Abstract
Objectives
This meta-analysis was performed to evaluate the accuracy of contrast-enhanced ultrasound (CEUS) in differentiating malignant from benign focal liver lesions (FLLs).
Methods
Cochrane Library, PubMed and Web of Science databases were systematically searched and checked for studies using CEUS in characterization of FLLs. Data necessary to construct 2×2 contingency tables were extracted from included studies. The QUADAS tool was utilized to assess the methodologic quality of the studies. Meta-analysis included data pooling, subgroup analyses, meta-regression and investigation of publication bias was comprehensively performed.
Results
Fifty-seven studies were included in this meta-analysis and the overall diagnostic accuracy in characterization of FLLs was as follows: pooled sensitivity, 0.92 (95%CI: 0.91–0.93); pooled specificity, 0.87 (95%CI: 0.86–0.88); diagnostic odds ratio, 104.20 (95%CI: 70.42–154.16). Subgroup analysis indicated higher diagnostic accuracy of the second-generation contrast agents (CAs) than the first-generation CA (Levovist; DOR: 118.27 vs. 62.78). Furthermore, Sonazoid demonstrated the highest diagnostic accuracy among three major CAs (SonoVue, Levovist and Sonazoid; DOR: 118.82 vs. 62.78 vs. 227.39). No potential publication bias was observed of the included studies.
Conclusion
CEUS is an accurate tool to stratify the risk of malignancy in FLLs. The second-generation CAs, especially Sonazoid may greatly improve diagnostic performance.
Key Points
• CEUS shows excellent diagnostic accuracy in differentiating malignant from benign FLLs.
• The second-generation CAs have higher diagnostic accuracy than first-generation CAs.
• Sonazoid demonstrates the highest diagnostic accuracy among three major CAs.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Accurate diagnosis focal liver lesions (FLLs) remains a dilemma [1, 2], whereas it is essential with regards to intervention and prognosis [3, 4]. The introduction of contrast-enhanced ultrasound (CEUS) with gas-filled microbubbles serving as contrast agents (CAs) has dramatically improved the characterization of FLLs when compared with conventional US (either B-mode or Doppler ultrasound) [5, 6].
All currently commercially available ultrasound CAs consist of an inert gas encapsulated by a shell molecule. The low-solubility gas component determines the major acoustic properties, while the shell mainly affects the stability and durability in blood [7, 8]. When employing an intravenous ultrasound contrast agent, CEUS makes it possible to observe the hemodynamic process in real-time. Advanced low mechanical index technologies along with sophisticated software provide high-resolution real-time contrast-specific imaging for detecting macro- and micro-vascularization in lesions [9]. Almost all malignancies show a contrast wash-out feature in the delayed phase compared to normal liver tissue; reversely benign lesions are typically iso- or hyper-enhancing. Consequently, many clinical studies have proved that CEUS is useful for characterization of FLLs based on the above characteristics [1, 10].
The US Food and Drug Administration finally approved the application of CEUS with SonoVue under the name of Lumason for liver examination in 2016 after years of off-label usage [11]. This license might result in a possible breakthrough in the field of CEUS study. Hence, we carry out a meta-analysis to present the diagnostic value of CEUS in the work-up of FLLs through summarizing the studies so far in order to give related researchers some reference. Additionally, there is a wide variety of contrast agents in the healthcare market, and sonographers are facing numerous choices. As there are still no comparative studies among different CAs published to date, CA selection was often done without any guidance from relevant theories. Therefore, the other aim of our study is to explore the diagnosis performances of different CAs, and then to offer a certain theoretical foundation for clinical practice.
Materials and methods
The systematic review was conducted according to the recommendations of the PRISMA guidelines.
Literature search
A comprehensive search was performed to identify suitable diagnostic studies from electronic databases (the Cochrane Library, PubMed and Web of Science) up to February 10th, 2017. The search terms used in this meta-analysis were as follows: (focal liver lesions OR FLL OR hepatocellular carcinoma OR cholangiocarcinoma OR metastatic hepatic carcinoma OR liver metastases OR liver tumor OR hepatic haemangioma OR focal nodular hyperplasia OR liver adenoma OR liver abscess OR liver neoplasms [Mesh]) AND (contrast-enhanced ultrasound OR contrast-enhanced US OR CEUS). The search had no language restriction, but only full articles written in English were further evaluated. The references of relevant reviews were also manually searched and screened to identify eligible studies.
