Abstract
Objectives
Accurate collimation helps to reduce unnecessary irradiation and improves radiographic image quality, which is especially important in the radiosensitive paediatric population. For AP/PA chest radiographs in children, a minimal field size (MinFS) from "just above the lung apices" to "T12/L1" with age-dependent tolerance is suggested by the 1996 European Commission (EC) guidelines, which were examined qualitatively and quantitatively at a paediatric radiology division.
Methods
Five hundred ninety-eight unprocessed chest X-rays (45 % boys, 55 % girls; mean age 3.9 years, range 0–18 years) were analysed with a self-developed tool. Qualitative standards were assessed based on the EC guidelines, as well as the overexposed field size and needlessly irradiated tissue compared to the MinFS.
Results
While qualitative guideline recommendations were satisfied, mean overexposure of +45.1 ± 18.9 % (range +10.2 % to +107.9 %) and tissue overexposure of +33.3 ± 13.3 % were found. Only 4 % (26/598) of the examined X-rays completely fulfilled the EC guidelines.
Conclusions
This study presents a new chest radiography quality control tool which allows assessment of field sizes, distances, overexposures and quality parameters based on the EC guidelines. Utilising this tool, we detected inadequate field sizes, inspiration depths, and patient positioning. Furthermore, some debatable EC guideline aspects were revealed.
Key Points
• European Guidelines on X-ray quality recommend exposed field sizes for common examinations.
• The major failing in paediatric radiographic imaging techniques is inappropriate field size.
• Optimal handling of radiographic units can reduce radiation exposure to paediatric patients.
• Constant quality control helps ensure optimal chest radiographic image acquisition in children.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Chest X-rays are among the most frequently performed radiological examination in adults and children [1, 2], and several radiation safety programs and recommendations on this topic are available [3–10]. Information regarding correct acquisition techniques for chest X-rays are provided by specialist books, the ACR Practice Guidelines [11], and the WHO manual of diagnostic imaging [12]. In 1996, the European Commission (EC) published the “European Guidelines on Quality Criteria for Diagnostic Radiographic Images in Paediatrics” [5] which, as compared to the others, provide the most detailed and in-depth information. Studies by Brennan et al., Grewal et al., and Muhogora et al. have addressed the adult counterpart of the EC radiography guidelines [13], reporting varying or moderate adherence and awareness [14–16]. To the authors’ knowledge, there are no such reports in the paediatric population.
There is consistent agreement throughout the literature that an optimal field size through correct collimation is an important factor in paediatric radiographic dose reduction [17–19]. Optimal collimation reduces (scatter) radiation and improves image quality, especially contrast and resolution [20]. Although radiation doses for individual chest radiographs are considered low [15, 21], both the collective dose applied due to the volume of examinations performed [22–24] and the individual patient dose from repeated chest X-rays can be notable.
The purpose of this study was to survey the actual AP/PA chest X-ray performance at the authors’ paediatric radiology division, specifically with regard to whether the EC guidelines could be satisfied qualitatively and quantitatively, particularly in terms of unnecessarily irradiated field size and tissue overexposure. An intra- and inter-observer validated semiautomatic quality control tool was developed in order to achieve this task in a time-efficient manner.
Materials and methods
Five hundred ninety-eight raw (unprocessed) digital radiographic (DR) chest images of 390 unique patients acquired at the authors’ institution from 1 June through 31 July 2013 were collected and retrospectively analysed. Only posteroanterior (PA) and anteroposterior (AP) X-ray studies were used, as lateral views were performed here only as an exception. Local ethics committee approval was obtained (No. 26–004 ex 13/14).
The mean patient age was 3.9 ± 5.0 years, with a range of 0 to 17.9 years. Two hundred seventy-two images of boys (45.5 %) and 326 of girls (54.5 %) were measured. For studying age dependency, patients were grouped based on the suggestion of the National Institute of Child Health and Human Development (NICHD) and the American Academy of Pediatrics [25, 26], as follows: newborn (0–29 days), infant (1–12 months), toddler (13–24 months), early childhood (2–5 years), middle childhood (6–11 years), and early adolescence (12–18 years).
