Abstract
Systemic lupus erythematosus (SLE) is a multifactorial autoimmune disease and polymorphisms in the cytokine genes and their receptors are thought to influence its development. The aim of this case–control study was to investigate the association of the IL-17A rs2275913, IL-17RC rs708567 and TGFB1 rs1800469 polymorphisms with SLE, its clinical manifestations and the polymorphisms influence on the IL-17A serum levels. Altogether 59 SLE patients with lupus nephritis and 95 healthy controls were genotyped by TaqMan assay. Serum levels were determined by Human IL-17A Platinum ELISA kit. From the studied polymorphisms, only TGFB1 T allele was found to be associated with SLE. Within the patient group, IL-17A GG genotype and TGFB1 -509T allele showed an association with the neurological disease and IL-17RC CC genotype appeared to be associated with lupus arthritis. The IL17A serum levels in the SLE and control groups (7.24 pg/ml and 5.76 pg/ml, respectively) did not show any statistical difference. A weak correlation between IL17A levels and SLEDAI-2K was observed. Our results indicate that IL-17A rs2275913, IL-17RCrs708567 and TGFB1 rs1800469 polymorphisms might play a role in the susceptibility and the clinical manifestations of SLE and IL-17A serum levels should be monitored in the course of the disease. The identification of subsets of SLE with an IL-17-driven disease could improve the therapeutic approach leading to more precise personalized treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Interleukin 17 (IL-17) is now recognized as a key cytokine in various inflammatory and autoimmune diseases and the IL-17 axis is a common target for biological therapies [1]. A growing body of evidence demonstrates that IL-17A and IL-17-producing cells are also implicated in the pathogenesis of systemic lupus erythematosus (SLE) [2], a complex polygenic autoimmune disease. It is therefore of paramount importance to unveil the molecular mechanisms that drive IL-17 recognition and signalling in SLE immunopathology. The single nucleotide polymorphisms (SNPs) are one of the diverse molecular mechanisms that could play a major role in the pathogenesis of SLE. Alterations of the nucleotide sequence of DNA (a substitution of adenine/guanine (A/G) or cytosine/thymine (C/T)) could be followed by a functional change in the coded protein and thus affecting the clinical manifestations and the response to treatment. This process can take place either in a single DNA strand or in both strands which form the individual genotype (i.e. GG/GA/AA or CC/CT/TT). The SNPs could be located in the gene of IL-17A itself as IL-17A rs2275913 G/A polymorphism, of its receptors as IL-17RC rs708567 C/T, or alternatively of a related cytokine such as TGFB1 rs1800469C/T.
IL-17 is a pro-inflammatory cytokine, produced primarily by a T helper cell subset termed ‘Th17’. The differentiation of the Th17 cells is driven by the simultaneous presence of transforming growth factor-β (TGF–β) and certain cytokines such as IL-6, IL-21, IL-23 [3]. Significantly lower levels of serum TGF-β1 were found in patients with SLE compared to the healthy controls [4, 5] and according to Peng et al. [6], rs1800469 SNP (-509C > T) was found to be related with TGF-β1 plasma concentration. In a classical twin study, the TT carriers had almost double the level of TGF-β1 in plasma compared to the CC ones [7].
Compelling evidence was found that Th17 cells are increased in the peripheral blood of patients with SLE [8,9,10]. Elevated Th17 cells are found to be accompanied by FoxP3 + Treg cells decrease in patients with lupus nephritis [11]. Furthermore, most studies show that the production of IL-17A in patients with SLE is abnormally high [12] and it correlates with SLE disease activity [10, 13, 14]. In addition, recent data suggest that guanine to adenine substitution at position -197 within the IL-17A promoter region has a functional activity and could influence IL-17A levels. In silico investigation showed that G197A gene polymorphism of IL-17A resulted in changes of the pattern in which the IRF-4 binds to the promoter, thereby affecting its activity [15], which in turn upregulates IL-17A-mediated immune responses. The rs2275913 polymorphism was already found to be associated with several other autoimmune diseases [16,17,18] but its role in SLE and lupus nephritis is controversial.
Importantly, IL-17 exerts its function through the IL-17 receptor (IL-17R) complex. Signal transduction for both IL-17A and IL-17F requires the presence of heterodimeric A and C receptors. However, according to Ho and Gaffin, the C subunit plays a key role in modulating IL-17 responses [19]. The SNP rs708567 C/T is a common missense mutation within the IL-17RC gene which may play an important role in impairing IL-17RC function [20].