Two reviewers selected eligible studies independently with disagreements resolved by consensus. The following inclusion criteria were utilized to recognize eligible studies: (1) human patients with suspected FLLs; (2) studies evaluated by CEUS in the differential diagnosis of FLLs; (3) only per-lesion or per-patient statistics had sufficient data to construct a diagnostic table (2×2 table); (4) each study consisted of at least 20 samples; (5) final diagnosis confirmed by histological or close clinical diagnosis with imaging follow-up for at least 6 months; (6) full articles were available and written in English.
Studies were excluded if: (1) types of literature such as reviews, letters, meta-analyses, case reports or editorial articles; (2) fewer than 20 patients; (3) could not provide sufficient data for diagnostic meta-analysis; (4) with FLLs after treatment. When data were presented in more than one study by the same authors, either the most recently published studies or the study with the largest sample size was included.
Data extraction
All selected studies were screened by two reviewers to retrieve the following data: first author’s name, publication year, country of origin, the number of patients, the number of lesions, average age, gender ratio, final diagnosis standard, final diagnosis (the specific disease types and quantities), the number of benign and malignant lesions, average lesion size, CA, true positive (TP), true negative (TN), false positive (FP) and false negative (FN).
Methodology quality assessment
The quality of eligible studies was evaluated by the Quality Assessment of Diagnostic Accuracy Studies (QUADAS) tool by the same reviewers who performed data extraction. Fourteen items (maximum score 14) were included to assess the overall quality of each study.
Statistical analysis
The estimates including sensitivity, specificity, diagnostic odds ratio (DOR), positive likelihood ratio (PLR), negative likelihood ratio (NLR) with corresponding 95% confidence intervals (CIs) are summarized for graphically represent the diagnostic value of CEUS in differentiating malignant from benign lesions in FLLs. Afterwards, the hierarchical summary receiver operating characteristic (HSROC) curve and the area under the curve (AUC) were calculated. The heterogeneity across the studies was assessed by a chi-square test and Q statistic. The random effects model (the DerSimonian Laird method) would be utilized if the heterogeneity was significant (P heterogeneity < 0.05 or I 2 ≥ 50%); otherwise, the fixed effects model (the Mantel–Haenszel method) would be used. The Spearman correlation coefficient was used to investigate the threshold effect. Subgroup analysis and meta-regression analysis were also utilized to further explore the potential sources of heterogeneity. Bias in publication was tested by funnel plots. All statistical analyses were performed by Meta-Disc (version 1.4) and STATA (version 13.1).
Results
Study identification and selection
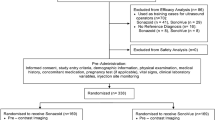
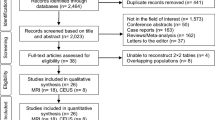
The initial databases search with the above strategy yielded a total of 4579 potentially relevant studies (29 from the Cochrane Library, 2642 from PubMed and 1908 from Web of Science). After 311 duplicated studies were deleted, 4268 potential studies remained. 4025 studies were further excluded according to the inclusion criteria by screening the titles and abstracts, and the remaining 243 studies were left for full text review. In accordance with the inclusion criteria, a further 186 records were excluded due to various reasons (seen in Fig. 1), leaving 57 eligible [1, 10, 12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66] studies selected in this meta-analysis. The detailed flow chart is shown in Fig. 1.
Characteristics of eligible studies
Basic characteristics of eligible studies are presented in Table 1 with the publication year from 2001 to 2017 (Fig. 2A). 35 studies were conducted in Western countries (10 from Germany, 9 from Italy and 16 from other Western countries), and the remaining 22 studies were conducted in Asian countries (10 from China, 8 from Japan and 4 from other Asian countries; Fig. 2B). The numbers of both patients and lesions varied from 30 to 1328. The average age of the included patients ranged from 13 (one study conducted in paediatric patients) to 70. Most of the malignant lesions were hepatocellular carcinomas (HCCs) and liver metastases, and most of the benign lesions were haemangiomas and regenerative or dysplastic nodules. The first-generation contrast agent (Levovist) was used in 12 studies, and the second-generation contrast agents were utilized in the other 45 studies [39 studies used SonoVue, 4 studies used Sonazoid (a particular US contrast agent, which has late liver-specific phase) and the remaining 2 studies used Definity and Optison]. QUADAS scores are also summarized in Table 1.
