Abstract
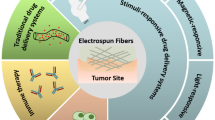
Nanotechnology is a rapidly increasing scientific field due to its immense potential for developing new materials with exceptional structure-dependant characteristics through electrospinning as a feasible technique for producing nanofibers having a wide range of potential applications in cancer detection and diagnostics. Cancer is one of the most deadly diseases that has been afflicting humans for many decades. When dealing with cancer, a regulated and continuous drug release is much desired and effective, because such drugs can cause damage to normal cells. Owing to the high-dose requirements for general anticancer drugs utilized during chemotherapy, they have serious side effects. Anticancer drug-laden nanofibers have been accomplished using nanotechnology for treating cancer, requiring less drug because the drug is stored in these nanofibers for an extended period of time with a tunable drug release profile. Due to the fact that electrospun nanofibers are one of the most advantageous and rapidly evolving products of modern technology, they are promising candidates for cancer therapy. Although numerous research reports have been published on the application of nanofibers, few have focused exclusively on the use of nanofibers in cancer care. Thus, this analysis not only provides a fundamental understanding of the mechanism of electrospinning process and the properties of nanostructured fibrous materials, but also highlights the electrospinning technique's potential as a promising tool for fabricating polymeric nanofibers used for cancer therapy.
Graphical abstract

Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Electrospinning process
Electrospinning is a method of forming nano- and micro-sized continuous fibres from materials in solution after the drying of electrically charged jets [1]. Electrospinning is distinguished from various other types of spinning (e.g. melt, dry spinning, etc.) by the electrostatic force stretching the polymer which is solubilized as it drops, causing the solvent to evaporate [2,3,4]. One of these process's advantages is its technological simplicity and adaptability. This procedure is applicable to both melt and solution polymers. Electrospun fibres have a good, large surface area, impressive surface modification, controllable surface conformation, consistent size, high biocompatibility, and complex pore structure that traditional fibre spinning techniques cannot achieve. This broadens the application of fibres to a variety of fields, including agriculture, tissue engineering, wound dressing, gas sensing, electronic devices, energy storage devices and materials, biomedical applications, drug delivery, catalysis, and defence set-ups, among others.
Set-up and mechanism
It is made up of four main components: a glass or plastic syringe [5,6,7,8,9,10] filled with polymer solution, a high-voltage power supply, a spinneret (a metallic needle), and a metallic collector (grounded and of variable morphology). Electrospinning utilizes direct current (DC) control, although it is also possible to use alternating current (AC) potentials. The polymer solution, also known as the melt, is fed into the syringe, which is then attached to the spinneret. The syringe pump enables a continuous, normal, and controllable rate of solution flow through the spinneret. When a high-voltage supply, typically between 1 and 30 kV is applied, the polymer solution becomes unstable due to the charges induced on the polymer droplet [5,6,7]. The solution at the spinneret's nozzle gets highly electrified, allowing the charges that are induced to be dispersed uniformly over the surface. This causes two forms of electrostatic forces to act on the drop: electrostatic repulsion between the charges on the surface and the Coulombic force applied by the external field. The charges generate a repulsion force that opposes the surface tension, causing the polymer solution to flow in the direction of the external electric field. These electrostatic interactions result in the distortion of the liquid drop into a conical object known as a Taylor cone [11]. The electrostatic forces will surpass the polymer arrangement’s surface tension when the electrical field strength exceeds a particular threshold value [12,13,14]. At that point, the electrified jet is stretched and whipped in the direction of the collector, forming long and thin threads. Only if the polymer solution contains adequate cohesive forces will a stable jet shape be obtained [4, 15]. Due to the continuous stretching and sliding of the polymer chains, its diameter can be reduced significantly from hundreds of micrometres to as little as tens of nanometres following solvent evaporation. After that, the charged fibre is drawn in and deposited by the ground collector located underneath the needle [15,16,17].
Fundamental parameters of electrospinning
The properties of electrospun nanofibers are determined by a variety of boundaries. These divisions are usually classified into three categories. The first category contains parameters relating to the method, which are, applied voltage, distance between capillary and collector, and the polymer flow rate. The second group, solution parameters, contains the solution concentration, the solution conductivity, the solution volatility, and the solvent's solubility. Thirdly, ambient conditions such as humidity and temperature have an effect on the polymer fibres' final morphology.
Properties of electrospun nanofibers
Unlike 1D nanostructures, nanofibers exhibit a variety of remarkable properties, including the ability to regulate their trajectory after being expelled from the nozzle by applying an external electric field. The following are only a few of the extraordinary characteristics that set them apart.
Extraordinarily long length
The continuous synthesis of nanofibers results in the creation of nanofibers with a length of several kilometres [17,18,19]. Due to their permeability, these extremely long fibres can also be assembled into three-dimensional nonwoven mats that can be used for a variety of applications. This may be a result of the spinning jet bending instability. Pawlowski et al. electrospun polymer nanofibers onto a wing frame on investigating lightweight wing skins for a miniature air vehicle [20]. Using metallic tweezers as a guide, Xia and Li demonstrated that single strands ranging in length from a few millimetres to centimetres could be operated independently using a collector with a void [21]. Since the collector is a macroscopic structure, it is possible to monitor individual nanofibers without using a microscope.
High surface area and a complex pore structure
Electrospun fibres, in general, have small diameters and a high surface-to-volume ratio. The strands of electrospun fibres begin to entangle, resulting in a dense network of pores. Kim and colleagues concluded that the Brunauer–Emmett–Teller (BET) surface spaces of electrospun mats varied between 9 and 51 m2 g1, the porosity varied between 25 and 80%, and the pore size varied between 2.737 and 0.167 lm [20, 22]. Despite the fact that electrospun fibres have a lower specific surface area than mesoporous materials such as molecular sieves, their pores are larger and more linked, forming a three-dimensional network. As a result, chemical species have full access to the entire surface.
