Abstract
Objective
To determine the diagnostic accuracy and predictive value of gadoxetic acid liver MRI (Gd-EOB-DTPA MRI) alone or in combination with diffusion-weighted imaging (DWI) as a second-line tool for detecting early hepatocellular carcinoma (HCC) recurrence in cirrhotic patients with previous HCC treated with resection or ablation.
Methods
Between 2014 and 2017, we prospectively included 34 cirrhotic patients with complete response to resection and/or ablation of early HCC in whom a new focal lesion enhancing in the arterial phase without washout was detected during follow-up with EC-MRI. After signing the informed consent, all patients underwent DWI and Gd-EOB-DTPA MRI; two readers analyzed signal intensities on each phase of dynamic study and on DWI. The final diagnosis was established by histology or follow-up EC-MRI. We used cross-tabulation to calculate indices of diagnostic accuracy.
Results
We evaluated 34 patients (7 women; 73.5% with hepatitis C virus) with a total of 53 new arterial-phase-enhancing foci (median size, 10 [IQR 9–14] mm). The final diagnosis, reached by histopathology in 15 (35.7%) lesions and EC-MR follow-up in 27 (64.3%), was HCC in 42 (79.2%) and benign conditions in 11 (21.8%). Hepatobiliary-phase hypointensity on Gd-EOB-DTPA MRI plus hyperintensity on DWI yielded 54.8% sensitivity, 90.9% specificity, 95.8% positive predictive value, and 34.5% negative predictive value for diagnosing HCC recurrence.
Conclusion
Among potential indices, combining hypointensity on hepatobiliary-phase Gd-EOB-DTPA MRI and hyperintensity on DWI has the highest specificity and positive predictive value to optimally detect HCC recurrence prior to confident diagnosis by conventional imaging criteria on EC-MRI in cirrhotic liver.
Key Points
• In patients at risk of HCC recurrence, the use of gadoxetic acid liver MRI and DWI may improve the differentiation of unspecific new arterial-enhancing foci from early hypervascular HCC recurrence in patients with non-conclusive findings on extracellular liver MRI.
• Combined findings on hepatobiliary-phase gadoxetic acid–enhanced liver MRI and DWI had high specificity (90.9%) and positive predictive value (95.8%) for detecting early hypervascular HCC recurrence, but limited sensitivity.
• Combining hepatobiliary-phase hypointensity on gadoxetic acid MRI and hyperintensity on diffusion-weighted imaging allows early diagnosis of hypervascular hepatocellular carcinoma and may help select patients for salvage therapy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Imaging assessment of tumor response after treatment is key for optimizing the management of patients with hepatocellular carcinoma (HCC). Within 5 years after surgery or ablation, HCC recurs in up to 70% of cirrhotic patients, and the rate of recurrence is particularly high during the first 2 years [1,2,3]. Early detection of HCC recurrence enables prompt salvage therapy and may improve the prognosis. Thus, these patients require close imaging follow-up. However, post-treatment cirrhotic livers often have small areas of parenchymal enhancement on arterial sequences that usually represent transient pseudolesions, but cannot be distinguished from HCC recurrence.
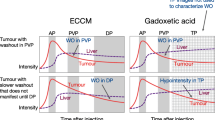
The current criteria for the non-invasive diagnosis of HCC are based on contrast enhancement in arterial phases followed by contrast washout in venous phases, using either extracellular or liver-specific contrast agents. These criteria have been endorsed by the European Association for the Study of the Liver (EASL) [4] and the American Association for the Study of Liver Diseases (AASLD) [5] and have been extensively validated in patients with newly detected nodules discovered by surveillance ultrasonography [6,7,8]. These criteria yield nearly 100% specificity for early HCC recurrence. However, small newly detected hypervascular HCCs often lack washout, so they require follow-up (delaying diagnosis in patients with recurrence) or percutaneous biopsy. Moreover, the pre-test risk of HCC is higher in the scenario of HCC recurrence than in cirrhotic patients with de novo–detected nodules [1, 2].