Image acquisition
Images were acquired with two DR modalities: 47.7 % with the stationary FD-X (Siemens AG, Erlangen, Germany) and 52.3 % with the mobile DX-S (Agfa-Gevaert N.V., Mortsel, Belgium). FD-X patients were standing (36.7 %) or sitting (11.0 %), whereas DX-S images were acquired with the patient in supine position. All used well-calibrated X-ray tubes based on current national standards [27]: divergence of light field and exposed field smaller than 3 % with regard to the left plus right borders, smaller than 3 % with regard to the cranial plus caudal borders, and smaller than 4 % when adding all four divergences at a film focus distance (FFD) of 1 m.
Comforters were instructed to put on lead aprons and thyroid shields. For exposures in sitting patients, they were positioned behind the digital detector and advised to raise the child's hands for all patients not able to do so at command [20].
Radiographers had not been informed of the planned image quality analyses, and therefore all imaging studies were performed in routine operation. The included chest X-rays were analysed qualitatively and quantitatively based on the 1996 EC paediatric guidelines [5].
Qualitative parameters
The qualitative parameters were derived from the EC guidelines and are listed in Table 1. Rotation and tilting errors not further described by the EC guidelines were investigated. Patient rotation was defined as mediolateral tube and/or patient angulation, assessed by inspecting the clavicular heads in relation to the spinous processes [28]. Tilting was defined as craniocaudal tube and/or patient angulation, which was assessed based on the vertical position and shape of the clavicles. Cropped images were excluded from quantitative analyses.
Quantitative parameters
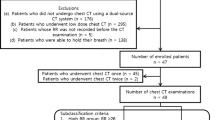
Quantitatively, the EC guidelines for paediatric AP/PA chest radiographs recommend a “minimal field size” (MinFS) extending from “just above the lung apices” to “T12/L1” [5]. The tolerated “maximal field size” (MaxFS) is obtained by adding the suggested age-dependent tolerance (listed in Table 1) “at each edge” of the MinFS, whereas the lateral borders are not explicitly described, and were chosen just outside the thoracic cage, which equals the borders of the thoracic wall in slim patients and balances out variable soft tissue mantles. Overexposure was defined as the additional percentage of irradiated area between MinFS and actual exposed area (AEA) in relation to the MinFS (=100 %), as depicted in Fig. 1. The percentages of irradiated tissue and age-dependent tolerance were automatically calculated using the tool that was developed. In addition, image rotation, distances from the MinFS to the corresponding AEA margins, and the position and possible truncation of the costophrenic angles were analysed.
Raw (unprocessed) sample chest X-ray of a 4-year-old girl. The green rectangle represents the minimal field size (MinFS = 100 %), and the blue rectangle represents the maximal field size (MaxFS) tolerated by the European Commission guidelines. The red polygon is the actual exposed (collimated) area (AEA). Overexposed sub-areas on all four sides (cervical, abdominal, left and right) are labelled in the figure
Workflow
Raw (unprocessed) DICOM images were exported to a personal computer running FIJI 1.47v [29], an ImageJ distribution (open source image processing software, http://rsbweb.nih.gov/ij/). A macro script was developed by the first author, supporting the user input of the EC guideline’s qualitative features. Quantitative standards were assessed by measuring and calculating all parameters semi-automatically on the basis of the following three user-dependent steps:
-
Step 1
Initially, the centre of T1 and T12 vertebral bodies and the tips of both costophrenic angles were selected and served as four landmark points (Fig. 2a). After completion, the image was automatically rotated by the angle calculated from the T1 to T12 coordinates versus a vertical line (Fig. 2b).
Fig. 2 (a–f) Raw (unprocessed) sample chest X-ray of a 4-years-old girl illustrating the steps of the measurement procedure explicitly described in the “Workflow” section within “Materials and methods”. Crosses represent user inputs, specific for the respective procedural stage
-
Step 2
The AEA was defined by a user-drawn four-sided polygon at the outer edges of collimation (Fig. 2c, e).
