Abstract
Objectives
To evaluate the diagnostic accuracy of transluminal attenuation gradient (TAG) for stenosis severity of calcified lesions assessed by coronary computed tomography angiography (CCTA).
Methods
One hundred seven patients who underwent CCTA and coronary angiography (CAG) were enrolled. TAGs of 309 major epicardial coronary arteries were measured. The impact of plaque composition, Agatston scores, and lesion length ratio on TAG were analyzed. Diagnostic performance vs. CAG of TAG, CCTA, and combined TAG/CCTA were evaluated, and incremental value of TAG for reclassification of CCTA stenosis severity in calcified lesions was also analyzed.
Results
TAG decreased consistently with stenosis severity. TAG was significantly lower in coronary arteries with calcification scores >300 and lesion length ratios >2/3. TAG improved diagnostic accuracy of CCTA (c-statistic =0.982 vs. 0.942, P = 0.0001) in calcified lesions, and the sensitivity, specificity, positive, and negative predictive values of TAG cutoff ≤ −11.33 were 72 %, 91 %, 88 %, and 78 %, respectively. The addition of TAG to CCTA resulted in significant reclassification (NRI =0.093, P = 0.022) in calcified vessels.
Conclusions
Measurement of TAG may improve diagnostic performance and reclassification of CCTA in coronary stenosis caused by calcified lesions.
Key Points
• TAG decreased as calcification scores and lesion length increased.
• TAG markedly improved the diagnostic performance of CCTA for calcified lesions.
• TAG improved reclassification of coronary artery stenosis severity in CCTA.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Multislice computed tomography (MSCT) has been proven to be a valuable tool in noninvasive coronary imaging, with high sensitivity and negative predictive value for coronary artery disease [1–3]. However, the evaluation of stenosis is often hampered by the occurrence of “blooming” artefacts as a result of calcification. These artefacts can cause an apparent enlargement of the calcified plaque and preclude visual observation of the intraluminal stenosis. Hence, coronary arterial calcification, especially severe calcification, would significantly influence the diagnostic performance of coronary computed tomography angiography (CCTA) [4–6]. The false-positive results have been observed primarily in highly calcified segments due to partial volume effects, leading to an overestimation of stenosis severity [7, 8].
Quantification of transluminal attenuation gradient (TAG), defined as the linear regression coefficient between luminal contrast opacification and distance from the coronary ostium, reflects the rate of fall-off of contrast opacification along a vessel, and thus has the potential to indirectly estimate coronary blood flow [9]. Initial work [10] has demonstrated that plots of TAG values are generally linear, and that TAG falls off more rapidly in the presence of a significant stenosis than in the absence of stenosis. A study from Choi et al. [11] validated that adding TAG to CCTA improved diagnostic accuracy, especially in vessels with calcified lesions. The addition of TAG also resulted in reclassification from one class of stenosis severity to another in coronary arteries with calcified lesions, but did not result in significant stenosis severity reclassification in coronary arteries with noncalcified lesions. In this regard, this technique may be of special use for estimating flow across non-evaluable coronary segments such as severe calcification or stents, and may improve the diagnostic accuracy of CCTA. There has no subsequent study, however, to further validate the added values of TAG for CCTA diagnostic performance and stenosis severity reclassification in severely calcified coronary arteries compared with coronary angiography (CAG), although some studies [12–14] have validated the diagnostic accuracy of TAG in predicting functional stenosis severity evaluated by fractional flow reserve (FFR).
Hence, the potential of TAG for improving diagnostic performance and reclassification in CCTA for calcified lesions must be further validated. In addition, some details such as the impact of plaque composition, Agatston score, and lesion length ratio on TAG have never been evaluated. Previous clinical studies in TAG have generally used 64- and 320-detector-row CT, and thus far, the assessment of TAG on dual-source CT has not been reported. The primary aim of this study was to determine the diagnostic performance of TAG and the CCTA/TAG combination using dual-source CT (DSCT) for the evaluation of calcified stenosis severity in patients undergoing invasive coronary angiography (CAG).
Materials and methods
Study population
One hundred seven consecutive patients with suspected or known coronary artery disease were prospectively screened for analysis. All patients underwent CCTA and diagnostic CAG within 30 days. Patients with arrhythmia (auricular fibrillation, atrial flutter, or recurrent atrial or ventricular premature beat), renal insufficiency (serum creatinine level greater than 1.5 mg/dl), a history of allergic reaction to contrast medium, a history of surgery or stenting for coronary artery disease, heart failure, or congenital heart disease were not included. The institutional review board committee approved the study protocol, and all patients provided written informed consent.
