Abstract
Purpose
To investigate the efficacy of percutaneous chemonucleolysis using ethanol gel (PCEG) in alleviating radicular pain due to disc herniation after failure of conservative treatment.
Materials and methods
After failure of conservative treatment, PCEG was performed under fluoroscopic guidance in 42 patients with sciatica >4/10 on a Visual Analog Scale (VAS) for at least 6 weeks and consistent disc herniation on MRI or CT <3 months. The VAS pain score was determined at baseline, then after 1 and 3 months. We assessed the influence of patient-related factors (age, gender, pain duration) and disc herniation-related factors (level, migration pattern, disc herniation-related spinal stenosis) on outcome of PCEG.
Results
Mean pain duration was 6.7 months. Pain intensity decreased by 44 % and 62.6 % after 1 and 3 months, respectively, versus baseline (P = 0.007). A mild improvement was noted by the rheumatologist in 30/42 (71.4 %) and 36/42 (85.7 %) patients after 1 and 3 months, respectively, and in 31/42 (73.8 %) and 33/42 (78.6 %) patients by self-evaluation. Patients who failed PCEG were significantly older (49.8 vs. 37.3 years, P = 0.03). None of the other variables studied were significantly associated with pain relief.
Conclusion
PCEG may significantly improve disc-related radicular pain refractory to conservative treatment.
Key Points
• Percutaneous chemonucleolysis using ethanol gel (PCEG) is feasible on an outpatient basis.
• PCEG improves disc-related radicular pain refractory to conservative treatment.
• PCEG is feasible on an outpatient basis.
• Failure of PCEG does not interfere with subsequent spinal surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Nerve root pain due to disc herniation is a common symptom responsible for functional disability, an impaired ability to work and engage in social activities and quality-of-life alterations. Conservative treatment is the first-line strategy and is associated with improvements in pain and function in 95 % of patients within 1 to 12 months [1, 2]. Open surgery is considered in patients with persistent pain and functional disability despite appropriate conservative care. Open surgery, although rapidly effective in most patients [3], is costly, exposes the patient to the risks inherent in general anaesthesia, and can be followed by post-operative complications, chronic pain, and persistent disability. In several studies, outcomes after 1-2 years were not significantly better after open surgery than after conservative treatment [4, 5]. A broad array of minimally invasive procedures for treating disc-related radiculopathy has been evaluated as alternatives to open surgery. Chemonucleolysis using chymopapain proved effective [6] but was banned in the early 2000s due to unacceptable adverse effects. Since then, many other percutaneous intradiscal procedures have been tested, including disc decompression using laser energy (laser discectomy) [7, 8], nucleoplasty based on Coblation® technology [9], automated percutaneous lumbar discectomy [10] and intradiscal oxygen-ozone injection [10–12]. None of these procedures seemed as effective as open surgery. Chemonucleolysis using pure ethanol is a potentially attractive method but has raised concern about the risk of direct nerve damage in the event of ethanol leakage into the epidural space or foramen [13]. An ethanol gel has been developed to limit ethanol diffusion, thereby preventing direct nerve toxicity.
Percutaneous chemonucleolysis using ethanol gel (PCEG) does not aim to be more effective than open surgery but aims to be either as good or sufficiently effective to reduce the pain to an acceptable level by the patient, with less complications and risks than surgery. Our objective was then to evaluate whether PCEG was a valid option in patients with sciatica due to lumbar disc herniation and refractory to conservative treatment. We prospectively studied 42 patients managed at a single institution and evaluated by a physician who was not involved in the percutaneous procedure.
Materials and methods
Institutional review board approval and written informed consent of the patients were obtained.
Patients
Between January 2009 and May 2013, consecutive patients seen at the outpatient clinic for sciatica were included by a single rheumatologist (JD). Inclusion criteria were age between 18 and 70 years; continuous radicular pain radiating to the lower limb, with a duration ≥6 weeks and an intensity >4/10 as rated by the patient on a visual analog scale (VAS); failure of conservative treatment combining analgesics, anti-inflammatory drugs, and at least two epidural steroid injections including at least one performed under fluoroscopic or computed tomography (CT) guidance; and evidence by CT or MRI within the past three months of a herniated disc putting pressure on a nerve root at a single lumbar level consistent with the clinical pain. We excluded patients with any of the following: contraindication to percutaneous chemonucleolysis (coagulopathy or infection), history of lumbar spine surgery, disagreement between the clinical and imaging findings, muscle strength ≤3/5 or impaired sphincter function, degenerative or developmental lumbar spinal stenosis (anteroposterior spinal canal diameter <12 mm by CT or MRI), calcified or excluded disc herniation, disc space narrowing ≥60 % (see the “Baseline Image analysis” section), spondylolisthesis or degenerative disease (intervertebral or lumbar facet joint osteoarthritis) as a possible contributor to the nerve root pain, or any medical condition or treatment that might interfere with pain evaluation.
