Abstract
Objectives
To evaluate diagnostic yield and accuracy of image-guided core needle biopsy (ICNB) of suspected malignant osseous lesions in a large cohort of adults, evaluate what factors influence these measures, and offer technical recommendations to optimize yield.
Methods
A retrospective analysis of 2321 ICNBs performed from 2010 to 2021 was completed. The diagnostic yield and accuracy of the biopsies as well as a series of patient, lesion-related, and technical factors were retrospectively analyzed. Multivariate statistical analysis was performed to evaluate what factors were associated with yield and accuracy. Different cutoff values of total core length and core number were then tested to determine threshold values in relation to increased diagnostic yield.
Results
Diagnostic yield was 98.2% (2279/2321) and accuracy was 97.6% (120/123). Increased total core length (odds ratio [OR] = 2.34, 95% confidence interval [CI] (1.41–3.90), p = 0.001), core number (OR = 1.51, 95% CI (1.06–2.16), p = 0.02) and presence of primary malignancy (OR = 2.81, 95% CI (1.40–5.62), p = 0.004) were associated with improved yield. Lesion location in an extremity (OR = 0.27, 95% CI (0.11–0.68), p = 0.006) and using fluoroscopic imaging guidance (OR = 0.33, 95% CI (0.12–0.90), p = 0.03) were associated with lower yield. Cutoff thresholds in relation to increased diagnostic yield were found to be 20 mm total core length (marginal OR = 4.16, 95% CI = (2.09–9.03), p < 0.001), and three total cores obtained (marginal OR = 2.78, 95% CI (1.34–6.54), p = 0.005). None of the analyzed factors influenced diagnostic accuracy.
Conclusions
ICNB has a high rate of diagnostic yield and accuracy. Several factors influence diagnostic yield; 20 mm core length and three total cores optimize yield.
Clinical relevance statement
Image-guided core needle biopsy of suspected malignant osseous lesions is a safe procedure with a very high rate of diagnostic yield and accuracy. Obtaining 20 mm total core length and three total cores optimizes diagnostic yield.
Key Points
• In a retrospective cohort study, image-guided core needle biopsy of suspected osseous malignant lesions in adults was found to have very high rates of diagnostic yield and accuracy.
• Increased total core length and core number of biopsies were each associated with increased diagnostic yield, and these relationships reached thresholds at 20 mm total core length and three total cores obtained.
• The presence of a known primary malignancy was also associated with increased yield while using fluoroscopic imaging guidance and lesion location in an extremity were associated with decreased yield.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Tissue sampling is often necessary for histopathologic diagnosis, treatment planning, and subsequent management of aggressive bone tumors. Image-guided core needle biopsy (ICNB) has become an increasingly common method of tissue sampling for adult patients at many institutions, as it has been shown to be safe and effective, with a lower complication rate and cost compared to open surgical biopsy [1,2,3,4]. Diagnostic yield of ICNB is an important metric as successful diagnosis leads to timely implementation of management plans and obviates the need for repeat biopsy with accompanying cost and potential complications. Diagnostic accuracy is also important, as inaccurate biopsies can lead to inappropriate patient management and treatment.
There is heterogeneity in the literature regarding the diagnostic efficacy of ICNBs of suspected malignant osseous lesions, with values ranging from 69 to 98% for diagnostic yield, and values ranging from 73 to 98% for diagnostic accuracy [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24]. Moreover, there is divergence on the technical, lesion-related, and patient factors that influence these two measures. [11, 18,19,20]. Additionally, while it has been reported that obtaining three total core specimens optimizes the diagnostic yield of ICNBs of osseous lesions, there have been (to our knowledge) no reports focusing on the total core length that should be obtained to optimize yield [5]. While intuitively, increased lesion sampling should increase diagnostic efficacy, it also might increase procedure time, potential for complications, sedation, and exposure to ionizing radiation. A threshold value for total core length that optimizes diagnostic yield therefore serves as an important recommendation to guide radiologists during biopsies. Additional study is also needed on top of the 88 bone biopsies so far reported to accurately determine the total number of core specimens that optimize diagnostic yield [5].