-
Step 3
Subsequently, the examiner plotted a rectangle, representing the MinFS (Fig. 2d, e). For intuitive operation, the macro pre-computed a user-adaptable first guess based on the landmark points mentioned above. In case of a cropped MinFS, the examiner verified that the image had a diagnostic field size.
After completion of user inputs, the macro script read DICOM image tags (study date, study time, birth date, sex, patient position, modality, and manufacturer) and automatically calculated areas, distances, and percentages (MinFS, MaxFS, AEA, overexposure, tolerance, left, right, cervical, and abdominal). To calculate the area of irradiated tissue, images were converted to black and white, which enabled automatic separation of air and tissue (Fig. 2f). In addition, verification that both costophrenic angles were inside the MinFS was performed.
Statistical analysis
Sample size calculation was performed with G*Power version 3.1.7 (http://www.gpower.hhu.de/) [30, 31], recommending at least 305 images (α error probability = 0.05, effect size f = 0.25) for the planned explorations. The data was analysed with descriptive statistics, t tests, and regression analyses.
All evaluations were performed by one observer (observer A: first author). In order to test inter-observer agreement, a random selection of 30 chest X-rays was quantified by two further examiners (observer B: R.M., radiology resident) and (observer C: M.G., radiology staff member). Observers B and C were informed on how to use the developed tool and studied the EC guidelines before their evaluation. For estimation of the intra-observer agreement, observer A re-evaluated these 30 chest X-rays after a delay of 4 weeks. Cohen’s kappa (ҡ) was used to assess qualitative differences. Absolute agreement regarding quantitative parameters was calculated with intraclass correlation coefficients (ICC [3, 1] - two-way mixed single measures).
P values less than 0.05 were assumed to be statistically significant. All statistical analyses were computed with SPSS Statistics Version 21 software (IBM Corp., Armonk, NY).
Results
The qualitative EC guideline recommendations, summarised in Table 1, were satisfied in the majority of the patients. Patients in the group of images with good inspiration were significantly older than those with X-rays considered to have poor inspiration (5.9 ± 5.2 years versus 2.0 ± 4.0 years, p < 0.001). With respect to rotation and tilting, correctly positioned patients were significantly older (mean age 4.8 ± 5.3 years versus 1.1 ± 2.6 years, p < 0.001).
At quantitative evaluation, mean image rotation was +0.6 ± 4.4° to the right, with a range of −14.7° (rotated to the left) to +17.0° (rotated to the right). Image rotation significantly decreased with patient age (R2 = 0.103, p < 0.001). Collimation had been applied in all 598 present cases. In 41.1 % (246/598) of images, MinFS truncations were present on one or more sides, and thus overexposure could not be calculated in these samples. In contrast, 95.0 % of all X-rays and 87.8 % (216/246) of images with a truncated MinFS had diagnostic field sizes, implying that these images were—at least partly—more narrowly collimated than recommended by the EC guidelines without losing clinically important information.
In the remaining 58.9 % (352/598), images with non-cropped MinFS, overexposure, and tissue overexposure in relation to the MinFS in total and for the sub-areas (summarised Tables 2 and 3) were computed. Total overexposure was +45.1 ± 18.9 % and tissue overexposure was +33.3 ± 13.3 %. Related findings are graphically shown in Fig. 3. The corresponding scatter plot, displaying the above-described age parameters, indicated that the peak overexposure occurred in patients aged approximately 6 months to 4 years, with lower overexposures in the youngest and oldest age groups. Analysis of the sub-areas revealed decreasing overexposure (R2 = 0.125, p < 0.001) and tissue overexposure (R2 = 0.257, p < 0.001) with age cervically, whereas it increased abdominally (R2 = 0.120, p < 0.001 and R2 = 0.103, p < 0.001). Overexposure and tissue overexposure in the lateral sub-areas were not affected by age. The greatest amounts of overexposure were detected in sitting patients (mean +66.1 ± 21.6 %) compared to radiographs in standing (mean +48.6 ± 15.4 %) and supine (mean +34.0 ± 15.1 %) positions. For all overexposed chest radiographs, the quality control tool computed a relative tissue irradiation of 76 ± 23 % cervically, 92 ± 8 % abdominally, and 61 ± 21 % in the lateral areas. Related findings are graphically shown in Fig. 4.