Diagnostic accuracy
The pooled sensitivity and specificity of CEUS for characterization of FLLs were 0.92 (95%CI: 0.91–0.93), and 0.87 (95%CI: 0.86–0.88), respectively (Fig. 3). The pooled PLR and NLR of CEUS were 7.38 (95%CI: 5.86–9.31) and 0.09 (95%CI: 0.07–0.11), respectively (Fig. S1). And the pooled DOR was 104.20 (95%CI: 70.42–154.16; Fig. S2). Figure 4 illustrates the SROC curve with AUC to be 0.9665. The Spearman correlation coefficient showed there was no significant correlation between sensitivity and specificity (r = -0.158, P = 0.242), which indicated no threshold effect.
Subgroup and meta-regression analysis
Several potential factors were explored to illustrate their capabilities in affecting the diagnostic accuracy (Table 2, Fig. 5). Since the DOR is a single entity which combines the data from sensitivity and specificity, we calculated pooled DOR to present the diagnostic accuracy. As seen in Table 2, number of lesions and CA type used in CEUS both greatly influenced the diagnostic accuracy. The DOR value of the big-sample-size group (number of lesion ≥100) appeared more improved than the small-sample-size group (number of lesion < 100; 135.86 vs. 58.19). Heterogeneity was still observed in the big-sample-size group (I 2 = 84.3%), while it was greatly reduced in the small-sample-size group (I 2 = 39.1%). CA type also affected the diagnostic accuracy. Because Definity was only applied in one study, as was Optison, the pooled DORs of these CAs could not be calculated in subgroup analysis. After eliminating these two types, Sonazoid had the highest DOR (DOR = 227.39), while Levovist had the lowest DOR (DOR = 62.78). Even more remarkable was the fact that heterogeneity was almost eliminated in the Sonazoid group (I 2 = 15.5%). Nevertheless, heterogeneity still existed in SonoVue and Levovist. When dividing the included studies according to different generations of CAs, the subgroup result demonstrated the second-generation CAs had higher diagnostic accuracy than the first-generation CA (Levovist; DOR: 118.27 vs. 62.78). However, heterogeneity still existed in both groups.
Meta-regression analysis was performed to take all the above factors into account. As shown in Table 3, none of the factors (including region, number of lesions and CA type) was the major source of heterogeneity.
Publication bias
Funnel plots were created to assess the publication bias of the eligible studies. As seen in Fig. 6, the plot was symmetric, indicating that there was no potential publication bias for the included studies (P = 0.630).
Discussion
The results of this meta-analysis showed that CEUS had excellent diagnostic capability in differentiating malignant from benign FLLs. The pooled sensitivity, specificity, DOR, PLR, NLR and AUC for CEUS in characterization of FLLs were 92%, 87%, 104.20, 7.38, 0.09 and 0.9665, respectively. Subgroup analyses demonstrated some factors might affect diagnostic performance such as number of lesions, CA generation and CA type.
Diagnostic performance of the big-sample-size group appeared greatly improved than the small-sample-size group (DOR: 135.86 vs. 58.19). The performance of CEUS is more strongly influenced by the experience of the sonographer compared with CT and MRI. The sonographers in large medical centers with adequate patients tend to have more professional experiences to distinguish FLLs for on-site reading in clinical practice [12].
Another major factor which greatly influenced the diagnostic accuracy of CEUS was the various kinds of CAs used in applications. Ultrasonic CAs have unique structures, consisting of inert gas and a shell molecule. Since the lifetime of air bubbles is very short, soft-shell materials are used to stabilize the CA, as well as improve the nonlinear oscillation. The terms “first- and second-generation ultrasound CA” are usually used to differentiate CAs, which are determined by different kinds of inert gas [7]. Though that's a bit of a simplification, in fact, the development of a second generation of ultrasound CAs leads to near complete disappearance of first-generation CAs on account of greatly improved image quality and effectiveness [7, 67]. In our study, the first-generation CA (Levovist) was used in 12 studies, and the second-generation CAs were utilized in the remaining 45 studies. The first-generation CA (Levovist) was used between 2001 to 2009; then the second-generation CAs replaced it entirely. Subgroup analysis indicated higher diagnostic accuracy of the second-generation CAs than the first-generation CA, Levovist (DOR: 118.27 vs. 62.78). The perfect DOR of second-generation CAs illustrated CA upgrade benefited diagnostic efficacies of FLLs.