The purpose of this study is to evaluate the diagnostic yield and accuracy of ICNB of suspected malignant osseous lesions in (to our knowledge) the largest cohort of adult patients thus far published, evaluate what factors influence these measures, and offer technical recommendations to optimize yield.
Materials and methods
Patient selection criteria
Institution review board approval was obtained for this Health Insurance Portability and Accountability Act–compliant retrospective study. Informed consent was waived for retrospective participation and data analysis. All consecutive patients who received an ICNB at a single tertiary care academic institution from July 2010 to October 2021 were identified using the radiology information system. Patients who received the biopsy for the sampling of suspected osteomyelitis were excluded, as additional clinical factors (such as antimicrobial exposure) could influence the diagnostic efficacy of ICNB, and evaluating these was outside the scope of the present study. Additionally, pediatric patients were excluded, as there might be limited generalizability between pediatric and adult patients due to potential differences in technical biopsy sampling as well as pathology. Lastly, lesions with classically benign appearances on prior imaging (e.g., osteoid osteoma, giant cell tumor, osteochondroma) which were biopsied immediately prior to lesion ablation were excluded, as they were sampled in very small numbers compared to the overall number of biopsies included in the study, and the overall findings of the study might not be generalizable to these lesions. This left only adult patients who were referred for biopsy for sampling of a suspected malignant lesion (based on both clinical history and prior radiologic findings) to be included. Furthermore, cases included in the study where there was subsequent surgical excision were also evaluated for diagnostic accuracy. Of this subset of patients, cases in which patients received radiation therapy or chemotherapy treatment following biopsy but prior to surgical excision of a lesion were excluded from accuracy analysis.
Patient, lesion-related, and clinical factors
For each biopsy, the following data from the procedure report and electronic medical record were documented: patient age, sex, type of lesion (lytic, sclerotic, mixed, or radiographically occult (visualized on MRI or PET/CT)), presence of a known primary malignancy, lesion anatomic location (spine, pelvis, extremity, clavicle/ribs/sternum/scapula, and skull), biopsy needle gauge, number of bone cores obtained, total core length obtained (sum length of all cores obtained, measured by the performing radiologist immediately after sample acquisition), imaging modality used (CT, fluoroscopy, or US), radiation dose, total monitored sedation time, doses of fentanyl and versed received, procedure-related complications and if the biopsy specimen was sufficient for diagnosis (histologically interpretable and adequate for diagnosis by the pathologist). Additionally, if the lesion was later surgically excised, it was recorded whether the surgical pathology from the excision was concordant with the pathology from ICNB and if any complications occurred during excision. Lesion size and extraosseous extension were not evaluated as they were absent from the majority of procedure reports and imaging was not available for analysis of earlier cases. Diagnostic yield was defined as the total number of biopsies that yielded a sufficient histopathologic diagnosis divided by the total number of biopsies. Diagnostic accuracy was defined as the number of biopsies in which the histopathologic diagnosis obtained from the biopsy was concordant with the histopathologic diagnosis of the final surgically excised specimen (which was considered the reference standard as maximal tissue is available for analysis), divided by the total number of lesions excised.
Biopsy technique
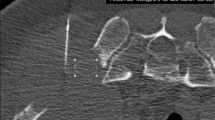
All biopsies were supervised and/or performed by a musculoskeletal radiology attending physician. The majority of the biopsies were performed by one of three attending physicians (including J.W.J., T.J.H., and J.C.B., each with 14, 12, and 12 years of post-fellowship experience respectively at the end of the study period). Greater than 90% of the biopsies were performed using a coaxial technique with the Oncontrol Needle system (Fig. 1). Once obtained, biopsy specimens were subsequently dislodged, placed in formalin with or without a bone tray, and sent for laboratory analysis (onsite histopathologic analysis was not performed). Pathologists were not blinded to clinical, procedural, or imaging data, including prior biopsy results of a lesion, during analysis of surgically excised lesions.