The aim of this case–control study was to investigate the association between the IL-17A rs2275913 G/A, IL-17RC rs708567 C/T and TGFB1 rs1800469 C/T polymorphisms and the susceptibility to SLE and its clinical manifestations as well as their influence on the IL-17A serum levels.
Materials and methods
Patients and controls
Fifty-nine (49 female and 10 male) patients with systemic lupus erythematosus were included in this study. The mean age was 41.3 ± 12.4 years with a range of 18–78 years. The patients have been followed for a mean of 10 years at the Department of Internal Medicine, Medical University-Sofia. All the patients met the classification criteria of the Systemic Lupus International Collaborating Clinics (SLICC) [21] and were diagnosed with lupus nephritis. The demographic and clinical parameters of the studied group are summarized in Table 1. Patients with other systemic autoimmune and rheumatologic diseases such as rheumatoid arthritis, systemic scleroderma, mixed connective tissue disease, multiple sclerosis were excluded, as well as patients with a history of malignant or concurrent decompensated metabolic disease and hepatitis.
Ninety-five non-related healthy individuals matched for sex, age and ethnicity were included as a control group and compared with the patients. The inclusion criteria for the control group were no previous medical history of autoimmune rheumatic disease and routine laboratory tests within the normal range. They were consecutively selected from the BioBank of the Molecular Medicine Center—associated member of BBMRI-ERIC. From the group of healthy volunteers were excluded those with anamnestic, clinical and laboratory data pointing to autoimmune diseases, as well as those with a family history for autoimmune diseases such as systemic lupus erythematosus, dermatomyositis, scleroderma, rheumatoid arthritis as well history of malignant or concurrent decompensated metabolic disease and hepatitis.
The scientific investigation presented in this article has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) and the study was approved by the local ethics committee of Medical University-Sofia (Reference number 9/25.04.2016).
Patients’ selection process and clinical data
All patients met the Systemic Lupus International Collaborating Clinics (SLICC) classification criteria [21] and have lupus nephritis. In this cross-sectional study, 18 patients (30%) were diagnosed with new-onset SLE at the time of the blood collection for DNA and IL17A level analysis and they were treatment-naive. The other 34 patients (58%) were on maintenance therapy with methylprednisolone 8 mg alone or in combination with either cyclophosphamide pulse therapy 10 mg/kg every 3 months or mycophenolate mofetil 2 g/d or azathioprine 1–2 mg/kg/d. Seven patients (12%) had a lupus flare despite maintenance therapy. Hydroxychloroquine was used in two patients only since the treatment was performed according to KDIGO guidelines 2012. The onset of the disease varied from 10 days to 9 years before the blood collection and we observed the patients from 2010 to 2020 for organ damage. Since the renal involvement (either proteinuria > 0.5 g/24 h or impaired renal function) was the main cause for hospital admission, a renal biopsy was performed in all cases at the time of the disease onset with the following distribution—class I—28.8%, class II—20.3%, class III—13.6%, class IV—28.8%, class V – 5.1% and class VI—3.4%. The SLEDAI-2 K index was calculated based on the clinical manifestations and laboratory tests at the time of the blood collection for DNA and IL-17A analysis. Patients with new-onset disease were further assessed for arthritis—11 patients showed signs of synovitis involving two or more joints. The skin check up showed malar rash in nine patients, discoid rash in four, oral ulcers in one and photosensitivity in nine patients. The neurological condition was assessed by physical examination, electromyography and magnetic resonance imaging by a certified neurologist. A complete comprehensive ocular exam was performed at the time of blood collection. The analysis was retrospective and based on the medical history for the patients already diagnosed with SLE. Finally, we analysed the association between the studied SNPs and ACR criteria based on the 10-year follow-up to assess the role of the SNPs as a predisposing factor for organ damage. SLICC/ACR damage index was not calculated since pulmonary hypertension and fibrosis were not assessed in all patients.
IL-17A serum analysis
The serum samples were centrifuged immediately after blood collection and the serum aliquoted and stored at − 80 °C. The serum IL-17A levels were determined by Human IL-17A Platinum ELISA kit of Affymetrix eBioscience™, according to the protocol provided by the manufacturing company.
