Abstract
Lumbar disc herniation is the most common cause of low back pain and sciatica in Western country with classical irradiation along the nerve root course.
Different minimally invasive, well-tolerated, and low-cost procedures have been developed to provide good clinical results without the associated drawbacks of surgery.
Chemiodiscolysis can be realized by two main agents: O2–O3 mixture and radiopaque gelified ethanol (DiscoGel®).
A mixture of ozone and oxygen (O2–O3) can be injected directly in the disc aiming to reduce herniation, relieving nerve root compression, with potential analgesic and anti-inflammatory effects. On the other hand, DiscoGel® has indication in patients with poor therapeutic outcome following O2–O3 therapy.
The best results are reported for small and medium size herniations with a normal spinal canal, without calcifications.
All techniques need a radiological specific support: CT or fluoroscopic guide. A standard technical protocol has not yet been provided, and every operator develops his own technique on the basis of experience and resources availability.
The O2–O3 chemonucleolysis is as effective as other percutaneous disc decompression techniques, which has a high therapeutic success rate (70–80%) with the lowest cost.
Percutaneous techniques do not need a long hospitalization period and they do not exclude the possibility, in case of failed treatment, to undergo surgery afterwards.
Literature data have demonstrated that they play a relevant role in the treatment of low back pain resistant to conservative therapy without motoric deficits.
Surgery is really indicated in emergency cases of cono-cauda syndrome, progressive neurologic deficit, and hyperalgesic sciatica.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Lumbar pain
- Herniated disc
- Oxygen–ozone therapy
- Spine procedures
- Infiltrations
- Lumbar disc herniation
- Chemiodiscolysis
9.1 Introduction
Lumbar disc herniation is the most common cause of low back pain and sciatica in Western country with classical irradiation along the nerve root course. Around 80% of adults suffer from low back pain during a lifetime, and 55% are suffering from back pain associated with radicular syndrome [1].
The natural history of herniated disc at cervical and lumbar level is well-described by several epidemiological study and with MRI correlation [2,3,4,5]. Normally, it is characterized by a disappearance of clinical symptoms in up to 70% with conservative treatment through simple rest for about 6 weeks of patients and shrinkage of the disc herniation revealed by CT or MR scans within 8–9 months after the onset of back pain [6,7,8]. It has also been demonstrated that the mean space-occupying ratio of herniation significantly decrease during 2-year MR follow-up with a progression of degeneration of the intervertebral disc and morphologic changes of lumbar disc herniation [9]. About 88% of patients affected by herniated disc show >50% reduction of the hernia during 3–12 months at MR follow-up after onset, with morphologic changes of the herniated mass well correlated with the clinical outcome [10, 11].
Nowadays, surgery is confined for treatment of patients with progressive neurological deficit, cauda equina syndrome, and severe intolerable pain, which makes it the treatment of choice quite often for extruded, migrated, and free fragment herniated disc.
Therefore, different minimally invasive, well-tolerated, and low-cost procedures have been developed to provide good clinical results without the associated drawbacks of surgery.
Chemiodiscolysis can be realized by two main chemical agents: O2–O3 mixture and radiopaque gelled ethanol (DiscoGel®) [12, 13].
Chemiodiscolysis with O2–O3 mixture with periradicular and periganglionic infiltration is a recent percutaneous technique widespread in Europe; it was first proposed in Italy in the 1980s as a treatment for herniated disc.
Ozone (O3), the triatomic form of oxygen, is a strong oxidant, capable of inducing several useful biological responses and, eventually, reversing chronic oxidative stresses such as those derived from degenerative processes. Ozone (O3) is a strongly oxidant gas with antiseptic, immunomodulating, analgesic, and anti-inflammatory properties.
O3 is administered in the form of O2–O3 at nontoxic concentrations ranging from 1 to 40 mg of O3 per mL of oxygen, using various percutaneous methods.
A mixture of ozone and oxygen (O2–O3) can be injected directly in the disc aiming to reduce herniation, relieving nerve root compression, with potential analgesic and anti-inflammatory effects [12].
