is correlated with a poor PFS of patients with initial pTa bladder cancer. In univariate Cox regression analysis, overexpression of survivin was a prognosticator for poor outcome, although it did not quite reach significance in multivariate analysis. To date the majority of the studies available investigate the role of survivin in muscle-invasive bladder cancer. Survivin-positive patients have a worse response rate to chemotherapy with cisplatin, and survivin is a suitable prognostic marker in bladder cancer cystectomy specimens correlated with adverse patients’ survival [16, 17].
When Swana et al. [18] firstly described survivin in bladder cancer, they found no expression of survivin in normal epithelium but more commonly in high-grade tumors. Furthermore, missing of survivin expression was associated with longer time to first tumor recurrence. Additionally to disease recurrence, Jeon et al. [19] could demonstrate a significant association between survivin expression and bladder cancer progression as well as mortality. In their recently published review and meta-analysis, 14 studies overall were included with 2165 patients total. Almost half of the patients presented with survivin overexpression, which was associated with high-grade tumors when prevailing in higher frequencies. In these heterogeneous studies, overexpression could be identified as a significant prognosticator for oncological outcome even if no correlation with pT stage was detected [19]. Particularly in non-muscle-invasive tumors, overexpression of survivin is correlated with recurrence and progression [20–22]. Since survivin is not expressed in normal tissue and still correlates with adverse survival, it seems to be a suitable marker to identify patients at higher risk. These data correspond to the results of our study showing that survivin expression is a good prognosticator for disease progression in pTa tumors. Besides, we did not subsume pTa und pT1 tumors as found in other current literature [21].
We identified E-cadherin as a second immunohistochemical marker that predicts progressive disease in pTa bladder cancer. Loss of E-cadherin expression and cadherin switching is generally considered as a late step in the molecular pathogenesis of bladder cancer [11]. Thus, not many studies have investigated E-cadherin expression solely in pTa tumors.
For advanced bladder cancer, higher rates of loss of E-cadherin expression can be detected, indicating a more aggressive and invasive disease. In cystectomy specimens with a long-term follow-up, Byrne et al. [13] showed that altered E-cadherin expression is associated with degree of invasiveness, lymph node metastasis, disease progression and thus increased risk of death from bladder cancer.
In noninvasive tumors, a high rate of tumors with normal positive expression of E-cadherin is prevalent, whereas most invasive tumors show an abnormal expression [23]. Otto et al. [24] were among the first to show that there is a significant correlation between E-cadherin negative tumors and progress, both in pTa/T1 and in pT2–3. Furthermore, loss of E-cadherin is more frequent in high-grade tumors than in low-grade tumors [25, 26]. Thus, aberrant E-cadherin staining in pTa tumors could identify patients at higher risk of recurrence or progression. Khorrami et al. [27] showed that abnormal E-cadherin staining was associated with recurrence in low-grade papillary tumors, whereas no association between loss of E-cadherin and progression could be found. Other studies, however, did not yield a correlation between loss of E-cadherin and recurrence or progression in superficial bladder cancer [28, 29].
On molecular level, loss of E-cadherin in bladder cancer is associated with p53 expression, a well-known predictor for more aggressive urothelial cancer. In this context, loss of E-cadherin is an independent predictor of poor survival [25]. Furthermore, tumors with a high proliferative activity have a reduced E-cadherin expression [26]. This also substantiates the important role of E-cadherin in bladder cancer development. Our data demonstrate that, even in pTa tumors, aberrant E-cadherin expression is a predictor of progressive disease. Besides, advanced cancers often display an abnormal E-cadherin expression, which was associated with progression to invasive and metastatic disease. In multivariate Cox regression analysis in our cohort of pTa tumors, loss of E-cadherin as well as multifocality and tumor size (>3 cm) were the only predictors of poor outcome. Furthermore, just like overexpression of survivin, aberrant expression of E-cadherin is correlated with a poor PFS. Thus, E-cadherin seems to be a potent marker for identifying patients with pTa bladder cancer, who are at risk of progressive disease potentially resulting in a more aggressive follow-up and therapeutic regimen.
