Abstract
Objectives
To develop an MR-based semi-quantitative meniscus scoring technique for postoperative assessment of the degree of meniscal resection, to test its reproducibility, and to study the relationship between the amount of resection and degenerative disease burden.
Methods
We studied the right knee of 135 participants from the Osteoarthritis Initiative that underwent meniscal surgery an average of 14 years previously. The amount of meniscal resection was assessed on baseline 3.0-T MRIs and calculated as meniscus resection score (MenRS) with a range of 0 to 18. Knee abnormalities at baseline and 48 months were graded using a modified Whole-Organ Magnetic Resonance Imaging Score (WORMS). Subjects were also stratified according to meniscal resection performed after injury versus without preceding injury. Statistical analysis included intra-class correlation coefficient (ICC) to determine reproducibility as well as regression models and partial correlations to correlate MenRS with WORMS outcomes.
Results
ICC values for intra- and inter-observer reproducibility of MenRS were 0.980 and 0.977, respectively. Overall, the amount of meniscal resection showed a significant correlation with baseline WORMS grades: higher MenRS was associated with higher total WORMS grades (p = 0.004) and cartilage (p = 0.004) and ligament (p < 0.001) subscores. However, no significant association between MenRS and change in WORMS grades over 48 months was found. The relationship between MenRS and baseline WORMS grades did not change after adjusting for a reported history of knee injury.
Conclusions
Postoperative assessment of the knee following partial meniscectomy using the newly developed MenRS showed excellent reproducibility and significant cross-sectional correlation with WORMS gradings.
Key Points
• The newly developed semi-quantitative MR-based meniscal resection score demonstrated excellent reproducibility.
• A significant correlation between the amount of meniscal resection measured using the newly developed score and the degree of overall knee joint degenerative disease and cartilage defects was found.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Conservative treatment for meniscal tears [1, 2] has been advocated over meniscectomy to reduce the risk of knee osteoarthritis (OA) [3,4,5]. However, partial meniscectomy is to some extent unavoidable [6] and is still commonly performed in the Western World with an incidence of 300 per 100,000 people annually [7].
A large number of predictive factors for the development of knee OA after meniscectomy have been discussed, with the amount of meniscus removed remaining the strongest predictor [8] and other important factors being degenerative tear [3], lateral meniscectomy [9], and age at surgery [10]. When comparing different meniscectomy techniques, partial meniscectomy has shown significantly better radiologic and functional outcomes than subtotal and total meniscectomy [11,12,13]; the benefits of more conservative meniscectomies were also highlighted by biomechanical evidence that joint stress on articular cartilage increased proportionally to the amount of meniscus resected [14,15,16]. Furthermore, Englund et al noted that the type of meniscal tears (degenerative or traumatic tears) may have confounded the association of the degree of resection with radiographic and symptomatic osteoarthritis [17, 18].
To the best of our knowledge, few studies have documented the amount of meniscal resection in clinical practice; thus, the exact effect of various size of resection on subsequent OA risk remains unknown. Hede et al calculated the percentage of removed meniscal surface on postoperative drawings which were made to indicate the area excised from each meniscus, and found it to be inversely related to knee joint function [12]. A quantitative MRI method has been validated to determine the reduction in meniscal volume after meniscectomy [19, 20]; however, manual segmentation of the meniscus is a time-consuming process, limiting its potential to be used in large clinical studies [21].
To date, MR imaging is the standard technique to analyze the postoperative appearance of the resected meniscus [22], detect meniscal deficiencies [23, 24], and reveal OA-associated abnormalities [25, 26]. Thus, the purpose of our study was (1) to develop an MR-based semi-quantitative scoring approach to assess the degree of meniscal resection (meniscus resection score, MenRS), (2) to evaluate its reproducibility, and (3) to correlate the MenRS with the degenerative disease burden both cross-sectionally and longitudinally.
Methods
This study utilized data from the Osteoarthritis Initiative (OAI; https://oai.epi-ucsf.org/), a longitudinal multicenter study of 4796 subjects aimed at identifying risk factors for knee OA. Informed consent was obtained from all participants; the study was compliant with the Health Insurance Portability and Accountability Act and was approved by the local institutional review boards of all participating centers.