Among the second-generation ultrasound CAs, Sonazoid is a particular kind. The unique feature of Sonazoid is the accumulation property in the reticuloendothelial system (RES), such as liver and spleen [68]. This phenomenon might involve the Kupffer cells, which present in the hepatic parenchyma. As the Kupffer cells do not exist in malignant lesions, the contrast-enhanced images can easily elucidate the difference of contrast effect between the malignant lesion from normal parenchyma or benign lesion in the post-vascular phase (also known as Kupffer phase) [9, 69]. This late liver-specific phase lasts from around 6 to 10 min to over 60 min. The advent of Sonazoid has become a big breakthrough in CEUS practice of characterizing FLLs. However, it is only available in Japan, South Korea and Norway, so far [9]. SonoVue, another kind of second-generation CA, is widely used in most countries and regions [2]. In our meta-analysis, we evaluated the diagnostic value of CEUS in differentiating malignant from benign FLLs, meanwhile, different kinds of CAs were explored for their diagnostic capabilities. Since no comparative studies between Sonazoid and SonoVue are available at present, our study may offer an evidence-based basis for clinical practice. In our meta-analysis, the liver-specific contrast agent (Sonazoid) was only utilized in 4 studies, much less than SonoVue (utilized in 39 studies). Nevertheless, Sonazoid demonstrated the highest diagnostic accuracy among three major CAs (SonoVue, Levovist and Sonazoid) used in CEUS practice (DOR: 118.82 vs. 62.78 vs. 227.39). The above results revealed that Sonazoid was an outstanding CA; however,it still needs global research to verify its diagnostic ability. Marked heterogeneity was found among the different studies. To deal with this issue, the Spearman correlation coefficient, subgroup analyses and meta regression were combined to detect the sources of heterogeneity. Number of lesions and CA type might contribute to heterogeneity of included studies according to subgroup analyses. Heterogeneity was mainly observed in the big-sample-size group and non-Sonazoid group. However, synthetic regression analysis did not provide evidence supporting the above results. This might be due to the multivariate factors involved in this clinical diagnostic procedure we were unable to statistically analyse. For example, Fracanzani’s [66] study indicated that the vascularity in a small nodule could not be easily assessed by CEUS. But since the data on small nodules couldn’t be obtained in most of the eligible studies, the diagnostic value of CEUS for small FLLs could not be estimated. Given that, the heterogeneity within our study may have influenced the reliability of our results. There are some limitations in this meta-analysis. Firstly, the performance of CEUS is strongly influenced by the experience of the sonographer. Heterogeneity among studies might not be fully eliminated. Secondly, in obese patients, or when the lesion is very deep, the lesion might be difficult to assess. This intrinsic limitation of CEUS might decrease the diagnostic performance to some extent. Thirdly, US techniques have evolved over the last decade; low mechanical index imaging along with phase inversion mode greatly improved spatial resolution [70]. This would result in significantly improved diagnostic capacity in recent studies compared to studies without these techniques. Lastly, meta regression failed to reveal the source of heterogeneity presented in this meta-analysis. The consequences might impact the credibility of this study, highlighting that further research is most pressing.
With regard to the above results, our meta-analysis indicates that CEUS has an outstanding performance in differentiating malignant from benign FLLs with both high sensitivity and specificity. The usage of second-generation CAs, especially Sonazoid, greatly promoted the diagnostic accuracy of CEUS. As CEUS becomes more widely available in the future, it’s role will increase in managing patients with FLLs.
