Abstract
Objectives
To assess the influence of tube potential on radiation dose and image quality of third-generation dual-source coronary CT angiography (CTA) in a phantom simulating an obese patient.
Methods
A thoracic phantom was equipped with tubular inserts containing iodine solution and water. A soft-tissue-equivalent ring around the phantom simulated an obese patient. Images were acquired at tube potentials of 80, 100, 120 and 140 kV with second-generation dual-source CT (DSCT) and 70–150 kV (in 10-kV increments) with third-generation DSCT. Contrast-to-noise ratio (CNR) was calculated and CT dose index was recorded.
Results
With second-generation DSCT, CNR was highest for 120 kV (19.0) and decreased with lower tube potential (12.0 at 80 kV) owing to disproportionately increased image noise. With third-generation DSCT, 70- and 80-kV acquisitions showed a smaller increase in noise. CNRs for third-generation DSCT were highest for 70 and 80 kV (21.1 and 21.2, respectively). Compared to 120 kV, radiation dose was 68 % and 49 % lower at 70 kV and 80 kV, respectively.
Conclusion
Third-generation DSCT enables one to perform coronary CTA at 70–80 kV in obese patients without compromising CNR and thus reduces radiation dose by 49–68 %.
Key points
• Low tube potential CT angiography is currently not suitable for obese patients.
• Third-generation DSCT offers substantially increased tube power at low tube potential.
• This enables one to perform coronary CT angiography at 70–80 kV in obese patients.
• Signal-to-noise ratio is maintained owing to increased tube current.
• This approach can be expected to reduce radiation dose by 49–68 %.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Decreasing the tube potential is a powerful strategy to reduce the radiation dose of CT angiography (CTA) [1]. The higher attenuation of iodine at low photon energies increases intravascular contrast. This increased contrast allows for higher image noise at lower tube potential thus reducing radiation dose while maintaining diagnostic image quality.
The eligibility of patients for low tube potential CTA, however, is predicated upon their body habitus and the technological performance of current CT systems. Current X-ray tubes are limited by the maximum tube current they can generate, particularly at low tube potentials. Typically, at 80 kV tube potential, not more than 600–800 mA is available in state-of-the-art CT systems. In obese patients, this maximum tube current is regularly insufficient to provide adequate photon flux at low tube potential, and excessive image noise results. The increased iodine contrast is insufficient to compensate for excessive image noise in these patients. Therefore, low tube potential CTA techniques are currently not suitable for obese patients.
Recently, a third-generation dual-source CT (DSCT) system was developed [2]. As one of the key features, this system has two X-ray tubes with substantially increased power (120 kW each) [2], enabling tube currents up to 1,300 mA each at 70 kV and 80 kV, respectively. Performing CTA examinations with low tube potential at substantially higher tube currents has thus become feasible. We hypothesized that this ability would extend the scope of low tube potential CTA to obese patients and reduce radiation dose in this setting. Therefore, the aim of this study was to evaluate the influence of tube potential on radiation dose and image quality of third-generation dual-source coronary CTA in a phantom model simulating an obese patient.
Materials and methods
Phantom setup
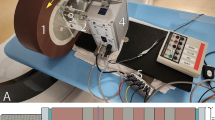
An anthropomorphic thoracic phantom (Cardio CT Phantom, QRM, Forchheim, Germany) was used in this study. This phantom resembles a human chest, with artificial lungs (resin with a CT density of approximately −800 HU at 120 kV) and a spine insert surrounded by soft-tissue-equivalent material and a chamber in the position of the heart. The phantom has a diameter of 30 cm in the lateral axis and 20 cm in the anteroposterior axis and was additionally fitted with an external soft-tissue-equivalent ring (5 cm thickness) to simulate an obese patient. A 50-mL syringe was filled with an iodine solution prepared by diluting iodine contrast medium (Omnipaque 350, GE Healthcare, Princeton, NJ) with water to a predetermined concentration of 15 mg iodine per millilitre. This concentration was chosen to match a typical intravascular concentration of iodine in CTA studies with an attenuation of approximately 350 HU at a tube potential of 120 kV. A second syringe was filled with water. The syringes were positioned in the central cardiac chamber and held in place by a foam insert. The phantom is depicted in Fig. 1a; Figs. 1b and c show the resulting transverse CT images.