Subjects
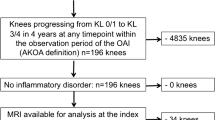
Subjects with meniscal surgery of the right knee were selected from the OAI, excluding individuals with end-stage OA of the right knee at baseline (baseline Kellgren-Lawrence (KL) grade higher than 3) and a history of rheumatoid arthritis. Individuals with multiple meniscal surgeries or ACL reconstruction were also excluded. The remaining subjects were categorized into two groups according to their reported history of preceding knee injury (badly enough to limit ability to walk for at least 2 days). For subjects with preceding knee injury, the follow-up question “Was this meniscal surgery performed to repair an injury episode?” was also part of the selection and needed to be answered as “yes.” To obtain a clear association of knee injury and meniscal surgery, we included only subjects who had meniscal surgery within 2 years after an episode of knee injury [8, 10]. In total, 158 subjects with preceding knee injury and 73 without were selected.
During the image analysis, 23 subjects showed severe meniscal deformity of the right knee, such as root or flap tears, severe extrusion, or maceration. Since this would limit the meniscus scoring [27] and may have an independent impact on accelerating knee degeneration [28, 29], these subjects were excluded from the analysis. Subjects with bilateral meniscectomy of the right knee were also excluded due to the small number (n = 3). To validate the score, we used the contralateral meniscus of the left knee as a reference [20, 30] and therefore excluded 70 subjects with meniscectomy or meniscal deformity with or without tears of the left knee at baseline. Using the above criteria, a total of 95 subjects with preceding injury and 40 without were selected as shown in Fig. 1. All subjects had undergone meniscal surgery on average 14 years (median 9 years, range 0–59 years) before baseline assessment and then were followed over an additional 48 months.
MR imaging
MR images were obtained at the four different clinical sites of the OAI with cross-calibrated 3.0-T imagers (Trio, Siemens) using quadrature transmit-receive coils (USA Instruments). Images obtained with the following three sequences were analyzed: (a) coronal 2D intermediate-weighted (IW) turbo spin-echo (TSE) sequences (repetition time (TR)/echo time (TE), 3700 ms/29 ms); (b) sagittal 2D IW TSE sequences with fat suppression (TR/TE, 3200 ms/30 ms); and (c) sagittal 3D dual-echo steady-state (DESS) sequences (TR/TE/flip angle, 16.3 ms/4.7 ms/25°). More details are available in the OAI MR protocol [31].
Meniscus resection score
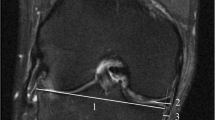
A consensus training session was performed by three musculoskeletal radiologists (D.S., J.N. and T.M.L.) to calibrate and standardize readings. Subsequently, the amount and location of meniscal resection were scored on baseline MR images of the right knee by a radiologist (D.S.). As shown in Fig. 2, a zone classification system modified from Cooper et al [32] was used. Each meniscus was divided into radial and circumferential zones, each comprising one third of the meniscus. Radial zones were referred to as A, B, and C for the medial meniscus (from posterior to anterior) and D, E, and F for the lateral meniscus (from anterior to posterior). The circumferential zones were 1 for the inner third, 2 for the middle third, and 3 for the outer third. The anterior and posterior horns were typically assessed in the sagittal plane of MR images, whereas the body of the meniscus was assessed in the coronal plane [33]. To avoid overlap between grades obtained in the different planes during our analyses, we cross-referenced the grades using the thin section axial multi-planar reformatting of the sagittal 3D DESS sequence, which allows better assessment of shape and subdivisions of the entire meniscus [21].
To evaluate the amount of meniscus resected, each zone was graded either as 0 (no resection), 1 (< 50% of the area resected), or 2 (> 50% of the area resected) as shown in Fig. 3 and then summed across zones. The maximum value of meniscus resection score (MenRS) for each meniscus was 18, which is consistent with near total meniscectomy. To validate the MenRS concerning the amount of meniscal resection, findings were compared with the contralateral meniscus, which was used as a reference [20, 30].