Growing evidence suggests that MRI using gadoxetic acid (Gd-EOB-DTPA), a hepatocyte-specific contrast agent, and diffusion-weighted imaging (DWI) can help detect focal liver lesions, but lesion characteristics in hepatobiliary-phase Gd-EOB-DTPA MRI and in DWI are not specific for HCC because of the risk of mistaking other malignancies [4, 9,10,11,12]. We hypothesized that incorporating hepatobiliary-phase characteristics alone or in combination with DWI might increase the diagnostic accuracy of MRI and might be helpful in the early detection of hypervascular HCC recurrence in clinical practice.
We aimed to determine the diagnostic accuracy and predictive value of Gd-EOB-DTPA MRI alone or in combination with DWI as a second-line tool for detecting early HCC recurrence in cirrhotic patients with previous HCC treated with resection or ablation.
Patients and methods
Patients
The institutional review board approved the study, and all patients provided written informed consent.
Between June 2014 and December 2017, we prospectively included consecutive asymptomatic patients with Child-Pugh A-B cirrhosis with a previous history of early HCC successfully treated with ablation and/or surgery in whom a new focal lesion enhancing in the arterial phase without washout was detected during follow-up with extracellular gadolinium-enhanced liver MRI (EC-MRI).
The inclusion criteria were (1) a past history of liver cirrhosis and early HCC treated with surgery and/or ablation, regardless of the number of previous treatments; (2) complete response to treatment on imaging according to the EASL criteria [12]; (3) no evidence of HCC recurrence at inclusion; and (4) ≥ 1 new arterial-phase-enhancing hepatic focus ≥ 7 mm without washout on EC-MRI; the 7 mm cutoff was selected based on the feasibility of percutaneous biopsy of the target lesion according to existing evidence [6].
The exclusion criteria were (1) contraindication for MRI; (2) poor renal function (eGFR < 30 mL/min/1.73 m2); (3) allergy to gadolinium; or (4) suspicion of local recurrence or incomplete treatment.
Diagnostic algorithm
Figure 1 summarizes the diagnostic algorithm followed in this study. Potential patients were identified by hepatologists (MR or AF) after reading MRI reports and invited to participate after a radiologist (JR with 13 years of experience in liver imaging) confirmed they fulfilled the inclusion criteria. If more than one arterial-enhancing focus was identified in the same EC-MRI study, only the two largest foci were selected for the analyses. Once the patient signed the informed consent form, we registered all demographic data and obtained a blood sample to determine liver, renal, and hematologic parameters. Within 1 month after EC-MRI, patients underwent Gd-EOB-DTPA MRI in the same scanner. Afterward, ultrasound-guided fine-needle biopsy specimens were obtained by radiologists aware of the location of target lesions. If the lesion was not seen initially on gray-scale ultrasound, 2.5 mL of intravenous contrast agent (Sonovue®, Bracco) was injected to detect arterial-enhancing lesions and to guide the biopsy. Patients with lesions not detected by contrast-enhanced ultrasound or biopsies negative for malignancy were followed up with EC-MRI every 3 months.
The gold standard for the final diagnosis of HCC was defined as histologic confirmation or arterial enhancement and portal or delayed venous washout on nodules ≥ 1 cm in size on follow-up EC-MRI [13, 14]. We did not consider an increase in size without convincing venous washout as diagnostic criteria of HCC given the lack of specificity for HCC.
MR technique
All examinations were performed on a 1.5-T unit with a phased-array coil (either Magnetom Aera, Siemens Medical Solutions, or Signa HDxt, GE Healthcare). The supplementary material reports the MRI acquisition protocols in detail.
For each patient, both EC-MRI and Gd-EOB-DTPA MRI studies were obtained in the same scanner.
Fine-needle biopsy
Radiologists experienced in needle biopsy used 18-gauge needles (Monopty; Bard Inc) to obtain core-needle specimens when technically feasible. Specimens were routinely processed and stained with hematoxylin-eosin. Although specific immunohistochemical staining was applied when necessary, no specific staining combination was used [4], and the International Working Party criteria [5] were used to establish the diagnosis of HCC.
