Abstract
Objectives
To describe the pathological appearance of the anterolateral ligament (ALL) on US and MRI in knees with an anterior cruciate ligament (ACL) tear.
Methods
This prospective study included 30 patients who had a suspected acute ACL tear. Their injured and contralateral knees were evaluated with radiography, US and MRI. Two radiologists evaluated the ALL on the MRI and US examinations. Agreement between these examiners’ findings was evaluated with Cohen’s kappa.
Results
On US examination, the ALL was found to be injured in 63% of cases (19/30; k = 0.93). The enthesis was found to be torn in 50% of cases (15/30; k = 1), with the tear located at the tibial attachment in all instances. On the MRI exam, the ALL was found to be injured in 53% of cases (16/30; k = 0.93). The enthesis was found to be torn in 13% of cases (4/30; k = 0.76), with the tear located at the tibial attachment in all instances (k = 0.93).
Conclusion
ALL injuries that occur with ACL tears are located at the tibial enthesis. They are often associated with bone avulsion at the enthesis and are better viewed on US.
Key Points
• ALL injuries often occur in combination with ACL tears.
• ALL injuries can be assessed with ultrasonography and MRI.
• ALL injuries associated with ACL tears are located at the tibial enthesis.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The knee's anterolateral ligament (ALL) has been the subject of an unusual level of media attention: Claes put the spotlight on this small ligament with his cadaver findings in 2013 [1]. However, this ligament had been described more than a century ago by Dr Paul Segond, who established a link between bone avulsion of the anterolateral part of the proximal tibia and internal rotation laxity; this injury was latter named the ‘Segond fracture’. He also showed that when the knee is internally rotating, tension is placed on a ‘pearly, resistant, fibrous band’, although this observation has mostly been forgotten [2]. Several anatomical studies reported that the ALL is present in 83–100% of individuals; it originates on the lateral femoral condyle, takes an oblique trajectory downward and forward, then inserts on the lateral edge of the tibial plateau [3,4,5,6].
Many studies have looked into the the function of the ALL [7,8,9,10,11]. The ALL is involved in controlling internal rotation and, more generally, in controlling the knee's rotational stability [3]. In 1979, Wood's team showed that a Segond fracture was pathognomonic of an anterior cruciate ligament (ACL) tear [12]. Recently, Sonnery-Cottet showed a strong correlation between ALL injury and the persistence of rotational instability after ACL reconstruction [11]. These observations have opened new treatment avenues that combine ACL reconstruction with ALL reconstruction [13]. However, the indications for extra-articular lateral tenodesis of the ALL still need to be defined; it is in these new avenues that imaging plays a key role. There is currently no gold standard for analysing the ALL in vivo; although there is a strong relationship with a high-grade pivot shift test, it is not specific, and the ALL is difficult to see using arthroscopy [11, 14, 15].
In a non-injured knee, MRI can detect the ALL in 97–100% of cases [4, 16, 17]. Cavaignac et al. showed that the ALL was visible on ultrasonography (US) in 100% of cadaver specimens [18]. After an ACL tear, the ALL was found to be injured in 26% of cases in one study and 62% in another [19, 20]. US, which has superior spatial resolution to MRI and allows real-time dynamic imaging, has never been used to analyse the ALL after an ACL tear [21].
Defining the pathological appearance of the ALL is a new challenge for imaging. The objective of this study was to describe the pathological appearance of the ALL on US and MRI in knees with an ACL tear.
Materials and methods
Patient selection
This study was approved by our hospital's research ethics committee and patients provided their written consent before participating. We prospectively and randomly enrolled 38 patients who were scheduled for ACL reconstruction at our facility because of a positive MRI diagnosis of ACL tear between November 2015 and February 2016. The inclusion criteria were patients 18 years of age or older with a recent (less than 3 months old) ACL tear that was confirmed on MRI. Exclusion criterion was a history of injury or surgery on either knee.
Eight of the enrolled patients did not meet the inclusion criteria: four did not undergo the full MRI examination (due to pain or claustrophobia) and four had a prior knee injury (healthy knee in three patients and injured knee in one patient). This resulted in 30 patients (22 men, eight women) with an average age of 29.3 ± 11.6 years being analysed in this study.