Abbreviations
- CEUS:
-
Contrast-enhanced ultrasound
- FLLs:
-
Focal liver lesions
- CAs:
-
Contrast agents
- CA:
-
Contrast agent
- QUADAS:
-
Quality Assessment of Diagnostic Accuracy Studies
- TP:
-
True positive
- TN:
-
True negative
- FP:
-
False positive
- FN:
-
False negative
- DOR:
-
Diagnostic odds ratio
- PLR:
-
Positive likelihood ratio
- NLR:
-
Negative likelihood ratio
- CIs:
-
Confidence intervals
- HSROC:
-
Hierarchical summary receiver operating characteristic
- AUC:
-
Area under the curve
- RDOR:
-
Relative diagnostic odds ratio
- UL:
-
Upper limit
- LL:
-
Lower limit
- HCCs:
-
Hepatocellular carcinomas
- RES:
-
Reticuloendothelial system
References
Gatos I, Tsantis S, Spiliopoulos S et al (2015) A new automated quantification algorithm for the detection and evaluation of focal liver lesions with contrast-enhanced ultrasound. Med Phys 42:3948–3959
Salvatore V, Borghi A, Piscaglia F (2012) Contrast-enhanced ultrasound for liver imaging: recent advances. Curr Pharm Des 18:2236–2252
Lencioni R, Piscaglia F, Bolondi L (2008) Contrast-enhanced ultrasound in the diagnosis of hepatocellular carcinoma. J Hepatol 48:848–857
Deng H, Shi H, Lei J, Hu Y, Li G, Wang C (2016) A meta-analysis of contrast-enhanced ultrasound for small hepatocellular carcinoma diagnosis. J Cancer Res Ther 12:C274–C276
Yoon JH, Park JW, Lee JM (2016) Noninvasive Diagnosis of Hepatocellular Carcinoma: Elaboration on Korean Liver Cancer Study Group-National Cancer Center Korea Practice Guidelines Compared with Other Guidelines and Remaining Issues. Korean J Radiol 17:7–24
Guang Y, Xie L, Ding H, Cai A, Huang Y (2011) Diagnosis value of focal liver lesions with SonoVue®-enhanced ultrasound compared with contrast-enhanced computed tomography and contrast-enhanced MRI: a meta-analysis. J Cancer Res Clin Oncol 137:1595–1605
Ignee A, Atkinson NS, Schuessler G, Dietrich CF (2016) Ultrasound contrast agents. Endosc Ultrasound 5:355–362
Paefgen V, Doleschel D, Kiessling F (2015) Evolution of contrast agents for ultrasound imaging and ultrasound-mediated drug delivery. Front Pharmacol 15:197
Maruyama H, Sekimoto T, Yokosuka O (2016) Role of contrast-enhanced ultrasonography with Sonazoid for hepatocellular carcinoma: evidence from a 10-year experience. J Gastroenterol 51:421–433
Kondo S, Takagi K, Nishida M et al (2017) Computer-Aided Diagnosis of Focal Liver Lesions Using Contrast-Enhanced Ultrasonography With Perflubutane Microbubbles. IEEE Trans Med Imaging 36:1427–1437
Seitz K, Strobel D (2016) A Milestone: Approval of CEUS for Diagnostic Liver Imaging in Adults and Children in the USA. Ultraschall Med 37:229–232
Hohmann J, Skrok J, Basilico R et al (2012) Characterisation of focal liver lesions with unenhanced and contrast enhanced low MI real time ultrasound: on-site unblinded versus off-site blinded reading. Eur J Radiol 81:e317–e324
Shan QY, Chen LD, Zhou LY et al (2016) Focal Lesions in Fatty Liver: If Quantitative Analysis Facilitates the Differentiation of Atypical Benign from Malignant Lesions. Sci Rep 6:18640
Quaia E, De Paoli L, Angileri R, Cabibbo B, Cova MA (2014) Indeterminate solid hepatic lesions identified on non-diagnostic contrast-enhanced computed tomography: assessment of the additional diagnostic value of contrast-enhanced ultrasound in the non-cirrhotic liver. Eur J Radiol 83:456–462
Ryu SW, Bok GH, Jang JY et al (2014) Clinically useful diagnostic tool of contrast enhanced ultrasonography for focal liver masses: comparison to computed tomography and magnetic resonance imaging. Gut Liver 8:292–297
Sporea I, Badea R, Popescu A et al (2014) Contrast-enhanced ultrasound (CEUS) for the evaluation of focal liver lesions - a prospective multicenter study of its usefulness in clinical practice. Ultraschall Med 35:259–266
Zhang P, Zhou P, Tian SM, Qian Y, Li JL, Li RZ (2014) Diagnostic performance of contrast-enhanced sonography and acoustic radiation force impulse imaging in solid liver lesions. J Ultrasound Med 33:205–214