Genetic analysis
All participants signed informed consent and genomic DNA was extracted from the peripheral blood with the Chemagen DNA purification kit, using Chemagic Magnetic Separation Module I.
The analysis of IL-17RC rs708567 and TGFB1 rs1800469 SNPs was performed using TaqMan genotyping assay. The allele calling was carried out with Applied Biosystems 7500 software version 2.0.5. The rs708567 context sequence (VIC/FAM) is GAAAAGTTTGGAGGAGCAGCTGACT[C/T]AGGGGTGGAGGAGCCTAGGAATGGT and the rs1800469 context sequence (VIC/FAM) is GAGGAGGGGGCAACAGGACACCTGA[A/G]GGATGGAAGGGTCAGGAGGCAGAC.
The TaqMan reaction was performed according to the instructions provided by Thermo Fisher Scientific in a volume of 5 μl containing 2.5 μl 2X TaqMan® Master Mix, 0.12 μl 40X Assay Working Stock, 0.88 μl dH2O, and 1.5 μl DNA template (10 ng/μl). The amplification conditions were initial denaturation at 95 °C for 10 min, followed by 40 cycles of 95 °C for 30 s and 60 °C for 90 s.
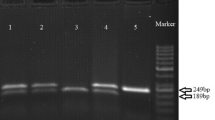
The analysis of IL-17 rs2275913 was performed using HRM analysis. The forward and reverse primers were 5′-ACATGAATTTCTGCCCTTCC-3′ and 5′-GTTCAGGGGTGACACCATTT3′, respectively. HRM reaction was performed in 25 μl final volume and contains 12.96 μl dH20, 2.5 μl (10X) buffer, 0.75 μl (50 mMMgCl2), 1.5 μl (5 mM) dNTPs, primer forward and reverse (10 pM), 1.50 μl (5 nM) dNTPs, Syto9(50 μM) 0.70 μl, DNA (15 ng/μl)3.33 ml and Taq polymerase 0.12 μl. The amplification conditions were initial denaturation at 95 °C for 3 min followed by 45 cycles—95 °C for 15 s, 58 °C for 20 s and 72 °C for 20 s. Melting analysis was with ramp rate from 70–98 °C rising by 0.1 degrees each step. Result analysis was performed on Rotor Gene 3000 Data Analysis software.
Statistical analysis
Statistics were calculated using SPSS 22.0 software (SPSS Inc, Chicago, USA). Shapiro–Wilk test was used to test the normality of IL17A serum levels. Since the distribution was not normal, non-parametrical test (Mann–Whitney test) was used to compare the IL-17A serum levels in the studied groups. One patient from the SLE group and one patient in the control group were excluded, determined as outliers. Spearman analysis was performed to check the correlation between the IL17A level and the disease activity defined by SLEDAI-2K.
The test for Hardy–Weinberg equilibrium was performed using chi-square (χ2) statistics. Changes in allelic and genotype frequencies in SLE patients and healthy individuals (controls) were compared in a case control study using Fisher’s exact test, and their significance was expressed by p value and odds ratios (OR) with exact 95% confidence intervals (CI).The same statistical methods were used to investigate the allelic and genotype distribution within the SLE group according to the presence or absence of the common clinical features to evaluate the allelic/genotype influence on the disease manifestation.
Results
Genetic analysis
All the polymorphisms studied were in Hardy–Weinberg equilibrium.
Among them only TGFB1 rs1800469 T allele was found to be associated with SLE (p = 0.04, OR 1.5, 95% CI 1–2.5) (Table 2). The TGFB1 T allele showed an association with neurological disease (p = 0.044, OR 2.5, 95% CI 1–6.4) (Table 3).
The IL-17A rs2275913G/A polymorphism showed no difference in its distribution among the patients and the controls (Table 2). The IL-17A GG genotype (p = 0.028, OR 4.83, 95% CI 1.2–20.3) and the G allele (p = 0.024, OR 3.8, 95% CI 1–13.6) were found associated with neurological disease (Table 4).
The IL-17RC rs708567 CC genotype appeared to be associated with lupus arthritis (p = 0.029, OR 5.1, 95% CI 1–25.2) (Table 5).
None of the SNPs was found to correlate with the IL-17A serum levels.