CT image acquisition and reconstruction
ECG-triggered spiral acquisition of CCTA was retrospectively performed on a second-generation 128-slice DSCT system (Somatom Definition Flash, Siemens Healthcare, Forchheim, Germany). Oral metoprolol was administered for patients with a heart rate >65 beats/min. Every patient received a sublingual dose of isosorbide dinitrate 2.5 mg (Isoket; Schwarz Pharma, Monheim, Germany) two minutes before imaging.
Non-enhanced imaging for calcium scoring was performed from 1 cm below the level of the tracheal bifurcation to the diaphragm in a craniocaudal direction using the following scanning parameters: detector collimation 64 × 0.6 mm; slice acquisition 128 × 0.6 mm, by means of a z-flying focal spot; gantry rotation time 0.28 s; pitch of 0.2–0.5, adapted to the heart rate; reference tube current 80 mAs per rotation; and tube potential 120 kV.
The CCTA imaging parameters were as follows: pitch of 0.2–0.5, adapted to the heart rate; collimation 2 × 64 × 0.6 mm; slice collimation 2 × 128 × 0.6 mm, by means of z-flying focal spot; tube voltage 100 kV; reference tube current 300 mAs, with automatic tube current modulation; gantry rotation time 0.28 s; and image acquisition range from 2 cm below the bifurcation of trachea to the diaphragm. Full tube current was applied from 65 % to 77 % of the R–R interval. Tube current was reduced to 4 % of full tube current outside the pulsing window.
An intravenous bolus of 1 ml/kg iopromide 370 (370 mg/ml, Ultravist 370, Bayer Schering Pharma, Berlin, Germany) was injected at a flow rate of 5 ml/s, followed by 40 ml saline solution. Contrast agent application was controlled by bolus tracking. The region of interest (ROI) was placed into the aortic root, and image acquisition started 5 s after the signal attenuation reached a predefined threshold of 100 Hounsfield units (HU).
For calcium scoring, non-overlapping images with a slice width of 3 mm were reconstructed using a medium-sharp convolution kernel (B35f). All CCTA images were reconstructed using a conventional FBP (filtered back-projection) algorithm with a medium-smooth kernel designed for cardiac imaging (B26f), and an edge-enhancing tissue convolution kernel for imaging of severely calcified coronary arteries (B46f). All images were reconstructed with a slice thickness of 0.75 mm and increment of 0.5 mm. All images were transferred to an external workstation (syngo MMWP VE 36A, Siemens Healthcare, Forchheim, Germany) for further evaluation.
Invasive coronary angiography
The maximal diameter stenosis in each major epicardial coronary artery was evaluated using quantitative CAG (AXIOM Artis dBA, Siemens Healthcare, Forchheim, Germany). This semi-automatic evaluation was performed by an experienced cardiologist (Li J.), who was blinded to TAG and CCTA findings.
CT image analysis
The mean Agatston score was calculated for each major coronary artery from the non-enhanced DSCT images, with a detection threshold of 130 HU, using semi-automated software (syngo Calcium Scoring, Siemens Healthcare, Forchheim, Germany).
For CCTA analysis, all images were interpreted by three cardiovascular radiologists who were blinded to clinical and invasive CAG results. Each coronary artery tree was divided into 18 segments [15]. Plaque composition was classified as noncalcified (<30 % calcified plaque volume), partially calcified (30 % to 70 %), or calcified (>70 %), according to the volume of calcific component (>130 HU) in the plaque. For convenience of analysis, partially calcified and calcified plaques were all treated as calcified plaques. Vessels were classified as noncalcified lesions if the most stenotic portion was noncalcified, and as calcified lesions if the most stenotic portion was calcified or partially calcified.
The severity of luminal stenosis was classified and expressed on an ordinal scale as mild (0 % to 49 %), moderate (50 % to 69 %), severe (70 % to 99 %), or total occlusion (100 %). For the analysis of maximum stenosis in each vessel, no stenosis to mild stenosis was considered as a single category.
The length of the lesion and all involved vessels were measured. The length of the coronary artery with complete absence of detectable luminal enhancement was determined, and the lesion length ratio (LLR) was calculated by dividing the lesion length by the coronary artery length. The LLR was used as an estimate for involving extent.