Molecular arrangement
During the electrospinning phase, the polymer chains are subjected to a strong shear force due to two main factors: the rapid elongation of an electrified jet and evaporation of the solvent. The polymer chains are then unable to unwind back to their equilibrium configurations because of the shear force and rapid hardening. As a consequence, the crystallinity and chain configuration of the polymer nanofibres generated should be unique. Foster and collaborators, for example, determined that the polymer chains in electrospun poly(ferrocenyldimethyl-silane) were aligned and extended parallel to the fibre axis using a technique called electron diffraction analysis [23]. Rabolt and colleagues discovered that electrospinning Nylon-6 resulted in the formation of the c-structure, rather than the a-structure seen in solution-cast films [22, 23]. Stephens 18 Using optical and nuclear power microscopy, Vancso and colleagues investigated the structure and alignment of electrospun PEO nanofibers and concluded that the fibre strands had a surface layer of strongly ordered polymer chains [24]. Pedicini and Farris investigated the stress–strain behaviour of electrospun poly(urethane) (PU) filament mats and concluded that the mats exhibited an essentially unique stress–strain reaction bend in uniaxial elastic studies [25]. Additionally, Martin and Lin reported that the orientation of electrospun fibres made of poly(hexyl isocyanate), a fluid glasslike polymer, was dependent on the fibre diameter [23,24,25].
Smart properties
Electrospun nanofibers have been endowed with “smart” properties that make them extremely useful in a myriad of applications for decades. Stimuli-responsive nanofibers fall under the broad category of smart nanofibers as they are capable of undergoing conformational, that is, volume-related, chemical, or wettability changes in response to an external stimulus. Shape-memory nanofibers, a type of stimuli sensitive nanofiber, are capable of assuming different shapes in response to an external stimulus by transforming from a deformed or temporary state to the original or permanent state [24, 25].
Manipulation of the structure and chemical composition of the polymer nanofibers may result in the creation of a self-cleaning surface. A self-cleaning surface can be formed by modifying the nanofibers' chemical composition and structure, thus altering the nanofiber composites' surface wettability. Additionally, electrospun nanofibers may be used to deliver healing agents for the purpose of fabricating self-healing materials by simulating the natural healing process of human skin. This helps them to self-repair losses, restoring their pristine properties in the process. “Living” nanofibers can also be produced during electrospinning by inculcating live microorganisms like microbes, cells. Additionally, nanofibers can be adjusted with special materials to detect environmental changes. To further distinguish them, these electrospun nanofibers are then combined with additional outstanding properties such as a wide specific surface area, durability, high porosity, portability, and low cost [25].
Why are nanofibers used in cancer treatment?
After the tumour cells are removed during surgery, they retain the potential to recur, making chemotherapy a critical component of resolving this problem. Due to the poor specificity of the drugs, they must also solve the obstacle of not killing normal cells when attacking the cancer cells. To ensure that the toxicity does not affect normal cells, the local area following surgery is maintained at an appropriate concentration of anticancer medication. Thus, the nanofibers loaded with anticancer drugs are designed to deliver the drug in a sustained manner at local sites, making them an ideal candidate for implantation into solid tumour cells. They not only decrease the risk of local recurrence of cancer following the surgery [26], but can also be directed directly at the tumour site [15, 27,28,29,30].
Applications in cancer therapy
Numerous polymers have been shown to entrap and deliver anticancer drugs to specific locations with a specific drug release profile. When handling cancer cells, it is critical to remember the polymer, fabrication process, and the drug along with its post-modification. The following are the most recent developments and advances in the various polymers-based nanofibers used in cancer therapy systems.
Synthetic polymers
Polylactic acid (PLA)
PLA, as a biopolymer, has found several applications in the medical field due to its non-toxicity and marvellous properties [31]. Compatibility with the polymer solution is a critical factor in ensuring effective drug delivery and release kinetics in the treatment of cancer. PLA degrades to lactic acid, and this property, combined with its potency, increases its suitability for medical applications [32]. As PLA nanofibers are electrospun, their core becomes amorphous and the sheaths become semi-crystalline. Furthermore, after collecting the aligned nanofibers on a rotating collector, they exhibited smoother morphology than randomly oriented PLA nanofibers which were collected on a grounded plate collector [33]. As a result, the amorphous core aided in drug diffusion from PLA nanofibers.
Zeng et al. [34] investigated the kinetics of drug release from electrospun PLA nanofibers loaded with paclitaxel, doxorubicin, and doxorubicin hydrochloride. The initial burst release of doxorubicin hydrochloride was observed in doxorubicin hydrochloride stacked PLA, but not in paclitaxel and doxorubicin. This was because doxorubicin was incompatible with the hydrophobic PLA Biopolymer due to its hydrophilic nature, whereas paclitaxel and doxorubicin fit seamlessly into the PLA arrangement due to their hydrophobic nature. Paclitaxel and doxorubicin, both hydrophobic drugs, exhibited zero-order kinetics of drug release due to their compatibility with PLA, which decreased the initial burst release. This aspect made it easier to tailor a drug's release from PLA fibres to be more attractive and maintained by selecting the drug to be loaded [34].
Curcumin-loaded PLA electrospun fibres were confirmed to have an inhibitory effect on rat C6 glioma cells, with up to 60–80% viability after 72 h. Curcumin demonstrated possible anticancer activity without cytotoxicity to normal cells, with the exception of a minor inhibitory effect on the normal cell line used, NIH 3T3 fibroblasts [35].
Xu et al. [36] also used rat glioma C6 cancer cells to investigate PLA–PEG electrospun fibres filled with the anticancer drug BCNU (1,3-bis(2-chloroethyl)-1-nitrosourea). At 48 h, 89% of cell growth was inhibited with a 20% drug loading. At 72 h, there was an increase in the restriction against glioma C6 cells from 89 to 93% using the original 20% drug loading. At 48 h, the virgin drug inhibited cell growth by 90%, but by 72 h, the inhibitory effect on glioma C6 cells had decreased to just 62% due to the drug's instability.
Chen et al. [37] demonstrated that smooth PLA nanofibres induced with a maximum of 15% titanocene dichloride had antitumour activity in vitro. The fibres were measured against human spca-1 lung cancer cells having real drug concentrations of 40, 80, 160, and 240 mg/l from both the fibre mats and the virgin drug. Both fibre mats and virgin medication inhibited cancer cell development by 68.20 and 73.10%, respectively. Initially, a burst release was observed, followed by a long period of slow and regulated release, which is beneficial. In vivo and in vitro, multilayer PLA nanofiber structures filled with oxaliplatin and dichloroacetate demonstrated enhanced cancer cell death. These PLA-based multilayer nanofibers could be conveniently applied to a surgically removed tumour site [38].