A weakness of this study is of course its retrospective design and also the fact that it only deals with single-center data. To achieve valid and reproducible results, independent multicenter studies are necessary to evaluate IHC markers.
Conclusion
For the first time, we were able to provide evidence that both survivin expression and loss of E-cadherin—known features of advanced and aggressive disease in bladder cancer—can predict progression in initial pTa bladder cancer. Adding these as immunohistochemical markers to the initial evaluation of TURB specimens, patients at risk of progressive disease might be identified more easily. Subsequently, these patients could then receive a more aggressive follow-up and therapeutic regimen with the aim of a better cancer-related survival.
References
Jemal A, Siegel R, Xu J, Ward E (2010) Cancer statistics, 2010. CA Cancer J Clin 60:277–300
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55:74–108
Sylvester RJ, van der Meijden AP, Oosterlinck W, Witjes JA, Bouffioux C, Denis L et al (2006) Predicting recurrence and progression in individual patients with stage Ta T1 bladder cancer using EORTC risk tables: a combined analysis of 2596 patients from seven EORTC trials. Eur Urol 49:466–477
Kalluri R, Weinberg RA (2009) The basics of epithelial–mesenchymal transition. J Clin Invest 119:1420–1428
van der Horst G, Bos L, van der Pluijm G (2012) Epithelial plasticity, cancer stem cells, and the tumor-supportive stroma in bladder carcinoma. Mol Cancer Res 10:995–1009
Blick T, Widodo E, Hugo H, Waltham M, Lenburg ME, Neve RM et al (2008) Epithelial mesenchymal transition traits in human breast cancer cell lines. Clin Exp Metastasis 25:629–642
Rosivatz E, Becker KF, Kremmer E, Schott C, Blechschmidt K, Höfler H et al (2006) Expression and nuclear localization of Snail, an E-cadherin repressor, in adenocarcinomas of the upper gastrointestinal tract. Virchows Arch 448:277–287
Fondrevelle M, Kantelip B, Reiter RE, Chopin DK, Thiery JP, Monnien F et al (2009) The expression of Twist has an impact on survival in human bladder cancer and is influenced by the smoking status. Urol Oncol 27:268–276
Peinado H, Olmeda D, Cano A (2007) Snail, Zeb and bHLH factors in tumour progression: an alliance against the epithelial phenotype? Nat Rev Cancer 7:415–428
Rangel MC, Karasawa H, Castro NP, Nagaoka T, Salomon DS, Bianco C (2012) Role of Cripto-1 during epithelial-to-mesenchymal transition in development and cancer. Am J Pathol 180:2188–2200
Bryan RT, Tselepis C (2010) Cadherin switching and bladder cancer. J Urol 184:423–431
Bryan RT, Atherfold PA, Yeo Y, Jones LJ, Harrison RF, Wallace DM et al (2008) Cadherin switching dictates the biology of transitional cell carcinoma of the bladder: ex vivo and in vitro studies. J Pathol 215:184–194
Byrne RR, Shariat SF, Brown R, Kattan MW, Morton RAJR, Wheeler TM et al (2001) E-cadherin immunostaining of bladder transitional cell carcinoma, carcinoma in situ and lymph node metastases with long-term followup. J Urol 165:1473–1479
Yun SJ, Kim WJ (2013) Role of the epithelial–mesenchymal transition in bladder cancer: from prognosis to therapeutic target. Korean J Urol 54:645–650
Babjuk M, Burger M, Zigeuner R, Shariat SF, van Rhijn BW, Compérat E et al (2013) EAU guidelines on non-muscle-invasive urothelial carcinoma of the bladder: update 2013. Eur Urol 64:639–653
Als AB, Dyrskjøt L, von der Maase H, Koed K, Mansilla F, Toldbod HE et al (2007) Emmprin and survivin predict response and survival following cisplatin-containing chemotherapy in patients with advanced bladder cancer. Clin Cancer Res 13:4407–4414
Shariat SF, Karakiewicz PI, Godoy G, Karam JA, Ashfaq R, Fradet Y et al (2009) Survivin as a prognostic marker for urothelial carcinoma of the bladder: a multicenter external validation study. Clin Cancer Res 15:7012–7019