Attenuation values measurement and TAG calculation
Cross-sectional images perpendicular to the vessel centreline were reconstructed for each major coronary artery, and manually corrected if necessary. The mean luminal attenuation (HU) was measured at 5-mm intervals, from the ostium to the distal level where the vessel cross-sectional area fell below 2.0 mm2 [11]. The ROI contour was positioned in the centre of the cross-sectional images, and the contour of the ROI was manually corrected if necessary. For reproducibility and agreement of measurement, three cardiovascular radiologists measured CT values in the same vessels six times in total (each one measured twice), and then the mean CT values of the six measurements in each vessel were recorded and used for TAG calculation. TAG was determined from the change in HU per 10-mm length of coronary artery, and defined as the linear regression coefficient between intraluminal attenuation (HU) and length from the ostium (mm). Representative examples are shown in Figs. 1 and 2.
An example of luminal attenuation measurement and TAG performance in coronary artery with mild stenosis. (A) Left circumflex artery with mild stenosis imaged by CAG. (B) Left circumflex artery with mild stenosis imaged by CCTA. (C–G) Curved planar reformation image and representative cross-sectional views with corresponding luminal attenuation (HU) of CCTA. (H) TAG was shown as -8.98 HU/10 mm. Black dots represent 5-mm intervals at which intraluminal attenuation (HU) was measured. TAG: transluminal attenuation gradient; CAG: coronary angiography; CCTA: coronary computed tomography angiography; HU: Hounsfield unit
An example of luminal attenuation measurement and TAG performance in coronary artery with severe stenosis. (A) Right coronary artery with severe stenosis imaged by CAG. (B) Right coronary artery with severe stenosis imaged by CCTA. (C–G) Curved planar reformation image and representative cross-sectional views with corresponding luminal attenuation (HU) of CCTA. (H) TAG was shown as -25.84 HU/10 mm. Black dots represent 5-mm intervals at which intraluminal attenuation (HU) was measured. TAG: transluminal attenuation gradient; CAG: coronary angiography; CCTA: coronary computed tomography angiography; HU: Hounsfield unit.
Impacts of plaque composition, Agatston score, and lesion length on TAG were analyzed. The diagnostic accuracy of TAG, CCTA, and the TAG/CCTA combination were compared with CAG on a per-vessel basis. The incremental value of TAG for reclassification of CCTA stenosis severity in calcified lesions was also analyzed.
Statistical analysis
All analyses were performed on a per-vessel basis, and no adjustments were made for multiple vessels or segments within individuals. Continuous variables were expressed as mean ± standard deviation (SD), whereas categorical variables were expressed as frequencies and percentages. Correlations between two continuous variables and continuous and categorical variables were tested using the Pearson correlation coefficient. Receiver operating characteristics (ROC) curve analysis was used to assess the diagnostic performance of CCTA, TAG, and the CCTA/TAG combination for detection of stenosis severity. The area under the ROC curve (AUC) was calculated, and AUCs were compared using the DeLong method and net reclassification improvement index [16]. The optimal cutoff of measured variables was determined by values with the highest Youden’s J statistics. With an optimal cutoff value, the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) were calculated on a per-vessel basis and expressed with a corresponding 95 % confidence interval. P < 0.05 was considered statistically significance.
All statistical analyses were performed using SPSS 17.0 (SPSS, Inc., Chicago, IL, USA) and MedCalc version 12.3.0.0 (MedCalc Software, Mariakerke, Belgium).
Results
Clinical characteristics
The CCTA studies from 111 patients with invasive coronary angiography were screened for evaluation. Four patients (3.5 %, 4/111) with CCTA images that were determined to be non-evaluable for TAG were excluded. Twelve coronary arteries (3.7 %, 12/321) with a diameter of less than 1.5 mm were also excluded. A total of 107 patients and 309 coronary arteries were enrolled for the final analysis. The clinical characteristics of the study population are summarized in Table 1.