Phantom setup and image analysis. a The anthropomorphic thoracic phantom with an external soft-tissue ring mimicking an obese body habitus is shown. Two syringes containing an iodine solution and water, respectively, are placed in the central chamber. Transverse CT images in full (b) and limited (c) field of view reconstructions are shown. The image in d illustrates placement of circular regions of interest in the water (1) and iodine (2) filled syringes
CT acquisition parameters
Experiments were carried out using second- and third-generation DSCT systems (SOMATOM Definition Flash and Force, Siemens Healthcare, Forchheim, Germany). Images were acquired in prospectively electrocardiogram (ECG)-triggered sequential acquisition mode using a simulated ECG with a heart rate of 60 beats per minute and sinus rhythm. All DSCT acquisitions were obtained with 0.28-s gantry rotation time. The third-generation system also offers a shorter gantry rotation time (0.25 s) but we chose to use 0.28 s for both systems to enhance comparability. Detector collimation was 2 × 60 × 0.6 mm for the second-generation DSCT system and 2 × 48 × 0.6 mm (adaptive sequence collimation) for the third-generation DSCT system. All available options for tube potential settings (kilovoltage, kV) were used. Thus, images were acquired at 80, 100, 120 and 140 kV on the second-generation DSCT system and at 70–150 kV (in 10-kV increments) on the third-generation DSCT system. On both CT systems, automated tube current modulation (CAREDose 4D, Siemens) was enabled. Automated tube potential selection (CAREkV, Siemens) was set in “Semi” mode in the “CT angiography” setting. In this setting, tube potential is selected by the operator, yet allowing the system to adjust the tube current as far as technically possible at the corresponding tube potential to maintain constant iodine contrast-to-noise ratio (CNR) [3]. In practice, CNR may decrease at lower tube potential in the “Semi” mode, because the appropriate tube current may not be available, resulting in insufficient radiation dose and disproportionally increased image noise. Target image quality was defined by choosing settings of 120 kV for quality reference tube potential and 300 mAs for quality reference tube current–time product.
Image reconstruction and analysis
All image data sets were reconstructed with 0.75-mm section thickness and 0.5-mm increment, using the iterative reconstruction algorithm of each CT system: sinogram affirmed iterative reconstruction (SAFIRE) strength 3 for the second-generation DSCT system and advanced modelled iterative reconstruction (ADMIRE) strength 3 for the third-generation DSCT system. A smooth vascular reconstruction kernel as commonly used in cardiac CT was chosen (I26f or Bv36, respectively). The reconstructed image data sets were evaluated on a dedicated analysis platform (syngo.via, Siemens). Data sets were presented in random order to an observer blinded to the acquisition parameters. Circular regions of interest (ROI) with a standardized size of 200 mm2 were placed centrally in each of the two phantom inserts to measure CT attenuation of iodine solution and water (Fig. 1d). The standard deviation of the CT attenuation in the iodine solution was used as a metric of image noise. A single acquisition was performed for each kV setting, but all measurements of CT attenuation and image noise were performed on three different sections and the results were averaged. CNR was calculated as
The same observer was subsequently unblinded to the image acquisition parameters and evaluated the visual image impression (noise, iodine attenuation and image quality) at the various tube potential settings in a descriptive manner.
Statistical analysis
For numerical values derived from multiple measurements, mean values and standard deviations were calculated. Objective image quality parameters and volume CT dose index were plotted against the tube potential. The potential for dose reduction for low tube potential acquisitions in third-generation DSCT was calculated using the 120-kV acquisition on the same CT system as the reference standard.
Results
Visual image impression
Representative sections for each CT acquisition are shown in Fig. 2 at standardized window settings (centre 300 HU, width 1,000 HU). A marked increase in iodine contrast at low tube potential is noted with both CT systems. The image quality of the 80-kV image acquired with the second-generation DSCT system is limited by excessive image noise because of insufficient tube current; as a result of the increased tube power this is not the case for the low tube voltage images acquired with the third-generation DSCT system.
Influence of tube potential on visual image impression. For both scanner generations, images acquired with all possible tube potential settings are shown. Images are displayed at standardized window settings (centre 300 HU, width 1,000 HU) to demonstrate the increase in iodine contrast at low tube potential. Excessive image noise is apparent in the 80-kV image acquired with the second-generation DSCT system, but not in the low tube voltage images acquired with third-generation DSCT
Objective image quality
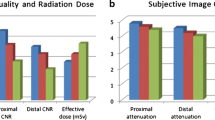
With second-generation DSCT, iodine attenuation decreased from 667 ± 4 HU at 80 kV to 315 ± 3 HU at 140 kV (Fig. 3a) and image noise decreased from 56 ± 4 HU at 80 kV to 18 ± 1 HU at 140 kV (Fig. 3b). CNR was highest (19.0) with 120 kV and markedly decreased with low tube voltage acquisitions with a CNR of 16.5 at 100 kV and 12.0 at 80 kV (Fig. 3c). With third-generation DSCT, iodine attenuation decreased from 782 ± 9 HU at 70 kV to 309 ± 4 HU at 150 kV (Fig. 3a) and image noise decreased from 37 ± 4 HU at 70 kV to 17 ± 2 HU at 150 kV (Fig. 3b). CNR was highest with 80 kV (21.2) followed by 70 kV (21.1) and remained within narrow limits (18.3–21.2) across all tube potentials (Fig. 3c).
