Abstract
Objectives
To evaluate the correlation between simple planimetric measurements in axial computed tomography (CT) slices and measurements of patient body composition and anthropometric data performed with bioelectrical impedance analysis (BIA) and metric clinical assessments.
Methods
In this prospective cross-sectional study, we analyzed data of a cohort of 62 consecutive, untreated adult patients with advanced malignant melanoma who underwent concurrent BIA assessments at their radiologic baseline staging by CT between July 2016 and October 2017. To assess muscle and adipose tissue mass, we analyzed the areas of the paraspinal muscles as well as the cross-sectional total patient area in a single CT slice at the height of the third lumbar vertebra. These measurements were subsequently correlated with anthropometric (body weight) and body composition parameters derived from BIA (muscle mass, fat mass, fat-free mass, and visceral fat mass). Linear regression models were built to allow for estimation of each parameter based on CT measurements.
Results
Linear regression models allowed for accurate prediction of patient body weight (adjusted R2 = 0.886), absolute muscle mass (adjusted R2 = 0.866), fat-free mass (adjusted R2 = 0.855), and total as well as visceral fat mass (adjusted R2 = 0.887 and 0.839, respectively).
Conclusions
Our data suggest that patient body composition can accurately and quantitatively be determined by using simple measurements in a single axial CT slice. This could be useful in various medical and scientific settings, where the knowledge of the patient’s anthropometric parameters is not immediately or easily available.
Key Points
• Easy to perform measurements on a single CT slice highly correlate with clinically valuable parameters of body composition.
• Body composition data were acquired using bioelectrical impedance analysis to correlate CT measurements with a non-imaging-based method, which is frequently lacking in previous studies.
• The obtained equations facilitate a quick, opportunistic assessment of relevant parameters of body composition.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The individual body composition is an important factor in various clinical scenarios. For example, in emergency care, accurate assessments of body weight would be helpful to correctly calculate dosage of urgent medications and anesthetics [1,2,3,4]. However, determining a patient’s body weight in the emergency department may be challenging, as patients might be unresponsive and attending medical professionals often lack the time and technical resources to assess body weight in this setting [3, 5, 6].
On the other hand, obesity has been shown to influence clinical outcomes in patients with diabetes, cancer, and viral infections [7,8,9]. More importantly, it has been shown that sarcopenia and sarcopenic obesity are independent risk factors for patient survival and postoperative complications [10,11,12,13,14,15]. In contrast to the obvious impact of body composition on human diseases, its assessment is usually not included in routine clinical workup of cancer patients.
Bioelectrical impedance analysis (BIA) represents a widely used method to assess body composition in patients under various clinical conditions including nutritional intervention or fluid management [16,17,18,19,20]. However, the consistency and reproducibility of BIA-generated data significantly depend on correct measurements and preparation of the patient (fasted state, lack of liquid reservoirs, hormonal cycle in women, etc.). The method therefore demands for prepared integration into clinical routine, but if conducted correctly, BIA data are consistent and highly reproducible [21, 22]. Other established methods to determine body composition comprise computed tomography (CT), magnetic resonance imaging (MRI), and dual-energy X-ray absorptiometry (DEXA). In contrast to BIA, the usage of CT and DEXA is hampered due to time or adverse effects of radiation exposure [16].
Given the widespread and frequent usage of computed tomography (CT) in oncological or emergency medicine settings in clinical routine, information about body composition is generated with CT, but not evaluated on a regular basis. Clinically indicated CT scans could therefore serve as a valuable source for anthropometric and metabolic assessments. Previous studies have shown that the determination of total body muscle status is possible by segmentation of skeletal muscles at the height of the third lumbar vertebra [13, 23, 24]. However, in contrast to the usage of surrogate parameters such as the skeletal muscle index (corresponding to muscle area at the third lumbar vertebra divided by the patient’s height squared), correlations between measurements on a single CT slice and non-imaging-based assessment of a patient’s total muscle or fat tissue mass are lacking in previous studies. Thus, the purpose of this study was to analyze if clinical anthropometric measures and body composition data derived from BIA measurements, as well as clinical anthropometric data, can be correctly estimated from simple and reliable 2D measurements in routine CT scans and to provide corresponding linear regression models.