Study protocol
Each included patient underwent:
-
standard X-rays of the injured knee
-
MRI of the injured knee
-
US of both knees on the day before the ACL reconstruction procedure.
Radiography
The radiographs were performed with the patient supine using orthogonal anteroposterior X-rays (55 kV, 10 mAs) with a biplanar table (Carestream DRX Evolution, New York, NY, USA).
Magnetic resonance imaging (MRI)
A 1.5-T unit (Optima®, General Electric Medical Systems, Milwaukee, WI, USA) was used with a knee-specific coil; the knee was placed in 10° flexion for the examination. The following protocol was used: axial, coronal and sagittal proton-density-weighted images with fat saturation (PD Fat SAT) (TR 3907 ms; TE 42 ms with 3.5 mm slice thickness, 224 × 320 mm matrix, 160 mm field of view (FOV)) and sagittal T1-weighted (TR 620 ms, TE 13 ms, 3.5 mm slice thickness, no interslice gap, 224 × 380 mm matrix, 160 mm FOV) sequences. The patients underwent the MRI examination an average of 25 ± 18.65 days after the injury event.
Ultrasonography (US)
Exploration of the ALL was performed using a high-frequency probe (Aplio 500 Toshiba, 14–18 MHz probe) with the patient supine, the knee partially flexed (70°) and the foot internally rotated – a position that places tension on the ALL [18]. The ALL was analysed on a coronal slice in its major axis. The US technique consisted of locating the iliotibial band at its insertion on Gerdy's tubercle, and then translating the probe posteriorly to locate the tibial insertion of the ALL. The upper end of the probe was rotated about 20° to make it easier to view the ALL in its major axis. Patients underwent the US examination an average of 50.65 ± 29.15 days after the MRI had been performed.
Image analysis
The radiographs and MRI images were analysed in a blinded manner by two radiologists with 13 years (MFB) and 7 years (OC) of experience, respectively, using a validated analysis protocol on a workstation using our facility’s PACS (McKesson®, New York, NY, USA). The US was performed in succession by the same two radiologists; they had no knowledge of each other's results. The ALL’s thickness was measured on US twice for each patient on the same day by each of the two radiologists (MF and OL), who were blinded to the other radiologist’s findings
Radiography analysis
The radiographs were analysed to look for bone avulsion at the anterolateral part of the tibial plateau (Segond fracture) [2].
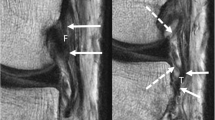
MRI analysis
In the first step of the analysis, the ACL tear was confirmed based on loss of the fibrillar appearance of the ACL's two bundles, which had increased signal on the PD Fat Sat sequences with fibre continuity [22]. The second step consisted of analysing the ALL and its femoral, meniscal and tibial insertions [4,5,6].
The ALL was considered normal if a low-intensity linear structure was visible between the femoral epicondyle and tibial plateau [16, 17, 19, 23, 24]. The ALL was considered injured if it was torn or had high signal intensity with irregular contours [19]. Avulsion of the ALL at its tibial insertion was considered a Segond fracture [5, 23, 24]. The presence of bone oedema at the tibial enthesis was labelled grade 1 if it was less than 5 mm in diameter at its widest point, and grade 2 if it was more than 5 mm in diameter [25]. Figure 1 shows examples of normal and injured ALLs on MRI.
Appearance of anterolateral ligament (ALL) on MRI. Anterolateral ligament of the knee in the coronal plane in fat-saturated proton density-weighted sequences. (A) Normal ALL. (B) Injured ALL: hyperintensity at tibial insertion and increased thickness. (C) Segond fracture: bone avulsion at tibial enthesis combined with hyperintensity at thickened tibial insertion
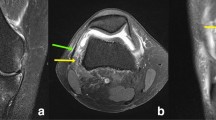
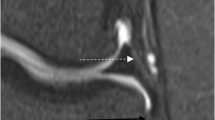
US analysis
The ligament mid-substance and the femoral, meniscal and tibial insertions of the ALL were analysed. The ALL was considered normal if a fibrillar anisotropic structure was visible [18]. The ALL was considered injured if it was torn, stretched or hypoechogenic with irregular contours and fluid accumulated around the ligament. The thickness of the ALL was measured in the injured and contralateral knees at the level of the tibial plateau. Avulsion of the ALL at its tibial insertion was considered a Segond fracture and labelled an ‘ultrasonographic Segond’ [5, 24, 26]. Figure 2 shows examples of normal and injured ALLs on US. Figure 3 shows an example of different findings on ultrasound and MRI.