Grading amount of meniscus resected for each involved zone. Schematic drawings (left) and MR images (right) show grade 1 < 50% (a) and grade 2 > 50% (b) of the subregional volume resected in the inner third of the body of medial meniscus (zone B1) in the right knee. The resected meniscal tissues, cross-hatched in schematic drawings, are noted as truncated appearance (arrow) in the coronal 2D intermediate-weighted turbo spin-echo sequence and substance loss (arrow) in the axial multi-planar reformatting of the sagittal 3D dual-echo steady-state sequence. The small MR images show the contralateral meniscus of the left knee which are used as a reference
WORMS grading
Baseline and 48-month follow-up images of the right knee were graded semi-quantitatively to assess fairly early knee degenerative changes, using the modified Whole-Organ Magnetic Resonance Imaging Score (WORMS) system [34]. To optimize reproducibility in the grading, all members in our group initially have to undergo a WORMS training. In this study, a trained radiologist (D.S.), blinded to subject characteristics, scored all MRIs under the supervision of a board-certified musculoskeletal radiologist (T.M.L.). Cartilage defects were scored from 0 to 6; bone marrow edema pattern (BMEP) as well as subarticular cysts were scored from 0 to 3 in each of the same six regions (patella, trochlea, medial/lateral femur, and medial/lateral tibia). Other abnormalities including those of the ligaments and joint effusion were also graded. Since meniscal surgery was our predictor, we did not include meniscal lesions as one of the outcomes. We calculated sum scores combining all five imaging parameter categories as well as for each imaging category individually over all subregions of each knee.
Reproducibility
Two radiologists (D.S., J.N.) independently graded meniscal resection in 20 randomly selected subjects to determine inter-reader reproducibility. After a 1-month interval, the grading was repeated to determine intra-reader reproducibility. Intra-reader reproducibility and inter-reader reproducibility of the amount of meniscal resection were assessed by the intra-class correlation coefficients (ICCs) and Bland-Altman plots.
Statistical analyses
Statistical analyses were performed with STATA (Version 14; Stata), using a two-sided, 0.05 level of significance. Subject characteristics were calculated separately in subjects with and without preceding injury. Between-group differences were assessed by Student’s independent t tests or chi-square tests as appropriate. Regression models and partial correlations were used to assess the associations of MenRS with baseline WORMS grades and change in WORMS grades (independent variable: MenRS, dependent variables: mean baseline WORMS parameters and mean increase in WORMS grades over 48 months). Linear regression models were used with numeric dependent variables (i.e., total WORMS grades as well as cartilage, BMEP, cysts, and ligaments subscales) while logistic regression models with binary dependent variables (i.e., the presence of effusion).
Since previous studies have highlighted that knee OA following meniscectomy is primarily found at the tibiofemoral joint [14, 35], four separate compartmental predictors were examined for cartilage defects, BMEP, and subchondral cysts: index compartment (surgical tibiofemoral joint), contralateral compartment (nonsurgical tibiofemoral joint), femoral compartment (lateral and medial femur), and tibial compartment (lateral and medial tibia).
In a subsequent analysis, we examined whether the occurrence of a preceding injury confounded the relationship between MenRS and WORMS grades by including injury as a covariate. All analyses were adjusted for age at baseline, age at surgery, sex, and baseline BMI.
Results
Subject characteristics
Subject characteristics are shown in Table 1. No significant differences were found between subjects with and without preceding injury except for the mean age at surgery, which was significantly higher in subjects without preceding injury compared to those with preceding injury (51.7 ± 12.0 years vs 41.2 ± 15.4 years, p < 0.001).
Validation using the contralateral side as a reference
Comparing the corresponding menisci of the resected right knee and the control left knee, differences in meniscal morphology were found in 96 of 135 menisci and all of these knees had a meniscal resection with MenRS = 1–18. Even after review with the contralateral side, no differences in meniscal morphology were found in 39 subjects. In these menisci, resection or debridement may have been minimal, which was not visualized with MRI, and therefore we scored them as MenRS = 0. In these 39 subjects, cartilage in the tibiofemoral compartment was found to be significantly less damaged at baseline than in those 96 subjects with meniscal resection grade 1–18 (2.31 ± 2.41 vs 4.79 ± 4.48, coefficient 2.94, p < 0.001) but longitudinal change over 48 months was not significantly different (p > 0.05).