Qiu et al. [39] prepared mesoporous Silica nanoparticles with an average diameter of 119 nm using a surfactant which is neutral or charged via template method. He then filled these mesoporous silica nanoparticles with the anticancer agent doxorubicin hydrochloride (DOX) and used them to treat HeLa cells. When the concentration of drug-loaded silica nanoparticles in PLA nanofibres was increased from 5 to 15%, the mechanical properties of nanofibers, such as tensile strength, Young's modulus, and elongation decreased. PLA nanofibers demonstrated an initial drug burst followed by sustained release for up to 808 h. The disadvantage was that, while these composite nanofibers of PLA exhibited less cytotoxicity with drug concentrations up to 25 g/ml when compared to free DOX, they exhibited a strong inhibitory effect on cell growth at 50 g/ml when compared to free DOX.
Ignatova et al. [40] electrospun poly(L-lactide-co-D, L-lactide) (coPLA) fibres loaded with quaternized chitosan in combination with DOX against HeLa cells and concluded [40, 41] that these fibres inhibited HeLa cells more effectively for the initial 6 h than pristine DOX. Additionally, Ignatova et al. [41] demonstrated the efficacy of coPLA electrospun fibres filled with quaternized chitosan in combination with DOX in the treatment of human breast carcinoma cell lines. Significant anti-proliferation activity was demonstrated by the drug-loaded quaternized chitosan fibres against carcinoma cells, indicating that the electrospun mats could be used to treat cancer carcinoma cells.
Toshkova et al. [42] defined an effective method for treating Graffi myeloid tumour cells with coPLA electrospun strands having quaternized chitosan and DOX. At 24 h, the cytotoxicity of electrospun filaments and free DOX was similar to that of tumour cells. With increasing concentrations of quaternized chitosan, an inhibitory effect was observed on the cell growth. Chitosan also killed Graffi apoptotic cells at a 100% rate, which may have inhibited its development through apoptotic changes, as Hasegawa et al. described against bladder tumour cells [43].
After coating the Fe3O4 NPs-loaded PLA electrospun fibres with tetraheptylammonium particles and daunorubicin (DNR) compound, it was confirmed to be effective against K562 leukaemia cancer cell lines [24]. Fe3O4 nanoparticles when combined with PLA nanofibers also enhanced the drug's cellular absorption. Due to the drug's positive nature, an improvement in DNR activity was accounted for. Following this, the negative charge of the PLA nanofibers caused DNR to accumulate on their surface, thereby leading to an increase in the absorption and bioactivity of DNR by tumour cells.
A reservoir-type anticancer drug delivery system was formulated using electrospun PLA–PEG fibres. Xu et al. [44] accomplished these results by emulsion electrospinning, in which DOX-loaded PLA–PEG electrospun fibres were emulsified with sodium dodecyl sulphate as a surfactant. He found that with an increase in the hydrophilic drug DOX concentration in the emulsion, there was an increase in the thickness of the sheath as well, yet the centre became thinner. Interestingly, the first and second stages of the drug release followed Fick's Law, owing to the reservoir-type scheme. According to Fick’s law of diffusion, the flux moves from regions of higher concentration to regions of lower concentration, and it was stated that the earlier stage of drug release was less than the later stage.
Luo et al. [45] investigated the anticancer activity of electrospun PEG–PLA nanofibers, known as PELA, containing hydroxycamptothecin (HCPT) against mouse Hepatoma H22 cancer cells. Initially, the fibres demonstrated burst release of HCPT accompanied by sustained in vitro release. Several primary findings included the following: up to 90% of the HCPT drug was released after 20 days of incubation, the degradation rate of the PELA fibres accelerated when the HCPT drug was added, and the drug was highly sensitive due to the existence of the lactone ring. When the fibres were tested in vitro for cytotoxicity, they demonstrated an inhibitory effect of 20-fold against HepG2 cancer cell lines when compared to HCPT, and their in vivo activity against H22 cancer cells in mice was meaningful.
Zhang et al. [46] sought to fabricate a heart/shell structure using electrospinning and thermoresponsive pNIPAM as the shell and polylactic acid PLA as the core. In the presence of a tubulin polymer known as combretastatin A4 (CA4), the PLA NFs were created.
The PLA Nanofibers were synthesized in the presence of combretastatin A4 (CA4), a tubulin polymerization inhibitor and model compound, as well as the cross-linker (N,N′-methylenebisacrylamide). The in vitro drug release was found to vary with decreasing critical solution temperature. The pNIPAM shell was effective at limiting the rate of CA4 release below the lower critical solution temperature (LCST), but greatly increased the rate of drug release above the lower critical solution temperature. Cicotte et al. investigated the reversible attachment of pNIPAM mats seeded with mammalian cells using two kinds of cells. They used both regular (MC3T3-E1) and cancerous (EMT6) cell lines. He discovered that pNIPAM mats made of small and dense fibres derived from high molecular weight pNIPAM polymers exhibited a rapid release process.
Similarly, Jing electrospun hydrophobic drug PTX and hydrophilic drug DOX into poly(ethylene glycol)–poly(l-lactic acid) (PEG–PLA) to achieve rapid and sustained release of DOX and PTX. Not only did sequential transmission from the dual system result in increased apoptosis and inhibition of rat glioma C6 cells, but it also resulted in increased antitumour efficacy. For instance, sequential administration of combretastatin A4, a vascular disrupting agent, and hydroxycamptothecin, a chemotherapeutic drug, sequentially killed endothelial and tumour cells, destroying tumour vasculature and resulting in limited tumour metastasis to the lung [47].
Using the property of randomly oriented nanofibers to successfully mimic the ECM architecture of tumour tissue, Mo and coworkers designed electrospun nanofiber scaffolds as 3D cancer models. They proved that L-929 cells permeated and multiplied within the 3D scaffolds, showing a side to side asymmetry.
Hingtgen engineered stem cells that secrete tumour necrosis factor-related apoptosis-inducing ligand (TRAIL) on electrospun PLA nanofiber implants. When the NFs released the antitumour protein TRAIL, a successful inhibition of residual glioblastoma regrowth was observed, as well as a longer median survival period in mice following their implantation into the surgical cavity [48].