Appearance of anterolateral ligament (ALL) on ultrasonography. Major axis of the anterolateral ligament of the knee; coronal plane image showing the ligament in the major axis. (A) Ultrasonography of normal ALL (arrows): hypoechogenic, fibrillar, thin structure crossing superficially the inferior genicular artery (arrow head) and popliteal tendon (star). (B) Ultrasonography of injured ALL: the tibial insertion is hypoechogenic and thickened (arrow) with fluid accumulation in the soft tissues around the ligament. (C) Ultrasonography of injured ALL: the tibial insertion is hypoechogenic and thickened (arrow) and there is a bone avulsion at the tibial enthesis (arrowhead), i.e. Segond fracture. FC femoral condyle, LM lateral meniscus, TP tibial plateau
Example of different findings on ultrasound and MRI. MRI coronal PD Fat Sat sequence (A) shows thickening at the anterolateral ligament (ALL)’s tibial insertion (thick arrow) without damage to the bone cortex at its enthesis, which is the site of grade 1 oedema. Ultrasound in the coronal plane (B) shows thickening at the ALL’s tibial insertion (thin arrow) and a discontinuity in the cortex (thick arrow) at its enthesis. FC femoral condyle, LM lateral meniscus, TP tibial plateau
Statistical analysis
The measurements done by the most experienced radiologist (MFB) were used for the descriptive analysis. Those of the second radiologist (OC) were used to assess measurement reproducibility. The descriptive analysis consisted of calculating the average and standard deviation values. Using Lancaster's method, we calculated that 30 subjects were needed for this pilot study [27]. To evaluate the reproducibility of the results, the agreement between observers was determined using Cohen's kappa (k) coefficient. The results were interpreted based on the rules defined by Landis and Koch [28]. A paired Student's t-test was used to compare the measured ALL thickness between knees. Using the receiver operating characteristic (ROC) method, we defined a threshold for the ALL thickness that allowed us to label it as injured. The correlation between the ALL’s condition on US and MRI, the correlation between the presence of bone avulsion at the enthesis on US and MRI, and the correlation between the ALL's condition on MRI and the degree of bone oedema was analysed using Pearson's Chi-squared test.
The statistical tests were carried out with Excel 2011 and MedCalc software®. A threshold of p < 0.05 was used to determine statistical significance in all tests.
Results
Radiography analysis
On the radiographs, one of the 30 patients (3%) had bone avulsion of the anterolateral portion of the tibial plateau.
MRI analysis
All 30 patients had a tear in both ACL bundles confirmed on MRI. The ALL was visible in 96% of patients (29/30; k = 0.91); the tibial insertion was visible in 96% of patients (29/30; k = 1), the femoral insertion in 40% (12/30; k = 0.86) and the meniscal insertion in 93% (28/30; k = 1) (Table 1).
In the 30 patients analysed, the ALL was damaged in 53% of cases (16/30; k = 0.93). The enthesis was torn in 13% of patients (4/30; k = 0.76), with the tear located at the tibial attachment in all instances (k = 0.93). In the patients with a torn enthesis, the ALL was thickened with fluid accumulation in the soft tissues around the ligament (4/30; k = 0.91). In 40% of patients (12/30; k = 0.89), the ALL was found to be injured on MRI, with no detectable detachment visible at the enthesis.
The presence of bone oedema at the enthesis on MRI is summarized in Table 2. There was a significant correlation between the condition of the ALL on MRI and the oedema grade (Chi-squared test =8, p < 0.05).
US analysis
The ALL was visible in all patients; the tibial insertion was visible in 100% of patients (30/30; k = 1) and the femoral insertion in 96% of cases (29/30; k = 0.63), but the meniscal insertion was not visible in any patient (0%; k = 1) (Table 1).