Scoring amount of meniscus resected
The amount and location of the resected meniscus, assessed with the proposed method on baseline MR images, are demonstrated in Table 2. Of the 96 subjects with MenRS > 0, the mean score in subjects with preceding injury was found to be significantly higher compared to those without preceding injury (7.83 ± 6.21 vs 5.01 ± 3.65, p = 0.03). In addition, scores ranging from 16 to 18, representing a resection of most meniscal tissue, were significantly more often present in subjects with preceding injury compared to those without preceding injury (16.8% vs 2.5%, p = 0.02).
Reproducibility
ICCs for intra- and inter-reader agreement of MenRS in the overall meniscus were 0.980 (95% CI 0.949, 0.992) and 0.977 (95% CI 0.941, 0.991), respectively. In the Bland-Altman plots of intra- and inter-reader assessments, most of the values ranged within a mean difference ± 1.96 SD of − 0.15 ± 2.72 and − 0.05 ± 2.95, respectively (Fig. 4). Furthermore, intra-reader ICCs of MenRS in the anterior horn, body, and posterior horn were 0.992, 0.968, and 0.966, while inter-reader ICCs were 0.998, 0.963 and 0.905. For WORMS gradings, the inter-reader reliability was good with ICCs of 0.876–0.919 for cartilage defects, BMEP, and cysts, as assessed during the training.
Association between amount of meniscus resected and degenerative disease burden
Significant associations were found between the amount of meniscus resected and baseline WORMS grades, with higher MenRS being associated with higher WORMS grades (Table 3, Fig. 5). The MenRS was significantly associated with total WORMS for all five MR imaging parameter categories (r = 0.25, p = 0.004), as well as separately for cartilage (r = 0.25, p = 0.004) and ligaments (r = 0.32, p < 0.001), but not for BMEP, subchondral cysts, and joint effusion (odds ratio 1.01, 95% CI 0.92–1.10, p = 0.86).
Sagittal intermediate-weighted turbo spin-echo fat-suppressed MR images of the left knee at baseline (a, d), the right knee at baseline (b, e), and the right knee over 48 months (c, f). a–c The MR images of a 45-year-old woman who had a knee injury and then underwent medial partial meniscectomy (arrows) (meniscal resection with a score of 4 at the posterior horn) when she was 30 years old. d–f The MR studies of a 57-year-old man who had no knee injury and underwent partial meniscectomy (arrows) (meniscal resection with a score of 2 at the posterior horn) when he was 50 years old. The 45-year-old woman with a large amount of meniscal resection demonstrated a full-thickness focal cartilage defect at the medial tibia at baseline (thin arrows) (medial tibial cartilage WORMS grade 5); over 48 months, she developed BMEP at the medial tibia (*) (medial tibial BMEP grade 0 in b and 2 in c) and thinning of the cartilage at the medial femoral condyle (arrowheads) (medial femoral cartilage WORMS grade 0 in b and 3 in c). In contrast, only a partial thickness cartilage defect at the medial femur (arrowheads) was seen in the 57-year-old man with a relatively small amount of meniscal resection and no progression was detected over 48 months (medial femoral cartilage WORMS grade 3 in b and c)
In separate analyses of index and contralateral compartments, the MenRS showed significant correlations with baseline total WORMS, cartilage lesions, and BMEP in the index compartment (r range 0.33–0.37, p ≤ 0.001), while no or only weakly significant correlations were found in the contralateral compartment (r range 0.18–0.21, p range 0.049–0.09). With respect to the femoral and tibial compartments, the correlations between MenRS versus baseline cartilage lesions and BMEP were both statistically significant (femoral, r range 0.33–0.36, p < 0.001; tibial, r range 0.43–0.49, p < 0.001).
However, the MenRS was not significantly associated with changes in WORMS grades over 48 months, except for BMEP of the index compartment (r = − 0.25, p = 0.03). After further adjustment for preceding knee injury, the associations of MenRS with baseline WORMS and change in WORMS grades remained nearly the same (Supplemental Table). Assessing clinical features, the MenRS did not show significant associations with the baseline Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC) scores as well as change in WOMAC scores over 48 months (linear regression, p range = 0.27–0.95).