Image interpretation
Two abdominal radiologists with access to demographic, clinical, and EC-MRI findings but blinded to the final diagnosis (A.D. and J.R., with 20 and 13 years of experience in liver imaging, respectively) independently registered the Gd-EOB-DTPA MRI characteristics of each initially selected target arterial-enhancing foci in an electronic database, reaching a consensus about discrepancies.
The location of target arterial-enhancing foci detected at EC-MRI was defined according to the Couinaud classification. We recorded the following Gd-EOB-DTPA MRI parameters: largest diameter of the target arterial-enhancing foci, fatty metamorphosis within the nodule (loss of signal intensity between T1 in and opposite phase), confirmation of arterial washin (using both arterial and subtraction sequences), portal washout, and the presence of enhancing peripheral capsule. Readers qualitatively assessed the intensity of the target arterial-enhancing foci with respect to the surrounding liver parenchyma in hepatobiliary-phase Gd-EOB-DTPA MRI and DWI (hypointense, isointense, or hyperintense). For the analysis of signal intensities on DWI, only the highest b value available was used (800 s/mm2 for the Siemens scanner and 600 s/mm2 for the GE).
Statistical analysis
No formal sample size was calculated for this pilot study. We report quantitative variables as medians and interquartile ranges (IQR 25th–75th percentiles) and categorical variables as absolute frequencies and percentages. To compare groups, we used the Mann-Whitney U test for continuous or ordinal variables and Fisher’s exact test for categorical variables. To calculate specificities, sensitivities, positive predictive values (PPV), negative predictive values (NPV), and relative risks (RR), we used cross-tabulation. We used the Kaplan-Meier method to calculate the time from EC-MRI detection of an arterial-enhancing focus to confirmation of HCC recurrence, and Cox regression models to calculate hazard ratios (HR) for the association between qualitative assessments of hepatobiliary-phase images and DWI sequences and time to confirmation of HCC recurrence. To determine the degree of interobserver agreement, we used the Kappa index. All tests were two-sided with p < 0.05 considered significant. SAS software, version 9.4, was used for all statistical analyses.
Results
Patients and lesion characteristics
Table 1 reports patients’ characteristics. Of the 40 subjects who fulfill the inclusion criteria and were invited to participate in the study, 6 were excluded (2 for new nodular arterial-enhancing foci treated by ablation without histological diagnosis of HCC after two biopsies but with contrast-enhanced ultrasound conclusive for HCC recurrence; 2 for withdrawal of consent; 1 for poor-quality MRI; and 1 for liver transplantation before Gd-EOB-DTPA MRI). Thus, 34 patients (27 men; 73.5% with hepatitis C virus) with a total of 53 new arterial-enhancing foci on EC-MRI were included in the analysis (Supplementary Figure 1).
Previous curative treatment was surgical resection in 11/34 subjects (32.4%) and radiofrequency ablation in 23/34 (67.6%). The median time between curative treatment and detection of arterial-enhancing foci on EC-MRI was 20.5 (IQR 8.5–42.25) months.
All target arterial-enhancing foci newly detected at EC-MRI were also seen at Gd-EOB-DTPA MRI, but in 3 patients, some additional small (< 5 mm) enhancing foci seen at EC-MRI and not categorized as target lesions because of their size were not seen at Gd-EOB-DTPA MRI.
The final diagnosis of HCC was established in 42/53 (79.2%) of the initially detected arterial-enhancing focus. Median arterial-enhancing focus size was 10 (IQR 9–14) mm. The diagnosis of HCC was by histology in 20 lesions (from ultrasound-guided biopsy specimens in 15 and after liver transplantation in 5) and by applying non-invasive criteria [13] during the EC-MRI follow-up in the remaining 22 lesions. Among the HCC diagnosed by histology, 14/20 (70%) were well-differentiated HCC, 5/20 (25%) were moderate-differentiate HCC, and the remaining HCC (5%) was a poor-differentiated HCC.