Images of the Oncontrol needle system used throughout the body demonstrating non-diagnostic and inaccurate biopsies. a Unenhanced axial CT image shows the outer cannula of the coaxial needle system (black arrow) and hollow biopsy needle (white arrow) traversing a lytic lesion in the T5 vertebral body. The biopsy specimen obtained was insufficient for histopathologic diagnosis. b Unenhanced axial CT image shows the outer cannula (black arrow) of the coaxial needle system as well as hollow biopsy needle (white arrow) sampling lytic lesion in the proximal humerus. This biopsy was inaccurate, as the histopathologic diagnosis from ICNB was necrosis with acute inflammation, but the histopathologic diagnosis after the lesion underwent surgical excision was necrotic metastatic adenocarcinoma. c Lateral fluoroscopy image shows the outer cannula of the coaxial needle system (black arrow) and hollow biopsy needle (white arrow) traversing the lesion in the L5 vertebral body. This biopsy was inaccurate, as the histopathologic diagnosis from ICNB was marrow fibrosis, but the histopathologic diagnosis after the lesion underwent surgical excision was Extranodal Rosai-Dorfman Disease. d Unenhanced axial CT image shows outer cannula (black arrow) of coaxial needle system as well as hollow biopsy needle (white arrow) sampling lesion in L2 spinous process. This biopsy was inaccurate, as the histopathologic diagnosis from ICNB was densely sclerotic bone with medullary fibrosis, but the histopathologic diagnosis after the lesion underwent surgical excision was metastatic pheochromocytoma
Statistical analysis
Multivariate logistic regression analysis was performed (by expert statistician C.L.) to analyze which factors (listed above) predicted diagnostic yield and accuracy using R statistical software (version 4.1.3, 2022, opensource). Factors were first tested in univariate analysis, and after backward stepwise selection, statistically significant factors were then subsequently tested in multivariate analysis to control confounding [25]. The odds ratio for categorical values was calculated in the usual fashion. For continuous values, the odds ratio represents the odds that a value produces an outcome compared to one unit less than that value. p values were obtained by the chi-square test for categorical factors, or t-test for continuous factors. A p value of < 0.05 was considered statistically significant. After multivariate analysis, different cutoff values (all values in the range of obtained data) of total core length and core number were tested and marginal odds ratios in relation to yield (odds that a biopsy above the cutoff is diagnostic compared to below the cutoff) were calculated. The statistically significant cutoff in which the marginal odds ratio plateaued was determined to optimize yield [26].
Results
Patient demographics and selection
Of the 4193 ICNBs performed on 3898 patients initially included in the study, 1872 ICNBs performed on 1719 patients were excluded per the exclusion criteria. This left 2321 ICNBs performed on 2179 patients as the study sample. Of those cases, 123 lesions that underwent ICNB in 122 patients were subsequently surgically excised and these data were used for analysis of diagnostic accuracy. See Fig. 2 for specifics regarding how many biopsies and patients were excluded for each exclusion criterion. The mean patient age was 62 years with a standard deviation of 14 years. There were 1190 male patients (54.6%) and 989 female patients (45.4%). Overall, 1491 (68.4%) of the patients had a known primary malignancy.
Diagnostic yield
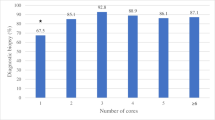
Details pertaining to lesion-related and technical factors are summarized in Table 1. Overall diagnostic yield was 98.2%, with 2279 of 2321 biopsies yielding a sufficient histopathologic diagnosis. In multivariate statistical analysis, increased total core length (odds ratio [OR] = 2.34, 95% CI (1.41–3.90), p = 0.001), core number (OR = 1.51, 95% CI (1.06–2.16), p = 0.02), and presence of primary malignancy (OR = 2.81, 95% CI (1.40–5.62), p = 0.004) were found to be associated with improved yield. Lesion location in an extremity (OR = 0.27, 95% CI (0.11–0.68), p = 0.006) and using fluoroscopic imaging guidance (OR = 0.33, 95% CI (0.12–0.90), p = 0.03) were found to be associated with lower yield. See Table 2 for univariate statistical analysis and Table 3 for multivariate statistical analysis of the factors selected after backward stepwise selection. The cutoff at which increased total core length reached a threshold value in relation to increased diagnostic yield was found to be 20 mm (marginal OR = 4.16, 95% CI = (2.09–9.03), p < 0.001) with corresponding box plot and contingency table shown in Fig. 3. The cutoff at which increased core number reached a threshold value in relation to increased yield was found to be 3 total cores obtained (marginal OR = 2.78, 95% CI (1.34–6.54, p = 0.005) with corresponding box plot and contingency table shown in Fig. 4. Marginal odds ratios of different tested cutoff values for total core length and number of cores can be seen in Table 4, and the values in this table for total core length are represented graphically in Fig. 5. The most common histopathological diagnoses of malignant lesions can be seen in supplemental Table 1 (electronic supplemental material).