TAG and CCTA in relation to luminal stenosis severity by CAG
TAG decreased progressively as CAG-determined stenosis severity increased, from −6.10 ± 6.97 HU/10 mm for stenosis <50 % to −20.45 ± 13.69 HU/10 mm for stenosis of 70 % to 99 % (P = 0.002). This tendency was similar in calcified vessels. However, the TAG for total-occlusion lesions (stenosis 100 %) was −17.96 ± 20.36 HU/10 mm, which was not lower than that for stenosis of 70 % to 99 %. TAG performance in different levels of stenosis severity is shown in Table 2. The stenosis severity determined by CCTA was positively correlated to that as determined by CAG.
Impact of plaque composition, Agatston score, and lesion length ratio on TAG
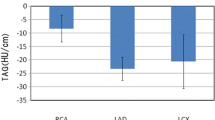
To facilitate analysis, partially calcified plaques (n = 57) and calcified plaques (n = 56) were considered as a single group, for a total of 113 (36.6 %) calcified lesions and 196 (63.4 %) noncalcified lesions among 309 coronary arteries. There was no significant difference in TAG between noncalcified plaques and calcified plaques in the total number of plaques or level of stenosis severity defined by CAG (P > 0.05 for all comparisons) (Table 3). In calcified lesions, TAG decreased progressively as Agatston scores increased, from −13.93 ± 14.84 HU/10 mm for scores of <100, to −28.64 ± 18.26 HU/10 mm for scores >300 (P = 0.000), although there was no significant difference in TAG between scores of <100 and scores of 100 to 300 (−13.93 ± 14.84 vs. −17.25 ± 13.91, P = 0.198) (Table 4, Fig. 3). TAG also decreased as lesion length ratio (LLR) increased, from −10.90 ± 10.19 HU/10 mm for LLR of <1/3 to −32.61 ± 16.64 HU/10 mm for LLR of 1/2 to 2/3 ( P = 0.000) (Table 4, Fig. 4). However, the TAG for LLR of >2/3 was −14.51 ± 10.58 HU/10 mm, which was not lower than that for LLR 1/2 to 2/3.
TAG performance in different Agatston scores grades. There was a significant difference of TAG between Agatston score 100–300 and Agatston score >300 (P = 0.004) or Agatston score <100 and Agatston score >300 (P = 0.000), respectively, but no significant difference of TAG between Agatston score <100 and Agatston score 100-300 (P = 0.198). TAG: transluminal attenuation gradient.
TAG performance in different lesion length ratios (LLR). There were significant differences of TAG among LLR <1/3, LLR 1/3-1/2 and LLR 1/2-2/3 (P < 0.05 for all comparisons). Other statistical comparisons are listed in Table 4. TAG: transluminal attenuation gradient.
Accuracy of CCTA in calcified lesions compared to CAG
The diagnostic performance of CCTA, TAG, and TAG + CCTA in total (Fig. 5A) and calcified vessels (Fig. 5B) was analyzed on a vessel basis and is shown in Table 5. CCTA showed relative high sensitivity [95 %; 95 % confidence interval (CI) =90–99 %] and moderate specificity (78 %; 95 % CI =70–84 %), while TAG showed moderate sensitivity (73 %; 95 % CI =66–80 %) and high specificity (92 %; 95 % CI =87–96 %). Adding TAG to CCTA significantly augmented the overall diagnostic performance of CCTA, especially in improved specificity. In calcified vessels, CCTA showed moderate sensitivity [70 %; 95 % CI =57–82 %] and low specificity (66 %; 95 % CI =54–76 %), while TAG showed moderate sensitivity (72 %; 95 % CI =64–79 %) and high specificity (91 %; 95 % CI =86–95 %). The addition of TAG to the CCTA markedly improved the diagnostic performance of CCTA for calcified lesions (Fig. 6), and resulted in increased sensitivity (84 %; 95 % CI =72–92 %) and specificity (89 %; 95 % CI =77–96 %).
Predicted probability of TAG in addition to CCTA stenosis severity. (A) Predicted probability of TAG in addition to CCTA stenosis severity in total relevant vessels on a reference of results from CAG. (B) Predicted probability of TAG in calcified vessels in addition to CCTA stenosis severity on a reference of results from CAG. Area under the ROC curve is shown as mean ± SD. (See Table 5 for details). TAG: transluminal attenuation gradient; CAG: coronary angiography; CCTA: coronary computed tomography angiography.