In the 30 patients analysed, the ALL was injured in 63% of cases (19/30; k = 0.93). The enthesis was torn (sonographic Segond) in 50% of cases (15/30; k = 1), with the tear located at the tibial attachment in every instance. All patients with enthesis involvement (15/30; k = 1) had an ALL that appeared injured. In 13% of cases (4/30; k = 0.91), the ALL was abnormal on the ultrasound examination but the enthesis was intact (Table 3).
The average thickness of the injured ALL was 1.46 ± 0.27 mm (min = 1.2 mm; max = 2.1 mm). The average thickness of the ALL when it was detached at the enthesis was 1.52 ± 0.27 mm (min = 1.3 mm; max = 2.1 mm). The average thickness of the non-injured ALL was 0.97 ± 0.13 mm (min = 0.7 mm; max = 1.1 mm). The average thickness of the ALL in the healthy contralateral knees was 0.91 ± 0.12 mm (min = 0.8 mm; max = 1.1 mm) (Table 3). Based on the ROC method, the ALL thickness threshold corresponding to an injured ligament was > 1.1 mm (sensitivity = 89.5%, specificity = 97.56%, p < 0.05).
Comparison of the US and MRI exams for the ALL
There was a significant correlation between the US and MRI findings for the ALL (Chi-squared test = 16, p < 0.001). The condition of the ALL was found to differ on MRI and US in three patients: the ALL was classified as injured on US and uninjured on MRI.
The detection of bone avulsion at the enthesis differed in 11 patients: in all of these, US found bone avulsion while the MRI did not. Of these 11 patients, eight had grade 1 bone oedema and three had grade 2 bone oedema on the MRI. There was a significant correlation between US and MRI for the description of bone avulsion at the enthesis (Chi-squared test = 4; p <0.05).
Discussion
This study described the pathological appearance of the ALL when associated with an ACL tear on US and MRI, with a strong correlation between the two imaging modalities (Pearson's Chi-squared = 16; p < 0.001).
US was able detect three more cases of ALL injury than did MRI. This can be explained by the fact that US has better spatial resolution and is therefore more sensitive for detecting this small ligament – which normally measures a few millimetres – that had a maximum thickness of 2.1 mm in this study [21]. The other reason has to do with the MRI method: the acquisition was performed in a strict coronal plane, not in the ALL plane, which is angled down and forward. Three-dimensional isotropic sequences could improve the detection of ALL injuries using MRI; these sequences have been used in non-injured knees, with the ALL being detected in 100% of cases [29].
We found an ALL injury rate of 43% on MRI and 53% on US. These results agree with published results on ALL injury rates associated with ACL tears: Van Dyck found a 26% combined ALL and ACL injury rate in 90 MRI cases, while Claes found a 78.8% rate in a series of 206 MRI cases [19, 30].
In our study, all of the ALL injuries were at its tibial insertion. Our results are consistent with the Van Dyck and Claes studies, who found tibial enthesis involvement in 71.8% and 77.8% of cases, respectively.
A Segond fracture was identified in 3% of patients on the radiographs, 13% of patients on MRI and 50% of patients on US. In their studies, Van Dyck and Claes found a Segond fracture in 37% and 1.8% of cases, respectively [19, 30]. The rate of Segond fractures found in the US portion of our study is greater than the one found in the MRI portion because the superior spatial resolution of US makes it possible to detect bone avulsions, even small ones [21]. The MRI protocol used in this study is the same one we use routinely to evaluate injured knees at our facility; it includes a T1-weighted sequence in the sagittal plane. Coronal plane images could have provided a better view the cortex of the ALL enthesis and made it possible to diagnose more Segond fractures with MRI.
Our study also found a statistically significant correlation between the presence of bone oedema at the tibial enthesis and ALL injury, but found no correlation between the degree of bone oedema and the presence of a Segond fracture. In our study, all of the injured ALLs also had bone oedema over Gerdy's tubercle. Of the four Segond fractures identified on MRI, three had grade 2 oedema and one had grade 1 oedema.