Materials and methods
Patient collective
Between July 2016 and October 2017, 62 consecutive melanoma patients admitted to our comprehensive cancer center (Center of Integrated Oncology, University Hospital Cologne, Germany) were included into this prospective analysis. All patients were evaluated per standard protocol with regard to clinical and radiologic staging at initial diagnosis and received additional nutritional status assessment including BIA-derived body composition analysis. Written informed consent was obtained from every patient and the study was approved by the institutional review board (No. 16-239, University of Cologne).
Anthropometric and bioelectrical impedance analyses
BIA assessments were performed in overnight-fasted patients within the morning hours using a multi-frequency BIA device (Seca mBCA 515, Seca). Tetrapolar measurements of bioelectrical impedance were performed in an upright position of the patient at 19 frequencies ranging from 1 kHz to 1 MHz [25, 26]. Anthropometric clinical data (body weight, height, and waist circumference) were determined by an integrated scale and standard measures.
CT image acquisition
All CT scans were conducted as required for the patients’ oncological management and for routine clinical indications. The acquisitions were performed on three different CT scanners: Philips iCT 256, Philips IQon, and Philips Brilliance 64 (Philips Healthcare), according to the institutions’ standard imaging protocols (contrast enhanced, portal venous phase). Eight patients received unenhanced examinations due to renal failure.
All images used in further evaluation for the purpose of this study were reconstructed in axial plane with a slice thickness of 2 mm and an increment of 1 mm using a hybrid-iterative reconstruction algorithm and a soft tissue reconstruction kernel (iDose 4, level 3, Philips Healthcare).
CT measurements
All measurements were performed by one radiologist (reader 1, DZ, 3 years of experience in abdominal radiology) within the standard DICOM viewing software used in our institution (Impax EE R20, XVII SU1, Agfa Healthcare). The third lumbar vertebra was identified in the sagittal plane and measurements were then subsequently carried out on an axial plane located at the center of the third lumbar vertebra. With the help of a freehanded tool, regions of interest (ROI) were drawn to determine the circumference and the area of the following regions at the aforementioned height: psoas muscles, autochthonous spine muscles, and total cross-sectional area of the patient’s body (see Fig. 1). The sum of the individual muscle areas was defined as total paraspinal muscle area.
Example of CT measurements on an axial slice using a freehanded tool to determine the area and circumference of the whole body cross-sectional (green), the area of psoas muscles (red), and the area of the autochthonous muscles (yellow). Regions of interest (ROI) are displayed, providing the area (A) in square millimeters (mm2) and the circumference (U) in millimeters (mm)
To evaluate intrareader reliability, measurements were repeated in 15 randomly selected CT scans by reader 1 after a period of 6 weeks to avoid recall bias. Interreader variability was assessed using measurements performed by a second radiologist (reader 2, NGH, 4 years of experience in abdominal radiology) in 15 randomly selected CT scans.
Statistics
Statistical analysis was performed using R 3.6.0 with RStudio 1.2.1335 [27]. Figures were plotted using the ggplot2 package [28]. Linear regression models for prediction of body weight, muscle mass, total fat mass, visceral fat mass, and fat-free mass were built using the lm() function and a manual exhaustive search. To indicate goodness of fit, adjusted R2 values are provided. Concordance correlation coefficients were used to measure intra- and interreader reliability. Continuous variables are reported as mean ± standard deviation (SD). Statistical significance was defined as p ≤ 0.05.
Results
Patient characteristics
Of the 62 included patients, 31 were male (median age 73 (30–85) years) and 31 were female (median age 60 (31–90) years). All CT and BIA scans were performed before treatment initiation. Detailed patient characteristics are shown in Table 1.