Scatter plot displaying overexposure with age (logarithmic notation for easier visualisation). Blue rectangles represent the total overexposure, red crosses the overexposed tissue, and black circles the respective age-dependent tolerance, all in relation to the MinFS (=100 %). Cubic trend lines with SD (95 %) confidence intervals are shown for overexposure and tissue overexposure
Of the total chest radiographs, 14.9 % were within the desired MinFS plus age-dependant tolerance levels (MaxFS). Based on the EC guidelines, 26 of 598 chest radiographs (4.3 %) completely fulfilled all qualitative standards, without MinFS truncation or MaxFS exceedance.
The mean distances from the MinFS to the corresponding AEA edges are listed in Table 3 and are graphically shown in Fig. 5a. Cervically (16 ± 13 mm) and laterally (12 ± 11 mm), distances from mean MinFS to AEA were regularly within the proposed guideline tolerance levels. The distance from the mean abdominal MinFS to AEA was 16 ± 24 mm. In newborns, the actual abdominal collimation edge was 3 mm higher (cranial) on average than the proposed MinFS border; thus radiographers collimated the abdominal margin more narrowly than guideline recommendations. This reversed with increasing age group: in early adolescents and middle childhood patients, radiographers collimated the abdominal margin about 4 cm wider (caudal) than recommended, minimising exclusion of the costophrenic angles. In 10.2 % of all images, and up to 36.5 % in the early adolescent age group, one or both costophrenic angles were below (not included inside) the proposed MinFS at the bottom edge (T12/L1), whereas they were effectively outside the AEA in only 1.5 %. Corresponding findings are shown in Figs. 5b and 6d. The abdominal MinFS margin was extended to L1/2 for testing purposes, resulting in reduction of costophrenic angle truncation to 0.4 %.
(a) Bar chart displaying the distances from the MinFS to its respective AEA edges among different age groups. (b) Mean distances (black lines, mm) from the lower costophrenic angle to the abdominal borders of MinFS (left diagram) and AEA (right diagram) compared to the corresponding percentages of costophrenic angles vertically outside (below) MinFS and AEA (bars, %)
Raw (unprocessed) chest radiographs of four patients with indicated MinFS. (a) AP chest film of a 3-month-old boy. The overexposure is +105 %, while the European guidelines would allow +38 %. (b) PA chest radiograph of a 6-year-old boy. The film demonstrates optimal and correct collimation, with minimal overexposure of +16 %, fulfilling all quantitative and qualitative requirements of the European guidelines. (c) PA chest radiograph of a 17-year-old adolescent, where both costophrenic angles are outside the recommended field size at the abdominal border. (d) PA sample image of a 3-year-old boy demonstrating a truncated MinFS at the right cervical corner because of image rotation (11.3°). Nevertheless, the image is diagnostic, but due to MinFS truncation, overexposure could not be calculated
Inter-observer assessment qualitatively showed a mean Cohen’s kappa of 0.79 (p = 0.007) among all observers. Poor agreement concerning the two guideline points “1.1 Performed at peak of inspiration” (ҡ = 0.39, p = 0.020) and “1.2 Reproduction of the thorax without rotation and tilting” (ҡ = 0.39, p = 0.027) was found. Quantitatively, average ICC among all observers was 0.92. Intra-observer mean ҡ was 0.92 (p < 0.001) on average, and mean ICC was 0.95.
Discussion
This study shows that EC guidelines for AP/PA chest radiography in paediatrics were only partially satisfied in the daily routine of a paediatric radiology division. While image quality itself was satisfactory, insufficient patient positioning and inspiration depth and inadequate field sizes were detected. On the other hand, some aspects of the EC guidelines were revealed to be less than ideal.