The conclusion reached was that PLA could be a viable option for extending the period of drug release up to 90 days. Additionally, depending on the type of drug used or the molecular mass of PLA, PLA nanofibers demonstrated a mixture of initial and sustained burst release, demonstrating their efficacy in destroying various cancer cell lines. While establishing a connection between in vitro and in vivo studies can prove difficult due to the large molecular diversity of PLAs, their interaction with drugs, and the changing biological climate.
Poly(L-Lactide)/PLLA
Paclitaxel (PTX) was incorporated into poly(L-lactic acid-co-caprolactone), in the ratio of 75:25 of PLLA-CL NFs. The injector was composed of a coaxial needle with an inner chamber filled with paclitaxel (PTX) solution and an outer chamber filled with the polymer [37]. Paclitaxel is a chemotherapeutic agent that is widely used to treat cancers of the breast, lung, ovary, prostate, and bladder. PTX was employed and dissolved it in 2,2,2-trifluoroethanol. Following that, he electrospun the PTX solution directly into a polymeric P(LLA-CL) shell. They synthesized a variety of cone/shell NFs with variable diameters that varied according to the polymer concentration and flow rate between the two solutions. After closely monitoring the drug delivery through the arrangement, it was determined that a brief burst of PTX occurred within the first 24 h, followed by a very slow release for the next 60 days. Without a doubt, the PTX-IN-P(LLA-CL) nanofibers, too, inhibited HeLa cell operation [37].
Lovastatin was fully dissolved in a solution of PLLA and hexafluoro-isopropanol as the solvent [49]. In PLLA, lovastatin was used at weight percentages of 0, 5, and 10%. At lovastatin concentrations of 5 or 10%, an improvement in the NFs properties was observed, not only in terms of alignment but also in terms of surface smoothness and diameter. Lovastatin encapsulated in PLLA Nanofibres demonstrated a high drug entrapment efficiency of 72–82% and also demonstrated a two-stage in vitro drug release behaviour. Initially, a rapid release was observed during the primary day, followed by a slower release that reached a steady level after 7 days.
Qiu et al. [50] formulated a drug-loaded implantable device to treat a tissue defect after tumour resection. UV spectroscopy was used to incorporate Mesoporous Silica Nanoparticles (MSNs) loaded with DOX into electrospun PLLA NFs, and then a few nanocomposite frameworks containing various MSNs and DOX material were developed. They discovered high DOX-loading capacities when they examined the in vitro antitumour viability against HeLa cells. Not only was the drug released continuously, but its in vitro antitumour efficacy was also higher as compared to free MSN particles. In this way, these composite nanofibers mats are extremely encouraging as a possible postsurgical malignancy treatment device.
Zhang et al. [35] used the ability of carbon nanotubes to absorb near infrared radiation to consolidate DOX and multi-walled carbon nanotubes (MWCNTs) in a methanol/chloroform solution dispersed with PLLA in CHCl3 to create nanofibers. Without the methanol/chloroform solution, the DOX release was extremely restricted in the PLLA. Nevertheless, when NIR light (2 W/cm2) was added to DOX-stacked MWCNTs in PLLA, burst arrival of the stacked DOX occurred in 2 h with 20% rate during the 30 min illumination cycle. It was concluded that the NIR radiation increased the temperature of the tumour area in contact with the Nanofibers.
Due to the tumour tissue's acidic microenvironment, the pH-dependent kinetics of drug release is accounted for, ranging from 7.4 (typical tissue) to 6.8 (tumour tissue) (harmful tissue). Cui and his colleagues demonstrated this by electrospinning poly(l-lactic) (PLLA) strands with CaCO3-coated DOX-mesoporous silica nanoparticles (MSN) [51]. CaCo3 interacts with the H + ions produced by the tumour cells' acids and produces CO2, thus increasing the penetration of water into the PLLA strands, assisting release of the drug.
Controlling adverse effects that can be fatal to nontumourigenic sound proliferating cells is one of the most difficult aspects of cancer therapy. Wu et al. also electrospun PLLA nanofibers as a carrier for titanocene dichloride against lung tumour cells, achieving inhibition rates of 11.2, 22.1, 44.2, and 68.2% with drug concentrations of 40, 80, 160, and 240 mg/L, respectively [35].
Jing developed doxorubicin-stacked PLLA electrospun nanofibers to inhibit incurable liver cancer and to prevent tumour recurrence following surgery. In doing so, he observed an improvement in the median survival time of mice carrying auxiliary hepatic carcinoma from 14 to 38 days.
Xu et al. [52] used an emulsion electrospinning process to build anticancer nanofiber layouts from composites of polyethylene glycol and poly(L-Lactic corrosive) diblock copolymer with paclitaxel and doxorubicin. Due to paclitaxel's hydrophobic nature, its doxorubicin release was found to be slower than that of the scaffold. Additionally, it was demonstrated that the combination therapy for cancer drug delivery using rat glioma C6 cells delivered more drug than the single-loaded drug system [52].
Poly(lactic-co-glycolic acid)/PLGA
Xie et al. synthesized the antitumour drug paclitaxel in PLGA electrospun nanofiber mats [53, 54]. The drug's release was studied in vitro using C6 glioma cells. He was able to monitor the diameter of the polymer fibres by studying their behaviour in presence of various polymer concentrations and quantities of an organic salt called tetrabutylammonium tetraphenylborate (TATPB) [53]. The diameter of the NFs was reduced from approximately 10 mm to 30 nm following the addition of salts [54]. There was a 99% encapsulation efficiency for PTX-IN-PLGA NFs, confirming a continuous drug release for up to 60 days. Ranganath et al. [55] have demonstrated that these submicron/nanoscale intracranial implants have promising paclitaxel pharmacokinetics within the brain or tumour with substantial tumour inhibition when used to treat malignant glioblastoma in mice.
Wei et al. [56] defined a method for incorporating nano- and microparticles into electrospun PLGA and gelatin fibres enveloped with ZnO nanoparticles. These were equipped with both the hydrophobic anticancer agent camptothecin (CPT) and the hydrophilic anticancer agent doxorubicin (DOX). This hybrid system demonstrated a low rate of DOX release. CPT, on the other hand, demonstrated a rapid release rate during in vitro research. Additionally, adding gelatin improved the mechanical properties of the fibres, resulting in a decrease in drug burst release. The composite fibres demonstrated a high level of antitumour activity against HepG-2 cancer cell lines.