Jacob J, Deganello A, Sellars ME, Hadzic N, Sidhu PS (2013) Contrast enhanced ultrasound (CEUS) characterization of grey-scale sonographic indeterminate focal liver lesions in pediatric practice. Ultraschall Med 34:529–540
Streba CT, Ionescu M, Gheonea DI et al (2012) Contrast-enhanced ultrasonography parameters in neural network diagnosis of liver tumors. World J Gastroenterol 18:4427–4434
Anaye A, Perrenoud G, Rognin N et al (2011) Differentiation of focal liver lesions: usefulness of parametric imaging with contrast-enhanced US. Radiology 261:300–310
Bartolotta TV, Taibbi A, Midiri M, Matranga D, Solbiati L, Lagalla R (2011) Indeterminate focal liver lesions incidentally discovered at gray-scale US: role of contrast-enhanced sonography. Investig Radiol 46:106–115
Giorgio A, Calisti G, di Sarno A et al (2011) Characterization of dysplastic nodules, early hepatocellular carcinoma and progressed hepatocellular carcinoma in cirrhosis with contrast-enhanced ultrasound. Anticancer Res 31:3977–3982
Strobel D, Bernatik T, Blank W et al (2011) Diagnostic accuracy of CEUS in the differential diagnosis of small (≤20 mm) and subcentimetric (≤10 mm) focal liver lesions in comparison with histology. Results of the DEGUM multicenter trial. Ultraschall Med 32:593–597
Beaton C, Cochlin D, Kumar N (2010) Contrast enhanced ultrasound should be the initial radiological investigation to characterise focal liver lesions. Eur J Surg Oncol 36:43–46
Ooi CC, Low SC, Schneider-Kolsky M et al (2010) Diagnostic accuracy of contrast-enhanced ultrasound in differentiating benign and malignant focal liver lesions: a retrospective study. J Med Imaging Radiat Oncol 54:421–430
Rognin NG, Arditi M, Mercier L et al (2010) Parametric imaging for characterizing focal liver lesions in contrast-enhanced ultrasound. IEEE Trans Ultrason Ferroelectr Freq Control 57:2503–2511
von Herbay A, Westendorff J, Gregor M (2010) Contrast-enhanced ultrasound with SonoVue: differentiation between benign and malignant focal liver lesions in 317 patients. J Clin Ultrasound 38:1–9
Inoue T, Kudo M, Maenishi O et al (2009) Value of liver parenchymal phase contrast-enhanced sonography to diagnose premalignant and borderline lesions and overt hepatocellular carcinoma. AJR Am J Roentgenol 192:698–705
Jang HJ, Kim TK, Wilson SR (2009) Small nodules (1-2 cm) in liver cirrhosis: characterization with contrast-enhanced ultrasound. Eur J Radiol 72:418–424
Liu GJ, Xu HX, Xie XY et al (2009) Does the echogenicity of focal liver lesions on baseline gray-scale ultrasound interfere with the diagnostic performance of contrast-enhanced ultrasound? Eur Radiol 19:1214–1222
Moriyasu F, Itoh K (2009) Efficacy of perflubutane microbubble-enhanced ultrasound in the characterization and detection of focal liver lesions: phase 3 multicenter clinical trial. AJR Am J Roentgenol 193:86–95
Quaia E, Alaimo V, Baratella E, Medeot A, Midiri M, Cova MA (2009) The added diagnostic value of 64-row multidetector CT combined with contrast-enhanced US in the evaluation of hepatocellular nodule vascularity: implications in the diagnosis of malignancy in patients with liver cirrhosis. Eur Radiol 19:651–663
Sugimoto K, Shiraishi J, Moriyasu F, Doi K (2009) Computer-aided diagnosis of focal liver lesions by use of physicians' subjective classification of echogenic patterns in baseline and contrast-enhanced ultrasonography. Acad Radiol 16:401–411
Trillaud H, Bruel JM, Valette PJ et al (2009) Characterization of focal liver lesions with SonoVue-enhanced sonography: international multicenter-study in comparison to CT and MRI. World J Gastroenterol 15:3748–3756
Wang WP, Wu Y, Luo Y et al (2009) Clinical value of contrast-enhanced ultrasonography in the characterization of focal liver lesions: a prospective multicenter trial. Hepatobiliary Pancreat Dis Int 8:370–376
Zuber-Jerger I, Schacherer D, Woenckhaus M, Jung EM, Schölmerich J, Klebl F (2009) Contrast-enhanced ultrasound in diagnosing liver malignancy. Clin Hemorheol Microcirc 43:109–118