The median time to establish the diagnosis of HCC recurrence, calculated by the Kaplan-Meier method, was 6 (95%CI, 4–7) months after initial detection by EC-MRI. To ensure benignity, arterial-enhancing foci categorized as benign were followed up for 27.1 (IQR 19.57–35.33) months.
Table 2 summarizes the characteristics of all arterial-enhancing foci on EC-MRI on Gd-EOB-DTPA MRI.
Hepatobiliary-phase and DWI characteristics and risk of developing HCC
Hypointensity on hepatobiliary-phase Gd-EOB-DTPA MRI of arterial-enhancing foci on EC-MRI for the diagnosis of HCC yielded 69.1% (95%CI, 55.1–83.0) sensitivity and 72.7% (95%CI, 46.4–99.1) specificity, whereas DWI hyperintensity of arterial-enhancing foci on EC-MRI yielded 85.7% (95%CI, 75.1–96.3) sensitivity and 72.7% (95%CI, 46.4–99.1) specificity. Combining hepatobiliary-phase hypointensity and DWI hyperintensity yielded 54.8% (95%CI, 39.7–69.81) sensitivity, 90.9% (95%CI, 73.9–100) specificity, 95.8% (95%CI, 87.8–100) PPV, and 34.5% (95%CI, 17.2–51.8) NPV (Table 3).
Table 4 reports HR for the association between the time from the EC-MRI detection of an arterial-enhancing focus to the confirmation of HCC recurrence and qualitative assessments of hepatobiliary-phase Gd-EOB-DTPA MRI and DWI hyperintensity. The strongest association with the risk of HCC recurrence was DWI hyperintensity (HR 4.08 [95%CI, 1.67–9.95], p = 0.002); adding hepatobiliary-phase hypointensity to DWI hyperintensity decreased the strength of the association (HR 3.09 [95%CI, 1.58–6.05], p = 0.001).
Interobserver agreement
The interobserver agreement between the two readers in the categorical classification of lesion signal intensity with respect to the surrounding liver parenchyma (hypointense, isointense, or hyperintense) was good for hepatobiliary-phase Gd-EOB-DTPA MRI (k = 0.726 [95%CI, 0.54–0.91] p < 0.001) and substantial for DWI (k = 0.69 [95%CI, 0.49–0.88] p < 0.001).
Discussion
The results of our study suggest that the best model to predict whether newly detected arterial-phase-enhancing foci represent HCC recurrence or not is the combination of hypointensity on hepatobiliary-phase Gd-EOB-DTPA MRI and DWI hyperintensity, allowing an earlier HCC recurrence diagnosis in 54% of cases with a very high specificity and positive predictive value despite the non-conclusive diagnosis (namely lack of venous-phase washout) by EC-MRI. To our knowledge, this is the first prospective study to evaluate the contributions of Gd-EOB-DTPA MRI and DWI to early detection of tumor recurrence in patients with early HCC (BCLC A) who achieved a complete response to ablation or resection but have non-conclusive imaging diagnosis of HCC recurrence using EC-MRI. This population is at high risk of HCC recurrence and deserves optimized imaging follow-up with well-established diagnostic criteria [1, 13, 14]. Most clinical practice guidelines recommend using strict non-invasive criteria based on arterial-phase contrast enhancement followed by venous-phase washout to confidently diagnose HCC and avoid overdiagnosis and overtreatment [13, 14]. However, although these criteria have been validated in treatment-naïve cirrhotic livers [6, 8, 15,16,17], scant data are available about their performance in the follow-up of patients previously treated for HCC.
The combination of arterial-enhancing lesion showing hypointensity on hepatobiliary phase and hypersignal on DWI showed to have the most stringent diagnostic criteria to avoid overdiagnosis of HCC and not over treat lesions different than HCC but acknowledging that at expenses to reduce the sensitivity (54.8%). In our opinion, these results should not be interpreted from the perspective that in nearly half of the HCC recurrences appearing as arterial-enhancing foci showing hypointensity on hepatobiliary phase and hypersignal on DWI the treatment is delayed. We prioritized specificity over sensitivity to avoid overdiagnosis of HCC recurrence and thus overtreatment on patients who do not have real HCC recurrence.