Vashisth et al. [52] investigated the treatment of Hep G2 cancer cell lines using PLGA/PEO electrospun fibres filled with ferulic acid (FA). Scanning electron microscope revealed the smooth surface of PLGA/PEO fibres loaded with FA with an average diameter of about 150 nm. In vitro, these fibres exhibited a high level of cytotoxicity against Hep G2 cells. The produced fibres outperformed isolated FA due to the prolonged release effect of FA. While isolated FA inhibited cancer cell growth by 51.90%, PLGA/PEO nanofibers loaded with FA inhibited growth by up to 71.30%, owing to FA’s sustained release.
To low-water-soluble molecules such as PTX, a hydrophilic anti-toxin drug called MefoxinR was electrospun into polymeric NFs using PLGA. A blend of PLGA/PEG-b-PLA/PLA was formed in the ratio 80:15:5, respectively [57]. The density and morphology of the nanofibers were observed to be dependent on the drug and ionic salt concentrations. After one hour of dosage administration, they acquired intriguing antimicrobial effects on Staphylococcus aureus cultures [57].
In the electrospun PLGA/gelatin NFs configuration, the PLGA MSNs increased the hydrophobicity of the electrospun NFs, while gelatin increased the mechanical properties. These nanoformulations with a final size of approximately 267 nm provided an optimal microenvironment for stem cell adhesion, development, and migration during nervous tissue regeneration [58, 59].
Additionally, Qi et al. [60] observed that the integration of MWCNTs, filled with DOX, into PLGA NFs increased their mechanical properties and investigated the in vitro viability of these composite nanofibers using 1929 cells. Not only did the dispersing DOX-loaded MWCNTs in PLGA cause reduction in burst release, but it also allowed sustained DOX release for more than 42 days. Additionally, Yu et al. used this CNTs-in-NFs method to electrospray DOX HCL. Although the amount of carbon nanotubes in the final mixture was altered, its in vitro antitumour efficacy against HeLa cells demonstrated a sustained, prolonged DOX release effectively inhibiting HeLa cell formation.
Sasikala et al. [61] developed an implantable hybrid NFs system with two important applications: magnetic hyperthermia in response to an AMF and a drug release specific to cancer cells, facilitating synergistic cancer therapy. Bortezomib (BTZ), a borate-containing anticancer drug and protease inhibitor, was used to achieve this. A mixture of Fe3O4 NPs dispersion, PlGA solution, and a polydopamine shell was fabricated using blend electrospinning. Polydopamine was used as a shell-mimicking mussel adhesive, causing several catechol moieties to bind to it and release an anticancer drug containing borate. The hybrid NFs demonstrated strong fibre morphology and some Fe3O4 aggregation within them. After three cycles of hyperthermia, PLGA nanofibers loaded with BTZ in Fe3O4 demonstrated increased antitumour efficacy in murine breast cancer cell lines (4T1).
A synergistic therapy was needed that could inhibit cancer cell proliferation, angiogenesis, and invasion simultaneously. Wang accomplished this by combining RNA interference with chemotherapy for brain tumour treatment, with each drug performing a unique role. To inhibit tumour cell proliferation, the anticancer drug PTX was used, and MMP-2 RNAi plasmids were used to inhibit cancer cell invasion and angiogenesis [62]. The benefit of this method was evaluated in an in vivo analysis using a mixture of PLGA, PTX, and PEG solution to create an intracranial xenograft tumour model in BALB/c strain of nude mice.
Hou et al. embedded novelcro chips in PLGA nanofibers and conjugated antibodies known as anti-CD146 which are specific to melanoma. This procedure was used to isolate individual circulating melanoma cells [62]. Electrospinning was used to encapsulate low molecular weight PLGA copolymers with curcumin, resulting in smooth nanofibers. Additionally, no aggregations were found on the soil. A sustained release of curcumin was seen in the in vitro experiments, as well as a cytotoxic effect on the A431 squamous carcinoma cell line.
Lee et al. used PLGA fibres sheets to deliver epigallocatechin-3-O-gallate to the damaged abdominal aorta in order to minimize intimal hyperplasia (EGCG). For 24 h, a burst release of EGCG was observed from the EGCG-loaded sheets. They exhibited continuous release in phosphate buffer for the next 30 days and longer. In vivo experiments with these EGCG-loaded fibres demonstrated that they were effective against intimal hyperplasia. To create an ideal implant carrier for radiotherapy with minimal side effects, Nie et al. [63] used electrospun PLGA ultrafine fibrous membranes and surface-modified them to stably bind radionuclide 90Y. The labelled nanofibrous membrane functioned as a novel radio-medical appliance, killing cancerous cells locally. It could be customized not only to the tumour's size but also quantitatively surface-modified with 90Y to meet the tumour's needs.
Koyakutty and coworkers employed a temozolomide-loaded poly(lactic-co-glycolic acid) (PLGA)/PLA/ PCL electrospun mat for the treatment of recurrent glioma [61, 62, 64].
Cellulose acetate
CA is formed when cellulose reacts with acetic anhydride and acetic acid in presence of sulphuric acid [62, 65]. To shape fibres, cellulose acetate in solution with an ideal degree of substitution (DS), typically between 2 and 2.5, is needed. CA is readily soluble in a variety of solvents, including acetone, methyl acetate, and dioxane, within this class of degree of substitution. CA is, however, soluble in dichloromethane if degree of substitution is greater than 2.5 [66, 67], almost completely (90–95%) when immersed in the solution. The electrospun CA fibres containing curcumin were found to be non-toxic to human dermal fibroblasts.
Poly(hydroxyalkanoate)/PHA
Polyhydroxyalkanoates (PHAs) fall under the category of green materials which are biocompatible and biodegradable and are formed by a variety of microorganisms [68, 69]. PHAs have been shown to be both healthy and effective for tissue regeneration and cell proliferation without causing tumours [70]. While PHA nanofibers were less crystalline than bulk film, they had a greater contact angle (130° for PHA versus 77° for bulk film), which could be attributed to the increased surface roughness of these fibres [71, 72]. Being a product of microorganism synthesis, commercialization of these polymers is a significant challenge due to the high cost of purity.
Researchers have found that the anticancer efficacy of cationic peptides has been increased when cationic peptides are conjugated to the depolymerized PHAs forming (R)-3-hydroxidecanic acid (R10). Conjugated or conjoint peptides are cytotoxic to a greater extent than in vitro non-conjugated peptides to colorectal cancer (HT-29), lung carcinoma (A549), T-celled leukaemia, human glioma (SNB-19), breast carcinoma (MDA-MB-231) and human pancreatic carcinoma (MiaPaCa) cell lines [71, 72].