CCTA, TAG, and CAG diagnostic performance in a 56-year-old man with suspected coronary artery disease (mean heart rate during imaging 77 bpm, Agatston score 536). (A) CCTA curved planar reformation image showed calcified plaque (arrow) in the proximal segment of left anterior descending artery, and the assessment of stenosis severity was difficult because of the cover of lumen by calcified plaque. A moderate stenosis was determined by three cardiovascular radiologists. (C) TAG showed a value of -6.787 HU/10 mm and predicted a mild stenosis. Combined with TAG and CCTA, the final diagnosis of stenosis severity was mild stenosis. (B) CAG validated a mild stenosis in the proximal segment of left anterior descending artery (arrow).
Adding TAG to CCTA resulted in reclassification from one class of stenosis severity to another in a large number of vessels with calcified lesions (net reclassification improvement [NRI] 0.093, net proportion of patients reclassified 5.31 %; P = 0.022). However, addition of TAG to CCTA did not result in significant stenosis severity reclassification among total vessels (NRI 0.009; P = 0.09).
Discussion
The results of this study confirmed that the addition of TAG to CCTA improved the diagnostic accuracy of CCTA. TAG showed high specificity and positive predictive value, and adding TAG to CCTA resulted in improved diagnostic accuracy of CCTA as well. Particularly in calcified lesions, the sensitivity, specificity, positive predictive value, and negative predictive value of CCTA significantly increased when TAG was taken into account.
This study firstly validated the potential impact of Agatston scores and lesion length ratios on TAG. TAG significantly decreased as Agatston scores increased, from −13.93 ± 14.84 HU/10 mm for scores of <100, to −28.64 ± 18.26 HU/10 mm for scores of >300 (P = 0.000). TAG also decreased as LLR increased, from −10.75 ± 10.14 HU/10 mm for LLR of <1/3, to −32.61 ± 16.64 HU/10 mm for LLR of 1/2 to 2/3 (P = 0.000). However, the TAG values for LLR of >2/3 were not progressively lower than for LLR of 1/2 to 2/3. This may have been due to the inconsistencies in measurements of CT attenuation values in vessels with extensive lesions, and some vessels with LLR of >2/3 were total-occlusion vessels (28.6 %, 8/28) with collateral blood supply. The study also confirmed that there was no significant difference in TAG between noncalcified plaque and calcified plaque in the total number of plaques or in different levels of stenosis severity (P >0.05 for all comparisons). Results from this study may contribute to improving diagnostic confidence in CCTA for calcified lesions that make visual estimation difficult. It should be noted that it took only approximately five minutes of additional analysis time for manually measuring ROIs and calculating TAG for each patient in this study. Therefore, this methodology may be feasible in daily clinical routine.
The results from this study demonstrated that TAG decreased consistently with maximum stenosis severity, in line with the results from two other studies [9, 10]. However, the TAG for total-occlusion lesions was not the lowest in all stenosis categories, and was slightly different from previous descriptions [11]. This may be due to distal retrograde flow derived from collateral circulation after chronic total occlusion [17], which could result in an increased attenuation gradient at the distal segment of total-occlusion vessels.
The results of this study revealed that there was no significant difference in TAG between noncalcified plaque and calcified plaque. These findings are consistent with those in CCTA and CAG; there were no significant differences in stenosis severity between noncalcified and calcified plaques in this cohort. However, TAG decreased consistently as Agatston coronary artery calcification score and lesion length increased. These results can be explained as follows. The calcification score is specifically related to atherosclerosis, and its extent is a good marker of the total burden of coronary atherosclerosis [18]. In a previous study [19], the total coronary calcification score was related to coronary stenosis. For a complex calcified lesion, where it is difficult to visually estimate stenosis severity, the decreased trend of TAG with calcification score may result in reclassification from one class of stenosis severity to another. Our results also suggest that the decreased tendency of TAG in parallel with increased lesion length may contribute to improve diagnostic confidence with regard to stenosis severity, as it provides relevant predictive information even though it is only a visual scale.
It is widely recognized that a reliable assessment of stenosis severity can be challenging in heavily calcified or complex coronary artery lesions. Moreover, an anatomic measure of stenosis is not a good predictor of functionally significance. The high sensitivity and negative predictive value of CCTA have been validated in prospective multicentre studies [20], but specificity and positive predictive value still have much room for improvement [21]. Increased specificity and a positive predictive value of CCTA could be critical for guiding or triggering revascularization or other treatment strategies [22, 23]. The diagnostic value of coronary stenosis severity assessed by TAG over anatomic stenosis evaluation by CCTA was demonstrated in a previous study [11]. The results from the present study provide further validation and detail.