IL17A serum levels
The means of IL-17A serum levels in the SLE patients and controls were 7.24 pg/ml and 5.76 pg/ml, respectively. When the Mann–Whitney U test was performed, no statistical significance was found (p = 0.799). IL-17A serum levels did not show any association with the clinical features of SLE according to SLICC, nor with the SNPs. However, Spearman correlation analysis showed an association between IL-17A levels and SLEDAI-2K (Rsp = 0.2581 p = 0.047) (Fig. 1).
Discussion
Recently, there are more data that Th17 cells and their effector cytokines, IL-17A and IL-17F, may play an important role in SLE susceptibility as well as in its activity and this could be related to the response to treatment. Therefore, we examined the impact of plasma IL-17A level on both SLE disease and its activity. Consequently, we investigated polymorphisms in IL-17A and IL-17 receptor C genes in patients with SLE and evaluated their association with the disease and IL-17A plasma concentration. Since there are data about a possible functional role of TGF-β-509C/T (rs1800469) in the TGF-β production and thus Th17 differentiation, we further investigated the corresponding SNP and its role within the IL17 pathway.
In agreement with our expectations previous studies and a recent meta-analysis [22, 23], we found elevated IL-17A levels in the patients with SLE compared to the controls although they were not statistically significant probably due to the ongoing therapy and the corresponding low disease activity (SLEDAI-2K score with a mean of 9.9). It still remains unknown why IL-17A production is increased in those patients, which cell subtype is responsible and whether it is related to the IL-17 pathway, to Interferon-γ/Th1, or IL23/Th17 axis, etc.
The correlation between IL-17A levels and the clinical parameters of the disease and its activity also varies among the different studies. Vincent et al. found an association between the IL-17A serum and the neurological disease in SLE [24]. In contrast, Zhao et al. [22] did not find any association between serum IL-17A levels and the clinical or laboratory parameters of the disease. This finding was consistent with our results. Furthermore, the authors reported no significant difference regarding serum IL-17A levels between SLE patients with nephritis and those without nephritis. However, when disease activity was taken into consideration, an association between serum IL-17A levels and the active lupus nephritis was found [25]. Similarly, when we performed Spearman correlation analysis between IL17A levels and SLEDAI-2K an association was observed (p = 0.047). The discrepancies between the studies can be explained by the small number of patients included, which is a limitation of most studies including the present one. Another cause for these divergent results is the heterogeneity of the disease and the possible diversity of defects in the cytokine axes. The different genetic backgrounds might account, too, suggesting that Th17 and Th1 cell responses might contribute to the disease by distinct pathways. The identification of subsets of SLE patients with an IL-17-driven disease could improve the selection of the "appropriate patients" before starting a trial and that is why more preclinical studies are needed to understand the underlying mechanisms.
The role of the IL-17A G-197A polymorphism on terms of IL-17A levels also remains unclear. A recent study has found that the mutant A-allele carriers of rs2275913 had decreased serum concentration of IL-17A [26]. In vitro stimulated T cells from healthy individuals possessing the 197A allele produced significantly more IL-17A than those without the 197A allele [27]. Nevertheless, two other studies found no correlation between the IL-17A polymorphism and the plasma IL-17A levels in patients with SLE and rheumatoid arthritis [15, 28]. Our study could not confirm the role of rs2275913 for IL-17A production.
Another study has shown no significant difference in the IL-17A G-197A distribution between the patients with lupus nephritis and the control group and in terms of the degree of renal abnormalities [15]. Our study did not confirm any relationship between the polymorphism and the development of lupus nephritis either. Several authors think that the IL-17A G allele and GG genotype could contribute to the development of SLE as part of more complex genotypes -rs2275913GG/rs763780AG/rs2397084A or haplotypes -rs2275913G/rs763780G/rs2397084A [14] and rs8193036T/rs3819024A/rs2275913G/rs8193037A [29]. A borderline relationship between the heterozygous genotype (AG) and the reduced risk of SLE was described and the A-allele was also shown as having a protective effect on SLE susceptibility [30].
