Abstract
Liver tumors are defined using quantitative dynamic contrast-enhanced ultrasound compared to histological diagnosis, respectively, long-term follow-ups. Forty-two focal liver lesions in 39 patients were examined by contrast harmonic imaging over a period of 2 min after bolus injection of 10-ml galactose-based contrast agent. Vascular enhancement was quantified by using a dedicated software that allowed us to place representative regions of interest (ROI) in the center of the lesion, in the complete lesion, in regular liver parenchyma and in representative liver vessels (artery, vein and portal vein). Peak enhancement was judged to be either in the arterial, portal venous or in the late phase of liver perfusion. The lesion was described as hypovascular, isovascular and hypervascular compared to liver parenchyma. Contrast uptake was described as centrifugal or centripetal and peripheral or homogenous, respectively. Characterization of the lesions was performed unenhanced and after contrast by four independent specialists unaware of histology. Diagnosis of malignancy was evaluated by using a receiver operating characteristic (ROC) analysis, also overall accuracy, average sensitivity, specificity and negative and positive predictive values were calculated. Interobserver agreement was defined by the Kappa statistics. Histologic examination revealed 29 malignant [hepatocellular carcinoma (HCC), n=11; cholangiocellular carcinoma (CCC), n=1; lymphoma, n=1; metastases, n=16)] and 7 benign [hemangioma, n=1; focal nodular hyperplasia (FNH), n=4, adenoma, n=2)] lesions. Six benign lesions (hemangioma n=1; FNH n=5) were proved by long-term follow-up. ROC analysis regarding the diagnosis of malignancy showed values from 0.43 to 0.62 (mean 0.57) before and from 0.70 to 0.80 (mean 0.75) after contrast agent, respectively. The average values for sensitivity, specificity, accuracy and negative and positive predictive values were 66, 26, 62, 45 and 73% unenhanced and 83, 49, 73, 65 and 82% after contrast, respectively. The interobserver agreement was 0.54 and 0.65 for unenhanced and enhanced examinations, respectively. Quantitative dynamic contrast-enhanced sonography improves the diagnosis of malignancy in liver lesions.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Gray-scale sonography is a sensitive screening technique for patients suspected of having liver tumors. However, a specific liver tumor diagnosis can rarely be established based on the gray-scale sonographic characteristics. Since the introduction of color Doppler imaging, many studies have been performed to depict the vascularization pattern of liver lesions in order to understand the lesion nature [1–4]. Although color Doppler sonography has opened up new diagnostic possibilities, it is limited in its ability to evaluate low-velocity blood flow in very small intratumoral vessels. Particularly small hepatic lesions and lesions distant to the transducer are difficult to examine due to the low intensity of Doppler signals or an insufficient Doppler shift. This lack of information has been compensated with the development of ultrasound contrast agents. Due to the increase of the signal-to-noise ratio, intravascular ultrasound contrast agents allow a more complete display of the vascularization pattern of the tumor [5–9]. By using contrast agents, focal liver lesions can be distinguished by their vascular pattern, e.g., the typical spoke-wheel sign of the FNH and the peripheral enhancement of the hemangiomas [10–16]. Recently, a highly sensitive microbubble-specific sonography technique called phase inversion has emerged; it displays nonlinear signals from microbubbles in B-Mode. This technique uses two sonographic pulses that are phase-shifted by 180° for one image frame. Linear signals from the two pulses will cancel each other, and the image is produced exclusively by the nonlinear scattering from the microbubbles [17, 18].
Previous studies using a galactose-based contrast agent focused on the detection of focal liver lesions, e.g., with stimulated acoustic emissions (SAE). This approach is based on the contrast agent’s unique characteristic to remain within the liver parenchyma even after blood pool clearance. Although the precise mechanism of the late microbubble accumulation is unknown, the temporal course and the distribution mimic uptake of liver-specific MR contrast agents with an affinity to the reticuloendothelial system. The disruption of the microbubbles caused by using a high mechanical index leads to a bright signal from normal liver parenchyma, whereas, e.g., liver metastases appear as a clear defect [19–21]. Other studies demonstrated an increase in the diagnostic accuracy for characterization of liver lesions by performing a dynamic sonography during the vascular phase of a galactose-based contrast agent [22, 23]. However, until now only one study has been performed to obtain the perfusion pattern of focal liver lesions by evaluating the echogenicity time changes after bolus injection of a galactose-based contrast agent [9]. With the development of a specific evaluation software, now it is possible to record a sequence of contrast-enhanced US over a period of 2 min, which allows to judge each phase of the tumor perfusion quantitatively. Thus, the purpose of this study was to evaluate the diagnostic accuracy of contrast-enhanced ultrasound by using quantitative parameters compared to non-contrast gray-scale sonography.