It was easier to see the ALL on US than on MRI. As in the Cavaignac and Oshima studies, US could identify the ALL in 100% of cases [18, 31]. As in both of those studies, the ALL's meniscal insertion was not visible, while its tibial insertion was visible in all cases. The femoral insertion was visible in 96% of cases in our study, versus 100% in the Cavaignac study and 77% in the Oshima study. The ALL's meniscal insertion was not visible on US because of the perpendicular orientation of the US probe to the ALL's fibres that insert on the meniscus.
MRI identified the ALL in 96% of patients in our study. The ALL has been analysed by MRI by several other teams; the consensus is that the ALL is difficult to analyse along its entire length. Claes identified the entire ALL in 76% of cases, Helito in 71.7% of cases (89.7% for the femoral portion, 94% for the meniscal portion and 79.4% for the tibial portion) and Taneja identified the entire ALL by MRI in only 11% of cases [16, 17, 30]. The challenges with identifying the ALL on MRI can be attributed to this ligament's orientation and thinness, and also to its proximity to neighbouring ligament structures, which makes it difficult to analyse its proximal bone attachment [4]. Hartigan et al. reported that the ALL was visible on MRI in 100% of cases, but found poor interobserver reproducibility for the analysis of ALL injuries [20].
The superior ability of US to detect the ALL (100%) relative to MRI (96%) can also be explained by the position in which the examination is performed: US is carried out with the knee flexed and internally rotated (which places tension on the ALL), while MRI is performed in 10° flexion and neutral rotation.
Interobserver correlation was excellent when the ALL's thickness was measured on US (k between 0.93 and 1). The thickness was not measured on MRI, as it was too thin to be measured reliably with existing methods. Oshima reported the ALL's thickness on MRI as 1.3 mm, while Claes found it to be 0.83 mm in a cadaver study [1, 31]. With US, we found the average thickness of the ALL in the non-injured contralateral knee to be 0.97 ± 0.13 mm (min = 0.7, max = 1.3 mm) over the tibial plateau, which is consistent with the above-mentioned studies [1]. Our study found a statistically significant correlation between the ALL being thicker than 1.1 mm and it being injured. The ALL's average thickness was greater (1.52 ± 0.27 mm; min = 1.5 mm; max = 2.1 mm) when it was associated with a Segond fracture.
Our study has certain limitations. The US examination was performed on a different day to the MRI exam. Since a larger number of injured ALLs were found on US, the time that elapsed between these two examinations may have allowed the inflammation around the ligament to resolve, thereby making it easier to determine whether the ALL was injured. This was a preliminary study on a small number of patients, as it is a component of a pilot study evaluating the intra-operative function of the ALL using clinical testing such as the pivot shift. This on-going work aims to correlate the ALL's status on US with the indications for extra-articular lateral tenodesis. Finally, a comparison of the diagnostic relevance of the two imaging methods could not be performed as there is currently no gold standard for analysing the ALL.
No validated arthroscopy method currently exists for viewing the ALL during ACL reconstruction procedures; however, two approaches have been published [15, 32]. Sonnery-Cottet et al. published an arthroscopic surgical technique for viewing the ALL. This is an aggressive technique that requires excision of the anterolateral capsule to expose the ALL. This was a technical note that did not disclose the inherent morbidity of this technique. It was a cadaver study that aimed to prove the ALL’s existence. It was not an identification method that can be used during ALL reconstruction. Ferretti et al. performed ACL reconstruction with a graft passed around the lateral condyle. They made an incision over the ALL, which allowed them to determine whether it was injured. Of note, they found the same prevalence of ALL injury as the prevalence found with US. The ACL reconstruction technique differs from the one used by the surgical team at our facility (without a lateral incision). The technique used by Ferretti and colleagues is more invasive; no study has compared these two techniques. Our surgical team and the research ethics board at our facility did not support altering our surgical practices for an observational study.
The role of these two imaging modalities must still be defined. Nevertheless, the accessibility and low cost of US, and especially the possibility of placing the ligament under tension during the examination and of performing dynamic manoeuvres, make US very attractive for analysing the ALL. Since MRI is routinely performed to diagnose ACL tears, use of three-dimensional sequences and acquisition performed in internal rotation could make it more effective for analysing the ALL.