It seems that rs1800469 TGF-β polymorphism plays a role in the development of SLE independently from IL-17 pathway since it did not show any influence on IL-17A levels. We found that TGF-β-509T allele is statistically associated with the disease and the TGF-β-509 TT genotype with its neurological manifestations. These results correspond to those obtained in other Slavic populations [31]. Beside the association of the TT genotype and the T allele with SLE in Polish patients, Paradowska-Gorycka et al. [31] report an association of this polymorphism with the mean value of C reactive protein (CRP), haemoglobin, activated partial thromboplastin time (aPTT), International Normalized Ratio (INR) and the presence of anti-Ro and anti-Sm antibodies. Thus, they conclude that TGF-β -509T allele and TT genotype may be considered as a possible genetic marker for SLE, confirmed by our results.
The signal transduction for IL-17A requires the presence of heterodimeric A and C receptors but the C subunit plays a key role in modulating IL-17 responses. IL-17RC rs708567 was found to be associated with the susceptibility to adolescent idiopathic scoliosis. Recently, the role of IL-17RC rs708567 in the pathogenesis of rheumatoid arthritis was investigated by Dhaouadi et al. and our team was the first to study its contribution to the development of SLE. Genotypes and allelic distributions of the IL-17RC polymorphism showed no statistical difference between patients with SLE and controls. We could not find any differences in the IL-17RC genotypes distribution in relation to IL-17A serum levels. However, data show that IL-17RC mRNA is highly expressed in joints [19] and this could be an explanation why we observe an association of rs708567 CC genotype with lupus arthritis.
Limitations
As already mentioned, the major limitation of this study is the relatively small number of patients. Nevertheless, the unique insights of our study would pave the way for larger investigations. We assume that our cohort is heterogeneous including patients with various disease activity and severity. Furthermore, only 30% of the patients were with new-onset SLE. Thus, the clinical features in some patients were assessed retrospectively based on the medical history. Another major limitation of the study was the different treatment regimens. Most of our patients were on maintenance therapy which has an important impact on the interleukin levels and thus the conclusion of the comparative analysis of IL17A levels between SLE patients and healthy subjects may be compromised.
Conclusion
Genetic polymorphisms in cytokine genes, which influence gene expression and cytokine production, may have an important impact on SLE suseptibility and and severity [32]. Monitoring IL-17A serum levels appears to be a useful marker in regard to disease activity and could be implicated in treatment response evaluation. Knowledge on the exact mechanisms of IL17 involvement in SLE is important especially regarding future treatment strategies—possible blockage of IFN pathway by Jak-Stat inhibitors or directly targeting IL17/IL17R/SEFIR which is Jak-Stat independent pathway, or blockage of the IL12/23 pathway. The identification of the exact cytokine axis and pattern could ease the personalized treatment and point towards the right multitarget therapy.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
de Morales J, Puig L, Dauden E et al (2020) Critical role of interleukin (IL)-17 in inflammatory and immune disorders: an updated review of the evidence focusing in controversies. Autoimm rev 19(1):102429. https://doi.org/10.1016/j.autrev.2019.102429
Koga T, Ichinose K, Kawakami A, Tsokos GC (2019) The role of IL-17 in systemic lupus erythematosus and its potential as a therapeutictarget. Expert Rev Clin Immunol 15(6):629–637. https://doi.org/10.1080/1744666X.2019.1593141
Hatton RD (2011) TGF-β in Th17 cell development: the truth is out there. Immunity 34(3):288–290. https://doi.org/10.1016/j.immuni.2011.03.009
Manolova I, Gerenova J, Ivanova M (2013) Serum levels of transforming growth factor-β1 (TGF-β1) in patients with systemic lupus erythematosus and Hashimoto’s thyroiditis. Eur Cytokine Netw 24(1):69–74. https://doi.org/10.1684/ecn.2013.0331