Subjects and methods
Thirty-nine patients with 42 solid liver lesions were enrolled in this prospective study (14 women and 25 men; age range, 21–86 years, mean age, 56 years ±18.3) with (n=20) or without (n=19) known malignancy. The study was approved by the ethics committee of our institution, and all patients gave informed written consent. Inclusion criterion was the presence of at least one focal liver lesion detected by US, CT or MRI, respectively. In patients with more than one focal lesion, all lesions were examined and judged separately. The final diagnosis of all malign lesions is listed in Table 1. Thirty-six lesions were histologically proven by surgical resection and CT-guided biopsy in 13 lesions and 23 lesions, respectively. The remaining six benign lesions were considered benign by 6-month ultrasound follow-up.
The size of the focal liver lesions ranged from 1 to 15.5 cm (mean size 4.6±2.8 cm). In the 16 cases of metastatic cancer, the primarily affected organ was the colon (n=10), the skin (n=3, melanoma), the lung (n=1), pancreatic gland (n=1) and one neuroendocrine carcinoma of unknown primary. The results of the contrast-enhanced ultrasound examination had no impact on the clinical decisions.
Method of dynamic sonography
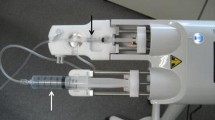
Scanning was performed by one experienced radiologist using a Sonoline Elegra scanner (Siemens, Issaquah, WA) with a convex 3.5-MHz transducer. Before injection of the ultrasound contrast agent, all patients underwent conventional sonography using tissue harmonic imaging (THI) in longitudinal and transverse sections for determination of the best scanning view to visualize the tumor and the nearest portal branch/liver vein. After baseline scanning, a bolus injection of 10 ml Levovist (Schering AG, Berlin) at 300 mg/ml into an antecubital vein was performed, followed by a 10-ml saline chaser bolus. Simultaneously, the evaluation software Axius ACQ (Siemens, Issaquah, WA) was started to obtain a baseline scanning. To minimize microbubble disruption, a low acoustic output was used as defined by a mechanical index between 0.3 and 0.5 and a low frame rate of 2 per s for imaging of the vascular-phase images. Using these adjustments, dynamic sonography was possible over a period of 2 min, limited due to the capacity of the ultrasound device. In this period of time, all perfusion phases of the liver lesions (arterial, portal-venous and late phase) were evaluated. All examinations were made in breathhold technique and were paused if the patient had to breath, without stopping the evaluation software. The whole examination was recorded on videotape and key pictures (e.g., maximum contrast uptake of the liver lesion) were digitally stored (Ali UltraPACS, A.L.I. Technologies, Inc., Canada). The average examination time was 20 min.
Image analysis
Six regions of interest (ROI) were used to define the perfusion of the liver lesions as well as their contrast uptake. The perfusion was judged according to the enhancement of the liver vessels and was divided into three phases: the arterial phase, the portal venous phase and the late phase. The time period between the injection and the enhancement of the liver arteries was defined as the arterial phase, followed by the enhancement of the portal branches (portal venous phase) and the enhancement of the liver veins (late phase). The perfusion patterns of the lesion were determined by two ROIs, one including the entire lesion, and one placed in the center of the lesion. A third ROI was positioned in normal liver parenchyma. The ROIs 4–6 were placed in liver vessels: this means a liver vein, portal branch or liver artery. The size of the operator-dependent ROIs depended on the lesion size and ranged between 784 and 49,580 pixels for the entire lesion, and between 450 and 6,216 pixels for the center of the lesion, respectively. Sizes of the ROIs placed in liver parenchyma and vessels were in the range of 500–3,000 pixels. Motion artifacts and larger blood vessels have been deleted from the evaluation, avoiding measurement errors. Enhancement of the lesions was defined qualitatively as hypovascular, isovascular or hypervascular in comparison to normal liver parenchyma for no absolute quantification (e.g., dB) was given by the software (e.g., hypervascular if the lesion appeared more echoic than adjacent liver parenchyma after contrast). Contrast uptake was described as centrifugal (contrast uptake from the center of the lesion towards the periphery) or centripetal (contrast uptake from the periphery of the lesion towards the center) and peripheral or homogenous, respectively.