Data collection
Each patient was evaluated at baseline then one month (M1) and three months (M3) after PCEG. A research assistant (OT) interviewed each patient by telephone at least eight months after PCEG. The interview collected information on return to work and current occupation, need for spinal surgery after PCEG, and percentage of residual pain intensity relative to pain intensity at M3.
Adverse events during and after PCEG were recorded.
Pain evaluations
Pain duration before chemonucleolysis and occupational status were recorded. A single rheumatologist (JD, with a 16-year experience in rheumatology consultation) used a VAS to assess pain intensity at baseline then at M1 and M3. Changes in pain intensity were computed as percentages for the following time intervals: baseline to M1, baseline to M3, and M1 to M3. We categorized the patients based on VAS pain score changes as described by Farrar JT et al. [14]: <20 %, failure; ≥20 % to <30 %, limited improvement; ≥30 % to <50 %, moderate improvement; and ≥50 %, substantial improvement. We computed the percentage of patients reporting a minimal clinically important improvement (MCII) defined as an at least 15 % decrease in absolute pain intensity or 20 % decrease in relative pain intensity versus baseline [15], at M1 and M3.
Pain relief at M1 and M3 was self-evaluated by the patients as none, mild, substantial, or complete. The percentage of patients in the patient acceptable symptom state (PASS) at M1 and M3 was determined. The PASS is a state of stable symptom intensity in which the patient reports feeling good (not necessarily better). For our study, a VAS score ≤4/10 was required for the PASS, in accordance with previous work [16].
Baseline image analysis
CT or MR images were read in random order by a single radiologist (ST) who had four years of experience in musculoskeletal imaging and was blind to the clinical data. A single workstation was used (CarestreamVue PACS 11.3, Carestream Health Inc., NY, USA). The time from CT or MRI to PCEG was recorded.
To verify patient eligibility for the study, the radiologist confirmed the presence of a single lumbar disc herniation putting pressure on a nerve root at a level consistent with the clinical findings, as well as the absence of disc calcification or complete disc extrusion (loss of all contact with the disc of origin). The following features of the herniated disc were then recorded: shape, recorded as protrusion (focal or asymmetric extension of the disk beyond the intervertebral space) or extrusion (marked extension of the disc beyond the intervertebral space) [17]; location within the spinal canal, recorded as central, paracentral, or foraminal; and disc migration, recorded as none, cephalad, or caudad.
Relative disc herniation size was estimated as the percentage of spinal-canal cross-section occupied by herniated disc material. The boundaries of the spinal canal and disc herniation were delineated using the computer mouse on an axial T2-weighted MRI image or on a CT image with soft tissue settings, at the level where the disc herniation was largest. Disc space narrowing was measured comparatively with the next cephalad-normal intervertebral disc space, as a ratio: disc space narrowing = 1 - [height of abnormal disc space/height of normal disc space]. Height was measured at the centre of the disc space on a midline sagittal MRI T1-weighted image or CT image with bone window settings. A ratio >0.6 was an exclusion criterion.