Discussion
In this study, we developed an MR-based semi-quantitative scoring method to assess the amount of meniscus removed in patients that underwent meniscectomy. The score showed excellent intra- and inter-reader reproducibility and was significantly associated with severity of postoperative knee OA using cross-sectional WORMS analysis. However, there was no significant association between the MenRS and WORMS change scores between baseline and 48 months. Furthermore, the association of MenRS with WORMS grades did not vary when further adjusted for preceding knee injury, though larger resections were found after previous injury.
Standard partial meniscus resection procedures like shaving or debridement make the exact measurement of the resected meniscal volume challenging [20]. To date, two approaches have been published for assessing meniscal resection. The International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine Knee Committee recently proposed for surgeons to calculate the percentage of resected meniscal surface area on a diagram created after reviewing operation records; however, this approach was found to be only moderately reliable (ICC = 0.65) [36]. Bowers et al validated a quantitative MRI approach for detecting a decrease in meniscal volume due to partial resection [19, 20]. Nevertheless, the time required for meniscal segmentation by different techniques varied between 30 and 90 min [21, 34, 37], and its validity in detecting a small amount of resection was questioned, especially for patients with meniscal hypertrophy [29].
The proposed scoring method offers a novel way to evaluate the degree of resection after meniscectomy using routine knee MRIs. The zone classification of meniscal resection in our method was based on Cooper’s classification system that has been widely used to standardize description of meniscal tears and guide surgical treatment [32, 36]. Using the menisci of the contralateral knee as a reference our approach showed excellent performance. The evaluation of the amount of the resected meniscus on a 3-point scale for each zone was concise and simple with 5–7 min required for a musculoskeletal radiologist to score each knee. The comparison with the contralateral knee only added approximately 2 min.
The intra-reader reproducibility and inter-reader reproducibility for the MenRS detected amount of resection per meniscus, and even per radial zone, were excellent. The MenRS showed significant positive associations with total WORMS as well as cartilage and ligament subscores, indicating that a larger amount of meniscal resection was associated with a higher number of knee osteoarthritic abnormalities. Biomechanical studies have repeatedly documented increases in contact stress and shear stress over articular cartilage, changes in pressure distributions, and loss of joint stability with respect to the amount of meniscus resected [15, 38, 39]. These adverse effects potentially increase the susceptibility of cartilage to damage and place the knee at higher risk of OA development [40], in line with our findings. No significant correlations between MenRS versus BMEP and subchondral cysts were found. This may be related to the variability of BMEP over time and the strong association between BMEP and subchondral cysts as described previously [41, 42]. As expected, separate analyses showed that the MenRS was significantly associated with WORMS grades of the index compartment but not of the contralateral compartment.
When correlating MenRS with changes in WORMS scores over 48 months, no significant differences were shown in the majority of imaging parameter categories and compartments. However, these findings do not suggest that the amount of meniscal resection is not associated with the progression of knee OA after meniscectomy. Subjects in our study had undergone meniscal surgery an average of 14 years earlier. At baseline assessment, many subjects already had radiographic knee OA and substantial cartilage lesions. We hypothesize that progression of degenerative changes may occur soon after surgery and then plateau or decrease as the joint adjusts to the meniscal resection [5, 35].
Our findings confirmed the observation of Englund et al [17, 18] that subjects with preceding injury appeared to undergo meniscectomy at a younger age and had a higher rate of total resection compared to subjects without preceding injury. Several previous studies reported higher evidence of knee OA following resection of degenerative than traumatic meniscal tears [35, 43]. Conversely, Matsusue et al found no significant difference in clinical outcomes between patients with and without a history of trauma [3]. In our study, when determining the association of amount of meniscal resection and the severity of postoperative knee OA, we found no significant difference between subjects with and without preceding injury. These findings indicate that in patients with meniscal surgery, the resection amount is likely the main risk factor for the subsequent knee joint degeneration, whereas the initial reason for meniscal resection seems to be subordinate.
Moreover, our proposed method could detect the part of the meniscus resected (lateral/medial, AH/body/PH). Subjects with a lateral meniscectomy sustained a significantly worse baseline WORMS outcomes in the global and index compartments when compared to those with medial meniscectomy. When investigating the association between side of resection and WOMAC scores, no significant differences were found between medial and lateral menisci. However, the limited number of lateral meniscectomies in our study (baseline: n = 14, 48 months: n = 10) should be noted.