Evaluation by different readers
The examinations with and without contrast enhancement were evaluated by four radiologists specialized in sonography. The readers were not involved in the examination of the patients and were unaware of the final diagnosis of the tumors or the clinical data of the patients. A receiver-operating characteristic (ROC) analysis was performed to display the discriminatory accuracy of ultrasound concerning whether a focal liver lesion is malign or benign. Confidence of diagnosis was judged as definitely malignant =5, probably malignant =4, indeterminate =3, probably benign =2 and definitely benign =1. Furthermore, the readers were also asked to define the tumor type. Possible diagnoses were adenoma, focal nodular hyperplasia, hemangioma, hepatocellular carcinoma, cholangiocellular carcinoma, metastases, lymphoma, focal fatty sparing or indeterminate, respectively. For the first read, only one unenhanced key picture of each liver lesion was evaluated. For the second read, 3 months later, information on the contrast enhancement patterns (blood supply, relative perfusion, contrast uptake) was added to the unenhanced key picture. Table 2 shows the typical appearance of focal liver lesions in conventional ultrasound, color Doppler and contrast-enhanced ultrasound. Those typical findings were used to determine whether a lesion was malign or benign.
Statistical analysis
ROC curves for each observer and for each study (unenhanced and enhanced) were calculated by using SPSS 10.0 (SPSS, Inc., Chicago, IL). The area under each ROC curve was used to indicate the overall performance of imaging techniques and observers [24, 25]. Additionally, overall accuracy, average values for sensitivity, specificity and positive and negative predictive values (unenhanced and enhanced) for the overall detection of malignancy were calculated. Interobserver agreement was defined by the Kappa statistics for unenhanced and contrast-enhanced examinations.
Results
Diagnosis of malignancy
The ROC analysis regarding the diagnosis of malignancy showed an increase with the use of the ultrasound contrast agent from 0.57 (mean) unenhanced to 0.75 (mean). Without using a contrast agent, the diagnosis of malignancy was close to the probability of rate (Fig. 1).The mean overall accuracies for the different readers were 0.62 (unenhanced) and 0.73 (enhanced) (Fig. 2). The mean sensitivities and specificities as well as the positive and negative predictive values are shown in Fig. 3. The interobserver agreement (Kappa statistic) showed an increase from 0.54 to 0.65 after the use of the ultrasound contrast agent. Contrast enhancement patterns of the different lesions are summarized in Table 3. All malignant lesions showed either an arterial (18/29) or a portal venous blood supply (11/29) (Fig. 4, 5). No lesion showed an enhancement in the late phase. Regarding the vascularity, the malignant lesions were either hypervascular (18/29) or hypovascular (10/29), except for one metastasis that was isovascular to the normal liver parenchyma. Except for one HCC, none of the malign lesions showed a centrifugal perfusion pattern. The contrast uptake was homogenous in 15/29 cases and peripheral in 14/29 cases, respectively. Most benign lesions (11/13) had an arterial blood supply, and 2/13 showed a contrast uptake in the late phase (hemangiomas, Fig. 6). Nine out of 13 were hypervascular; 4/13 lesions were hypovascular. No benign lesion was isovascular to normal liver parenchyma. A centrifugal perfusion pattern was found in 7/13 (all FNH). The contrast uptake was homogenous in 11/13, respectively, and peripheral in 2/13 (all hemangiomas).