Percutaneous chemonucleolysis with ethanol gel (PCEG)
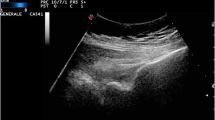
Fluoroscopic guidance (C-arm X-ray system, Siemens Healthcare, Germany) was used to inject ethanol gel (Discogel®, Gelscom, France) into the nucleus pulposus. Analgesia was achieved by inhalation of an equimolar nitrous oxide/oxygen mixture (Kalinox™, AirLiquide Healthcare, France) and local injection of lidocaine into the subcutaneous tissue then liberally during needle advancement. A posterolateral approach to the intervertebral disc was used as described by Laredo et al. [18]. A spinal needle (18G, 15 cm) was positioned at the disc surface and a Chiba needle (22G, 22 cm, Optimed®, Germany) was introduced through the spinal needle and advanced to the centre of the disc space. Contrast material (0.5-1 mL) (Visipaque™ 320, GE Healthcare, France) was injected under fluoroscopic guidance in order to check needle tip position and to observe the pattern of contrast distribution within the disc space. The volume of contrast agent had to be sufficient to dye the disc space but was limited in order not to increase the intradiscal pressure and, therefore, the patient’s pain and to allow, secondarily, the injection of a sufficient volume of ethanol gel. A large disc rupture with rapid epidural leakage was ruled out by fluoroscopy and discograms taken at the end of contrast material injection (Fig. 1). A volume of 0.5 to 1 mL of ethanol gel was injected slowly (0.1 mL /min), depending on disc resistance to injection and the pain intensity described by the patient during the procedure. Total radiation exposure during the procedure was recorded. The patient was monitored for six hours after the procedure before hospital discharge.
Male patient of 37-years-old with a 6-month history of sciatica refractory to conservative treatment. MR T2 weighted sagittal (a) and axial (b) images immediately prior to PCEG show a paracentral extrusion of the disc at L5-S1 level putting pressure on the left S1 nerve root consistent with the radicular pain. Standard lateral (c) and anteroposterior (d) radiographs taken during PCEG show L5-S1 discograms after injection of the contrast agent and before injection of ethanol gel into the disc
Statistical analysis
Differences between pain intensities at the three time points (baseline, M1, and M3) and between M3 and residual pain were assessed using the Kruskal-Wallis or the Mann-Whitney test. We used the Cochran-Armitage test to evaluate the difference between M1 and M3 in the proportion of patients with failed PCEG according to the rheumatologist and the patient self-evaluation.
We evaluated the potential influence of several variables on pain relief at M3 versus baseline. The influence of categorical variables (gender, disc level, location of the herniation, and migration patter) was assessed using the t test, Mann-Whitney test or, in case of multiple comparisons, the Kruskal-Wallis test followed by Dunn’s multiple comparisons test if the Kruskal-Wallis test was globally significant. The influence of continuous variables (age, pain duration at PCEG, relative disc herniation size, and disc space narrowing ratio) was evaluated by computing Spearman’s correlation coefficient. Differences in pain intensity changes across groups defined by the abovementioned variables were assessed using the Kruskal-Wallis test followed, in the event of a significant difference, by Dunn’s multiple comparisons test.
P values <0.05 were considered significant. We computed 95 % confidence intervals (95%CIs). The statistical analyses were performed using SAS/STAT 9.3 software (SAS Institute, Cary, NC, USA).
Results
Patients: baseline characteristics
The study included 42 patients, 25 (59.5 %) males and 17 (40.5 %) females (male/female ratio, 1.5) with a mean age of 39.1 ± 10.8 years (range, 18-66). Of the 37 (88.1 %) employed patients, 22 (59.5 %) were on sick leave because of their nerve root pain at baseline. Pain duration at PCEG was 6.7 ± 4 months (range, 2.5-20).
MRI was performed before PCEG in 30 (71.4 %) of patients and CT in 12 of the patients (28.6 %). Mean time from MRI or CT to PCEG was 29.2 ± 34.7 days (range, 0-111). The disc herniation was at L3-L4 in one (2.4 %) patient, L4-L5 in 14 (33.3 %) patients, and L5-S1 in 27 (64.3 %) patients. The disc was protruded in 39 (92.9 %) patients and extruded in three patients (7.1 %). The disc herniation was located centrally in the spinal canal in ten (23.8 %) patients, in the right paracentral region in 13 patients (31 %), and in the left paracentral region in 19 patients (45.2 %). Migration relative to the disc space was absent in 19 (45.2 %) patients, cephalad in four patients (9.6 %) and caudad in 19 patients (45.2 %). Mean relative disc herniation size was 37 % ± 13 % (range, 7-65), and mean disc space narrowing ratio was 17 % ± 11 % (range, -3 to +41).
Chemonucleolysis
The mean ethanol gel volume injected was 0.85 ± 0.18 mL (range, 0.5-1). Total radiation exposure was 2.2 ± 1.3 mGy · m2 (range, 0.63-6.2). Mean duration of PCEG was 60 ± 20 minutes.