Our study has several limitations. Firstly, surgical reports of meniscectomy were not available for participants in the OAI dataset due to the HIPAA compliance. However, to ensure accuracy on the information about the participants’ meniscectomy, we used the self-reported questionnaires to identify participants with meniscectomy, and moreover, all MRIs were reviewed thoroughly by a musculoskeletal radiologist for signs of meniscal surgery. Secondly, baseline MRI scans were acquired with long interval following surgery, potentially not capturing important imaging findings occurring directly after meniscectomy. Finally, preoperative MRIs are more readily available in clinical trials and would be helpful for further investigating the type of meniscal tears [17]. In our study, we utilized contralateral knee MRIs and found them to be a reliable reference. Of further note was that the index (right) knee showed significantly higher WOMAC scores both at baseline and 4-year FU when compared to the contralateral (left) knee, which was in line with previous studies finding that radiographic OA was substantially more frequent in the operated knee than in the contralateral knee [44, 45].
In conclusion, the described MR-based semi-quantitative scoring method is a concise and reproducible technique for assessing various degrees of partial meniscectomy and the score is significantly correlated with the severity of postoperative knee OA. Subjects had an increased risk of cartilage defects, BMEP, and ligamentous abnormalities with increased meniscus resection, particularly in the index compartment.
Abbreviations
- BMI:
-
Body mass index
- DESS:
-
Dual echo at steady state
- ICC:
-
Intra-class correlation coefficient
- KL:
-
Kellgren-Lawrence
- MenRS:
-
Meniscus Resection Score
- OA:
-
Osteoarthritis
- OAI:
-
Osteoarthritis Initiative
- WOMAC:
-
Western Ontario and McMaster Universities Osteoarthritis Index
- WORMS:
-
Whole-Organ Magnetic Resonance Imaging Score
References
Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM (2016) Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. Br J Sports Med 50:1473–1480
Stein T, Mehling AP, Welsch F, von Eisenhart-Rothe R, Jäger A (2010) Long-term outcome after arthroscopic meniscal repair versus arthroscopic partial meniscectomy for traumatic meniscal tears. Am J Sports Med 38:1542–1548
Matsusue Y, Thomson NL (1996) Arthroscopic partial medial meniscectomy in patients over 40 years old: a 5-to 11-year follow-up study. Arthroscopy 12:39–44
Sihvonen R, Paavola M, Malmivaara A et al (2013) Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 369:2515–2524
Roemer FW, Kwoh CK, Hannon MJ et al (2017) Partial meniscectomy is associated with increased risk of incident radiographic osteoarthritis and worsening cartilage damage in the following year. Eur Radiol 27:404–413
Pujol N, Barbier O, Boisrenoult P, Beaufils P (2011) Amount of meniscal resection after failed meniscal repair. Am J Sports Med 39:1648–1652
Abrams GD, Frank RM, Gupta AK, Harris JD, McCormick FM, Cole BJ (2013) Trends in meniscus repair and meniscectomy in the United States, 2005-2011. Am J Sports Med 41:2333–2339
Papalia R, Del Buono A, Osti L, Denaro V, Maffulli N (2011) Meniscectomy as a risk factor for knee osteoarthritis: a systematic review. Br Med Bull 99:89–106
Chatain F, Adeleine P, Chambat P, Neyret P (2003) A comparative study of medial versus lateral arthroscopic partial meniscectomy on stable knees: 10-year minimum follow-up. Arthroscopy 19:842–849
Bolano LE, Grana WA (1993) Isolated arthroscopic partial meniscectomy. Functional radiographic evaluation at five years. Am J Sports Med 21:432–437
Andersson-Molina H, Karlsson H, Rockborn P (2002) Arthroscopic partial and total meniscectomy. Arthroscopy 18:183–189
Hede A, Larsen E, Sandberg H (1992) The long term outcome of open total and partial meniscectomy related to the quantity and site of the meniscus removed. Int Orthop 16:122–125
King D (1936) The function of semilunar cartilages. JBJS 18:1069–1076