D'Onofrio M, Faccioli N, Zamboni G et al (2008) Focal liver lesions in cirrhosis: value of contrast-enhanced ultrasonography compared with Doppler ultrasound and alpha-fetoprotein levels. Radiol Med 113:978–991
Hatanaka K, Kudo M, Minami Y, Maekawa K (2008) Sonazoid-enhanced ultrasonography for diagnosis of hepatic malignancies: comparison with contrast-enhanced CT. Oncology 75:42–47
Shiraishi J, Sugimoto K, Moriyasu F, Kamiyama N, Doi K (2008) Computer-aided diagnosis for the classification of focal liver lesions by use of contrast-enhanced ultrasonography. Med Phys 35:1734–1746
Strobel D, Seitz K, Blank W et al (2008) Contrast-enhanced ultrasound for the characterization of focal liver lesions--diagnostic accuracy in clinical practice (DEGUM multicenter trial). Ultraschall Med 29:499–505
Wang ZL, Tang J, Weskott HP et al (2008) Undetermined focal liver lesions on gray-scale ultrasound in patients with fatty liver: characterization with contrast-enhanced ultrasound. J Gastroenterol Hepatol 23:1511–1519
Catala V, Nicolau C, Vilana R et al (2007) Characterization of focal liver lesions: comparative study of contrast-enhanced ultrasound versus spiral computed tomography. Eur Radiol 17:1066–1073
Celli N, Gaiani S, Piscaglia F et al (2007) Characterization of liver lesions by real-time contrast-enhanced ultrasonography. Eur J Gastroenterol Hepatol 19:3–14
Dai Y, Chen MH, Yin SS et al (2007) Focal liver lesions: can SonoVue-enhanced ultrasound be used to differentiate malignant from benign lesions? Investig Radiol 42:596–603
Jung EM, Clevert DA, Schreyer AG et al (2007) Evaluation of quantitative contrast harmonic imaging to assess malignancy of liver tumors: a prospective controlled two-center study. World J Gastroenterol 13:6356–6364
Quaia E, D'Onofrio M, Cabassa P et al (2007) Diagnostic value of hepatocellular nodule vascularity after microbubble injection for characterizing malignancy in patients with cirrhosis. AJR Am J Roentgenol 189:1474–1483
Xu J, Wu Y, Dong F (2007) Clinical value of contrast-enhanced ultrasound in differentiating benign and malignant focal liver lesions. J Huazhong Univ Sci Technolog Med Sci 27:703–705
Leen E, Ceccotti P, Kalogeropoulou C, Angerson WJ, Moug SJ, Horgan PG (2006) Prospective multicenter trial evaluating a novel method of characterizing focal liver lesions using contrast-enhanced sonography. AJR Am J Roentgenol 186:1551–1559
Nicolau C, Vilana R, Catalá V et al (2006) Importance of evaluating all vascular phases on contrast-enhanced sonography in the differentiation of benign from malignant focal liver lesions. AJR Am J Roentgenol 186:158–167
Wang JH, Lu SN, Hung CH et al (2006) Small hepatic nodules (< or =2 cm) in cirrhosis patients: characterization with contrast-enhanced ultrasonography. Liver Int 26:928–934
Wu W, Chen MH, Yin SS et al (2006) The role of contrast-enhanced sonography of focal liver lesions before percutaneous biopsy. AJR Am J Roentgenol 187:752–761
Xu HX, Liu GJ, Lu MD et al (2006) Characterization of small focal liver lesions using real-time contrast-enhanced sonography: diagnostic performance analysis in 200 patients. J Ultrasound Med 25:349–361
Kim SH, Lee JM, Lee JY et al (2005) Value of contrast-enhanced sonography for the characterization of focal hepatic lesions in patients with diffuse liver disease: receiver operating characteristic analysis. AJR Am J Roentgenol 184:1077–1084
Bryant TH, Blomley MJ, Albrecht T et al (2004) Improved characterization of liver lesions with liver-phase uptake of liver-specific microbubbles: prospective multicenter study. Radiology 232:799–809
Dietrich CF, Ignee A, Trojan J et al (2004) Improved characterisation of histologically proven liver tumours by contrast enhanced ultrasonography during the portal venous and specific late phase of SHU 508A. Gut 53:401–405
Klein D, Jenett M, Gassel HJ, Sandstede J, Hahn D (2004) Quantitative dynamic contrast-enhanced sonography of hepatic tumors. Eur Radiol 14:1082–1091