Antiga E, Del Bianco E, Difonzo E, Fabbri P, Caproni M (2011) Serum levels of the regulatory cytokines transforming growth factor-β and interleukin-10 are reduced in patients with discoid lupus erythematosus. Lupus 20(6):556–560. https://doi.org/10.1177/0961203310392424
Peng Z, Zhan L, Chen S, Xu E (2011) Association of transforming growth factor-β1 gene C-509T and T869C polymorphisms with atherosclerotic cerebral infarction in the Chinese: a case-control study. Lipids Health Dis 10:100. https://doi.org/10.1186/1476-511X-10-100
Grainger DJ, Heathcote K, Chiano M et al (1999) Genetic control of the circulating concentration of transforming growth factor type β1. Hum Mol Genet 8(1):93–97. https://doi.org/10.1093/hmg/8.1.93
Crispin JC, Oukka M, Bayliss G et al (2008) Expanded double negative T cells in patients with systemic lupus erythematosus produce IL-17 and infiltrate the kidneys. J Immunol 181(12):8761–8766. https://doi.org/10.4049/jimmunol.181.12.8761
Yang J, Chu Y, Yang X et al (2009) Th17 and natural treg cell population dynamics in systemic lupus erythematosus. Arthritis Rheum 60(5):1472–1483. https://doi.org/10.1002/art.24499
Wong CK, Lit LCW, Tam LS et al (2008) Hyperproduction of IL-23 and IL-17 in patients with systemic lupus erythematosus: implications for Th17-mediated inflammation in auto-immunity. Clin Immunol 127(3):385–393. https://doi.org/10.1016/j.clim.2008.01.019
Xing Q, Wang B, Su H et al (2012) Elevated Th17 cells are accompanied by FoxP3+ Treg cells decrease in patients with lupus nephritis. Rheumatol Int 32(4):949–958. https://doi.org/10.1007/s00296-010-1771-0
Wong CK, Ho CY, Li EK, Lam CWK (2000) Elevation of proinflammatory cytokine (IL-18, IL-17, IL-12) and Th2 cytokine (IL-4) concentrations in patients with systemic lupus erythematosus. Lupus 9(8):589–593. https://doi.org/10.1191/096120300678828703
Doreau A, Belot A, Bastid J et al (2009) Interleukin 17 acts in synergy with B cell-activating factor to influence B cell biology and the pathophysiology of systemic lupus erythematosus. Nat Immunol 10(7):778–785. https://doi.org/10.1038/ni.1741
Hammad A, Osman E, Mosaad Y, Wahba M (2017) Serum interleukin-17 in Egyptian children with systemic lupus erythematosus: is it related to pulmonary affection? Lupus 26(4):388–395. https://doi.org/10.1177/0961203316665709
Gunawan A, Susianti H, Indyanty E et al (2016) The association between G-197A gene polymorphism of IL-17A with changes in protein interaction of IL-17A, levels of urinary IL-17, and degree of lupus nephritis abnormality. Comp Clin Pathol 25:535–541. https://doi.org/10.1007/s00580-016-2222-4
Shu Q, Yang P, Hou S et al (2010) Interleukin-17 gene polymorphism is associated with Vogt-Koyanagi-Harada syndrome but not with Behçet’s disease in a Chinese Han population. Hum Immunol 71(10):988–991. https://doi.org/10.1016/j.humimm.2010.06.020
Holster A, Teräsjärvi J, Lauhkonen E et al (2018) IL-17A gene polymorphism rs2275913 is associated with the development of asthma after bronchiolitis in infancy. Allergol Int 67(1):109–113. https://doi.org/10.1016/j.alit.2017.05.010
Xu H, Pan Y, Li W et al (2016) Association between IL17A and IL17F polymorphisms and risk of Henoch-Schonlein purpura in Chinese children. Rheumatol Int 36(6):829–835. https://doi.org/10.1007/s00296-016-3465-8
Ho AW, Gaffen SL (2010) IL-17RC: a partner in IL-17 signaling and beyond. Semin Immunopathol 32(1):33–42. https://doi.org/10.1007/s00281-009-0185-0
Zhou S, Qiu XS, Zhu ZZ, Wu WF, Liu Z, Qiu Y (2012) A single-nucleotide polymorphism rs708567 in the IL-17RC gene is associated with a susceptibility to and the curve severity of adolescent idiopathic scoliosis in a Chinese Han population: a case-control study. BMC Musculoskelet Disord 13:181. https://doi.org/10.1186/1471-2474-13-181
Petri M, Orbai AM, Alarcón GS et al (2012) Derivation and validation of systemic lupus international collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum 64(8):2677–2686. https://doi.org/10.1002/art.34473
Zhao XF, Pan HF, Yuan H et al (2010) Increased serum interleukin 17 in patients with systemic lupus erythematosus. Mol Biol Rep 37(1):81–85. https://doi.org/10.1007/s11033-009-9533-3
Shen HH, Fan YN, Zhao CN et al (2020) Elevated circulating Interleukin-17 levels in patients with systemic lupus erythematosus: a meta-analysis. Immunol Invest 49(6):662–675. https://doi.org/10.1080/08820139.2019.1699107