HCC in a 67-year-old male patient with known liver cirrhosis and hepatitis C. a B-Mode scan shows a hypoechoic, inhomogeneous lesion subcapsular in the right liver lobe. b The Power Mode shows unenhanced irregular tumor vessels in the periphery of the lesion. c Thirty-five seconds after application of the ultrasound enhancer, peripheral irregular tumor vessels can be seen (arrow). d The contrast-enhanced evaluation showed irregular tumor vessels arterially supplied
Metastasis of a neuroendocrine tumor of unknown primary in a 44-year-old male patient. a Unenhanced baseline sonogram shows a 6-cm huge hyperechoic lesion in the right liver lobe. b Arterial phase dynamic sonogram obtained 25 s after contrast injection reveals a peripheral arterial supply of the lesion (single arrow; double-headed arrows = liver artery; X = portal vein). c Quantitative analysis of the lesion regarding the plots 1 and 2 (centre of the lesion and complete lesion) in comparison with the liver arteries (plot 3) reveals an arterial supplied hypervascular tumor
A 47-year-old woman with a hemangioma in the right liver lobe. a A large peripheral hyperechoic mass with central hypoechoic parts is present in segment six on the conventional image. b Quantification of the contrast uptake shows a peripheral uptake in the late phase with a centripetal perfusion. Plot 1 (center of the lesion) shows no significant contrast enhancement during the entire examination. Plot 2 indicates the perfusion pattern of the whole lesion with a late contrast enhancement corresponding with the contrast enhancement of the liver veins (plot 3). Plot 4 shows the early contrast enhancement of the liver arteries
Enhancement patterns of focal liver lesions
Focal nodular hyperplasia
All FNHs (9/9) showed an arterial blood supply with a homogenous contrast uptake in comparison to normal liver parenchyma. Most of the FNH (8/9) were judged as hypervascular, except for one very small FNH (diameter =1 cm), which was judged as hypovascular. In 7/9 cases, a centrifugal contrast perfusion with a spoke-wheel sign (typical finding of a central feeding artery, and a stellate vascular pattern in many cases of FNH) could be detected (Fig. 7).
Histologically confirmed focal nodular hyperplasia (FNH) in an 86-year-old male patient. a The unenhanced B-Mode scan shows a fatty liver with a hypoechoic lesion next to a portal branch in the right liver lobe. b Arterial phase dynamic sonogram obtained after 30 s. The arrow indicates the central scar with the early onset of the ultrasound contrast agent. No enhancement could be seen peripherally. c Dynamic evaluation shows the typical centrifugal perfusion pattern of a FNH with an arterial peak enhancement after 30 s and d a later peak enhancement of the entire lesion after 33 s
Hepatocellular carcinoma
No characteristic perfusion pattern/contrast uptake could be seen within this entity. Six out of 11 showed an arterial blood supply with a peripheral contrast uptake and were judged to be hypervascular in comparison to the normal liver parenchyma. Five out of 11 HCCs showed an homogeneous contrast uptake in the portal venous phase and were hypovascular to the liver parenchyma. A centripetal perfusion pattern could be seen in 10/11 cases.
Metastases
Most of the metastases (10/16) showed an arterial blood supply with a peripheral or homogeneous contrast uptake (8/8). Most of them were judged as hypervascular to the liver parenchyma (11/16) and were hypovascular in four cases and isovascular in one case. No characteristic perfusion pattern/contrast uptake could be seen within this entity. Due to the small numbers of the remaining lesions (hemangioma n=2; adenoma n=2; CCC n=1; lymphoma n=1), no specific perfusion pattern of these lesions have been considered.
Discussion
In the present study, the diagnostic performance of unenhanced and contrast-enhanced ultrasound for the characterization of focal liver lesions was evaluated. The evaluation of the unenhanced images showed poor results. With the use of an ultrasound contrast agent and dynamic quantitative analysis, the differentiation between benign and malign lesions was significantly improved. Furthermore, the dynamic quantitative analysis showed a high diagnostic value in the characterization of hepatic tumors.