Lee SJ, Aadalen KJ, Malaviya P et al (2006) Tibiofemoral contact mechanics after serial medial meniscectomies in the human cadaveric knee. Am J Sports Med 34:1334–1344
Peña E, Calvo B, Martinez M, Palanca D, Doblaré M (2005) Finite element analysis of the effect of meniscal tears and meniscectomies on human knee biomechanics. Clin Biomech (Bristol, Avon) 20:498–507
Zielinska B, Donahue TL (2006) 3D finite element model of meniscectomy: changes in joint contact behavior. J Biomech Eng 128:115
Englund M, Roos EM, Roos HP, Lohmander LS (2001) Patient-relevant outcomes fourteen years after meniscectomy: influence of type of meniscal tear and size of resection. Rheumatology (Oxford) 40:631–639
Englund M, Roos EM, Lohmander LS (2003) Impact of type of meniscal tear on radiographic and symptomatic knee osteoarthritis: a sixteen-year followup of meniscectomy with matched controls. Arthritis Rheum 48:2178–2187
Bowers ME, Tung GA, Fleming BC, Crisco JJ, Rey J (2007) Quantification of meniscal volume by segmentation of 3T magnetic resonance images. J Biomech 40:2811–2815
Bowers ME, Tung GA, Oksendahl HL et al (2010) Quantitative magnetic resonance imaging detects changes in meniscal volume in vivo after partial meniscectomy. Am J Sports Med 38:1631–1637
Paproki A, Engstrom C, Chandra SS, Neubert A, Fripp J, Crozier S (2014) Automated segmentation and analysis of normal and osteoarthritic knee menisci from magnetic resonance images--data from the Osteoarthritis Initiative. Osteoarthritis Cartilage 22:1259–1270
White LM, Schweitzer ME, Weishaupt D, Kramer J, Davis A, Marks PH (2002) Diagnosis of recurrent meniscal tears: prospective evaluation of conventional MR imaging, indirect MR arthrography, and direct MR arthrography. Radiology 222:421–429
Boutin RD, Fritz RC, Marder RA (2014) Magnetic resonance imaging of the postoperative meniscus: resection, repair, and replacement. Magn Reson Imaging Clin N Am 22:517–555
Vance K, Meredick R, Schweitzer ME, Lubowitz JH (2009) Magnetic resonance imaging of the postoperative meniscus. Arthroscopy 25:522–530
Peterfy CG, Guermazi A, Zaim S et al (2004) Whole-Organ Magnetic Resonance Imaging Score (WORMS) of the knee in osteoarthritis. Osteoarthritis Cartilage 12:177–190
Joseph GB, McCulloch CE, Nevitt MC et al (2017) Tool for osteoarthritis risk prediction (TOARP) over 8 years using baseline clinical data, X-ray, and MRI: data from the osteoarthritis initiative. J Magn Reson Imaging 47:1517–1526
Pauli C, Grogan SP, Patil S et al (2011) Macroscopic and histopathologic analysis of human knee menisci in aging and osteoarthritis. Osteoarthritis Cartilage 19:1132–1141
Lance V, Heilmeier UR, Joseph GB, Steinbach L, Ma B, Link TM (2015) MR imaging characteristics and clinical symptoms related to displaced meniscal flap tears. Skeletal Radiol 44:375–384
Jung KA, Lee SC, Hwang SH et al (2010) High frequency of meniscal hypertrophy in persons with advanced varus knee osteoarthritis. Rheumatol Int 30:1325–1333
Yoon JR, Jeong HI, Seo MJ et al (2014) The use of contralateral knee magnetic resonance imaging to predict meniscal size during meniscal allograft transplantation. Arthroscopy 30:1287–1293
Peterfy CG, Schneider E, Nevitt M (2008) The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthritis Cartilage 16:1433–1441
Cooper DE, Arnoczky SP, Warren RF (1991) Meniscal repair. Clin Sports Med 10:529–548
Englund M, Roemer FW, Hayashi D, Crema MD, Guermazi A (2012) Meniscus pathology, osteoarthritis and the treatment controversy. Nat Rev Rheumatol 8:412–419
Rauscher I, Stahl R, Cheng J et al (2008) Meniscal measurements of T1ρ and T2 at MR imaging in healthy subjects and patients with osteoarthritis. Radiology 249:591–600
Zikria B, Hafezi-Nejad N, Roemer FW, Guermazi A, Demehri S (2017) Meniscal surgery: risk of radiographic joint space narrowing progression and subsequent knee replacement-data from the Osteoarthritis Initiative. Radiology 282:807–816
Anderson AF, Irrgang JJ, Dunn W et al (2011) Interobserver reliability of the International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine (ISAKOS) classification of meniscal tears. Am J Sports Med 39:926–932