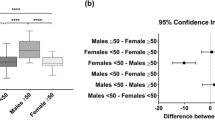
Correlation BIA results and CT parameters
By using patient gender (encoded as 0 for female and1 for male), patient body height, and the CT measurements as potential input variables to our models, we were able to fit linear regression models that allowed for the best possible estimation of patient’s total body weight, muscle mass, total fat mass, visceral fat mass, and fat-free body mass (Figs. 2 and 3).
a Multivariate regression analysis of predicted fat mass and fat mass measured with bioelectrical impedance analysis (BIA) in kilogram (kg). b Multivariate regression analysis of predicted fat-free mass and fat-free mass measured with BIA in kg. c Multivariate regression analysis of predicted visceral fat mass and visceral fat mass measured with BIA in kg
Patient’s total body weight was best estimated using only the patients total cross-sectional body area as input variable for the linear regression model (adjusted R2 0.886, p < 0.001):
For the estimation of the patient’s muscle mass, the following model yielded the best performance (adjusted R2 0.866, p < 0.001):
Optimal linear regression models were found for total fat mass (adjusted R2 0.887, p < 0.001), visceral fat mass (adjusted R2 0.839, p < 0.001), and fat-free mass (adjusted R2 0.855, p < 0.001), respectively:
Estimates and their respective 95% confidence intervals can be found in Table 2. All CT measurement showed excellent intra- and interreader reliability (Table 3).
Discussion
Various approaches have been described to assess body composition with CT scans: manual or (semi-) automated muscle segmentation, attenuation-based methods, and volumetric methods [29, 30]. Commonly, muscle segmentation is carried out at the height of the third lumbar vertebra. At this landmark, the cross-sectional muscle area has been suggested to have a linear relation to the patient’s overall muscle mass [13, 31, 32]. However, to be included in the daily clinical routine, simple and reliable measurements are needed. In addition, most approaches using CT and MRI to assess body composition are commonly not compared with non-imaging-based methods, such as BIA and DEXA. This prospective study meets these needs and investigated to which extend simple measurements in axial CT slices can accurately predict parameters of body composition obtained from BIA. We found a strong correlation between patient weight and total lumbar cross-sectional area, whereby patient weight could precisely be predicted using a linear regression model. Similarly, the patient’s muscle mass and fat mass could be predicted in multivariate linear regression models with simple equations.
Previous studies were able to show significant correlations between single-slice measurements and compartment volumes, such as paraspinal muscle or adipose tissue volumes [29, 32]. Our results are in line with a study from Geraghty et al who determined important anthropometric parameters from a single CT slice [33]. However, these studies did not correlate their findings to other established methods, such as BIA, as they only compare imaging-based parameters among each other [29, 32, 34]. To the best of our knowledge, this is the first study to compare single-slice measurements to a non-imaging-based reference standard. A straightforward determination of essential parameters of body composition, such as patient weight and muscle mass, is essential in the field of sarcopenia, which has received growing attention as a potential predictor of adverse outcomes after surgical interventions or overall survival [10, 14, 15, 35]. Sarcopenia and sarcopenic obesity show a clear association with poorer overall survival in various malignant diseases [36,37,38]. Due to the aging population worldwide, the role of sarcopenia will play an increasingly important role in patient care [12, 15]. Besides, a fast and reliable determination of patient weight might be very beneficial in different clinical and scientific settings, such as drug dosing in polytrauma patients or in a retrospective assessment of weight in closed prospective trials. Currently, the skeletal muscle index is frequently used to depict sarcopenia and is computed by the ratio of muscle area to body height (cm2/m2) [23]. The parameters available through the presented regression models could hold the potential to provide a more accurate, realistic representation of sarcopenia, for example, the ratio of muscle mass to body weight.