a Boxplot displaying total core lengths of diagnostic and non-diagnostic biopsies, with a 20 mm total core length cutoff shown as a horizontal line on the box plot. b 2 x 2 contingency table compares diagnostic and non-diagnostic biopsies with biopsies above and below the 20mm total core length cutoff. Marginal odds ratio shown below table
a Boxplot displaying the total number of cores obtained from diagnostic and non-diagnostic biopsies, with three core cutoffs shown as a horizontal line on the box plot. b 2 x 2 contingency table compares diagnostic and non-diagnostic biopsies with biopsies above and below the three-core cutoff. Marginal odds ratio shown below table
Diagnostic accuracy
Overall diagnostic accuracy was 97.6%, with pathology from the initial bone biopsy specimen being concordant with the surgically excised specimen in 120 of 123 lesions. The sensitivity of ICNB diagnosing malignancy was 97.9% (93/95, 95% CI (92.6–99.7%)) and specificity was 100% (28/28, 95% CI (87.7–100%)) (Fig. 6). No analyzed factors were found to be statistically significant predictors of accuracy. Specific histopathologic diagnoses in nonconcordant biopsies are also provided in Table 5.
Complications
Complications were documented in 0.5% (12/2321) of biopsies. In seven biopsies, patients experienced hematomas and three patients experienced pneumothoraces, all without change in hemodynamic status. One patient experienced a foot drop after a sacral biopsy and the patient was lost to follow-up. In one patient the needle tip fractured and a 1.7 cm needle fragment was embedded in the bone. Complications from surgical excision were experienced in 0.8% (1/123) of patients, in which the patient experienced an intraoperative femur fracture.
Discussion
In the literature, estimates of diagnostic yield and accuracy of ICNB of suspected malignant osseous lesions are relatively divergent, there is heterogeneity concerning which factors influence these measures, and few studies offer technical recommendations to optimize diagnostic yield [5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23,24]. By examining a large cohort of patients, our study aimed to evaluate diagnostic yield and accuracy, further expand upon what factors influence these measures, and offer technical recommendations that operators may use to optimize the diagnostic yield of biopsies. We found diagnostic yield and accuracy to be 98.2% (2279/2321) and 97.6% (120/123) respectively and found that increased total core length, core number, and presence of primary malignancy were associated with improved yield, while lesion location in an extremity and using fluoroscopic imaging guidance were associated with lower yield. We also found that obtaining a total core length of 20 mm and three total cores optimized diagnostic yield.
The values we obtained for diagnostic yield and accuracy are on the higher end of those reported in the literature. In relatively older studies, Yang et al (in an analysis of 508 biopsies) reported yield to be 91%, Omura et al (in an analysis of 444 biopsies) reported yield to be 71%, and Sung et al (in an analysis of 309 biopsies) reported yield to be 92% [19, 20, 24]. Notably, M Wu et al (in an analysis of 96 biopsies) also reported a yield of 98% [7]. In more contemporary studies, Yang et al (in an analysis of 247 biopsies) reported yield to be 80%, and Kirhira et al (in an analysis of 585 biopsies) reported yield to be 82% [6, 17]. M Wu et al and Yang et al both reported a diagnostic accuracy of 98%, similar to our study results [7, 24]. Other studies, however, report lower accuracy values than what we found in our current study. Sung et al reported accuracy to be 84%, Omura et al reported accuracy to be 86%, and Rimondi et al (in an analysis of 430 biopsies) reported accuracy to be 93% [19, 20, 22].