On the other hand, DiscoGel® has indication in patients with poor therapeutic outcome following O2–O3 therapy [13, 14].
9.2 Ozone Mechanism of Action
The ozone and oxygen mechanisms of action are currently being investigated and include inhibition of inflammatory inducers and pain-producing mediators in the disease site [15].
Oxygen–ozone inhibits the synthesis and release of prostaglandins, bradykinin, and various algogenic molecules and increases the release of antagonists of proinflammatory cytokines. The effect of ozone on solving or decreasing chemical radiculitis can also explain the clinical effectiveness of intraforaminal O2–O3 injection without intradiscal therapy. Moreover, the direct effect of ozone on the mucopolysaccharides can release the mechanical pressure and compression on the nerves. The effect was confirmed by histologic disc specimens removed during surgical microdiscectomy, previously treated with intradiscal O2–O3 mixture injection, with features of nucleus pulposus fibrillary matrix dehydration and signs of regression [15,16,17,18,19,20,21,22].
On the other side, oxygen–ozone plays significant role in hyper-oxygenation of the area of interest; disc herniation impinges on the venous and arterial flow, causing phlebostasis and arteriolo-stenosis, which lead to hypoxemia of the tissues; by applying O2–O3 mixture in the herniated site and oxygen concentration increases.
O2–O3 mechanism of action has been investigated using three approaches: mathematical models of intervertebral disc space to explore the relationship between disc pressure and volume; ozonolysis experiments using glycosaminoglycans (GAGs) from a Chinese hamster ovary cell line that were similar in composition to GAGs found in human nucleus pulposus; and experiments in which live Yucatan miniature pigs received various concentrations of percutaneous, image-guided intradiscal oxygen–ozone treatment and were examined (after sacrifice) with histology and semiquantitative analysis of disc cytokine concentrations [23].
Porcine disc histology and Chinese hamster ovary GAG ozonolysis results showed that administered ozone reacted with fragmented disc proteoglycans, reducing disc volume through disc dehydration. Cytokine analysis of porcine discs found that each of four cytokines measured (interleukin [IL]-1β, IL-6, IL-8, and tumor necrosis factor α) increased in concentration after 2-week ozone treatment [23].
Finally, ozone stimulates the repair process, promoting the fibroblastic activity and inducing collagen deposition. Experimental studies have demonstrated that a mixture of O2–O3 at concentration used by intradiscal injection produced the same results of steroid on cytokine production and so it reduces pain.
It was evidenced that the mixture of O3–O2 has dose-related effects. At “high” concentrations (40–70 μg O3/O2 mL), it enhances alterations and destruction of tissue structures, at medium concentrations (20–30 μg O3/O2 mL), it appears to affect the regulation of the immune system, and at lower concentrations (<20 μg O3/O2 mL), it improves microcirculation [15, 24].
The administrated dose for treating the disc is 30–40 μm/mL, and it is resulted to be the best concentration to dehydrate the nucleus and to reduce the inflammation, according to experimental studies [23]. A recent study has evaluated the quality of pain alleviation using two different doses of intradiscal injections of O3–O2 mixture of 40 and 30 μg/mL [25]. There were no significant differences between the two groups regarding the clinical outcomes; however, both the ODI and VAS evaluations showed highly significant improvement (decreased) (P < 0.01) after injection and during the entire follow-up period [25].
9.3 The Selection of Patients: Indication and Contraindications
The selection of patients undergoing minimally invasive treatments is the most important factor for the technique’s success and most of all because it is an alternative treatment to classical surgery, already standardized by world guidelines. The following selection criteria are usually adopted for enrolment.
General exclusion criteria are:
-
Extruded herniated disc.
-
Free herniated fragment.
-
Spine infection.
-
High arm and foot progressive motor deficit.
-
Cono-cauda syndrome.
-
Hyperalgesic sciatica.
Last three conditions are absolute indication to surgery.
Among all the techniques illustrated, the oxygen–ozone therapy has the advantage of no absolute contraindications.
The best results are reported for small and medium size herniations with a normal spinal canal, without calcifications. Prognostic factors for an unsuccessful outcome are the presence of a calcified herniated disc, a high grade of spinal stenosis, presence of a small descending herniated disc in the lateral spinal recess, or recurred herniation.