Conclusion
In this study, we found that in patients with an ACL injury, the ALL is also injured in 43% of cases based on MRI and 53% of cases based on US. US made it possible to detect a larger number of tibial enthesis detachments called ‘Segond-like fractures’ than did MRI; all of the ALL injuries occurred at the tibial enthesis. Based on our US findings, an ALL that is thicker than 1.1 mm at the tibial plateau can be considered injured. Because it allows the ALL to be evaluated under tension, US could have an important role as a supplementary assessment for anterolateral instability of the knee.
Abbreviations
- ALL:
-
Anterolateral ligament
- ACL:
-
Anterior cruciate ligament
References
Claes S, Vereecke E, Maes M, Victor J, Verdonk P, Bellemans J (2013) Anatomy of the anterolateral ligament of the knee. J Anat 223:321–328
Segond P (1879) Recherches cliniques et expérimentales sur les épanchements sanguins du genou par entorse [Internet]. National Library of France, 1879: Paris [cité 5 mai 2015]. 1–85 p. Disponible sur: http://www.ncbi.nlm.nih.gov/pubmed
Pomajzl R, Maerz T, Shams C, Guettler J, Bicos J (2015) A review of the anterolateral ligament of the knee: current knowledge regarding its incidence, anatomy, biomechanics, and surgical dissection. Arthroscopy 31:583–591
Caterine S, Litchfield R, Johnson M, Chronik B, Getgood A (2015) A cadaveric study of the anterolateral ligament: re-introducing the lateral capsular ligament. Knee Surg Sports Traumatol Arthrosc 23:3186–3195
Dodds AL, Halewood C, Gupte CM, Williams A, Amis AA (2014) The anterolateral ligament: Anatomy, length changes and association with the Segond fracture. Bone Joint J 96-B:325–331
Vincent J-P, Magnussen RA, Gezmez F, Uguen A, Jacobi M, Weppe F et al (2012) The anterolateral ligament of the human knee: an anatomic and histologic study. Knee Surg Sports Traumatol Arthrosc 20:147–152
Kennedy MI, Claes S, Fuso FAF, Williams BT, Goldsmith MT, Turnbull TL et al (2015) The Anterolateral Ligament: An Anatomic, Radiographic, and Biomechanical Analysis. Am J Sports Med 43:1606–1615
Helito CP, Bonadio MB, Rozas JS, Wey JMP, Pereira CAM, Cardoso TP et al (2016) Biomechanical study of strength and stiffness of the knee anterolateral ligament. BMC Musculoskelet Disord 17:193
Lutz C, Sonnery-Cottet B, Niglis L, Freychet B, Clavert P, Imbert P (2015) Behavior of the anterolateral structures of the knee during internal rotation. Orthop Traumatol Surg Res 101:523–528
Parsons EM, Gee AO, Spiekerman C, Cavanagh PR (2015) The biomechanical function of the anterolateral ligament of the knee. Am J Sports Med 43:669–674
Sonnery-Cottet B, Lutz C, Daggett M, Dalmay F, Freychet B, Niglis L et al (2016) The Involvement of the Anterolateral Ligament in Rotational Control of the Knee. Am J Sports 44:1209–1214
Woods GW, Stanley RF, Tullos HS (1979) Lateral capsular sign: x-ray clue to a significant knee instability. Am J Sports Med 7:27–33
Sonnery-Cottet B, Thaunat M, Freychet B, Pupim BHB, Murphy CG, Claes S (2015) Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique With a Minimum 2-Year Follow-up. Am J Sports Med 43:1598–1605
Dodds AL, Gupte CM, Neyret P, Williams AM, Amis AA (2011) Extra-articular techniques in anterior cruciate ligament reconstruction: a literature review. J Bone Joint Surg Br 93:1440–1448
Sonnery-Cottet B, Archbold P, Rezende FC, Neto AM, Fayard J-M, Thaunat M (2014) Arthroscopic Identification of the Anterolateral Ligament of the Knee. Arthrosc Technol 3:e389–e392
Taneja AK, Miranda FC, Braga CAP, Gill CM, Hartmann LGC, Santos DCB et al (2015) MRI features of the anterolateral ligament of the knee. Skeletal Radiol 44:403–410
Helito CP, Helito PVP, Costa HP, Bordalo-Rodrigues M, Pecora JR, Camanho GL et al (2014) MRI evaluation of the anterolateral ligament of the knee: assessment in routine 1.5-T scans. Skeletal Radiol 43:1421–1427