This population has a very high pre-test prevalence of HCC; in our cohort, the accumulated recurrence rate of HCC was nearly 80%. Thus, to avoid the risks associated with delayed diagnosis of HCC recurrence, a more sensitive approach might be justified. In our study, only one of 24 arterial-phase-enhancing foci that were hyperintense on DWI and hypointense on hepatobiliary-phase Gd-EOB-DTPA MRI was not diagnosed as HCC by the gold standard (Fig. 2). This was an 18-mm nodule detected in an HCV-positive cirrhotic patient12 months after ablation. On imaging follow-up, the lesion’s size remained stable but the number of hypervascular foci in the liver increased; although none of these lesions had venous-phase washout during the 10-month follow-up, the findings were highly suspicions of multifocal HCC recurrence.
MR images of a 67-year-old with HCV-related liver cirrhosis. Axial Gd-EOB-DTPA shows a 10-mm arterial-enhancing focus in liver segment V previously detected at EC-MRI. The lesion was hyperintense in the arterial phase (arrow in a) and isointense to liver parenchyma in the portal venous phase (b). In the axial hepatobiliary-phase 20 min after contrast injection, there was no contrast uptake (arrow in c). On diffusion-weighted imaging (b = 600 s/mm2), the lesion was hyperintense (arrow in d). Histological analysis of ultrasound-guided biopsy specimen diagnosed a moderately differentiated hepatocellular carcinoma
Importantly, 12 of 42 HCC recurrences were hyperintense on hepatobiliary-phase images (Fig. 3). This result corroborates previous observations [18, 19] and should be taken into consideration to avoid misclassifying an HCC as a benign lesion based on hepatobiliary-phase uptake. We have noted that 28.5% of the HCC recurrences showed hyperintensity on hepatobiliary-phase that is higher than in other studies’ observations [18, 19]. We hypothesize that the high rate of well-differentiated representing 70% of the histologically proven HCC can explain this unexpected finding.
MR images of a 78-year-old woman with HCV-related cirrhosis. In the axial arterial phase on Gd-EOB-DTPA MRI, a 9-mm-size hypervascular focus in segment VII was identified (arrow in a). The focus was isointense in the portal venous phase (b) and hyperintense in the hepatobiliary phase 20 min after contrast injection (arrow in c). On axial diffusion-weighted imaging (b = 600 s/mm2), the nodule showed mild restriction (arrow in d). The lesion did not meet the EASL/AASLD diagnostic criteria for hepatocellular carcinoma. Histology of US-guided biopsy specimens categorized the lesion as a well-differentiated hepatocellular carcinoma
One potential concern when using Gd-EOB-DTPA is the quality of hepatobiliary-phase images, which is usually linked to liver function [20]. Most of our cirrhotic patients were Child-Pugh A with optimal liver function. These patients might benefit most from improved MRI differentiation between pseudolesions and recurrence of HCC because they can benefit from salvage therapy and thus survive longer. Moreover, the quality of hepatobiliary-phase images is normally better in Child-Pugh A patients, because a poor liver function is associated with lower liver parenchyma uptake in the hepatobiliary phase, making it more difficult to detect hypointensity of focal liver lesions in this phase in patients with more advanced liver disease [21, 22].
Our results are in line with those reported in Motosugi et al’s retrospective study [23], which attempted to distinguish between benign lesions (arterioportal shunts or pseudolesions) and hypervascular HCC. Of 104 pseudolesions, 16 (15%) were hypointense in the hepatobiliary phase, and more interestingly, no nodular pseudolesions were visible on DWI.
One potential concern on the use of DWI for the detection of HCC recurrence is the potential artifacts on segment II just below the heart. In our series, only 5 arterial-enhancing foci (diameter ranging 10–25 mm) were located in segment II and all except one displayed high signal intensity on DWI.