Poly(styrene)/PS
Polystyrene (PS) is a man-made polymer with a very low biodegradation rate. These nanofibers have been successfully used for magnetic hyperthermia treatment of cancer cells when loaded with iron oxide nanoparticles (IONPs) [73]. Hyperthermia therapy works by killing cancer cells by applying heat to a targeted region. On exposing it to an alternative magnetic field, the iron oxide nanoparticles-loaded-PS nanofibers produce heat. Additionally, coating these PS nanofibers with collagen improved cancer cell adhesion to the nanofibers. Within ten minutes, they eliminate all human ovarian cancer cells, SKOV- 3, attached to its surface.
Daunorubicin, an anticancer drug, was stated to form electrospun fibres when loaded in poly(N-iso-propylacrylamide)-co-polystyrene. These fibres effectively treated and decreased multiple drug resistance (MDR) of leukaemia 562 cancer cell lines, which resulted in increased drug absorption [74]. When MDR leukaemia 562 cells were treated with nanofibers, the cells displayed increased fluorescence, indicating that the nanofibers had an effect on P-glycoprotein, a multi-drug-resistant protein. The MDR-protein, in its purest form, repels the drug. When the drug is loaded into the nanofibers, the cancer cells' MDR-protein does not detect it and the drug becomes bound to the nanofibers. Thus, there is a release of daunorubicin from nanofibers, efficiently penetrating cancer cells and resulting in increased fluorescence [73, 74].
Huang et al. dispersed and ultrasonicated [75] 50 mm Fe3O4 NPs in THF and then used blend electrospinning to form a mixture of PS solution. Due to the fibres’ high loading ability, the hybrid Fe3O4-in-PS NFs device underwent a significant heating process following AMF application. Additionally, collagen could be functionalized on the surface of the hybrid NFs to promote cell attachment. This technique has two critical advantages: The fibres can be filled in a safe and controlled manner with magnetic nanoparticles and magnet resonance imaging (MRI) can locate the composite fibres in the body [75].
Metalloproteinase 9 is a promising and recognized candidate for diagnostic cancer owing to its widespread upregulation in malignant tissues. This was detected by Koh and Han through the combination of a hydrogel-framed electrospun polystyrene/poly(styrene-alt-maleic anhydride (PS/PSMA) nanofiber with a microfluidic device. Additionally, they discovered that they can also facilitate the handling and integration into microfluidic systems with the incorporation of hydrogel micropatterns into the electrospun matrix [75, 76].
Poly(vinyl alcohol)/PVA
PVA is a biodegradable and biocompatible polymer that has been used as a capping agent in drug delivery applications [77]. Detection of cancer at an early stage is proven to be extremely helpful. Zhao et al. [78] used electrospun PVA and polyethyleneimine (PEI) nanofibers with a diameter of approximately 460 nm to detect and capture CD44 cancer cells in their early stages. The nanofibers developed were smooth and exhibited high haemocompatibility and cytocompatibility [78, 79]. Additionally, Fan et al. [79] immobilized folic acid on PVA/PEI nanofibers in order to detect and diagnose early-stage cancer using folic acid receptors.
The ability of PVA nanofibers loaded with Pt (iv) micelles and Dichloroacetate (DCA) to treat cancer cells with less systemic toxicity and increased anticancer system efficacy has been documented. DOX-loaded PVA-with chitosan-loaded core–sheath nanofibers are also well-known for their ability to treat SKOV3 ovarian cancer cells with tunable DOX release. Singh et al. sought to avoid extravasation, inflammation, and other adverse effects associated with chemotherapy while treating oral cancer. He electrospun Docetaxel (DOC) into polyvinyl alcohol (PVA) fibre to create a mucoadhesive nanocarrier DOC-PVA. It demonstrated that anticancer drugs can be successfully administered locally using polymeric NF in in vitro studies [79,80,81].
Core–sheath structured nanofibers were developed using blend electrospinning with PVA, active-targeting micelles, being the core component and cross-connected gelatin as the layer of sheath. The micelle-in-nanofiber system implantable DOX-loaded device has the potential to significantly reduce drug administration frequency, adverse effects, and dosage while remaining very effective against an artificial solid tumour [81, 82]. Although achieving uniform micelle dispersion in the polymer solution is a significant challenge, encapsulating micelles in electrospun nanofibers will improve micelle stability and provide a longer time of sustained release.
Malhotra and colleagues synthesized a paper-based conducive framework using electrospun poly(3,4-ethylenedioxythiophene) and poly(4-styrene-sulfonate)/PVA, that is, (PEDOT:PSS/PVA) fibres. Monoclonal anti-carcinoembryonic antibodies were physically absorbed onto the system of nanofibers to ensure the identification of cancer biomarkers [80,81,82]. With a linear detection range of 0.2 to 25 ng/mL, a higher sensitivity of 14.2 A ng/mL cm2, and a shelf-life of 22 days, this paper biosensor has shown improved sensing efficiency for the detection of the cancer biomarker carcinoembryonic antigen.
Thundat exploited cancer cells' ability to absorb glucose and excrete lactate to deposit pH-sensitive PVA/PAA electrospun nanofibers. This was accomplished successfully on a light-addressable potentiometric sensor surface to measure or quantify the cancer cell acidification. It aided them in noninvasively comprehending not only their metabolic activities, but also their response to chemotherapies. Regulated, controlled release for about 24 h, combined with a decline in the viability of basal-cell (BCC) cell line was observed in the in vitro and ex vitro drug release profile of 5-fluorouracil-chitosan and polyvinyl alcohol (PVA) mixtures. The combination of photothermal-induced hyperthermia and pharmaceutical supply has shown increased cytotoxicity in vitro and in vivo in Hela cancer cells. By electrospinning, Barzegar et al. [83, 84] introduced graphene into PVA NFs to generate hybrid NFs of graphene/PVA.
Polyvinyl pyrrolidone (PVP)
Electrospinning resulted in smooth and homogeneous curcumin-loaded polyvinyl pyrrolidone (PVP) nanofibers. Curcumin-loaded PVP nanofibers demonstrated enhanced anticancer activity when tested in vitro against the B16 murine melanoma cell line. Additionally, they demonstrated an enhanced tumour inhibitory effect when tested in vivo on C57BL/6 mice [83, 84].