For reclassification of coronary artery stenosis severity, however, the results were discrepant. Choi et al. [11] found that TAG contributed to improved classification of coronary artery stenosis severity, particularly in severely calcified lesions. The results from another study [13], however, demonstrated that the addition of TAG to CCTA did not result in significant reclassification. The disparity between results in these two studies may be due to different reference standards, namely invasive CAG and fractional flow reserve (FFR), respectively. In the present study, with CAG as reference standard, although there was no improvement in total reclassification of coronary artery stenosis severity, TAG did improve the reclassification of calcified coronary artery stenosis severity. These results also conflict with those of a previous study [11]. A possible explanation might be that the frequency of calcified lesions (36.6 %, 113/309) in this study was higher than in the previous study (32 %, 117/370). In addition, different imaging systems may also influence the results of the measurement of TAG [12].
There were several limitations to our study. The first is the generally limiting nature of a single-centre study. The results from this study represent a prospective experience involving 309 vessels in 107 patients, and thus require confirmation involving larger multicentre studies. Second, in this study, TAG was measured in major epicardial vessels derived from attenuation values taken at points of the artery with cross-sectional areas of <2.0 mm2. The values at smaller luminal sizes or in main branches were not measured and thus are unknown. Third, the use of dual-source CT with retrospectively ECG-triggered acquisition is limited by its inherent longitudinal axis coverage of 3.8 cm, and may not allow the entire heart volume to be imaged in a single heartbeat. Therefore, the value of TAG may be non-flat in nature. Finally, the TAG cutoff value from this study using dual-source CT may not be generalizable for studies performed on other MDCT systems with different imaging techniques, as value may differ.
Abbreviations
- AUC:
-
Area under the ROC curve
- CAG:
-
Coronary angiography
- CCTA:
-
Coronary computed tomography angiography
- CI:
-
Confidence interval
- DSCT:
-
Dual-source CT
- FBP:
-
Filtered back-projection
- FFR:
-
Fractional flow reserve
- HU:
-
Hounsfield units
- LLR:
-
Lesion length ratio
- MSCT:
-
Multislice computed tomography
- NPV:
-
Negative predictive value
- NRI:
-
Net reclassification improvement
- PPV:
-
Positive predictive value
- ROC:
-
Receiver-operating characteristics
- ROI:
-
Region of interest
- TAG:
-
Transluminal attenuation gradient
References
Cademartiri F, Runza G, Marano R et al (2005) Diagnostic accuracy of 16-row multislice CT angiography in the evaluation of coronary segments. Radiol Med 109:91–97
Leschka S, Alkadhi H, Plass A et al (2005) Accuracy of MSCT coronary angiography with 64-slice technology: first experience. Eur Heart J 26:1482–1487
Achenbach S, Ropers D, Kuettner A et al (2006) Contrast-enhanced coronary artery visualization by dual-source computed tomography–initial experience. Eur J Radiol 57:331–335
Budoff MJ, Dowe D, Jollis JG et al (2008) Diagnostic performance of 64-multidetector row coronary computed tomographic angiography for evaluation of coronary artery stenosis in individuals without known coronary artery disease: results from the prospective multicenter ACCURACY (Assessment by Coronary Computed Tomographic Angiography of Individuals Undergoing Invasive Coronary Angiography) trial. J Am Coll Cardiol 52:1724–1732
Pundziute G, Schuijf JD, Jukema JW et al (2007) Impact of coronary calcium score on diagnostic accuracy of multislice computed tomography coronary angiography for detection of coronary artery disease. J Nucl Cardiol 14:36–43
Ong TK, Chin SP, Liew CK et al (2006) Accuracy of 64-row multidetector computed tomography in detecting coronary artery disease in 134 symptomatic patients: influence of calcification. Am Heart J 151:1323.e1–6
Burgstahler C, Reimann A, Drosch T et al (2007) Cardiac dual-source computed tomography in patients with severe coronary calcifications and a high prevalence of coronary artery disease. J Cardiovasc Comput Tomogr 1:143–151
Mollet NR, Cademartiri F, van Mieghem CA et al (2005) High-resolution spiral computed tomography coronary angiography in patients referred for diagnostic conventional coronary angiography. Circulation 112:2318–2323