Inclusion criteria are:
-
1.
Clinical criteria: low back pain and sciatica resistant to conservative medical therapy, physical therapy, and others manipulations for a time not shorter than 2–3 months.
-
2.
Neurological criteria: paresthesia or hypoesthesia over the dermatome involved, mild muscle weakness and signs of root-ganglion irritation.
-
3.
Psychological criteria: a firm resolve on the part of the patient to recover with a commitment to cooperate and undergo subsequent physiotherapy with postural and motor rehabilitation.
-
4.
Neuroradiological (CT, MR).
-
(a)
Evidence of small- and medium-sized herniated discs correlating with the patient’s symptoms with or without degenerative disc vertebral disease complicated by intervertebral disc changes (protrusion, herniation).
-
(b)
Residual of surgical (micro)-discectomy with herniation recurrence and/or hypertrophic fibrous scarring.
-
(a)
9.4 Neuroradiological Technique
The choice among any different techniques depends on the confidence of the operator about the technique itself and availability of a good quality machine on the territory. All techniques need a radiological specific support: CT or fluoroscopic guide.
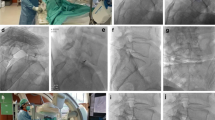
A standard technical protocol has not yet been provided, and every operator develops his own technique on the basis of experience and resources availability. Working in sterile conditions is essential. Fluoro- (Fig. 9.1) or computed tomography (CT) guidance are both feasible depending on the operator choice. The patient lies in a prone position and a pillow can be placed under the abdomen to increase the lumbosacral angle. The approach with the patient lying laterally on the healthy site has been also described.
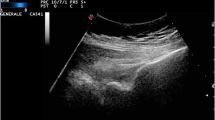
CT guide allows the operator to avoid the intradiscal administration of contrast that even if with low dose reduces the ozone absorption and causes obstruction to the intraforaminal injection of the mixture O2–O3.
Disc access is gained with a posterolateral extra-pedicular approach on the symptomatic side at the level of the disc herniation (Fig. 9.2), even if the puncture site is 6–10 cm away from the vertebral midline, using a 15 cm needle 19–22 G, depending on the patient build, with an angle of about 40–45°. When the needle enters the disc, a soft resistance is felt. The needle position in the centre of the disc must be confirmed by fluoroscopy or CT imaging; the ideal needle position is considered to be at the junction between the posterior and the middle third of the disc. Gas mixture (1–3 mL: 2% O3 (30–40 mg/mL) in 98% O2) is injected into the disc. Then the needle tip is withdrawn into the intervertebral foramen (where the operator feels minor resistance) where another 10 mL of O2–O3 and 2 mL of corticosteroid/local anesthetic (1/1) are injected; indeed the rationale to puncture the symptomatic and not the healthy side when adopting this technique is based on the concept that the effects of the O2–O3 and corticosteroid/local anesthetic mixture are not limited to the disc but affect the intraforaminal nerve root tract as well.
Under CT guidance, the distribution of the O2–O3 in the disc, foraminal-perigangliar, and epidural spaces can be observed. Finally, the needle is removed, and the patient is required to lie in the bed (in a supine position) for 1 h before being dismissed to home. Heavy activity must be avoided for the following two weeks.
If the posterolateral approach at L5–S1 level is unfeasible due to the high position of the iliac crests, a curved steerable needle can be adopted: these devices are able to deflect from a straight rigid direction and the tip can be bent in order to bypass a bone structure. If these devices are not available, a translaminar approach can be considered (Fig. 9.3). In this case, CT guidance is advised because it allows the visualization of the dural sac. The puncture site is 2 cm away from the diseased spinal process in the intervertebral space, and the needle is advanced stepwise into the hernia through the space between the medial border of the articular process and the lateral border of the dural sac; the ideal position of the needle tip is inside the herniated portion of the disc. Before injecting slowly O2–O3 (5–6 mL), an aspiration test is mandatory to make sure that the needle tip is not located in a blood vessel or in the subarachnoidal space, containing cerebrospinal fluid.