In clinical practice, ultrasound of the abdomen and the liver is the first examination in patients with the question of an existing malignancy. It is characterized by a high validity, low costs and widespread availability. However, in most cases, the detection of a focal liver lesion is followed by further examinations, i.e., spiral CT or MRI of the liver. Using these imaging modalities, a more precise characterization of liver lesions is possible by the assessment of morphology, unenhanced density or signal intensity, respectively, and contrast uptake. Criteria of diagnosis for several different liver lesions have been established using both CT and MRI [26–28]. However, several attempts also have been made to characterize liver lesions by ultrasound imaging. Many authors tried to improve the diagnostic accuracy by using the color Doppler Mode or the Power-Mode by depicting the lesion vascularization pattern to understand the lesion’s nature [1–4]. These studies have shown that both, color Doppler as well as the Power-Mode, can provide useful clinical information on a focal liver lesion. Tanaka et al. suggested that specific vascularity patterns could be associated with certain lesions types, e.g., the basket pattern (a fine blood flow network surrounding the tumor nodule) seen in HCCs [29].
Despite recent improvements in color Doppler sonographic equipment, conventional color Doppler is still limited by its lack of sensitivity in the detection of flow in intranodular microvessels or flow in deeply located liver lesions and is limited by motion artifacts (heartbeat, breath motion artifacts). Attempts to improve the color Doppler imaging led to the development of ultrasound contrast agents based on gas-filled microbubbles such as albumin-encapsulated microspheres, saccharide microparticle suspensions and perfluorcarbons [30–32]. The clinical use of these contrast agents was limited by the lack of transpulmonary stability. With the development of microbubble suspensions with transpulmonary stability, researchers were able to detect more intratumoral vessels than by conventional color Doppler. The first transpulmonary contrast agent Levovist (Schering, Berlin), which was originally developed to enhance Doppler signals during an early vascular phase, showed the side effect of accumulating in the normal liver parenchyma during a late liver-specific phase. This effect has been used to detect liver metastasis by using a highly sensitive microbubble-specific sonography technique called phase inversion [20, 21]. Tanaka et al. showed an improvement from 29 to 86% in the detection rate of intratumoral vascularity using a transpulmonary contrast agent in a small series of HCC [31].
Focusing on the characterization of focal liver lesions, Strobel et al. [23] reported an increase in the detection of intratumoral vascularity in metastases from 35 to 71% after the use of an ultrasound contrast agent. The aim of this study was to depict a specific tumor vascularity for any entity and for the differentiation of malign and benign lesions. It was shown that it is possible to differentiate between an FNH and a malign lesion according to their perfusion patterns and the clinical information of the patients. With the use of all modalities of ultrasound (gray-scale sonography, conventional color Doppler and contrast-enhanced color Doppler), a diagnosis was possible in 79% (n=105 lesions). More recently, improvements in the sonographic equipment, e.g., the pulse inversion imaging technique, have made contrast-enhanced ultrasound more sensitive in the detection of the low intensity second harmonics caused by the microbubbles. By performing sequential scans of focal liver lesions comparable to dynamic CT and the use of the new ultrasound techniques, Tanaka et al. judged the liver lesions according to a CT classification proposed by Nino-Murcia et al. with a diagnostic accuracy for the detection of HCCs of 92%, CCC of 90% and hemangiomas of 60%, respectively [22, 26, 33]. However, without quantitative analysis of the enhancement patterns of focal liver lesions the results still remain subjective.
A more promising approach is the quantitative analysis carried out by using a dedicated evaluation software. Quantification can be divided into “passive” and “active” methods [35]. In the passive approach, the passage of a contrast bolus is recorded with minimal microbubble disruption. Thus, low insonating energies are employed. With active approaches, microbubbles are deliberately destroyed. Thus, the replenishment of a tissue can be measured, e.g., in the measurement of myocardial blood flow. There have been approaches to quantify the perfusion of focal liver lesions. Ramnarine et al. stored the contrast-enhanced examination on video tape and performed an evaluation by digitizing it with a personal computer equipped with commercial available software (Adobe Photoshop 4) [33].