Lackner K, Bovenschulte H, Stutzer H et al (2010) In vitro measurements of flow using multislice computed tomography (MSCT). Int J Cardiovasc Imaging 27:795–804
Steigner ML, Mitsouras D, Whitmore AG et al (2010) Iodinated contrast opacification gradients in normal coronary arteries imaged with prospectively ECG-gated single heart beat 320-detector row computed tomography. Circ Cardiovasc Imaging 3:179–186
Choi JH, Min JK, Labounty TM et al (2011) Intracoronary transluminal attenuation gradient in coronary CT angiography for determining coronary artery stenosis. JACC Cardiovasc Imaging 4:1149–1157
Wong DT, Ko BS, Cameron JD et al (2013) Transluminal attenuation gradient in coronary computed tomography angiography is a novel noninvasive approach to the identification of functionally significant coronary artery stenosis: a comparison with fractional flow reserve. J Am Coll Cardiol 61:1271–1279
Choi JH, Koo BK, Yoon YE et al (2012) Diagnostic performance of intracoronary gradient-based methods by coronary computed tomography angiography for the evaluation of physiologically significant coronary artery stenoses: a validation study with fractional flow reserve. Eur Heart J Cardiovasc Imaging 13:1001–1007
Yoon YE, Choi JH, Kim JH et al (2012) Noninvasive diagnosis of ischemia-causing coronary stenosis using CT angiography: diagnostic value of transluminal attenuation gradient and fractional flow reserve computed from coronary CT angiography compared to invasively measured fractional flow reserve. JACC Cardiovasc Imaging 5:1088–1096
Raff GL, Abidov A, Achenbach S et al (2009) SCCT guidelines for the interpretation and reporting of coronary computed tomographic angiography. J Cardiovasc Comput Tomogr 3:122–136
Pencina MJ, D’Agostino RB Sr, D’Agostino RB Jr et al (2008) Evaluating the added predictive ability of a new marker: from area under the ROC curve to reclassification and beyond. Stat Med 27:157–172, discussion 207–212
Li M, Zhang J, Pan J et al (2013) Obstructive coronary artery disease: reverse attenuation gradient sign at CT indicates distal retrograde flow: a useful sign for differentiating chronic total occlusion from subtotal occlusion. Radiology 266:766–772
Rumberger JA, Simons DB, Fitzpatrick LA et al (1995) Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area: a histopathologic correlative study. Circulation 92:2157–2162
Kajinami K, Seki H, Takekoshi N et al (1995) Noninvasive prediction of coronary atherosclerosis by quantification of coronary artery calcification using electron beam computed tomography: comparison with electrocardiographic and thallium exercise stress test results. J Am Coll Cardiol 26:1209–1221
Tonino PA, De Bruyne B, Pijls NH et al (2009) Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 360:213–224
Hulten EA, Carbonaro S, Petrillo SP et al (2011) Prognostic value of cardiac computed tomography angiography: a systematic review and meta-analysis. J Am Coll Cardiol 57:1237–1247
Sarno G, Decraemer I, Vanhoenacker PK et al (2009) On the inappropriateness of noninvasive multidetector computed tomography coronary angiography to trigger coronary revascularization: a comparison with invasive angiography. JACC Cardiovasc Interv 2:550–557
Choi JH, Choe YH, Min JK (2010) From stenosis imaging to functional imaging: a new horizon of coronary computed tomography. Int J Cardiovasc Imaging 27:1045–1047
Acknowledgements
We thank Dr. Lichy Matthias, Yan Jia, and Fufu Chen of Siemens Healthcare for their thoughtful suggestions and technical support. The scientific guarantor of this publication is Hong Yin. The authors of this manuscript declare no relationships with any companies whose products or services may be related to the subject matter of the article. The authors state that this work has not received any funding. One of the authors has significant statistical expertise. Institutional Review Board approval was obtained. Written informed consent was obtained from all subjects (patients) in this study. Methodology: prospective/retrospective
Author information
Authors and Affiliations
Corresponding author
Additional information
Mengqi Wei contributed equally to the work and should be regarded as co-first author.
Rights and permissions
About this article
Cite this article
Zheng, M., Wei, M., Wen, D. et al. Transluminal attenuation gradient in coronary computed tomography angiography for determining stenosis severity of calcified coronary artery: a primary study with dual-source CT. Eur Radiol 25, 1219–1228 (2015). https://doi.org/10.1007/s00330-014-3519-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00330-014-3519-9