As automated segmentation of anatomical structures and pathologies continues to improve and with the recent advent of artificial intelligence, first automated approaches to assess muscle areas in CT have been reported [39,40,41]. However, these approaches are not widespread and manual validation is mandatory.
This study has several limitations that need to be considered. First, the estimation of body composition with BIA is potentially susceptible to mistakes, as a standardization of measurements and patient preparation is indispensable. Especially in patients with fluid shifts or regarding the determination of intra-abdominal fat, the accuracy of BIA seems to be limited in comparison with other established methods, such as DEXA or MRI [42, 43]. However, it can be argued that small statistical differences between BIA and other methods might not be of clinical relevance [18]. Since we only included patients with malignant melanoma, a selection bias cannot be ruled out. The proposed equations to estimate parameters of body composition require the cross-sectional area and muscle area at a certain height; therefore, this approach is limited to patients who undergo a CT of the abdomen or a whole-body scan. Furthermore, an additional validation, potentially in a larger patient collective, may be necessary. Manual measurements are likely prone to a higher inter- or intrareader variability in comparison with (semi-)automated measurements. However, we found an excellent intra- and interreader agreement, most probably due to the simplicity of the measurements.
In conclusion, parameters of body composition with high clinical relevance can accurately be determined in clinical examinations by using simple measurements in a single axial CT slice. By routinely providing such measurements, radiology could strengthen its role in delivering personalized medicine through providing clinical target parameters with only little additional effort.
Abbreviations
- BIA:
-
Bioelectrical impedance analysis
- CI:
-
Confidence interval
- CT:
-
Computed tomography
- DEXA:
-
Dual-energy X-ray absorptiometry
- MRI:
-
Magnetic resonance imaging
- SD:
-
Standard deviation
References
Bae KT, Tao C, Gürel S et al (2007) Effect of patient weight and scanning duration on contrast enhancement during pulmonary multidetector CT angiography. Radiology 242(2):582–589
Fernandes CM, Clark S, Price A, Innes G (1999) How accurately do we estimate patients’ weight in emergency departments? Can Fam Physician 45:2373–2376
Lorenz MW, Graf M, Henke C et al (2007) Anthropometric approximation of body weight in unresponsive stroke patients. J Neurol Neurosurg Psychiatry 78(12):1331–1336
Gascho D, Ganzoni L, Kolly P et al (2017) A new method for estimating patient body weight using CT dose modulation data. Eur Radiol Exp 1(1):23
Cubison TC, Gilbert PM (2005) So much for percentage, but what about the weight? Emerg Med J 22(9):643–645
Leary TS, Milner QJ, Niblett DJ (2000) The accuracy of the estimation of body weight and height in the intensive care unit. Eur J Anaesthesiol 17(11):698–703
Gallagher D, Kelley DE, Yim JE et al (2009) Adipose tissue distribution is different in type 2 diabetes. Am J Clin Nutr 89(3):807–814
Scherzer R, Shen W, Bacchetti P et al (2008) Comparison of dual-energy X-ray absorptiometry and magnetic resonance imaging-measured adipose tissue depots in HIV-infected and control subjects. Am J Clin Nutr 88(4):1088–1096
Buckley RG, Stehman CR, Dos Santos FL et al (2012) Bedside method to estimate actual body weight in the emergency department. J Emerg Med 42(1):100–104
Jang M, Park HW, Huh J et al (2018) Predictive value of sarcopenia and visceral obesity for postoperative pancreatic fistula after pancreaticoduodenectomy analyzed on clinically acquired CT and MRI. Eur Radiol. https://doi.org/10.1007/s00330-018-5790-7