Our study has some limitations. First, only 53 arterial-phase-enhancing foci in 34 patients were included in this pilot study to explore the potential role of functional techniques in a different clinical scenario than previously analyzed. Second, only 20 lesions were studied histologically; all these were confirmed as HCC. Thus, a subanalysis of only histologically confirmed cases would have too few cases to allow conclusions about the diagnostic accuracy of Gd-EOB-DTPA MRI. Finally, our study did not compare the accuracy of EC-MRI and Gd-EOB-DTPA MRI, since the latter was performed after inconclusive findings on EC-MRI. Therefore, the design of our study precludes recommendations of Gd-EOB-DTPA MRI as a first-line tool for detecting early recurrence but supports the use of EOB-DTPA MRI in selected cases when findings on EC-MRI are non-conclusive.
In summary, to our knowledge, this is the first prospective study to evaluate the contribution of functional MRI techniques in predicting the risk of HCC recurrence from new arterial-phase-enhancing foci non-conclusive for HCC recurrence in EC-MRI of cirrhotic patients that achieved a complete response after surgical resection or ablation of previous HCC. In lesions that are hypervascular on EC-MRI, hypointensity on hepatobiliary-phase Gd-EOB-DTPA MRI and hyperintensity on DWI have high specificity and PPV for the detection of HCC recurrence in cirrhotic livers, improving the selection of patients for salvage therapy.
Abbreviations
- AASLD:
-
American Association for the Study of Liver Diseases
- DWI:
-
Diffusion-weighted imaging
- EASL:
-
European Association for the Study of the Liver
- EC-MRI:
-
Extracellular gadolinium-enhanced liver MRI
- Gd-EOB-DTPA:
-
MRI using gadoxetic acid
- HCC:
-
Hepatocellular carcinoma
- HR:
-
Hazard ratio
- IQR:
-
Interquartile range
- MRI:
-
Magnetic resonance imaging
- RR:
-
Relative risk
References
Poon RT, Fan ST, Lo CM, Liu CL, Wong J (2002) Long-term survival and pattern of recurrence after resection of small hepatocellular carcinoma in patients with preserved liver function. Ann Surg 235:373–382
Tabrizian P, Jibara G, Shrager B, Schwartz M, Roayaie S (2015) Recurrence of hepatocellular cancer after resection: patterns, treatments, and prognosis. Ann Surg 261:947–955
Sala M, Llovet JM, Vilana R et al (2004) Initial response to percutaneous ablation predicts survival in patients with hepatocellular carcinoma. Hepatology 40:1352–1360
European Association for the Study of the Liver (2018) EASL Clinical Practice Guidelines: Management of hepatocellular carcinoma. J Hepatol 69:182–236
Marrero JA, Kulik LM, Sirlin CB et al (2018) Diagnosis, Staging, and Management of Hepatocellular Carcinoma: 2018 Practice Guidance by the American Association for the Study of Liver Diseases. Hepatology 68:723–750
Forner A, Vilana R, Ayuso C et al (2008) Diagnosis of hepatic nodules 20 mm or smaller in cirrhosis: prospective validation of the noninvasive diagnostic criteria for hepatocellular carcinoma. Hepatology 47:97–104
Sangiovanni A, Manini MA, Iavarone M et al (2010) The diagnostic and economic impact of contrast imaging techniques in the diagnosis of small hepatocellular carcinoma in cirrhosis. Gut 59:638–644
Khalili K, Kim TK, Jang H-J et al (2011) Optimization of imaging diagnosis of 1-2 cm hepatocellular carcinoma: an analysis of diagnostic performance and resource utilization. J Hepatol 54:723–728
Joo I, Lee JM, Lee DH, Jeon JH, Han JK, Choi BI (2015) Noninvasive diagnosis of hepatocellular carcinoma on gadoxetic acid-enhanced MRI: can hypointensity on the hepatobiliary phase be used as an alternative to washout? Eur Radiol 25:2859–2868