Vincent FB, Northcott M, Hoi A et al (2013) Clinical associations of serum interleukin-17 in systemic lupus erythematosus. Arthritis Res Ther 15(4):R97. https://doi.org/10.1186/ar4277
PeliçariKde O, Postal M, Sinicato NA et al (2015) Serum interleukin-17 levels are associated with nephritis in childhood-onset systemic lupus erythematosus. Clinics (Sao Paulo) 70(5):313–317. https://doi.org/10.6061/clinics/2015(05)01
Xie M, Cheng B, Ding Y et al (2019) Correlations of IL-17 and NF-κB gene polymorphisms with susceptibility and prognosis in Acute Respiratory Distress Syndrome in a Chinese population. Biosci Rep. https://doi.org/10.1041/BSR20181987
Espinoza JL, Takami A, Nakata K et al (2011) A genetic variant in the IL-17 promoter is functionally associated with acute graft-versus-host disease after unrelated bone marrow transplantation. PLoS ONE 6(10):e26229. https://doi.org/10.1371/journal.pone.0026229
Dhaouadi T, Chahbi M, Haouami Y et al (2018) IL-17A, IL-17RC polymorphisms and IL17 plasma levels in Tunisian patients with rheumatoid arthritis. PLoS ONE 13(3):e0194883. https://doi.org/10.1371/journal.pone.0194883
Montúfar-Robles I, Barbosa-Cobos R, Alemán-Ávila I, Ramírez-Bello J (2019) IL17A haplotype confers susceptibility to systemic lupus erythematosus but not to rheumatoid arthritis in Mexican patients. Int J Rheum Dis 22(3):473–479. https://doi.org/10.1111/1756-185X.13426
Sharifzadeh M, Naeimi S, Nasiri M et al (2018) IL-17A gene polymorphism at position G197A and systemic lupus erythematosus. Rheumatol Res 3(3):107–112
Paradowska-Gorycka A, Roszak M, Stypinska B et al (2019) IL-6 and TGF-β gene polymorphisms, their serum levels, as well as HLA profile, in patients with systemic lupus erythematosus. Clin Exp Rheumatol 37(6):963–975
Georgiev T, Stoilov R (2019) Bulgarian Rheumatology: science and practice in a cost-constrained environment. Rheumatol Int 39(3):417–429. https://doi.org/10.1007/s00296-018-4202-2
Funding
The study was fulfilled with the financial support of Medical University-Sofia Grant D-67/2016.
Author information
Authors and Affiliations
Contributions
MH: patient recruitment,conceptualization, investigation—ELISA IL17A serum levels, statistics, funding acquisition, writing the original draft, approval of the final manuscript; ZK: conceptualization, help with writing the original draft, critical revision for important intellectual content, approval of the final manuscript; GD: investigation TGFB1 rs1800469 TaqMan genotyping assay, critical revision for important intellectual content, approval of the final manuscript; SN: investigation IL17RCrs708567 TaqMan genotyping assay, critical revision for important intellectual content, funding acquisition, approval of the final manuscript; RH: ophthalmology check, statistics, approval of the final manuscript; KM: investigation of IL17Ars2275913using HRM analysis, critical revision for important intellectual content, approval of the final manuscript; AV: neurology check, approval of the final manuscript; TG: rheumatology check, review and editing, critical revision for important intellectual content, approval of the final manuscript; JP: dermatology check, critical revision for important intellectual content, approval of the final manuscript; RK: methodology and validation, critical revision for important intellectual content, approval of the final manuscript; AS: methodology and validation, critical revision for important intellectual content, approval of the final manuscript; AK: patient recruitment, critical revision for important intellectual content, approval of the final manuscript; LD: dermatology check, supervision, funding acquisition, approval of the final manuscript. Each author agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
No competing financial interests exist.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study has been approved by the local ethics committee of Medical University-Sofia with protocol number 9/25.04.2016.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hristova, M., Kamenarska, Z., Dzhebir, G. et al. The role of IL-17 rs2275913, IL-17RC rs708567 and TGFB1 rs1800469 SNPs and IL-17A serum levels in patients with lupus nephritis. Rheumatol Int 41, 2205–2213 (2021). https://doi.org/10.1007/s00296-021-04996-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-021-04996-z