Faron A, Pieper CC, Schmeel FC et al (2019) Fat-free muscle area measured by magnetic resonance imaging predicts overall survival of patients undergoing radioembolization of colorectal cancer liver metastases. Eur Radiol. https://doi.org/10.1007/s00330-018-5976-z
Lenchik L, Boutin RD (2018) Sarcopenia: beyond muscle atrophy and into the new frontiers of opportunistic imaging, precision medicine, and machine learning. Semin Musculoskelet Radiol 22(3):307–322
Shachar SS, Williams GR, Muss HB, Nishijima TF (2016) Prognostic value of sarcopenia in adults with solid tumours: a meta-analysis and systematic review. Eur J Cancer 57:58–67
Chang KV, Chen JD, Wu WT, Huang KC, Hsu CT, Han DS (2018) Association between loss of skeletal muscle mass and mortality and tumor recurrence in hepatocellular carcinoma: a systematic review and meta-analysis. Liver Cancer 7(1):90–103
Sconfienza LM (2019) Sarcopenia: ultrasound today, smartphones tomorrow? Eur Radiol 29(1):1–2
Sergi G, de Rui M, Stubbs B, Veronese N, Manzato E (2017) Measurement of lean body mass using bioelectrical impedance analysis: a consideration of the pros and cons. Aging Clin Exp Res 29(4):591–597
Lemos T, Gallagher D (2017) Current body composition measurement techniques. Curr Opin Endocrinol Diabetes Obes 24(5):310–314
Ward LC (2019) Bioelectrical impedance analysis for body composition assessment: reflections on accuracy, clinical utility, and standardisation. Eur J Clin Nutr 73(2):194–199
Kuriyan R (2018) Body composition techniques. Indian J Med Res 148(5):648–658
Gonzalez MC, Heymsfield SB (2017) Bioelectrical impedance analysis for diagnosing sarcopenia and cachexia: what are we really estimating? J Cachexia Sarcopenia Muscle 8(2):187–189
Chula de Castro JA, Lima TR, Silva DAS (2018) Body composition estimation in children and adolescents by bioelectrical impedance analysis: a systematic review. J Bodyw Mov Ther 22(1):134–146
Chien MY, Huang TY, Wu YT (2008) Prevalence of sarcopenia estimated using a bioelectrical impedance analysis prediction equation in community-dwelling elderly people in Taiwan. J Am Geriatr Soc 56(9):1710–1715
Prado CM, Lieffers JR, McCargar LJ et al (2008) Prevalence and clinical implications of sarcopenic obesity in patients with solid tumours of the respiratory and gastrointestinal tracts: a population-based study. Lancet Oncol 9(7):629–635
Derstine BA, Holcombe SA, Ross BE, Wang NC, Su GL, Wang SC (2018) Skeletal muscle cutoff values for sarcopenia diagnosis using T10 to L5 measurements in a healthy US population. Sci Rep 8(1):11369
Thurlow S, Taylor-Covill G, Sahota P, Oldroyd B, Hind K (2018) Effects of procedure, upright equilibrium time, sex and BMI on the precision of body fluid measurements using bioelectrical impedance analysis. Eur J Clin Nutr 72(1):148–153
Bosy-Westphal A, Jensen B, Braun W, Pourhassan M, Gallagher D, Müller MJ (2017) Quantification of whole-body and segmental skeletal muscle mass using phase-sensitive 8-electrode medical bioelectrical impedance devices. Eur J Clin Nutr 71(9):1061–1067
R Core Team (2014) R: A language and environment for statistical computing; Available via Available via: http://www.r-project.org/
Wickham H (2009) ggplot2: An implementation of the Grammar of Graphics. Available via Available via http://ggplot2.tidyverse.org/
Faron A, Luetkens JA, Schmeel FC, Kuetting DLR, Thomas D, Sprinkart AM (2019) Quantification of fat and skeletal muscle tissue at abdominal computed tomography: associations between single-slice measurements and total compartment volumes. Abdom Radiol (NY) https://doi.org/10.1007/s00261-019-01912-9