Zhang and colleagues used a series of steps to isolate cancer cells from synthetic circulating tumour cells blood samples using a sequence of steps. To begin, a TiO2 nanofiber substrate was created by calcining titanium n-butoxide (TBT) by electrospinning it with polyvinylpyrrolidone (PVP) fibres [85]. Then, using N-hydroxysuccinimide (NHS)/maleimide chemistry, streptavidin (SA) was introduced onto the surface of TiO2 nanofiber coated with N-maleimidobutyryloxy succinimide ester (GMBS). Finally, biotinylated epithelial cell adhesion molecule antibody (anti-EpCAM) was combined with substrates coated with SA. Additionally, in vitro examinations demonstrated the capability of the NF system to capture whole blood samples from patients with gastric and colorectal cancer.
Polyacrylonitrile (PAN)
Using a radiotherapeutic method, radioactive holmium-166 (166Ho) was used to create a bandage by inserting it into electrospun PAN nanofibers. To begin, the bandage was fused with nonradioactive holmium-165 (165Ho) iron garnet nanoparticles. Following that, neutron activation was used to generate 166Ho, which not only provided stable bandages but also avoided any significant leakage, meeting the safety requirements for treatment of skin cancer lesions without harming healthy cells. Additionally, photothermal therapy (PTT) has been used by photothermal agents such as gold nanostructures and graphene oxide to transform near infrared (NIR) light into heat, thus ablating tumours [85,86,87].
Additionally, self-immolating polymer (SIP)/polyacrylonitrile (PAN) fibres [88] were used to fabricate stimuli-responsive NFs for antitumour drug delivery. When exposed to an external stimulus, these NFs rapidly depolymerize, resulting in instantaneously releasing transported molecules at the specified time.
Feng et al. [63] employed blend electrospinning to fabricate a mixture of Fe3O4 NP and functionalized graphene oxide sheets, which were then introduced into PAN to form nanofiber films. These hybrid films showed strong magnetic properties after being dispersed in tertbutanol solution. Additionally, the external graphene oxide (GO) on the surface of the fibres facilitated cell membrane protein adhesion, resulting in a high degree of biocompatibility. Due to these properties, breast cancer cells were captured on the surface of these Short-Fibres.
Polycaprolactone (PCL)
In vitro-cytosis of human breast cancer cells, MCF7 and lung cancer, A459, cell lines as opposed to 1% of PCL nanofibers loaded with cis-platinum cells (on commercial grading) after 24 h of incubation has been demonstrated in the presence of curcumin and natural extract-laden PCL nanofibres [89]. The mechanical characteristics of PCL nanofibers were enhanced by the adding of aloe vera. On the other hand, turmeric and neem extract had a negative effect on their mechanical characteristics. However, in comparison with commercially available PCL-loaded cis-platin fibres, the fibres produced superior inhibition of growth against the tested cancer cell lines [89].
Yohe et al. [90] investigated how air trapped inside nanofibers could be used to enhance the stability of PCL electrospun fibres encapsulated in a hydrophobic poly(glycerol monostearate-co-caprolactone) (PGC-C18) polymer. This was validated using two different forms of anticancer medications. When the nanofibers were tested against human colorectal cancer cells, it was discovered that they were cytotoxic for above 90 days and that adding PGC-C18 conferred superhydrophobicity on the fibres. Additionally, adding PFG-C18 raised the water contact angle from 121 to 143°, but resulted in a slower and more prolonged drug release. On the whole, the super-hydrophobic nature and the entrapped air resulted in less hydrolysis and longer-lasting drug release [90, 91].
Chen et al. developed a formulation of indomethacin (MC) using PCL and gelatin fibres. He then combined this structure with DOX-loaded nanoparticles of the core–shell form. This device was tested against mouse tumour cells and demonstrated sustained drug release and 96% inhibition of cancer cells [92].
Green tea phenols were loaded into PCL and multiwall carbon nanotubes (MWCNTs) by Shao et al. [93]. These nanofibers were then screened for treatment of cancer hepatoma, Hep G2 and human epithelial, A549 cancer cells. It was observed that the green tea phenol-loaded nanofibers had a greater antitumour efficacy against Hep G2 cells than A549 cells during in vitro study. Using PCL electrospun nanofibers coated with polydopamine, Xie et al. fabricated a pH-responsive drug delivery system. The polydopamine coating was used because it was permeable to charged molecules at a wide range of pH values. DOX drug release was also observed in acidic instead of neutral or basic aqueous solutions, drastically to decrease cancer cell viability [94].
Hadjiargyrou electrospun PCL nanofibers with plasmid DNA encoding small/short hairpin RNA (shRNA) directed against the cell cycle-specific protein Cdk2. The electrospun nanofiber scaffolds filled with DNAs were observed to be capable of delivering bioactive and intact plasmid DNA for more than 21 days, resulting in reducing the proliferation of MCF-7 breast cancer cells by 40%.
Lannutti and colleagues developed core/shell structured fibres and an oxygen-sensitive probe using PCL as the shell. To detect oxygen, it also contained platinum-octaethylporphyrin (PtOEP) and tris(4,7-diphenyl-1,10-phenanthroline) ruthenium (II) (Ru(dpp)) with polydimethylsiloxane (PDMS) as the nucleus. The sensor responded rapidly in a span of 0.5 s, owing to the porosity of the structure and the high oxygen permeability of PDMS for cancer detection [95].
Viapiano examined the migratory ability of metastatic cancer cells using closely aligned PCL nanofibers. The alignment of glioma cells on aligned nanofibers activated STAT3, also known as the transcription factor, which is a critical regulator of tumour metastasis and progression in solid cancers [96].
The effect of an electrospun nanofibre substrate on chemoresistance was examined by Kmiec as a critical factor in the failure of current chemotherapy treatments. He studied the activity of highly chemotherapy-resistant breast cancer stem-like cells (BCSCs) that develop on PCL/chitosan nanofibers and found that BCSCs increased mammary cell markers and increased their potential to form spheres [97].