Open surgical biopsy has long been considered the reference standard for tissue acquisition of bone tumors [27]. Given the low complication rate, a vast number of biopsies included, and very high rates of diagnostic accuracy and yield found in this study however, we believe that our study results suggest that ICNB could be considered the gold standard and preferential method of tissue sampling for suspected malignant osseous lesions. The most notable benefits of ICNB versus open biopsy are the reduced cost and complication rate [1,2,3,4]. Other studies have also reported no statistically significant difference in diagnostic accuracy between ICNB and open biopsy for bone tumors, and further support the implementation of ICNB over open biopsy [3, 28].
Identifying factors associated with diagnostic yield might identify ways in which to improve yield. Increased core number and total core length being positively associated with increased yield is an intuitively expected result; however, in the literature, it has not always been replicated. J Wu et al produced similar results to our study and found that an increased number of cores and total core length were associated with improved diagnostic yield [5]. In larger retrospective studies, however, Yang et al found no difference in diagnostic yield with increased core number, and Li et al found no difference with increased total core length [6, 16]. Our study did not find an association between needle gauge and yield and is concordant with other studies in the literature in this regard [5, 16].
The only other positive predictor of diagnostic yield found in our study was the presence of a known primary malignancy. A similar result has been obtained by Hwang et al who reported that cancer history is associated with increased yield [10]. This association might be due to the known primary malignancy lowering the quality of specimens needed by the pathologist to diagnose metastatic lesions.
The two factors found in our study to be associated with lower yield were fluoroscopic imaging guidance and lesion location in an extremity. Several smaller studies have reported no difference between CT and fluoroscopic imaging guidance but might have been underpowered to detect such a difference [6, 19, 20]. Compared to CT guidance, fluoroscopic guidance might decrease yield due to its limited visualization of small lesions [21]. However, in larger lesions with complete marrow replacement, fluoroscopic guidance would not seem to be inferior to CT guidance. Furthermore, fluoroscopic guidance may improve procedure efficiency and decrease ionizing radiation exposure, and operators should weigh these factors when choosing which imaging modality to use [21]. In this study, CT guidance was primarily utilized to provide better soft tissue visualization and was used for lesions in which the biopsy tract ran adjacent to sensitive soft tissue structures. For lesions in anatomic areas without important adjacent soft tissue structures (such as the feet or lumbar spine), fluoroscopic guidance was generally favored.
Yang et al reported a similar result to our finding that lesion location in an extremity decreases yield and reported that elbow and forearm lesions had lower yield compared to other central locations [24]. Other studies in which lesions were grouped into peripheral and central lesions, however, found no association between lesion location and yield [16, 20]. Lesions in extremities might have decreased yield by having a greater relative proportion of cortex to the medulla, making them technically harder to sample.
Notably in our study, we did not find that lytic lesions increased yield, similar to the results reported by Omura et al [20]. Several other studies in the literature however have reported lytic lesions to have increased yield [5, 6, 16].
While our study has shown that increased lesion sampling via increased core number and total core length increases diagnostic yield, increased sampling ostensibly also increases procedure time and might increase the potential for complications, sedation, and exposure to ionizing radiation. Thus, obtaining threshold values for the core number and total core length at which diagnostic yield plateaus is important. The only study in the literature that has focused on optimizing technical parameters for bone biopsy (to our knowledge) has been the study by J Wu et al, who in an analysis of 88 bone biopsies, reported that diagnostic yield reached a plateau at three total cores obtained [5]. Our current study of 2321 biopsies has replicated this finding. Additionally (to our knowledge), no other studies in the literature have investigated the total core length that optimizes diagnostic yield. We found that the relationship between increased total core length and increased yield starts to plateau at 20 mm. Thus, we recommend that for bone biopsies of suspected malignant lesions, operators should attempt to obtain three cores and 20 mm total core length to optimize diagnostic yield.
Our study did not find any factors that influenced diagnostic accuracy. However, due to the relatively small sample size of lesions included in the accuracy analysis, it is possible this analysis was underpowered. Other study limitations include that the study reflects the experience of only one academic institution, and thus demographics of the population, biopsy referring patterns, and preferential use of certain equipment or imaging modalities might not reflect the diversity of clinical practice. Additionally, patients were not randomized, and some data such as lesion size and extraosseous extension were unavailable. Furthermore, there might be relatively limited generalizability of the study results for primary osseous malignancy as only 2.2% of the lesions included in the study were malignant primary bone tumors.