Differently from other percutaneous techniques, the infiltration of mixture of O2–O3 can be performed safely at the cervical level with some differences compared to the lumbar level.
The indications are very restricted and selective.
Only the soft herniated disc without calcified element or central spinal stenosis or lateral foraminal stenosis associated can be treated. Symptomatic herniated disc with important motor deficit at upper limb is contraindicated and it is a surgery indication. A pretreatment imaging with CT, MR, and EMG are recommended.
Then for the treatment at cervical level, there are same technical differences: the needle used for cervical level is thinner and smaller than other one used for lumbar level; the procedure is always performed in patient in supine position and it can be done under CT guidance or fluoroscopy; the technique is always performed by right anterolateral approach with carotid-axis manual dislocation; the amount of mixture of O2–O3 is less than lumbar level: only 1–2 cc must be injected into cervical disc; the procedure is never associated with anesthetic drug injection to avoid breathing disturbances; as for lumbar level, a peri-foraminal steroid injection can be associated.
9.5 Complication and Results
The O2–O3 chemonucleolysis is as effective as other percutaneous disc decompression techniques, which has a high therapeutic success rate (70–80%) with the lowest cost (best cost/benefit ratio) and lowest complication rate (<0.1%) [16,17,18,19,20,21,22, 26]. No early or late neurological or infectious complications have been reported following O2–O3 injection [16,17,18,19,20,21,22].
In the literature, there have been reported: bilateral vitreoretinal haemorrhages; thunderclap headache after O2–O3 therapy related to pneumoencephalus as a consequence of inadvertent intrathecal puncture; paresthesias on the anterolateral portion of the left leg and foot, suggesting nerve injury; a few temporary episodes of impaired sensitivity; one case of vertebrobasilar stroke and a subcutaneous haematoma at the puncture site [27].
Regarding infections, a case of L5–S1 discitis and a case of fatal septicaemia have been described. As O2–O3 has disinfecting properties, it is not likely for the gas mixture to be infected; probably these complications were due to inadequate asepsis and iatrogenic inoculation of the bacteria during the injection [27].
In the study of Dall’Olio et al. [24], the pain relief and motor improvement were noted early after 2 weeks. Some researchers studied local ozone injection for low back pain in one group of patients and in one definite dose.
In 2013, Magalhães et al. [28] investigated the epidural injection of ozone upon a single group of 13 sequential adult patients with chronic low lumbar pain after failed back surgery syndrome. The patients had a reduction of low back pain by 43.7% in 6 months followed by 44.0% of improvement in the ODI. Another single group of 30 adult patients with LBP with DH underwent intradiscal injection of O3–O2 mixture (4 mL, 40 μg/mL).
Some studies compared O3–O2 mixtures alone and with additives upon a series of cases of herniated disc. In 2013, some Authors [29] compared the epidural usage of O3–O2 mixture and with steroids added to the same mixture in two groups of 172 patients with disc herniation who failed to respond to conventional therapy and found excellent pain alleviation by nucleolysis in both the groups with insignificant difference. They recommended that the use of O3–O2 could only be sufficient to reduce the disc size and alleviate the pain. They also recommended the use of ozone before recourse to surgical intervention or when surgery is not possible.
A comparison was done by Apuzzo et al. [30] between O3–O2 therapy and global postural reeducation in complicated chronic LBP reeducation or a combination of the two therapeutic options. Follow-up showed that pain severity was lower in the O3–O2 group than in the global postural reeducation alone group. This study denoted that ozone alone can produce a sharp decrease of pain in short term, and the use of global postural education could increase the duration of pain alleviation.
In the appropriate clinical/imaging context, intra-discal injection of O2–O3 has a reported success rate that reaches 90% at short-term follow-up (6 months) and a 75–82% success rate at long-term follow-up (12 months) with no major or minor side effects. Around 73% of the patients who went through O2–O3 therapy are still better at 5 and 10 years [12].
An average reduction in pain intensity in VAS from 7.58 before treatment to 2.64 two years after treatment has been reported, with similar results in ODI classification [12].