Swana HS, Grossman D, Anthony JN, Weiss RM, Altieri DC (1999) Tumor content of the antiapoptosis molecule survivin and recurrence of bladder cancer. N Engl J Med 341:452–453
Jeon C, Kim M, Kwak C, Kim HH, Ku JH (2013) Prognostic role of survivin in bladder cancer: a systematic review and meta-analysis. PLoS ONE 8:e76719
Sun YW, Xuan Q, Shu QA, Wu SS, Chen H, Xiao J et al (2013) Correlation of tumor relapse and elevated expression of survivin and vascular endothelial growth factor in superficial bladder transitional cell carcinoma. Genet Mol Res 12:1045–1053
Karam JA, Lotan Y, Ashfaq R, Sagalowsky AI, Shariat SF (2007) Survivin expression in patients with non-muscle-invasive urothelial cell carcinoma of the bladder. Urology 70:482–486
Yin W, Chen N, Zhang Y, Zeng H, Chen X, He Y et al (2006) Survivin nuclear labeling index: a superior biomarker in superficial urothelial carcinoma of human urinary bladder. Mod Pathol 19:1487–1497
Sun W, Herrera GA (2002) E-cadherin expression in urothelial carcinoma in situ, superficial papillary transitional cell carcinoma, and invasive transitional cell carcinoma. Hum Pathol 33:996–1000
Otto T, Birchmeier W, Schmidt U, Hinke A, Schipper J, Rübben H et al (1994) Inverse relation of E-cadherin and autocrine motility factor receptor expression as a prognostic factor in patients with bladder carcinomas. Cancer Res 54:3120–3123
Garcia del Muro X, Torregrosa A, Muñoz J, Castellsagué X, Condom E, Vigués F et al (2000) Prognostic value of the expression of E-cadherin and beta-catenin in bladder cancer. Eur J Cancer 36:357–362
Lipponen PK, Eskelinen MJ (1995) Reduced expression of E-cadherin is related to invasive disease and frequent recurrence in bladder cancer. J Cancer Res Clin Oncol 121:303–308
Khorrami MH, Hadi M, Gharaati MR, Izadpanahi MH, Javid A, Zargham M (2012) E-cadherin expression as a prognostic factor in transitional cell carcinoma of the bladder after transurethral resection. Urol J 9:581–585
Koksal IT, Ates M, Danisman A, Sezer C, Ciftcioglu A, Karpuzoglu G et al (2006) Reduced E-cadherin and alpha-catenin expressions have no prognostic role in bladder carcinoma. Pathol Oncol Res 12:13–19
Clairotte A, Lascombe I, Fauconnet S, Mauny F, Félix S, Algros MP et al (2006) Expression of E-cadherin and alpha-, beta-, gamma-catenins in patients with bladder cancer: identification of gamma-catenin as a new prognostic marker of neoplastic progression in T1 superficial urothelial tumors. Am J Clin Pathol 125:119–126
Acknowledgments
The authors thank Mrs. Stefanie Götz for her excellent assistance in immunohistochemical procedures.
Author contributions
J Breyer wrote/edited the manuscript and analyzed the data; M Gierth wrote/edited the manuscript and developed the protocol/project; S Shalekenov, J Schäfer and C Giedl contributed to data collection or management; A Aziz analyzed the data; M Burger, S Denzinger and F Hofstädter developed the protocol/project; W Otto wrote/edited the manuscript, contributed to data collection or management, analyzed the data and developed the protocol/project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Statement of human rights
For this type of study, formal consent is not required.
Informed consent
Informed consent was obtained from all the individual participants included in the study.
Additional information
Johannes Breyer and Michael Gierth have contributed equally to the manuscript.
Rights and permissions
About this article
Cite this article
Breyer, J., Gierth, M., Shalekenov, S. et al. Epithelial–mesenchymal transformation markers E-cadherin and survivin predict progression of stage pTa urothelial bladder carcinoma. World J Urol 34, 709–716 (2016). https://doi.org/10.1007/s00345-015-1690-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-015-1690-5