Kamiya N, Li J, Kume M, Fujita H, Shen D, Zheng G (2018) Fully automatic segmentation of paraspinal muscles from 3D torso CT images via multi-scale iterative random forest classifications. Int J Comput Assist Radiol Surg 13(11):1697–1706
Kazemi-Bajestani SM, Mazurak VC, Baracos V (2016) Computed tomography-defined muscle and fat wasting are associated with cancer clinical outcomes. Semin Cell Dev Biol 54:2–10
Shen W, Punyanitya M, Wang Z et al (2004) Total body skeletal muscle and adipose tissue volumes: estimation from a single abdominal cross-sectional image. J Appl Physiol (Bethesda 1985) 97(6):2333–2338
Geraghty EM, Boone JM (2003) Determination of height, weight, body mass index, and body surface area with a single abdominal CT image. Radiology 228(3):857–863
Irlbeck T, Massaro JM, Bamberg F, O’Donnell CJ, Hoffmann U, Fox CS (2010) Association between single-slice measurements of visceral and abdominal subcutaneous adipose tissue with volumetric measurements: the Framingham Heart Study. Int J Obes (Lond) 34(4):781–787
Lenchik L, Lenoir KM, Tan J et al (2018) Opportunistic measurement of skeletal muscle size and muscle attenuation on computed tomography predicts one-year mortality in Medicare patients. J Gerontol A Biol Sci Med Sci. https://doi.org/10.1093/gerona/gly183
Mintziras I, Miligkos M, Wächter S, Manoharan J, Maurer E, Bartsch DK (2018) Sarcopenia and sarcopenic obesity are significantly associated with poorer overall survival in patients with pancreatic cancer: Systematic review and meta-analysis. Int J Surg. https://doi.org/10.1016/j.ijsu.2018.09.014
Mei KL, Batsis JA, Mills JB, Holubar SD (2016) Sarcopenia and sarcopenic obesity: do they predict inferior oncologic outcomes after gastrointestinal cancer surgery? Perioper Med (Lond) 5:30
Deluche E, Leobon S, Desport JC, Venat-Bouvet L, Usseglio J, Tubiana-Mathieu N (2018) Impact of body composition on outcome in patients with early breast cancer. Support Care Cancer 26(3):861–868
Baum T, Lorenz C, Buerger C et al (2018) Automated assessment of paraspinal muscle fat composition based on the segmentation of chemical shift encoding-based water/fat-separated images. Eur Radiol Exp 2(1):32
Hashimoto F, Kakimoto A, Ota N, Ito S, Nishizawa S (2019) Automated segmentation of 2D low-dose CT images of the psoas-major muscle using deep convolutional neural networks. Radiol Phys Technol 12(2):210–215
Burns JE, Yao J, Chalhoub D, Chen JJ, Summers RM (2019) A machine learning algorithm to estimate sarcopenia on abdominal CT. Acad Radiol. https://doi.org/10.1016/j.acra.2019.03.011
Murphy J, Bacon SL, Morais JA, Tsoukas MA, Santosa S (2019) Intra-abdominal adipose tissue quantification by alternative versus reference methods: a systematic review and meta-analysis. Obesity (Silver Spring) https://doi.org/10.1002/oby.22494
Looijaard WGPM, Molinger J, Weijs PJM (2018) Measuring and monitoring lean body mass in critical illness. Curr Opin Crit Care 24(4):241–247
Funding
This study has received funding from the Koeln Fortune Program/Faculty of Medicine, University of Cologne (Koeln Fortune 339/2018 to N. Große Hokamp), and from the Else Kröner-Fresenius Stiftung (2016-Kolleg-19 to J. Knuever).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Daniel Pinto dos Santos.
Conflict of interest
The authors declare that they have no conflict of interest.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• cross-sectional study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Zopfs, D., Theurich, S., Große Hokamp, N. et al. Single-slice CT measurements allow for accurate assessment of sarcopenia and body composition. Eur Radiol 30, 1701–1708 (2020). https://doi.org/10.1007/s00330-019-06526-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06526-9