In the present study, with the use of the evaluation software it was possible to judge the perfusion pattern of focal liver lesions quantitatively during the whole vascular phase of the liver. The enhancement patterns of dynamic sonography corresponded well to the findings in the dynamic CT [26] as well as in contrast-enhanced ultrasound [5, 8, 9, 22, 34]. For example, characteristic findings such as the homogeneous arterial contrast enhancement of the FNH and the peripheral contrast uptake of the hemangiomas could clearly be visualized. However, only the FNHs (n=9) were clearly distinguishable from the malignant lesions. All other lesions could not be characterized clearly, and a definite differentiation between benign and malign lesions could not be achieved by our study.
Limitations and clinical implications
Evaluation of the interoberserver variability of ultrasound examinations is limited by the dynamic nature of the procedure. Ideally, a serial examination of the patients by all observers should be performed, which is not possible in clinical practice. In the present study, the readers were only given non-dynamic information, i.e., one key picture and the evaluation of the contrast enhancement patterns. For future studies, the presentation of the findings to the readers can be improved by presentation of cine loops with and without contrast enhancement. The examination technique was limited in lesions located deep within the liver or in patients with a fatty liver. In these cases, the signal of the ultrasound contrast agent was too low. Thus, the mechanical index had to be increased, causing SAE effects. Another limitation is that the contrast agent used was the only available agent with transpulmonary stability when the study was initiated. Levovist has to be employed by intermittent high acoustic power imaging to destroy bubbles producing a wideband signal (SAE) [19–21]. The low acoustic power mode, as used in our study, is not suitable for Levovist, which presents low harmonic behavior, while it may be applied to second generation US contrast agents such as a perfluorocarbon-based microbubble contrast agent. Although the study was performed prospectively, the results of contrast-enhanced US had no impact on the clinical decision. Thus, the true performance of contrast-enhanced ultrasound in clinical practice has to be determined in future studies using improved evaluation techniques and new generation contrast agents.
However, the study showed a significant improvement in the definition of liver lesions with the use of contrast enhancement compared to unenhanced ultrasound. Thus, in the future, the use of dynamic contrast-enhanced ultrasound of the liver possibly will reduce further diagnostic procedures such as CT or MRI.
Conclusion
The differentiation between benign and malignant lesions is significantly improved by contrast-enhanced quantitative dynamic ultrasound imaging for the assessment of the contrast enhancement patterns. Thus, this examination technique is superior to the conventional B-Mode. However, further improvement as expected by the introduction of the newer contrast agents is necessary for a reliable definition of liver lesions.
References
Bartolozzi C, Lencioni R (1997) Differentiation of hepatocellular adenoma and focal nodular hyperplasia of the liver: comparison of power Doppler imaging and conventional color Doppler sonography. Eur Radiol 7:1410–1415
Wang LY, Wang JH (1997) Hepatic focal nodular hyperplasia: findings on color Doppler ultrasound. Abdom Imaging 22:178–181
Learch TJ, Ralls PW (1993) Hepatic focal nodular hyperplasia: findings with color Doppler sonography. J Ultrasound Med 12:541–544
Gaiani S, Casali A (2000) Assessment of vascular patterns of small liver mass lesions: value and limitation of the different Doppler ultrasound modalities. Am J Gastroenterol 12:3537–3546
Hosten N, Puls R (1999) Contrast-enhanced power Doppler sonography: Improved detection of characteristic flow patterns in focal liver lesions. J Clin Ultrasound 27:107–115
Maruyama M, Matsutani S (2000) Enhanced color flow images in small hepatocellular carcinoma. Abdom Imaging 25:164–171
Pennisi F, Farina R (1998) Hepatic focal lesions: role of color Doppler ultrasonography with contrast media. Radiol Med 96:579–587