Additionally, the lack of information regarding whether patients were oligometastatic or had diffuse disease might affect the diagnostic yield/accuracy if the majority of patients had multiple lesions to choose from. Lastly, operator heterogeneity of the radiologists who performed the biopsies might have confounded results.
In conclusion, image-guided core needle biopsy is a safe procedure with a very high rate of diagnostic yield and accuracy. Our study results suggest ICNB could be considered the preferential method for tissue acquisition in suspected malignant osseous lesions. Increased total core length, core number, and presence of primary malignancy are associated with improved yield, while lesion location in an extremity and using fluoroscopic imaging guidance are associated with lower yield. We recommend that operators attempt to obtain a total core length of at least 20 mm and three total cores to optimize diagnostic yield.
Abbreviations
- CI:
-
Confidence Interval
- ICNB:
-
Image-guided core needle biopsy
- IQR:
-
Interquartile range
- OR:
-
Odds ratio
- R:
-
Range
References
Veltri A, Bargellini I, Giorgi L, Almeida P, Akhan O (2017) CIRSE guidelines on percutaneous needle biopsy (PNB). Cardiovasc Inter Radiol 40(10):1501–1513
Welker JA, Henshaw RM, Jelinek J, Shmookler BM, Malawer MM (2000) The percutaneous needle biopsy is safe and recommended in the diagnosis of musculoskeletal masses. Cancer 89(12):2677–86
Traina F, Errani C, Toscano A et al (2015) Current concepts in the biopsy of musculoskeletal tumors: AAOS exhibit selection. J Bone Joint Surg Am 97(2):e7
Fraser-Hill MA, Renfrew DL, Hilsenrath PE (1992) Percutaneous needle biopsy of musculoskeletal lesions. 2. Cost-effectiveness. AJR Am J Roentgenol 158(4):813–8
Wu JS, Goldsmith JD, Horwich PJ, Shetty SK, Hochman MG (2008) Bone and soft-tissue lesions: what factors affect diagnostic yield of image-guided core-needle biopsy? Radiology 248(3):962–70
Yang SY, Oh E, Kwon JW, Kim HS (2018) Percutaneous image-guided spinal lesion biopsies: factors affecting higher diagnostic yield. AJR Am J Roentgenol 211(5):1068–1074
Wu MH, Xiao LF, Liu HW et al (2019) PET/CT-guided versus CT-guided percutaneous core biopsies in the diagnosis of bone tumors and tumor-like lesions: which is the better choice? Cancer Imaging 19(1):69
Hillen TJ, Talbert RJ, Friedman MV et al (2017) Biopsy of CT-occult bone lesions using anatomic landmarks for CT guidance. AJR Am J Roentgenol 209(1):214–221
Chang IJ, Ilaslan H, Sundaram M, Schils J, Subhas N (2018) CT-guided percutaneous biopsy of sclerotic bone lesions: diagnostic outcomes. Skeletal Radiol 47(5):661–669
Hwang S, Lefkowitz RA, Landa J et al (2011) Percutaneous CT-guided bone biopsy: diagnosis of malignancy in lesions with initially indeterminate biopsy results and CT features associated with diagnostic or indeterminate results. AJR Am J Roentgenol 197(6):1417–25
Suh CH, Yun SJ (2019) Diagnostic outcome of image-guided percutaneous core needle biopsy of sclerotic bone lesions: a meta-analysis. AJR Am J Roentgenol 212(3):625–631
Datir A, Pechon P, Saifuddin A (2009) Imaging-guided percutaneous biopsy of pathologic fractures: a retrospective analysis of 129 cases. AJR Am J Roentgenol 193(2):504–8
Yao L, Nelson SD, Seeger LL, Eckardt JJ, Eilber FR (1999) Primary musculoskeletal neoplasms: effectiveness of core-needle biopsy. Radiology 212(3):682–6
Jelinek JS, Murphey MD, Welker JA et al (2002) Diagnosis of primary bone tumors with image-guided percutaneous biopsy: experience with 110 tumors. Radiology 223(3):731–7