Influence of tube potential on objective image quality and radiation dose. This figure illustrates the influence of tube potential on iodine attenuation (a), image noise (b), contrast-to-noise-ratio (CNR, c). With second-generation DSCT, CNR markedly decreases at low tube potential (80–100 kV) because of excessive image noise; this effect is not seen with third-generation DSCT
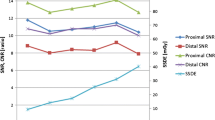
Radiation dose and potential for dose reduction
With second-generation DSCT, there was only a moderate increase in tube current–time product with decreasing tube potential from 280 mAs at 140 kV to 328 mAs at 80 kV (Fig. 4a). With third-generation DSCT, tube current–time product markedly increased from 334 mAs at 150 kV to 673 mAs at 80 kV and 672 mAs at 70 kV. Radiation dose measured as volume CT dose index (CTDIvol) increased from 3.8 mGy at 80 kV to 17.6 mGy at 140 kV with second-generation DSCT (Fig. 4b). With third-generation DSCT, CTDIvol ranged from 3.9 mGy at 70 kV to 20.1 mGy at 150 kV. Owing to the higher tube current–time product available with third-generation DSCT at low tube potentials, CTDIvol at 80 kV was substantially higher with the third-generation system compared to the second-generation system (6.4 vs. 3.8 mGy); to a lesser extent the same effect was observed at 100 kV (9.1 vs. 8.1 mGy). Values for CTDIvol were similar between both CT systems at 120 kV (12.4 vs. 12.0 mGy) and at 140 kV (17.5 vs. 17.6 mGy). With the third-generation CT system, reducing the tube potential to 70, 80, 90 or 100 kV reduced CTDIvol by 68, 49, 38 and 27 %, respectively, compared with the 120-kV acquisition on the same CT system at maintained CNR (Fig. 5).
Influence of tube potential on objective image quality and radiation dose. This figure illustrates the influence of tube potential on tube current–time product (a) and volume CT dose index as a metric of the applied radiation dose (b). With third-generation DSCT, tube current–time product can be markedly increased to preserve image quality at low tube potential
Discussion
Lowering the tube potential is a well-recognized strategy to reduce the radiation dose of CTA. However, this approach has thus far not been feasible in obese patients because of the excessive image noise at low tube potential due to insufficient maximum tube current with existing CT systems. The hypothesis of this phantom study was that this limitation could be overcome with third-generation DSCT, which is equipped with two X-ray tubes with substantially increased tube power at low tube potential and may thus prevent the excessive increase in image noise by adequately increasing tube current at low tube potential.
A previous study has suggested that 100-kV coronary CTA may yield reasonable diagnostic accuracy in overweight patients [4]. However, in a less selected obese population, 100-kV acquisitions are likely to result in a large number of non-diagnostic examinations with standard equipment. Even at 120 kV, image quality of coronary CTA studies can still be limited in patients with a large body habitus, which has prompted some practitioners to increase tube potential to 140 kV for morbidly obese patients. However, a recent study comparing coronary CTA at 140 kV compared to 120 kV for overweight and obese individuals found similar image quality but higher radiation dose at 140 kV [5]. Hence, 120 kV is currently considered the standard tube potential for coronary CTA in obese patients.
We therefore chose the 120-kV acquisition as the reference to calculate the potential dose reduction that can be expected by reducing tube potential in obese patients with third-generation DSCT. We found a potential dose reduction of 68 % with 70 kV at maintained CNR. To date, no studies of coronary CTA using 70 kV have been published and thus no clinical experiences are available for comparison. Several clinical studies on the effect of reduced tube potential (80–100 kV) on the resulting radiation dose of coronary CTA in normal-weight individuals have been published. The multicenter PROTECTION I and II trials demonstrated a 31–53 % dose reduction with 100 kV compared to 120 kV [1, 6]. A subsequent multicentre trial conducted by LaBounty and colleagues demonstrated that a further radiation dose reduction of 47 % can be achieved by reducing the tube potential from 100 to 80 kV [7]. Similar results have been described in smaller, single-centre studies [8–11].