Peschl R, Werle A, Mathis G (2004) Differential diagnosis of focal liver lesions in signal-enhanced ultrasound using BR 1, a second-generation ultrasound signal enhancer. Dig Dis 22:73–80
Quaia E, Calliada F, Bertolotto M et al (2004) Characterization of focal liver lesions with contrast-specific US modes and a sulfur hexafluoride-filled microbubble contrast agent: diagnostic performance and confidence. Radiology 232:420–430
Suzuki S, Iijima H, Moriyasu F et al (2004) Differential diagnosis of hepatic nodules using delayed parenchymal phase imaging of Levovist contrast ultrasound: comparative study with SPIO-MRI. Hepatol Res 29:122–126
von Herbay A, Vogt C, Willers R, Häussinger D (2004) Real-time imaging with the sonographic contrast agent SonoVue: differentiation between benign and malignant hepatic lesions. J Ultrasound Med 23:1557–1568
Isozaki T, Numata K, Kiba T et al (2003) Differential diagnosis of hepatic tumors by using contrast enhancement patterns at US. Radiology 229:798–805
Karabacakoglu A, Karakose S, Cil AS, Kaya A (2003) Contrast media-enhanced power Doppler sonography for evaluation of hemangiomas and malignant tumors in the liver. J Gastroenterol Hepatol 18:92–98
Strobel D, Raeker S, Martus P, Hahn EG, Becker D (2003) Phase inversion harmonic imaging versus contrast-enhanced power Doppler sonography for the characterization of focal liver lesions. Int J Color Dis 18:63–72
Beissert M, Delorme S, Mutze S et al (2002) Comparison of B-mode and conventional colour/power Doppler ultrasound, contrast-enhanced Doppler ultrasound and spiral CT in the diagnosis of focal lesions of the liver: Results of a multicentre study. Ultraschall Med 23:245–250
von Herbay A, Vogt C, Häussinger D (2002) Late-phase pulse-inversion sonography using the contrast agent levovist: differentiation between benign and malignant focal lesions of the liver. AJR Am J Roentgenol 179:1273–1279
Fracanzani AL, Burdick L, Borzio M et al (2001) Contrast-enhanced Doppler ultrasonography in the diagnosis of hepatocellular carcinoma and premalignant lesions in patients with cirrhosis. Hepatology 34:1109–1112
Perera RH, Hernandez C, Zhou H, Kota P, Burke A, Exner AA (2015) Ultrasound imaging beyond the vasculature with new generation contrast agents. Wiley Interdiscip Rev Nanomed Nanobiotechnol 7:593–608
Yanagisawa K, Moriyasu F, Miyahara T, Yuki M, Iijima H (2007) Phagocytosis of ultrasound contrast agent microbubbles by Kupffer cells. Ultrasound Med Biol 33:318–325
Claudon M, Cosgrove D, Albrecht T et al (2008) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS) -. update 2008. Ultraschall Med 29:28–44
Jang HJ, Yu H, Kim TK (2009) Contrast-enhanced ultrasound in the detection and characterization of liver tumors. Cancer Imaging 9:96–103
Funding
This study has received funding by the Youth Science Foundation of the Second Hospital Center Laboratory of Tianjin Medical University (2016YDEY01), Science Foundation of Tianjin Medical University (2016KYZQ06 and 2014KYM15), Foundation of Tianjin Health and Family Planning Commission (16KG115).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Guarantor
The scientific guarantor of this publication is Xuening Zhang.
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Statistics and biometry
No complex statistical methods were necessary for this paper.
Informed consent
Written informed consent was not required for this study because the study concerns a meta-analysis.
Ethical approval
Institutional review board approval was not required because the study concerns a meta-analysis.
Methodology
• diagnostic study
• performed at one institution
Additional information
Menglin Wu and Liang Li are co-first authors.
Rights and permissions
About this article
Cite this article
Wu, M., Li, L., Wang, J. et al. Contrast-enhanced US for characterization of focal liver lesions: a comprehensive meta-analysis. Eur Radiol 28, 2077–2088 (2018). https://doi.org/10.1007/s00330-017-5152-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-5152-x