Maresca G, Barbaro B (1994) Color Dopler ultrasonography in the differential diagnosis of focal hepatic lesions. The SH U 508 A (Levovist) experience. Radiol Med 5:41–49
Bertolotto M, Dalla Palma L (2000) Characterization of unifocal liver lesions with pulse inversion harmonic imaging after Levovist injection: preliminary results. Eur Radiol 9:1369–1376
Uggowitzer M, Kugler C (1998) Sonographic evaluation of focal nodular hyperplasias (FNH) of the liver with a transpulmonary galactose-based contrast agent (Levovist). Br J Radiol 71:1026–1032
Wermke W (1998) Tumordiagnostik der Leber mit Echosignalverstärkern. Springer, Berlin Heidelberg New York
Dietrich CH (2000) Signalverstärkte Farbdopplersonographie des Abdomens. Schnetztor, Konstanz
Blomley MJK, Sidhu PS (2001) Do different types of liver lesions differ in their uptake of the microbubble contrast agent SHU-508 A in the late liver phase? Early experience. Radiology 220:661–667
Quaia E, Bertolotto M (2002) Characterization of liver hemangiomas with pulse inversion harmonic imaging. Eur Radiol 12:537–544
Dill-Macky M, Burns P (2002) Focal hepatic masses: enhancement patterns with SHU-508 A and pulse-inversion US. Radiology 222:95–102
Wilson SR, Burns PN (2000) Harmonic hepatic ultrasound with microbubble contrast agent: initial experience showing improved characterization of hemangioma, hepatocellular carcinoma and metastasis. Radiology 215:153–161
Frinking P, Bouakaz A (2000) Ultrasound contrast imaging: current and new potential methods. Ultrasound Med Biol 26:965–975
Jang HJ, Lim H (2000) Ultrasonographic evaluation of focal hepatic lesions: comparison of pulse inversion harmonic, tissue harmonic, and conventional imaging techniques. J Ultrasound Med 19:293–299
Harvey C, Blomley M (2000) Pulse-inversion mode imaging of liver specific microbubbles: improved detection of subcentimetre metastases. Lancet 355:807
Albrecht T, Hoffmann C (2001) Phase-inversion sonography during the liver-specific late phase of contrast enhancement: improved detection of liver metastases. Am J Roentgenol 176:1191–1198
Kim TK, Choi BI (2000) Improved imaging of hepatic metastases with delayed pulse inversion harmonic imaging using a contrast agent SHU 508 A: preliminary study. Ultrasound Med Biol 26:1439–1444
Tanaka S, Ioka T (2001) Dynamic sonography of hepatic tumors. Am J Roentgenol 177:799–805
Strobel D, Krodel U (2000) Clinical evaluation of contrast-enhanced color doppler sonography in the differential diagnosis of liver tumors. J Clin Ultrasound 28:1–13
Oestmann J, Galanski M (1989) ROC: A method to compare the diagnostic performance of imaging systems. Rofo Fortschr Geb Rontgenstr Neuen Bildgeb Verfahr 151:89–92
Hanley J, McNeil B (1882) The meaning and the use of the area under a receiver operating characteristic (ROC) curve. Radiology 143:29–38
Nino-Murcia M, Olcott EW (2000) Focal liver lesions: pattern based classification scheme for enhancement at arterial phase CT. Radiology 215:746–751
King L, Burkill G (2002) MnDPDP enhanced magnetic resonance imaging of focal liver lesions. Clin Radiol 57:1047–1057
Op de Beeck B, Luypaert R (1999) Benign liver lesions: differentiation by magnetic resonance. Eur J Radiol 32:52–60
Tanaka S, Kitamra T (1990) Color Doppler flow imaging of liver tumors. Am J Roentgenol 154:509
Cosgrove D (1996) Ultrasound contrast enhancement of tumors. Clin Radiol 51:44
Leen E, McArdle CS (1996) Ultrasound contrast agents in liver imaging. Clin Radiol 51:35
Schlief R (1996) Developments in echo-enhancing agents. Clin Radiol 51:5
Tanaka S, Kitamara T (1995) Effectiveness of galactose-based intravenous contrast medium on color Doppler sonography of deeply located hepatocellular carcinoma. Ultrasound Med Biol 21:157
Ramnarine K, Kyriakopoulou K (2000) Improved characterisation of focal liver tumours: dynamic power Doppler imaging using NC100100 echo-enhancer. Eur J Ultrasound 11:95–104
Martínez-Noguera A, Montserrat E (2002) Ultrasound imaging of hepatic cirrhosis and chronic hepatitis. Med Imaging Int 12–16
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Klein, D., Jenett, M., Gassel, HJ. et al. Quantitative dynamic contrast-enhanced sonography of hepatic tumors. Eur Radiol 14, 1082–1091 (2004). https://doi.org/10.1007/s00330-004-2299-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-004-2299-z