Muto et al. [17, 20, 24] reported their experience in three studies published in the course of 10 years enrolling more than 3500 patients and they found an 80% success rate; they used CT guidance and excluded subjects with extruded hernia and free disc fragments; furthermore, they reassessed patient status after 1 month, and those showing only partial success were scheduled for a second treatment session.
Andreula et al. [18] treated 600 patients and compared intradiscal O2–O3 and intradiscal O2–O3 associated with periganglionic injection of corticosteroid and anesthetic: they found success in 70% with intradiscal O2–O3 alone and in 78% with intradiscal O2–O3 and periganglionic injection, concluding that combined intradiscal and periganglionic injection have a cumulative effect enhancing the overall outcome of treatment. Oder et al. [31] reported successful treatment in 620 subjects with reduction of pain measured by means of a VAS score with excellent results in one-third of the patients (reduction from 8 to <3); the better results were encountered in those patients with a single disc herniation <50 years of age.
The study group of Lehnert et al. [32] focused on the physical effects of O2–O3 on the disc volume: they analysed data from 283 treated lumbar disc herniations and concluded that intradiscal administration of medical ozone is associated in 96% of the cases with a statistically significant volume reduction of the herniated lumbar disc. This value correlates negatively with the patient’s age and positively with the initial disc volume; on the other hand, patient’s sex does not affect the volume change after therapy.
Xu et al. [33] treated 187 patients and they followed their cohort up to 4 years with an effective rate of 82%; interestingly they divided this sample into three groups according to the number of O2–O3 sessions (1, 2, or 3), and they did not describe any significant correlation between the injections number and success rate.
Alexandre et al. [34] published a multicentre study reporting follow-up at 5 years on 6665 patients treated in Italy, Spain, and Argentina treated with intradiscal ozone followed by four paravertebral injections, and they reported complete elimination of pain in 80%, improvement in 12% and no improvement in 7%.
Buric et al. [35] reported on 108 patients treated with a single intradiscal injection of O2–O3. They followed up with 107 patients at 5 years and 60 patients at 10 years; They acquired MR imaging at 6 months after the ozone injection that demonstrated a reduction of the disc herniation volume in 79%. During the long-term follow-up, only 19 of 107 patients underwent to surgery while among those that avoided surgery 82% were improved at 5 years and 88% were improved at 10 years. Critically on long-term follow-up, on MR imaging the treated discs stayed hydrated and did not become a low signal. At 6 months MR follow-up, approximately 75–96% of patients had a significant herniation volume reduction, with the higher reduction observed in larger discs. It has been recently reported that the T2 shine-through effect increases already 2 months after O2–O3 nucleolysis, which, in the future, may be used to predict shrinkage of lumbar disc herniation. Furthermore, the high negative predictive value of DWI-ADC analysis could be useful to select those patients who will require further treatment with ozone. Moreover, starting a physical rehabilitation programme is strongly recommended.
Recently, Ezeldin et al. [26] have analyzed 52 patients, with symptomatic herniated lumbar discs, who underwent fluoroscopic-guided intradiscal oxygen–ozone mixture injection (5 mL) at a concentration of 27–30 μg/mL and periradicular injection of the same O2–O3 mixture (10 mL), steroid (1 mL), and local anesthetic (1 mL). Clinical outcomes were evaluated, based on the Oswestry Disability Index (ODI) and pain intensity (0–5) scale results, which were obtained initially and at 2- and 6-month controls. They proved a significant decrease in pain disability and intensity, with a significant reduction in ODI. Negative results were related to long symptoms duration of more than 1 year. No complications were recorded.
9.6 Radiopaque Gelled Ethanol (DiscoGel®)
Radiopaque gelled ethanol (DiscoGel®) is a sterile viscous solution containing ethyl alcohol, cellulose derivative product, added to a radiopaque element, the tungsten, that, injected into the vertebral disc, relieves low back pain, radicular, or lumbar-radicular pain. The 96% pure ethyl alcohol produces a local necrosis of the nucleus pulposus. Its action is mechanical via a dehydration of the turgescent and protruding disc, which is compressing the peripheral nerves of the rachis and causing extreme pain. The product is injected into the nucleus pulposus under radiological control (CT or fluoroscopy guide) with posterolateral approach for thoracic or lumbar level and anterolateral approach for the cervical level [13].