Adverse events
Two adverse events in two different patients were recorded. One patient experienced transient pain exacerbation starting one week after PCEG and followed by complete pain resolution. The other had transient episodes of urinary incontinence triggered by coughing during the month following PCEG, which also resolved completely. Both patients underwent postoperative MRI of the lumbar spine and spinal cord, which showed no change in the appearance of the herniated disc and no new abnormalities.
Variation of pain
Preoperative and postoperative VAS pain values are provided in Table 1 and Fig. 2. Variation in pain VAS is shown in Table 2. Categorization of pain variation according to the rheumatologist and patient self-evaluation are shown in Fig. 3a and b, respectively.
Evolution of pain intensity values on the Visual Analog Scale (VAS) at the initial consultation (M0) and at one month (M1) and three months (M3) after chemonucleolysis. A telephone interview evaluated the Residual Pain (RP) from eight months after the nucleolysis. Note−. M, Month; RP, residual pain as assessed during the telephone interview eight to 48 months after percutaneous chemonucleolysis with ethanol gel. The whiskers show the range of values and the horizontal line within each box the median
According to the rheumatologist, a “mild” or greater improvement was observed in 30/42 (71.4 %) patients at M1 and 36/42 (85.7 %) at M3.
According to the self-patient evaluation, a “mild” or greater improvement was reported at M1 by 31/42 (73.8 %) patients and at M3 by 33/42 (78.6 %) patients.
The percentage of patients with a MCII was 30/42 (71.4 %) at M1 and 36/42 (85.7 %) at M3, and the percentage of patients with PASS was 23/42 (54.8 %) at M1 and 31/42 (73.8 %) at M3.
Effect of PCEG on pain intensity
Table 1 and Fig. 2 report the absolute VAS pain score values before and after PCEG and Table 2 the changes in VAS pain scores. Figure 3a and b, reports the categorization of the patients according to the evaluations by the rheumatologist and patient, respectively. The analysis of changes in absolute and relative VAS pain scores is reported in Tables 1 and 2, respectively. Significant pain relief versus baseline was noted at M3 and at the telephone interview (P = 0.01).
According to the rheumatologist, the improvement was limited or greater in 30 (71.4 %) patients at M1 and 36 (85.7 %) at M3. Patients self-evaluated their pain relief as mild or greater in 31 (73.8 %) cases as M1 and 33 (78.6 %) cases at M3. The minimal clinically important improvement was achieved by 30 (71.4 %) patients at M1 and 36 (85.7 %) at M3 and the PASS by 23 (54.8 %) patients at M1 and 31 (73.8 %) at M3. The difference in PCEG failure rates between M1 and M3 according to the rheumatologist was significant (P = 0.02), whereas the difference in the same variable according to the patient self-evaluation was not significant (P = 0.35).
All patients were interviewed by telephone. Mean time from PCEG to interview was 23.5 ± 10.9 months (range, 8-48; median, 21). Residual pain was assessed in 40 (95.2 %) patients (Fig. 2). Spinal surgery was required because of persistent pain in nine (21.4 %) patients, four males and five females, a mean of 6.1 ± 3.9 months (range, 3-15; median, 4) after PCEG. No pathological damage possibly related to ethanol gel injection was found intraoperatively. Of the 22 patients on sick leave at baseline, 14 (63.6 %) returned to work, a mean of 8.7 ± 8 months (range, 1-27; median, 7) after PCEG. Return to work occurred within six months after PCEG in 8/14 (57.1 %) patients and within three months in 4/14 (28.6 %) patients.
Evaluation of factors potentially associated with the treatment response
The VAS pain score change from baseline to M3 was not significantly influenced by gender (P = 0.37), disc level (P = 0.36), location of disc herniation (P = 0.43), migration pattern (P = 0.58), age (P = 0.40), pain duration (P = 0.12), relative disc herniation size (P = 0.30), or disc space narrowing ratio (P = 0.30). Patients with PCEG failure at M3 were significantly older compared to the other patients (mean age, 49.8 ± 12.2 years versus 37.3 ± 9.9 years, respectively; P = 0.03). These two groups were not significantly different for gender (P = 0.98), pain duration (P = 0.11), relative disc herniation size (P = 0.10), disc space narrowing ratio (P = 0.46), or migration pattern (P = 0.96).