Altuntas AO, Slavin J, Smith PJ et al (2005) Accuracy of computed tomography guided core needle biopsy of musculoskeletal tumours. ANZ J Surg 75(4):187–91
Li Y, Du Y, Luo TY et al (2014) Factors influencing diagnostic yield of CT-guided percutaneous core needle biopsy for bone lesions. Clin Radiol 69(1):e43-7
Kihira S, Koo C, Lee A, Aggarwal A, Pawha P, Doshi A (2020) Reduction of radiation dose and scanning time while preserving diagnostic yield: a comparison of battery-powered and manual bone biopsy systems. AJNR Am J Neuroradiol 41(3):387–392
Kubo T, Furuta T, Johan MP, Sakuda T, Ochi M, Adachi N (2018) A meta-analysis supports core needle biopsy by radiologists for better histological diagnosis in soft tissue and bone sarcomas. Medicine (Baltimore) 97(29):e11567
Sung KS, Seo SW, Shon MS (2009) The diagnostic value of needle biopsy for musculoskeletal lesions. Int Orthop 33(6):1701–6
Omura MC, Motamedi K, UyBico S, Nelson SD, Seeger LL (2011) Revisiting CT-guided percutaneous core needle biopsy of musculoskeletal lesions: contributors to biopsy success. AJR Am J Roentgenol 197(2):457–61
Tomasian A, Hillen TJ, Jennings JW (2020) Bone biopsies: what radiologists need to know. AJR Am J Roentgenol 215(3):523–533
Rimondi E, Staals EL, Errani C et al (2008) Percutaneous CT-guided biopsy of the spine: results of 430 biopsies. Eur Spine J 17(7):975–81
Cohen MG, McMahon CJ, Kung JW, Wu JS (2016) Comparison of battery-powered and manual bone biopsy systems for core needle biopsy of sclerotic bone lesions. AJR Am J Roentgenol 206(5):W83-6
Yang J, Frassica FJ, Fayad L, Clark DP, Weber KL (2010) Analysis of nondiagnostic results after image-guided needle biopsies of musculoskeletal lesions. Clin Orthop Relat Res 468(11):3103–11
Agresti A (2019) Building and Applying Logistic Regression Models. An introduction to categorical data analysis. 2nd ed. 137–63
Harrell F (2015) Ordinal Logistic Regression. Regression modeling strategies: with applications to linear models, logistic and ordinal regression, and survival analysis. 2nd ed. 311–24
Bickels J, Jelinek JS, Shmookler BM, Neff RS, Malawer MM (2019) Biopsy of musculoskeletal tumors Current concepts. Clin Orthop Relat Res 368:212–9
Pohlig F, Kirchhoff C, Lenze U et al (2012) Percutaneous core needle biopsy versus open biopsy in diagnostics of bone and soft tissue sarcoma: a retrospective study. Eur J Med Res 17(1):29
Funding
Funding was provided to W.W. by the Washington University in St. Louis School of Medicine Dean’s Medical Student Research Fellowship
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jack Jennings.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Chongliang Luo, an expert statistician, kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Study subjects or cohorts overlap
Around 300 biopsies overlap with the below study:
Wallace AN, McWilliams SR, Wallace A, Chang RO, Vaswani D, Stone RE, Berlin AN, Liu KX, Gilcrease-Garcia B, Madaelil TP, Shoela RA, Hillen TJ, Long J, Jennings JW. Drill-Assisted Biopsy of the Axial and Appendicular Skeleton: Safety, Technical Success, and Diagnostic Efficacy. J Vasc Interv Radiol. 2016 Oct;27(10):1618-22. doi: 10.1016/j.jvir.2016.05.036. PMID: 27670996.
Methodology
• retrospective
• observational
• performed at one institution
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Winkler, W.L., Baker, J.C., Tomasian, A. et al. Diagnostic efficacy of image-guided core needle biopsy of suspected malignant osseous lesions: a retrospective cohort study from a single academic institution. Eur Radiol 34, 5760–5772 (2024). https://doi.org/10.1007/s00330-024-10663-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-024-10663-1