ICRP Publication 121 states that “Good radiographic technique requires attention to patient positioning and immobilisation…” [6]. Our data shows that proper patient positioning and immobilisation is most difficult in toddlers and early childhood, as young children may be fidgeting, uncooperative, or even hostile towards X-ray procedures [32, 33]. Therefore, comforters were routinely utilised in these age groups. Overall, patient “rotation and tilting” and “peak of inspiration” were more often fulfilled in older patients. Regarding inspiration depth, adult literature recommends that at least 10 posterior ribs should be visible above the diaphragm [28, 34], while paediatric references intergrade two additional steps of optimal inspiration with 8 posterior ribs in children younger than 3 years and 9 posterior ribs in children between 3 and 7 years of age [35, 36]. Both guideline points, inspiration depth and rotation and tilting, were subjective in inter-observer tests and should be less ambiguously delineated. The EC guideline actual image quality parameters were able to be adequately fulfilled in routine. However, points 1.4 to 1.7 of the guideline were found to overlap to a great extent, possibly providing an opportunity to combine them.
Only 4 % of the investigated images satisfied all of the EC guideline points (Fig. 6b), which leaves room for improvement at our division and raises the question of whether the current recommendations are fully applicable. Collimation was regularly within tolerance levels at the cervical and lateral MinFS borders. In this respect, ICRP Publication 121 claims that “…a certain degree of flexibility may be necessary…” and “…repeated use of unnecessarily large field sizes in paediatric patients is inappropriate”. Related studies highlight the necessity of proper collimation in paediatric radiography [37–39]. Furthermore, ICRP Publication 121 states that “…a field that is too small increases the risk of a diagnostic error or may require a second exposure”. In our study, all diagnostically necessary structures were included in 95 % of image samples. Therefore, a second exposure due to inappropriate field size should be less than 5 %, which is comparable to that reported in the existing literature [40, 41]. However, we expect a lower unavoidable retake rate, as a given clinical question may often be answered without the entire minimal field size.
Debateable issues were detected for the proposed abdominal MinFS margin at “T12/L1”. Application of the EC guidelines resulted in an abdominal MinFS margin that was too low (caudal) in newborns and infants, and increasingly too high (cranial) in patients in middle childhood and early adolescence. This would have caused truncation of one or both costophrenic angles in 10 % of our images and up to 37 % in the early adolescent age group, possibly requiring a second exposure. On the other hand, images in the newborn and infant age groups rarely exceeded the proposed field size tolerance levels. When the abdominal MinFS border was expanded to L1/2 for testing purposes, costophrenic angle truncation decreased to 0.4 %. It is questionable whether a static osseous collimation landmark defined at “T12/L1” is suitable for the mobile diaphragm, especially in growing patients with changing body proportions. This study’s results suggest that costophrenic angles are rarely below vertebral levels of T11/T12 in patients younger than 1 year, T12/L1 in patients aged 1 to 5 years, and L1/2 in patients older than 6 years. For simplicity, we would suggest defining the abdominal MinFS margin just below the costophrenic angles, which would be in compliance with the American College of Radiology-Society for Pediatric Radiology guidelines [11, 42].
The EC guidelines define a minimal field size, but conflictingly, the lateral borders are not clearly described. Although lateral amounts of irradiated tissue were low, insufficient or missing lateral collimation degrades image quality and increases scatter radiation [5, 6, 20]. Examples of suboptimal and ideal collimation are shown in Fig. 6a, b. Our results indicate proper recommended tolerance levels, with the exception of young infants aged 29 days to approximately 3 months (compare black circles in Fig. 3), where tolerated overexposure was above average. This was the result of an abrupt tolerance shift from 1 to 2 cm between newborns and infants. Comparing the data from Fig. 3 and common growth charts [43], a better cut-off level would be 3 months when switching from 1 to 2 cm. Another alternative would be patient size-dependent tolerance levels.