Patients who underwent spinal surgery following PCEG were not significantly different from the other patients for gender (P = 0.35), age (P = 0.65), pain duration at PCEG (P = 0.63), disc space narrowing ratio (P = 0.56), or migration pattern (P = 0.23). A trend was found towards an association between spinal surgery and larger disc herniation (mean relative disc herniation size, 44 % ± 12.6 % in the group with surgery versus 35.1 % ± 12.6 % in the group without surgery; P = 0.06).
Discussion
In our study, nerve root pain related to disc herniation and refractory to conservative treatment improved significantly after PCEG. At M3, most patients were improved and had achieved the PASS. Only one fifth of patients required spinal surgery because of persistent pain. Among patients on sick leave, two thirds had returned to work by the time of the telephone interview. Only two patients experienced adverse events, which were mild and resolved spontaneously in both cases.
To our knowledge, four studies have investigated the efficacy of PCEG in alleviating disc-related nerve root pain refractory to conservative treatment [19–22]. Success rates were higher than in our study. Differences in study design may contribute to explain this discrepancy. In the study by De Sèze et al. ([21], the pain was evaluated by a nurse immediately and eight days after PCEG then by the physician who performed the procedure eight weeks after PCEG. Immediate postoperative pain reflects the patient’s experience of the procedure but is heavily influenced by the operating conditions (analgesics, environment, placebo effect, and physician-patient interaction) and does not provide information on clinical efficacy. In addition, evaluation by the physician who performed the procedure can introduce evaluation and attrition bias. In our study, pain was evaluated by a rheumatologist who was not involved in the PCEG procedure. In the study by Theron et al. [19], nearly 90 % of patients were improved at M1 but a facet-joint steroid injection was given at the time of PCEG and may have contributed to the pain relief. Stagni et al. [20] reported a 75 % success rate of PCEG after six months in patients who had failed oxygen-ozone chemonucleolysis. Thus, the study population was not representative of the general population of patients with refractory nerve root pain. Finally, the study by Bellini et al. [22] showed a high rate of success but inclusion criteria are less strict: cervical and lumbar disc herniations are pooled together, some patients have multiple herniations, one patient had a previous history of spine surgery. Moreover, the conservative treatment did not include epidural steroid injections. Our lower success rate may be explained by the differences in inclusion criteria and study design.
The efficacy of PCEG and its interest as a therapeutic option could be best assessed in comparison with surgery. Spinal surgery provides rapid and lasting improvements in over 80 % of carefully selected patients with predominant nerve root pain. The improvements are sustained after one year in more than two thirds of cases [23]. We found a nonlinear increase in pain relief over time, with the greatest changes occurring over the first month. Although pain relief is delayed after PCEG compared to surgery, our results are encouraging since the patients had failed to respond to conservative treatment given for a mean of 6.7 months.
Only two patients experienced adverse events, whose relationship with the ethanol gel injection is unclear. We found no plausible explanation to the transient episodes of urinary incontinence experienced by one of these patients. MRI showed no displacement of the herniated disc material or evidence of inflammation of the disc, bone, or nervous tissue, and neither did the laboratory tests show any evidence of inflammation.
We looked for associations linking clinical and imaging-study features to PCEG outcomes. Most of the features studied had no significant associations with the treatment response, in keeping with previous studies comparing conservative treatment and surgery for disc herniation [4]. That pain duration at PCEG had no influence on pain relief is consistent with the results of surgical case-series studies [24, 25]. However, we found a nonsignificant trend (P = 0.06) toward an association between a larger relative size of the disc herniation and PCEG failure defined as both absence of pain relief and need for spinal surgery. Finally, patients with PCEG failure at M3 were significantly older compared to the other patients. Further studies of PCEG should seek to confirm that patient age and disc herniation size should be taken into account when choosing between PCEG and surgery.
Since the withdrawal of chymopapain from the market in the early 2000s, no other percutaneous agent has been proven effective in relieving disc-related nerve root pain refractory to conservative treatment. Ethanol gel may act by inducing both immediate necrosis of the nucleus pulposus and delayed scarring and sealing of the annulus fibrosus [19, 21]. We suggest that percutaneous chemonucleolysis using ethanol gel is a safe outpatient procedure that may obviate the need for spinal surgery in many patients with disc-related sciatica refractory to conservative treatment.