Generally, a small 18-G needle is used for thoracic and lumbar level, while for cervical level it is recommended to use a 20-G needle [13, 14, 36].
Inclusion criteria for DiscoGel® chemonucleolysis are:
-
Lumbago, cruralgia, and sciatica lasting at least 3 months and resistant to conservative management, medication, and physical therapies; sometimes in association with paresthesia.
-
Poor therapeutic outcome following O2–O3 therapy performed at least 6 months before DiscoGel® treatment.
Neuroradiological criteria (CT and/or MR):
-
Imaging findings of one or more small or medium uncalcified disc herniations in a location congruent with symptoms, complicated or not by degenerative disc disease.
Exclusion criteria for treatment with O2–O3 and DiscoGel® were:
-
Neuroradiological evidence of calcified herniation or free disc fragments.
-
Major neurological deficit with impaired lower limber motility congruent with observed disc disease (this criterion is an indication for surgery).
The quantity of jellified ethyl alcohol injected varies between 0.2 and 0.8 mL, according to the dimension of the disc and extent of the hernia.
It is recommended to use:
-
0.2 mL of jellified ethyl alcohol for cervical discs.
-
0.3–0.5 mL of jellified ethyl alcohol for thoracic discs.
-
0.6–0.8 mL of jellified ethyl alcohol for lumbar discs.
At the beginning of the injection, the patient may experience a transitional scalding sensation in the region of injection which disappears in the course of injection. To minimize this risk, the product must be injected very slowly. Once the product has been injected, the needle is left 2 min before being withdrawn.
The viscosity of jellified ethyl alcohol depends on the temperature. Avoid an administration of the product warmed up above room temperature because gel becomes more liquid and is below optimum viscosity. To increase its viscosity, jellified ethyl alcohol can be refrigerated just prior to injection.
It is not indicated for pregnant woman and for patients known to be allergic to one of the components, patients in severe depression, or any other condition making the interpretation of pain difficult.
Experimental study on pigs performed by injecting DiscoGel intradiscal, intraforaminal, epidural and, intramuscular elements demonstrated that the DiscoGel® does not produce any morpho-structural changes in contact with nervous structures or muscular tissue. In fact, no tissue alteration was found but only some inflammatory elements like lympho-monocyte cells and venous stasis with same granular material colored black by hematoxylin and eosin method (the tungsten) in paravertebral tissue in the muscular and connective tissue. The nucleus pulposus, disc, chondro-myxoid, and root ganglion were normal, without morpho-structural changes in nuclear tissue and annulus at contact with DiscoGel [36].
The success rate is achieved between 89% and 91% of cases without any minor or major complications [13, 14, 36].
9.7 Conclusion
Percutaneous techniques, in particular chemodiscolysis, can be a good alternative to surgery treatment for herniated disc for patients affected by low back pain and sciatica.
They have a low rate of complications and easy feasibility. They do not need a long hospitalization period, and they do not exclude the possibility, in case of failed treatment, to undergo surgery afterwards.
Literature data have demonstrated that they play relevant role in the treatment of low back pain resistant to conservative therapy without motoric deficits.
In our experience, among all techniques, chemodiscolysis with O2–O3 mixture with periradicular and periganglionic infiltration is the best and most competitive technique with good therapeutic results and lower costs, also related to cost-benefit ratio and absence of complications.
Surgery is really indicated in emergency cases of cono-cauda syndrome, progressive neurologic deficit and hyperalgesic sciatica.
References
Long MD. Decision making in lumbar disc disease. Clinical Neurosurg. 2001;39:36–51.
Bozzao A, Gallucci M, Masciocchi C, Aprile I, Barile A, Passariello R. Lumbar disk herniation: MR imaging assessment of natural history in patients treated without surgery. Radiology. 1992;185(1):135–41.