In the literature, only a few studies have investigated field sizes and collimation in paediatric chest radiography, all of which reported considerable amounts of unnecessarily irradiated structures [18, 44–46]. If our results are adapted to match the only related quantitative study, craniocaudal extension to non-thoracic structures was 34 %, smaller than the previously reported 43 % [44].
In a critical evaluation of the EC guidelines for paediatric chest radiographs by reference to our data, some debatable issues were revealed. First and foremost, the suggested abdominal MinFS border seemed to be suboptimal in large age ranges. Moreover, the field size tolerance of 2 cm appeared to be too loose in young infants. The qualitative parameters “without rotation and tilting” and “peak of inspiration” were found to be subjective. In contrast, the actual image quality parameters were consistently met, indicating redundancy. It is the authors’ opinion that condensation and clarification of the current EC guidelines for AP/PA chest radiographs, based on this study’s results and as discussed in the literature, could be approached follows:
-
1.
Minimal field size (MinFS): should extend from just above the lung apices to directly below both costophrenic angles, sideways just outside the thoracic cage.
-
2.
Depth of Inspiration: at least 8 posterior ribs in newborns, infants and toddlers, 9 in early childhood, and 10 in all older patients visible above the diaphragm.
-
3.
Patient rotation: spinous processes horizontally centred between clavicle heads and clavicle heads vertically at a vertebral level of T2 to T4.
-
4.
Sharpness and contrast: sharp and high-contrast reproduction of vascular lung pattern, retrocardiac lung and spine.
Our quality control tool can be requested free of charge from the corresponding author. With a measuring time of approximately 30 seconds per image, the procedure presented herein time-efficiently provides constructive data to assist in achieving the best possible results for paediatric patients.
The following study limitations must be mentioned. Due to the retrospective design, single examinations could not be linked to the responsible radiographers, as there were no such records saved within the DICOM headers. Individual differences were therefore not assessed. Actual exposure parameters and radiation doses were not analysed, yet they were repeatedly well below diagnostic reference levels in mandatory national audits [47].
In conclusion, this study introduces a new quality control tool which allows for time-efficient evaluation of field sizes, related distances, overexposures, and quality parameters in chest radiographs based on the EC guidelines. With the use of this tool, partly overexposed field sizes were detected at the authors’ paediatric radiology division. In contrast, the proposed paediatric EC guideline’s abdominal collimation border was revealed to be inadequate in children to some extent, and parts of the quality suggestions were found to be either subjective or redundant. Depending on respective age spans, strict EC guideline adherence could lead to cropped or needlessly overexposed field sizes, possibly requiring a second exposure. Therefore, future EC guideline adaptions appear reasonable and should be discussed.
Abbreviations
- ACR:
-
American College of Radiology
- AEA:
-
Actual exposed area
- AP:
-
Anteroposterior
- DICOM:
-
Digital Imaging and Communications in Medicine
- DR:
-
Digital radiography
- EC:
-
European Commission
- FFD:
-
Film focus distance
- ICC:
-
Intraclass correlation coefficient
- ICRP:
-
International Commission on Radiological Protection
- MaxFS:
-
Maximal field size
- MinFS:
-
Minimal field size
- PA:
-
Posteroanterior
- SD:
-
Standard deviation
- WHO:
-
World Health Organisation
References
International Atomic Energy Agency (2001) Proceedings of an international conference held in Málaga, Spain, 26–30 March 2001, International Conference on Radiological Protection of Patients in Diagnostic and Interventional Radiology, Nuclear Medicine and Radiotherapy. IAEA, Malaga, p 165