Cavaignac E, Wytrykowski K, Reina N, Murgier J, Laumond G, Faruch M et al (2016) Ultrasonographic Identification of the Anterolateral Ligament of the Knee. Arthroscopy 32:120–126
Van Dyck P, Clockaerts S, Vanhoenacker FM, Lambrecht V, Wouters K, De Smet E et al (2016) Anterolateral ligament abnormalities in patients with acute anterior cruciate ligament rupture are associated with lateral meniscal and osseous injuries. Eur Radiol 26:3383–3391
Hartigan DE, Carroll KW, Kosarek FJ, Piasecki DP, Fleischli JF, D’Alessandro DF (2016) Visibility of Anterolateral Ligament Tears in Anterior Cruciate Ligament-Deficient Knees With Standard 1.5-Tesla Magnetic Resonance Imaging. Arthroscopy 32:2061–2065
Nazarian LN (2008) The top 10 reasons musculoskeletal sonography is an important complementary or alternative technique to MRI. AJR Am J Roentgenol 190:1621–1626
Robertson PL, Schweitzer ME, Bartolozzi AR, Ugoni A (1994) Anterior cruciate ligament tears: evaluation of multiple signs with MR imaging. Radiology 193:829–834
Kosy JD, Mandalia VI, Anaspure R (2015) Characterization of the anatomy of the anterolateral ligament of the knee using magnetic resonance imaging. Skeletal Radiol 44:1647–1653
De Maeseneer M, Boulet C, Willekens I, Lenchik L, De Mey J, Cattrysse E et al (2015) Segond fracture: involvement of the iliotibial band, anterolateral ligament, and anterior arm of the biceps femoris in knee trauma. Skeletal Radiol 44:413–421
Brittberg M, Winalski CS (2003) Evaluation of cartilage injuries and repair. J Bone Joint Surg Am 85-A:58–69
Porrino J, Maloney E, Richardson M, Mulcahy H, Ha A, Chew FS (2015) The anterolateral ligament of the knee: MRI appearance, association with the Segond fracture, and historical perspective. AJR Am J Roentgenol 204:367–373
Lancaster GA, Dodd S, Williamson PR (2004) Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract 10:307–312
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Yokosawa K, Sasaki K, Muramatsu K, Ono T, Izawa H, Hachiya Y (2016) Visualization of Anterolateral Ligament of the Knee Using 3D Reconstructed Variable Refocus Flip Angle-Turbo Spin Echo T2 Weighted Image. Nihon Hoshasen Gijutsu Gakkai Zasshi 72:416–423
Claes S, Bartholomeeusen S, Bellemans J (2014) High prevalence of anterolateral ligament abnormalities in magnetic resonance images of anterior cruciate ligament-injured knees. Acta Orthop Belg 80:45–49
Oshima T, Nakase J, Numata H, Takata Y, Tsuchiya H (2016) Ultrasonography imaging of the anterolateral ligament using real-time virtual sonography. Knee 23:198–202
Ferretti A, Monaco E, Fabbri M, Maestri B, De Carli A (2017) Prevalence and Classification of Injuries of Anterolateral Complex in Acute Anterior Cruciate Ligament Tears. Arthroscopy 33:147–154
Acknowledgements
The authors wish to thank Joanne Archambault, PhD for the editorial assistance provided during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Guarantor
The scientific guarantor of this publication is Marie Faruch Bilfeld.
Conflict of interest
The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article.
Funding
The authors state that this work has not received any funding.
Statistics and biometry
One of the authors has significant statistical expertise.
Informed consent
Written informed consent was obtained from all subjects (patients) in this study.
Ethical approval
Institutional review board approval was obtained.
Methodology
• prospective
• cross-sectional, diagnostic study
• performed at one institution
Rights and permissions
About this article
Cite this article
Faruch Bilfeld, M., Cavaignac, E., Wytrykowski, K. et al. Anterolateral ligament injuries in knees with an anterior cruciate ligament tear: Contribution of ultrasonography and MRI. Eur Radiol 28, 58–65 (2018). https://doi.org/10.1007/s00330-017-4955-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-017-4955-0