The dose reductions of 49 % at 80 kV and 27 % at 100 kV (relative to 120 kV) in our study are thus comparable to, although somewhat lower, than what has been observed in clinical studies involving normal-weight patients. This difference can easily be explained by technical considerations: In our study, preserved image quality at low tube potential despite the large phantom size was possible only because the third-generation DSCT system is able to substantially increase tube current at low tube potential, as demonstrated in our study by the stability of CNR across all tube potentials. In contrast, the substantial drop in CNR at low tube potential observed in the second-generation DSCT acquisitions reflects the inability of hitherto existing systems to sufficiently increase the tube output at lower kV in obese patients. With third-generation DSCT, the increase in tube current at low tube potential is more pronounced for the large body phantom than would be necessary for normal-sized patients and thus explains why the potential for dose reduction is slightly lower for obese patients compared to normal-weight individuals. Nevertheless, the potential for dose reduction identified in our study is substantial with a predicted dose saving of 49–68 % by performing coronary CTA in obese patients at 70 or 80 kV.
For this study, we assessed objective image quality on image series reconstructed with iterative reconstruction. Iterative reconstruction is well known to reduce image noise and thus increase CNR [12–15]. The decision to use iterative reconstruction in our study was driven by the consideration that iterative reconstruction is widely replacing filtered back projection in clinical practice and is increasingly regarded as the standard of care [16–18]. Since we applied iterative reconstruction to all images both for the second- and third-generation DSCT data sets, the relative changes in noise and CNR would likely be very similar if other reconstruction techniques had been used.
In order to systematically assess the influence of tube potential on radiation dose and image quality, we used the “Semi” mode of the automated tube potential selection algorithm for this study, such that the tube potential was selected by the operator, yet allowing the system to adjust the tube current to maintain constant CNR. In clinical routine, this algorithm would likely be used in the automatic mode, in which the system uses the attenuation profile of the topogram images to automatically choose the most dose-efficient combination of tube potential and tube current. Thus, low tube potential CTA in obese patients could easily be implemented in clinical routine without the operator having to make the decision as to whether an individual obese patient is suitable for a specific low tube potential.
The results of our study need to be seen in the context of the study design and its limitations. The low tube voltage acquisition in a large body size phantom is only feasible because of the high tube power of the investigated third-generation DSCT system. The results cannot be generalized to other CT systems of the same or other manufacturers. We further used a static phantom, which does not take into account the influence of breathing and cardiac motion. However, changes in tube potential are independent of acquisition speed and temporal resolution; it is therefore unlikely that the effect of motion and motion artefacts would have influenced our results. In addition, the experiments were performed in a single phantom size mimicking a moderately obese patient. The image quality of coronary CTA at low tube potential may not be sufficient for extremely obese patients. More importantly, while image noise and CNR are powerful metrics to objectively compare image quality, other factors can influence the interpretability of coronary CTA studies in the clinical setting. This can be seen in patients with heavily calcified vessels or coronary stents, where blooming and beam hardening artefacts are much more pronounced at low tube voltages and can thus limit the interpretability (and thus potentially the diagnostic accuracy) of coronary CTA despite a nominally equal CNR. In such patients, high tube potential acquisitions may still be necessary to allow accurate assessment of the coronary arteries. In light of these limitations, our findings should be regarded as preliminary evidence derived from the controlled setting of a phantom study, which needs confirmation in a clinical environment.
In conclusion, our phantom experiments indicate that the high tube power of third-generation DSCT can prevent the disproportionate increase in image noise, which has so far precluded the use of low tube potential CTA in obese patients. Our phantom data suggests that third-generation DSCT will also enable one to perform coronary CTA at 70–80 kV in obese patients without compromising image quality. Compared to 120 kV, which is currently the clinical standard in obese patients, this approach can be expected to reduce radiation dose by 49–68 % at maintained CNR.