Our study has several limitations. We used an open design with no comparison to a placebo or spinal surgery. However, this design was appropriate for a pilot study performed as a preliminary to randomized trials. Also, we applied stringent criteria for patient selection, the PCEG procedure, and the assessment of outcomes. The patient recruitment at a single center may have introduced selection bias. More specifically, the occupational profile of our patients may not be representative of all patients with refractory disc-related nerve root pain. The time from PCEG to the telephone interview varied from eight to 48 months. However, no patient was lost-to-follow-up and all patients who finally required surgery were identified. Moreover, mid-term and long-term pain assessments may be less relevant than the assessment within the first six months for evaluating the efficacy of chemonucleolysis: in studies comparing prolonged conservative therapy to surgery, the difference in pain improvement decreased over time due to the spontaneously favorable course of nerve root pain. Thus, in a comparison of surgical and conservative treatments, the differences in outcomes decreased significantly after six months [26]. In another study, the initial difference between surgery and prolonged conservative treatment was no longer apparent after one year [3]. Therefore, the first six months probably constitute the optimal time window for evaluating the efficacy of the percutaneous treatments of disc-related nerve root pain.
In conclusion, our findings suggest that PCEG may hold promise in patients with disc-related nerve root pain refractory to conservative treatment. The pain improves gradually, with the largest gains being achieved during the first month. Failure of the procedure is more common in older patients. Other features such as pain duration, patient gender, morphology of the herniated disc, and intervertebral disc height have no significant influence on the treatment response. PCEG is an outpatient percutaneous procedure that does not interfere with subsequent spinal surgery.
References
Kraemer J (1995) Natural course and prognosis of intervertebral disc diseases. International Society for the Study of the Lumbar Spine Seattle, Washington, June 1994. Spine 20:635–639
Legrand E, Bouvard B, Audran M, Fournier D, Valat JP (2007) Sciatica from disk herniation: medical treatment or surgery? Jt Bone Spine Rev Rhum 74:530–535
Peul WC, van Houwelingen HC, van den Hout WB, Brand R, Eekhof JAH, Tans JTJ et al (2007) Surgery versus prolonged conservative treatment for sciatica. N Engl J Med 356:2245–2256
Deyo RA (2007) Back surgery–who needs it? N Engl J Med 356:2239–2243
Imagama S, Kawakami N, Tsuji T, Ohara T, Matsubara Y, Kanemura T et al (2011) Perioperative complications and adverse events after lumbar spinal surgery: evaluation of 1012 operations at a single center. J Orthop Sci Off J Jpn Orthop Assoc 16:510–515
Fraser RD (1984) Chymopapain for the treatment of intervertebral disc herniation. The final report of a double-blind study. Spine 9:815–818
Gangi A, Dietemann JL, Ide C, Brunner P, Klinkert A, Warter JM (1996) Percutaneous laser disk decompression under CT and fluoroscopic guidance: indications, technique, and clinical experience. Radiogr Rev Publ Radiol Soc N Am Inc 16:89–96
Grönemeyer DHW, Buschkamp H, Braun M, Schirp S, Weinsheimer PA, Gevargez A (2003) Image-guided percutaneous laser disk decompression for herniated lumbar disks: a 4-year follow-up in 200 patients. J Clin Laser Med Surg 21:131–138
Eichen PM, Achilles N, Konig V, Mosges R, Hellmich M, Himpe B et al (2014) Nucleoplasty, a minimally invasive procedure for disc decompression: a systematic review and meta-analysis of published clinical studies. Pain Physician 17:E149–E173
Revel M, Payan C, Vallee C, Laredo JD, Lassale B, Roux C et al (1993) Automated percutaneous lumbar discectomy versus chemonucleolysis in the treatment of sciatica. A randomized multicenter trial. Spine 18:1–7
Muto M, Andreula C, Leonardi M (2004) Treatment of herniated lumbar disc by intradiscal and intraforaminal oxygen-ozone (O2-O3) injection. J Neuroradiol J Neuroradiol 31:183–189