Granito A, Galassi M, Piscaglia F et al (2013) Impact of gadoxetic acid (Gd-EOB-DTPA)-enhanced magnetic resonance on the noninvasive diagnosis of small hepatocellular carcinoma: a prospective study. Aliment Pharmacol Ther 37:355–363
Haradome H, Unno T, Morisaka H et al (2017) Gadoxetic acid disodium-enhanced MR imaging of cholangiolocellular carcinoma of the liver: imaging characteristics and histopathological correlations. Eur Radiol 27:4461–4471
Bruix J, Sherman M, Llovet JM et al (2001) Clinical management of hepatocellular carcinoma. Conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 35:421–430
Tremosini S, Forner A, Boix L et al (2012) Prospective validation of an immunohistochemical panel (glypican 3, heat shock protein 70 and glutamine synthetase) in liver biopsies for diagnosis of very early hepatocellular carcinoma. Gut 61:1481–1487
International Consensus Group for Hepatocellular Neoplasia The International Consensus Group for Hepatocellular Neoplasia (2009) Pathologic diagnosis of early hepatocellular carcinoma: A report of the International Consensus Group for Hepatocellular Neoplasia. Hepatology 49:658–664
Rimola J, Forner A, Tremosini S et al (2012) Non-invasive diagnosis of hepatocellular carcinoma ≤ 2 cm in cirrhosis. Diagnostic accuracy assessing fat, capsule and signal intensity at dynamic MRI. J Hepatol 56:1317–1323
Iavarone M, Sangiovanni A, Forzenigo LV et al (2010) Diagnosis of hepatocellular carcinoma in cirrhosis by dynamic contrast imaging: the importance of tumor cell differentiation. Hepatology 52:1723–1730
Darnell A, Forner A, Rimola J et al (2015) Liver imaging reporting and data system with MR imaging: evaluation in nodules 20 mm or smaller detected in cirrhosis at screening US. Radiology 275:141–132
Choi JW, Lee JM, Kim SJ et al (2013) Hepatocellular carcinoma: imaging patterns on gadoxetic acid–enhanced MR images and their value as an imaging biomarker. Radiology 267:776–786
Sugimoto K, Kim SR, Imoto S et al (2015) Characteristics of hypovascular versus hypervascular well-differentiated hepatocellular carcinoma smaller than 2 cm - focus on tumor size, markers and imaging detectability. Dig Dis 33:721–727
Yoon JH, Lee JM, Kang H et al (2019) Quantitative assessment of liver function by using gadoxetic acid–enhanced MRI: hepatocyte uptake ratio. Radiology 290:125–133
Kim AY, Kim YK, Lee MW et al (2012) Detection of hepatocellular carcinoma in gadoxetic acid-enhanced MRI and diffusion-weighted MRI with respect to the severity of liver cirrhosis. Acta Radiol 53:830–838
Nakamura Y, Tashiro H, Nambu J et al (2013) Detectability of hepatocellular carcinoma by gadoxetate disodium-enhanced hepatic MRI: tumor-by-tumor analysis in explant livers. J Magn Reson Imaging 37:684–691
Motosugi U, Ichikawa T, Sou H et al (2010) Distinguishing hypervascular pseudolesions of the liver from hypervascular hepatocellular carcinomas with gadoxetic acid-enhanced MR imaging. Radiology 256:151–158
Funding
This study has received funding by Sociedad Española de Radiología Médica (SERAM).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Jordi Rimola.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Victor Sapena kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained.
Methodology
• prospective
• diagnostic or prognostic study
• performed at one institution
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 1161 kb)
Rights and permissions
About this article
Cite this article
Rimola, J., Forner, A., Sapena, V. et al. Performance of gadoxetic acid MRI and diffusion-weighted imaging for the diagnosis of early recurrence of hepatocellular carcinoma. Eur Radiol 30, 186–194 (2020). https://doi.org/10.1007/s00330-019-06351-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-019-06351-0