Splendiani A, Puglielli E, De Amicis R, Barile A, Masciocchi C, Gallucci M. Spontaneous resolution of lumbar disk herniation: predictive signs for prognostic evaluation. Neuroradiology. 2004;46(11):916–22.
Casey E. Natural history of radiculopathy. Phys Med Rehabil Clin N Am. 2011;22(1):1–5.
Awad JN, Moskovich R. Lumbar disc herniations: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006;443:183–97.
Muto M, De Maria G, Izzo R, Fucci G. Non-discal lumbar radiculopathy: combined approach by CT and MR. Riv Neuroradiol. 1997;10:165–73.
Bush K, Cowan N, Katz DE, Gishen P. The natural history of sciatica associated with disc pathology. A prospective study with clinical and independent radiologic follow-up. Spine. 1992;17(10):1205–12.
Van de Velden J, de Bakker DH. Basis rapport: morbiditeit in de huisartsenpraktijk. Utrecht: Nivel; 1990.
Masui T, Yukawa Y, Nakamura S, Kajino G, Matsubara Y, Kato F, Ishiguro N. Natural history of patients with lumbar disc herniation observed by magnetic resonance imaging for minimum 7 years. J Spinal Disord Tech. 2005;18(2):121–6.
Takada E, Takahashi M, Shimada K. Natural history of lumbar disc hernia with radicular leg pain: spontaneous MRI changes of the herniated mass and correlation with clinical outcome. J Orthop Surg. 2001;9(1):1–7.
Singh V, Piryani C, Liao K. Percutaneous disc decompression using coblation in the treatment of chronic discogenic pain. Pain Phys. 2002;5:250–9.
Giurazza F, Guarnieri G, Murphy KJ, Muto M. Intradiscal O2O3: rationale, injection technique, short- and long-term outcomes for the treatment of low back pain due to disc herniation. Can Assoc Radiol J. 2017;68(2):171–7.
Guarnieri G, De Dominicis G, Muto M. Intradiscal and intramuscular injection of Discogel(®)—radiopaque gelified ethanol: pathological evaluation. Neuroradiol J. 2010;23(2):249–52.
Stagni S, Simonetti L, Stafa A, Leonardi M, et al. A minimally invasive treatment for lumbar disc herniation: DiscoGel® chemonucleolysis in patients unresponsive to chemonucleolysis with oxygen-ozone. Interv Neuroradiol. 2012;18(1):97–104.
Chang JD, Lu HS, Chang YF, Wang D. Ameliorative effect on ozone on cytokine production in mice injected with human rheumatoid arthritis synovial fibroblast cells. Rheumatol Int. 2005;26:141–51.
Andreula C, Muto M, Leonardi M. Interventional spinal procedures. Eur J Radiol. 2004;50:112–9.
Muto M, Andreula C, Leonardi M. Treatment of herniated lumbar disc by intradiscal and intraforaminal oxygen-ozone injection. J Neuroradiol. 2004;31(3):183–9.
Andreula CF, Simonetti L, Leonardi M. Minimally invasive oxygen-ozone therapy for lumbar disk herniation. AJNR. 2003;24:996–1000.
Tian JL, et al. Changes of CSF and spinal path-morphology after hight concentration ozone injection into the subarachnoid space:an experimental study in pigs. AJNR. 2007;28:1051–4.
Muto M, Avella F. Percutaneous treatment of herniated lumbar disc by intradiscal oxygen-ozone injection. Interv Neuroradiol. 1998;4(4):279–86.
Muto M, Guarnieri G, et al. Low back pain and sciatica: treatment with intradiscal-intraforaminal O(2)-O (3) injection. Our experience. Radiol Med. 2008;113(5):695–706.
Bonetti M, Cotticelli B, et al. Oxygen-ozone therapy versus epidural steroid injection. Riv Neuroradiol. 2000;13:203–6.
Murphy K, Elias G, Steppan J, Boxley C, Balagurunathan K, Victor X, Meaders T, Muto M. Percutaneous treatment of herniated lumbar discs with ozone: investigation of the mechanisms of action. J Vasc Interv Radiol. 2016;27(8):1242–1250.e3.