References
Hausleiter J, Martinoff S, Hadamitzky M et al (2010) Image quality and radiation exposure with a low tube voltage protocol for coronary CT angiography results of the PROTECTION II Trial. JACC Cardiovasc Imaging 3:1113–1123
Siemens (2014) SOMATOM Force. http://www.healthcare.siemens.com/computed-tomography/dual-source-ct/somatom-force. Accessed 2 Jan 2014
Winklehner A, Goetti R, Baumueller S et al (2011) Automated attenuation-based tube potential selection for thoracoabdominal computed tomography angiography: improved dose effectiveness. Invest Radiol 46:767–773
Ho JS, Barlow CE, Reinhardt DB, Wade WA, Cannaday JJ (2010) Effect of increasing body mass index on image quality and positive predictive value of 100-kV coronary computed tomographic angiography. Am J Cardiol 106:1182–1186
Lee AM, Engel LC, Hui GC et al (2013) Coronary computed tomography angiography at 140 kV versus 120 kV: assessment of image quality and radiation exposure in overweight and moderately obese patients. Acta Radiol. doi:10.1177/0284185113502745
Bischoff B, Hein F, Meyer T et al (2009) Impact of a reduced tube voltage on CT angiography and radiation dose: results of the PROTECTION I study. JACC Cardiovasc Imaging 2:940–946
LaBounty TM, Leipsic J, Poulter R et al (2011) Coronary CT angiography of patients with a normal body mass index using 80 kVp versus 100 kVp: a prospective, multicenter, multivendor randomized trial. AJR Am J Roentgenol 197:W860–W867
Ripsweden J, Brismar TB, Holm J et al (2010) Impact on image quality and radiation exposure in coronary CT angiography: 100 kVp versus 120 kVp. Acta Radiol 51:903–909
Cao JX, Wang YM, Lu JG, Zhang Y, Wang P, Yang C (2013) Radiation and contrast agent doses reductions by using 80-kV tube voltage in coronary computed tomographic angiography: a comparative study. Eur J Radiol. doi:10.1016/j.ejrad.2013.06.032
Jun BR, Yong HS, Kang EY, Woo OH, Choi EJ (2012) 64-slice coronary computed tomography angiography using low tube voltage of 80 kV in subjects with normal body mass indices: comparative study using 120 kV. Acta Radiol 53:1099–1106
Leschka S, Stolzmann P, Schmid FT et al (2008) Low kilovoltage cardiac dual-source CT: attenuation, noise, and radiation dose. Eur Radiol 18:1809–1817
Hou Y, Liu X, Xv S, Guo W, Guo Q (2012) Comparisons of image quality and radiation dose between iterative reconstruction and filtered back projection reconstruction algorithms in 256-MDCT coronary angiography. AJR Am J Roentgenol 199:588–594
Renker M, Nance JW Jr, Schoepf UJ et al (2011) Evaluation of heavily calcified vessels with coronary CT angiography: comparison of iterative and filtered back projection image reconstruction. Radiology 260:390–399
Yin WH, Lu B, Li N et al (2013) Iterative reconstruction to preserve image quality and diagnostic accuracy at reduced radiation dose in coronary CT angiography: an intraindividual comparison. JACC Cardiovasc Imaging 6:1239–1249
Wang R, Schoepf UJ, Wu R et al (2012) Image quality and radiation dose of low dose coronary CT angiography in obese patients: sinogram affirmed iterative reconstruction versus filtered back projection. Eur J Radiol 81:3141–3145
Renker M, Geyer LL, Krazinski AW, Silverman JR, Ebersberger U, Schoepf UJ (2013) Iterative image reconstruction: a realistic dose-saving method in cardiac CT imaging? Expert Rev Cardiovasc Ther 11:403–409
McCollough CH, Chen GH, Kalender W et al (2012) Achieving routine submillisievert CT scanning: report from the summit on management of radiation dose in CT. Radiology 264:567–580
Leipsic J, Heilbron BG, Hague C (2012) Iterative reconstruction for coronary CT angiography: finding its way. Int J Cardiovasc Imaging 28:613–620
Acknowledgements
The scientific guarantor of this publication is U. Joseph Schoepf, MD. The authors of this manuscript declare relationships with the following companies: Dr. Schoepf is a consultant for and receives research support from Bayer, Bracco, GE and Siemens. Mr. Canstein, Dr. Sedlmaier, Dr. Schmidt and Dr. Flohr are Siemens employees. The other authors have no conflict of interest to disclose. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional review board approval was not required because this is a phantom study and does not involve human subjects. None of the study subjects or cohorts have been previously reported. Methodology: experimental phantom study, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Meinel, F.G., Canstein, C., Schoepf, U.J. et al. Image quality and radiation dose of low tube voltage 3rd generation dual-source coronary CT angiography in obese patients: a phantom study. Eur Radiol 24, 1643–1650 (2014). https://doi.org/10.1007/s00330-014-3194-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3194-x