Joarde R, Crundwell N, Joarder R (2009) Chest x-ray in clinical practice [Ebook], 1st edn. Springer, London
Don S, Macdougall R, Strauss K et al (2013) Image gently campaign back to basics initiative: ten steps to help manage radiation dose in pediatric digital radiography. AJR Am J Roentgenol 200:W431–W436
Moore QT, Don S, Goske MJ et al (2012) Image gently: using exposure indicators to improve pediatric digital radiography. Radiol Technol 84:93–99
European Commission (1996) European Guidelines on Quality Criteria for Diagnostic Radiographic Images in Paediatrics. ECSC-EC-EAEC, Brussels
Khong PL, Ringertz H, Donoghue V et al (2013) ICRP publication 121: Radiological protection in paediatric diagnostic and interventional radiology. Ann ICRP 42:1–63
Willis CE, Slovis TL (2005) The ALARA concept in pediatric CR and DR: dose reduction in pediatric radiographic exams–a white paper conference. AJR Am J Roentgenol 184:373–374
Amis ES Jr, Butler PF (2010) ACR white paper on radiation dose in medicine: three years later. J Am Coll Radiol 7:865–870
Amis ES Jr, Butler PF, Applegate KE et al (2007) American College of Radiology white paper on radiation dose in medicine. J Am Coll Radiol 4:272–284
Herrmann TL, Fauber TL, Gill J et al (2012) Best practices in digital radiography. Radiol Technol 84:83–89
American College of Radiology (ACR), Society for Pediatric Radiology (SPR) (2011) ACR–SPR Practice Guideline for the Performance of Pediatric and Adult Chest Radiography. American College of Radiology, Reston, p 5
Sandström S, Ostensen H, Pettersson H, Åkerman K, World Health Organization., International Society of Radiology (2003) Radiographic Technique and Projections. In: Ostensen H, Pettersson H (eds) The WHO manual of diagnostic imaging. World Health Organization (WHO) and International Society of Radiology (ISR), Geneva, p 135
European Commission (1996) European Guidelines on Quality Criteria for Diagnostic Radiographic Images. ECSC-EC-EAEC, Brussels
Brennan PC, Johnston D (2002) Irish X-ray departments demonstrate varying levels of adherence to European guidelines on good radiographic technique. Br J Radiol 75:243–248
Grewal RK, Young N, Colins L, Karunnaratne N, Sabharwal N (2012) Digital chest radiography image quality assessment with dose reduction. Australas Phys Eng Sci Med 35:71–80
Muhogora WE, Nyanda AM, Kazema RR (2001) Experiences with the European guidelines on quality criteria for radiographic images in Tanzania. J Appl Clin Med Phys 2:219–226
Goske MJ, Charkot E, Herrmann T et al (2011) Image Gently: challenges for radiologic technologists when performing digital radiography in children. Pediatr Radiol 41:611–619
Kostova-Lefterova D, Taseva D, Ingilizova K, Hristova-Popova J, Vassileva J (2011) Potential for optimisation of paediatric chest X-ray examination. Radiat Prot Dosim 147:168–170
Gogos KA, Yakoumakis EN, Tsalafoutas IA, Makri TK (2003) Radiation dose considerations in common paediatric X-ray examinations. Pediatr Radiol 33:236–240
Oppelt B (2010) Pediatric radiology for medical-technical radiology assistants/radiologists, 1st edn. Thieme, Stuttgart
Suliman II, Elawed SO (2013) Radiation dose measurements for optimisation of chest X-ray examinations of children in general radiography hospitals. Radiat Prot Dosim 156:310–314
Bly R, Jarvinen H, Korpela MH, Tenkanen-Rautakoski P, Makinen A (2011) Estimated collective effective dose to the population from X-ray and nuclear medicine examinations in Finland. Radiat Prot Dosim 147:233–236
Teles P, Carmen de Sousa M, Paulo G et al (2013) Estimation of the collective dose in the Portuguese population due to medical procedures in 2010. Radiat Prot Dosim 154:446–458
Zenone F, Aimonetto S, Catuzzo P et al (2012) Effective dose delivered by conventional radiology to Aosta Valley population between 2002 and 2009. Br J Radiol 85:e330–e338