Dall’Olio M, Princiotta C, Cirillo L, Budai C, de Santis F, Bartolini S, Serchi E, Leonardi M. Oxygen-ozone therapy for herniated lumbar disc in patients with subacute partial motor weakness due to nerve root compression. Interv Neuroradiol. 2014;20:547–54.
Elawamy A, Kamel EZ, Hassanien M, Wahba OM, Amin SE. Implication of two different doses of intradiscal ozone-oxygen injection upon the pain alleviation in patients with low back pain: a randomized, single-blind study. Pain Physician. 2018;21(1):E25–31.
Ezeldin M, Leonardi M, Princiotta C, Dall'olio M, Tharwat M, Zaki M, Abdel-Wanis ME, Cirillo L. Percutaneous ozone nucleolysis for lumbar disc herniation. Neuroradiology. 2018;60(11):1231–41. https://doi.org/10.1007/s0O234-018-2083-4.
De Oliveira MF, Dotta L, Sasse A, et al. Ozone therapy as a treatment for low back pain secondary to herniated disc: a systematic review and meta-analysis of randomized controlled trials. Pain Physician. 2012;15:E115–29.
Magalhães FN, Soares SC, Torres JM, Ungaretti A, Cacciacarro MF, Teixeira MJ, Fonoff ET. Effects of ozone applied by spinal endoscopy in patients with chronic pain related to failed back surgery syndrome: a pilot study. Neuropsychiatr Dis Treat. 2013;9:1759–66.
Zhang Y, Ma Y, Jiang J, Ding T, Wang J. Treatment of the lumbar disc herniation with intradiscal and intraforaminal injection of oxygen-ozone. J Back Musculoskelet Rehabil. 2013;26:317–22.
Apuzzo D, Giotti C, Pasqualetti P, Ferrazza P, Soldati P, Zucco GM. An observational retrospective/horizontal study to compare oxygen-ozone therapy and/ or global postural re-education in complicated chronic low back pain. Funct Neurol. 2014;29:31–9.
Oder B, Loewe M, Reisegger M, Lang W, Ilias W, Thurnher SA. CT-guided ozone/steroid therapy for the treatment of degenerative spinal disease: effect of age, gender, disc pathology and multi-segmental changes. Neuroradiology. 2008;50:777e85.
Lehnert T, Naguib N, Wutzler S, et al. Analysis of disk volume before and after CT-guided intradiscal and periganglionic ozoneeoxygen injection for the treatment of lumbar disk herniation. J Vasc Interv Radiol. 2012;23:1430e6.
Xu L, Li ZL, He XF, et al. Evaluation of the clinical curative effect of an O2-O3 mixture to treat lumbar disc herniation with different treat- ment sessions. Interv Neuroradiol. 2009;15:159e63.
Alexandre A, Buric J, Paradiso R, et al. Intradiscal injection of O2-O3 to treat lumbar disc herniations. Results at five years. Riv Ital Ossigeno Ozonoterapia. 2002;1:165e9.
Buric J, Rigobello L, Hooper D. Five and ten year follow-up on intradiscal ozone injection for disc herniation. Int J Spine Surg. 2014;8:17.
Theron J, Guimaraens L, Casasco A, Sola T, Cuellar H, Courtheoux P. Percutaneous treatment of lumbar intervertebral disk hernias with radiopaque gelified ethanol: a preliminary study. J Spinal Disord Tech. 2007;20:526–32.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Leone, G., Muto, M., Guarnieri, G., Gatta, L.D., Bonetti, M., Muto, M. (2020). Minimally Invasive Treatment of Herniated Disc: How to Remove the Disc with Chemical Tools. In: Manfrè, L., Van Goethem, J. (eds) The Disc and Degenerative Disc Disease. New Procedures in Spinal Interventional Neuroradiology. Springer, Cham. https://doi.org/10.1007/978-3-030-03715-4_9
Download citation
DOI: https://doi.org/10.1007/978-3-030-03715-4_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-03714-7
Online ISBN: 978-3-030-03715-4
eBook Packages: MedicineMedicine (R0)