Gallucci M, Limbucci N, Zugaro L, Barile A, Stavroulis E, Ricci A et al (2007) Sciatica: treatment with intradiscal and intraforaminal injections of steroid and oxygen-ozone versus steroid only. Radiology 242:907–913
Riquelme C, Musacchio M, Mont’Alverne F, Tournade A (2001) Chemonucleolysis of lumbar disc herniation with ethanol. J Neuroradiol J Neuroradiol 28:219–229
Farrar JT (2010) Advances in clinical research methodology for pain clinical trials. Nat Med 16:1284–1293
Tubach F, Ravaud P, Martin-Mola E, Awada H, Bellamy N, Bombardier C et al (2012) Minimum clinically important improvement and patient acceptable symptom state in pain and function in rheumatoid arthritis, ankylosing spondylitis, chronic back pain, hand osteoarthritis, and hip and knee osteoarthritis: results from a prospective multinational study. Arthritis Care Res 64:1699–1707
Tubach F, Dougados M, Falissard B, Baron G, Logeart I, Ravaud P (2006) Feeling good rather than feeling better matters more to patients. Arthritis Rheum 55:526–530
Jensen MC, Brant-Zawadzki MN, Obuchowski N, Modic MT, Malkasian D, Ross JS (1994) Magnetic resonance imaging of the lumbar spine in people without back pain. N Engl J Med 331:69–73
Rose J, Petrover D, Laredo J-D (2011) Infiltrations et Techniques Interventionnelles ostéo-articulaires radioguidées : Infiltrations, Biopsies, Cimentoplasties. Sauramps Médical, Montpellier, 228 p
Theron J, Guimaraens L, Casasco A, Sola T, Cuellar H, Courtheoux P (2007) Percutaneous treatment of lumbar intervertebral disk hernias with radiopaque gelified ethanol: a preliminary study. J Spinal Disord Tech 20:526–532
Stagni S, de Santis F, Cirillo L, Dall’olio M, Princiotta C, Simonetti L et al (2012) A minimally invasive treatment for lumbar disc herniation: DiscoGel(®) chemonucleolysis in patients unresponsive to chemonucleolysis with oxygen-ozone. Interv Neuroradiol J Peritherapeutic Neuroradiol Surg Proced Relat Neurosci 18:97–104
De Sèze M, Saliba L, Mazaux J-M (2013) Percutaneous treatment of sciatica caused by a herniated disc: an exploratory study on the use of gaseous discography and Discogel(®) in 79 patients. Ann Phys Rehabil Med 56:143–154
Bellini M, Romano DG, Leonini S, Grazzini I, Tabano C, Ferrara M et al (2014) Percutaneous injection of radiopaque gelified ethanol for the treatment of lumbar and cervical intervertebral disk herniations: experience and clinical outcome in 80 patients. AJNR Am J Neuroradiol 36(3):600–605
Silverplats K, Lind B, Zoëga B, Halldin K, Rutberg L, Gellerstedt M et al (2010) Clinical factors of importance for outcome after lumbar disc herniation surgery: long-term follow-up. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deform Soc Eur Sect Cerv Spine Res Soc 19:1459–1467
Rihn JA, Hilibrand AS, Radcliff K, Kurd M, Lurie J, Blood E et al (2011) Duration of symptoms resulting from lumbar disc herniation: effect on treatment outcomes: analysis of the Spine Patient Outcomes Research Trial (SPORT). J Bone Joint Surg Am 93:1906–1914
Omidi-Kashani F, Ghayem Hasankhani E, Kachooei AR, Rahimi MD, Khanzadeh R (2014) Does duration of preoperative sciatica impact surgical outcomes in patients with lumbar disc herniation? Neurol Res Int 2014:565189
Peul WC, van den Hout WB, Brand R, Thomeer RTWM, Koes BW, Leiden-The Hague Spine Intervention Prognostic Study Group (2008) Prolonged conservative care versus early surgery in patients with sciatica caused by lumbar disc herniation: two year results of a randomised controlled trial. BMJ 336:1355–1358
Acknowledgements
The scientific guarantor of this publication is: Pr Jean-Denis LAREDO. The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. No complex statistical methods were necessary for this paper. Institutional Review Board approval was obtained. Written informed consent was obtained from all patients in this study. No subjects or cohorts of our study have previously been reported. Methodology and design : prospective, observational, performed at one institution.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Touraine, S., Damiano, J., Tran, O. et al. Cohort study of lumbar percutaneous chemonucleolysis using ethanol gel in sciatica refractory to conservative treatment. Eur Radiol 25, 3390–3397 (2015). https://doi.org/10.1007/s00330-015-3740-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-015-3740-1