Williams K, Thomson D, Seto I et al (2012) Standard 6: age groups for pediatric trials. Pediatrics 129:S153–S160
NICHD (2015) Guidance for Clinical Researchers: Harmonizing Pediatric Terminology. Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), Bethesda, MD. Available via https://www.nichd.nih.gov/health/clinicalresearch/clinical-researchers/terminology/Pages/index.aspx accessed 02-02-2015
ÖNORM national (2008) ÖNORM S 5240–8: Sicherung der Bildqualität in röntgendiagnostischen Betrieben - Teil 8: Konstanzprüfung an medizinischen Röntgen-Projektionsradiographie-Einrichtungen mit digitalen Bildempfängersystemen. ÖNORM, Vienna
Hobbs DL (2007) Chest radiography for radiologic technologists. Radiol Technol 78:494–516
Schindelin J, Arganda-Carreras I, Frise E et al (2012) Fiji: an open-source platform for biological-image analysis. Nat Methods 9:676–682
Faul F, Erdfelder E, Buchner A, Lang A-G (2009) Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav Res Methods 41:1149–1160
Faul F, Erdfelder E, Lang AG, Buchner A (2007) G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods 39:175–191
Alexander M (2012) Managing patient stress in pediatric radiology. Radiol Technol 83:549–560
Yoo S-J, MacDonald C, Babyn PS (2010) Chest radiographic interpretation in pediatric cardiac patients, 1st edn. Thieme, New York, p 317
Bontrager KL (2001) Textbook of radiographic positioning and related anatomy, 5th edn. Mosby, St. Louis
Hardy M, Boynes S (2003) Paediatric radiography. Blackwell Science, Oxford
Bramson RT, Griscom NT, Cleveland RH (2005) Interpretation of chest radiographs in infants with cough and fever. Radiology 236:22–29
Bomer J, Wiersma-Deijl L, Holscher HC (2013) Electronic collimation and radiation protection in paediatric digital radiography: revival of the silver lining. Insights Imaging 4:723–727
Fauber TL, Dempsey MC (2013) X-ray field size and patient dosimetry. Radiol Technol 85:155–161
Hawking NG, Sharp TD (2013) Decreasing radiation exposure on pediatric portable chest radiographs. Radiol Technol 85:9–16
Akhtar W, Aslam M, Ali A, Mirza K, Ahmad N (2008) Film retakes in digital and conventional radiography. J Coll Physicians Surg Pak 18:151–153
Polunin N, Lim TA, Tan KP (1998) Reduction in retake rates and radiation dosage through computed radiography. Ann Acad Med Singap 27:805–807
American College of Radiology (ACR), Society for Pediatric Radiology (SPR) (2011) ACR–SPR Practice Parameter for the Performance of Portable (Mobile Unit) Chest Radiography. American College of Radiology, Reston, p 7
Grummer-Strawn LM, Reinold C, Krebs NF, (CDC) CfDCaP (2010) Use of World Health Organization and CDC growth charts for children aged 0–59 months in the United States. MMWR Recomm Rep 59:1–15
Soboleski D, Theriault C, Acker A, Dagnone V, Manson D (2006) Unnecessary irradiation to non-thoracic structures during pediatric chest radiography. Pediatr Radiol 36:22–25
Alt CD, Engelmann D, Schenk JP, Troeger J (2006) Quality control of thoracic X-rays in children in diagnostic centers with and without pediatric-radiologic competence. Röfo 178:191–199
Engelmann D, Dutting T, Wunsch R, Troger J (2001) Quality of ambulatory thoracic radiography in the child–a pilot study. Radiologe 41:442–446
Billinger J, Nowotny R, Homolka P (2010) Diagnostic reference levels in pediatric radiology in Austria. Eur Radiol 20:1572–1579
Acknowledgments
The scientific guarantor of this publication is Prof. Dr. Erich Sorantin. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors (Prof. Dr. Erich Sorantin) has significant statistical expertise. Institutional review board approval was obtained. Written informed consent was waived by the institutional review board. Methodology: retrospective, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tschauner, S., Marterer, R., Gübitz, M. et al. European Guidelines for AP/PA chest X-rays: routinely satisfiable in a paediatric radiology division?. Eur Radiol 26, 495–505 (2016). https://doi.org/10.1007/s00330-015-3836-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3836-7