Bloecker K, Wirth W, Hudelmaier M, Burgkart R, Frobell R, Eckstein F (2012) Morphometric differences between the medial and lateral meniscus in healthy men - a three-dimensional analysis using magnetic resonance imaging. Cells Tissues Organs 195:353–364
Vadher SP, Nayeb-Hashemi H, Canavan PK, Warner GM (2006) Finite element modeling following partial meniscectomy: effect of various size of resection. Conf Proc IEEE Eng Med Biol Soc 1:2098–2101
Atmaca H, Kesemenli CC, Memişoğlu K, Özkan A, Celik Y (2013) Changes in the loading of tibial articular cartilage following medial meniscectomy: a finite element analysis study. Knee Surg Sports Traumatol Arthrosc 21:2667–2673
Haemer JM, Song Y, Carter DR, Giori NJ (2011) Changes in articular cartilage mechanics with meniscectomy: a novel image-based modeling approach and comparison to patterns of OA. J Biomech 44:2307–2312
Kornaat PR, Kloppenburg M, Sharma R et al (2007) Bone marrow edema-like lesions change in volume in the majority of patients with osteoarthritis; associations with clinical features. Eur Radiol 17:3073–3078
Crema MD, Roemer FW, Zhu Y et al (2010) Subchondral cystlike lesions develop longitudinally in areas of bone marrow edema-like lesions in patients with or at risk for knee osteoarthritis: detection with MR imaging--the MOST study. Radiology 256:855–862
Englund M, Lohmander LS (2004) Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum 50:2811–2819
Paradowski PT, Lohmander LS, Englund M (2016) Osteoarthritis of the knee after meniscal resection: long term radiographic evaluation of disease progression. Osteoarthritis Cartilage 24:794–800
Longo UG, Ciuffreda M, Candela V et al (2018) Knee osteoarthritis after arthroscopic partial meniscectomy: prevalence and progression of radiographic changes after 5 to 12 years compared with contralateral knee. J Knee Surg. https://doi.org/10.1055/s-0038-1646926
Acknowledgements
We would like to thank the participants and staff of the Coordinating Center of the OAI for their invaluable assistance with patient selection, statistical analysis, and technical support.
Funding
The analyses in this study were funded through the NIH/NIAMS (National Institute of Arthritis and Musculoskeletal and Skin Diseases grants R01AR064771 and P50-AR060752). This study was also supported by grants from the National Scientific Foundation of China (NSFC, No. 31630025, 81571643, and 81320108013). The entire project was supported by the Osteoarthritis Initiative, a public–private partnership comprising 5 NIH contracts (National Institute of Arthritis and Musculoskeletal and Skin Diseases contracts N01-AR-2-2258, N01-AR-2-2259, N01-AR-2-2260, N01-AR-2-2261, and N01-AR-2-2262), with research conducted by the Osteoarthritis Initiative Study Investigators. The study was also funded in part by the Intramural Research Program of the National Institute on Aging, NIH. Private funding partners include Merck Research, Novartis Pharmaceuticals, GlaxoSmithKline, and Pfizer; the private sector funding for the Osteoarthritis Initiative is managed by the Foundation for the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Thomas M. Link.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
Gabby B. Joseph, PhD, kindly provided statistical advice for this manuscript.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional Review Board approval was obtained for this study.
Methodology
• Longitudinal, prospective cohort study with retrospective data analysis.
• Diagnostic or prognostic study.
• Multicenter study.
Electronic supplementary material
ESM 1
(DOCX 20 kb)
Rights and permissions
About this article
Cite this article
Sun, D., Neumann, J., Joseph, G.B. et al. Introduction of an MR-based semi-quantitative score for assessing partial meniscectomy and relation to knee joint degenerative disease: data from the Osteoarthritis Initiative. Eur Radiol 29, 3262–3272 (2019). https://doi.org/10.1007/s00330-018-5924-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-018-5924-y