Bellamkonda developed a novel anticancer therapeutic method and termed it as the “tumour guide” unit, which used aligned PCL nanofibers as a guide. The intriguing property of these NFs is that they structurally resemble blood vessels and white matter tracts, allowing invasive tumour cells to migrate away from the tumour site and into the extracortical space. In vitro analysis revealed that the glioblastoma cells- U87MG-eGFP were elongated on the aligned fibres, in contrast to the polygonal form on the smooth film. Additionally, over a 10-day period, the cells migrated 4–4.5 mm along the aligned nanofiber but only 1.5 mm along the smooth films. The glioblastoma cells’ movement along the aligned nanofibers not only reduced the total tumour volume significantly, but also moved and inhibited the growth of primary tumours [98].
Hartman et al. electrospun perlecan domain IV (PlnDIV) peptide with 3D PCL/gelatin nanofiber scaffolds and demonstrated that these scaffolds aided C4-2B cancer cell proliferation, survival, and migration [99].
Holzapfel combined tubular PCL scaffolds with human mesenchymal cells and rhBMP-7 to create a humanized bone organ using melt electrospinning. The resulting framework stimulated the proliferation of human prostate cancer cells and resulted in the creation of macro-metastases [100].
Zhang et al. [95] synthesized a triblock copolymer system from poly(L-glutamic acid)-b-poly-(propylene oxide)-b-poly(L-glutamic acid). Since the micelles were capable of delivering drugs with a low water solubility, such as PTX, at clinically appropriate concentrations, they could be used as drug-loaded nanocarriers. They were then electrospun onto NFs scaffolds composed of (poly(L-lactide-co-caprolactone) (PLCL):fibrinogen; 2:1 (w/w)).
Yang et al. suggested coaxial electrospinning to incorporate DOX into the PCL-PEG copolymer. Following their incorporation into a PVA solution dissolved in distilled water, the micelles were functionalized with folic acid targeting the tumour cells directly. The outer shell layer of the NFs is made of cross-linked gelatin. The drug release findings aided to conclude that the implantable system significantly decreased the dosage of the chemotherapeutic drug, the frequency with which it was administered, and its side effects while remaining highly effective against solid tumours.
Curcumin and neem have also been loaded, through electrospinning, into nanofibers containing polycaprolactone (PCL) [101]. After 72 h of treatment with dual drug system, enhanced anticancer activity against A431 cancer cells with no registry of toxicity to HaCaT skin cells [101].
The PCL nanofibers were also filled with the imiquimod anticancer medication drug in one of these experiments, which resulted in two main findings: sustained, continued in vitro drug release and 50% decrease in melanoma cell viability. It was therefore concluded that nanofibers filled with imiquimod are possible and ideal for treatment of melanomas and basal-cell carcinomas [102, 103].
The antibiotic doxycycline was electrospun into PCL/gelatin nanofibers and this hybrid nanocomposite also contained hydroxyapatite nanoparticles. On comparing it with 4T1 and CACO-2 cancer cell lines, the matrix of nanofibres demonstrated the greatest antitumour activity against the A431 epidermoid carcinoma cell line. Thus, it was concluded that nanofibers are feasible and appropriate for treating skin cancer [104].
PCL and Chitosan were also combined to form core/shell electrospun nanofibers with a core of 5-fluorouracil (5-FU) and PVP. This system of fabricated nanofibers exhibited remarkable properties, including high mechanical power, high drug encapsulation ability, and inhibitory activity against the melanoma cell line- B16F10, as indicated by a rise in the number of early apoptotic cells [105].
Additionally, PCL nanofibers have been used to treat skin cancer using molybdenum (MOL) nanoparticles [106]. Molybdenum has been shown to be important in shielding the skin from cancer [107]. The findings demonstrated that Mo-loaded nanofibers significantly decreased the viability of cancer cells in the in vivo skin cancer model induced in zebra fish. Covering tumour sites with PCL-Mo resulted in a substantial reduction in cancer development, rehabilitating them for delivery of the drug [106, 107].
Wang et al. demonstrated that membranes built from electrospinning bifunctional PCL nanofiber composites containing uniformly distributed Cu2S nanoparticles as a localized photothermal agent, responded well to NIR irradiation. This increased the death rate of A375 and B16F10 skin cancer cells in vitro and in vivo, establishing it as a photothermal sensitive anticancer platform [108, 109].
Copper silicate hollow microspheres (CSO HMSs) were synthesized in conjunction with SiO2 as a sacrificing template for the synthesis of a novel dual purpose scaffold.
Additionally, after hydrothermally loading trametinib (Tra) into these hollow microspheres, they were electrospun into a PCL/PLA (PP) matrix, forming Tra-CSO-PP scaffolds. These nanofiber composites exhibited excellent photothermal properties, enhancing the in vitro and in vivo synergistic therapeutic activity against skin cancer [109, 110].
Natural polymers
Chitosan
Chitosan (CS) is one of the most researched natural polymers for drug delivery, tissue engineering, and various other medical applications due to its well-established anticancer properties [64, 110, 111]. The only disadvantage of Chitosan is that it does not provide continuous release for an extended period of time, as Chitosan is hydrophilic and its swelling behaviour permits for fast drug diffusion from fibres. Additionally, it is well recognized that Chitosan cannot be easily electrospun without the assistance of supporting polymers, like PVA or PEO, majority of which are hydrophilic. As a result, achieving sustained anticancer drug release for an extended period of time (weeks) is comparatively difficult.
Ma et al. [112] electrospun nanofibers which were highly porous, using a mixture of CS and PEO. Its porous nature was achieved by removing PEO from fibrous material through a post-spinning water treatment. Rather than having the drug incorporated into the spinning solution, he soaked the porous Chitosan nanofibers in paclitaxel solution and then cross-linked them with hyaluronic acid (HA) solution. Initially, they demonstrated a rapid burst release accompanied by a sustained release after 48 h of incubation. These nanofibers have been shown to inhibit cell growth in DU145 prostate cancer cells, HeLa breast cancer cell lines, and myeloid cells [38, 39].
Ardeshirzadeh et al.[113] loaded fibres made by electrospinning CS/PEO/graphene oxide (GO) with DOX to inhibit A549 cell growth in vitro for 72 h. Though he recognized that the CS/PEO/GO electrospun fibres were less effective than CS/PEO drug-loaded fibres due to an interaction between DOX and GO. Finally, the electrospun fibres composed of CS/PEO/GO demonstrated pH-dependent drug release and a sustained release at pH 7.4.
Li et al. [91, 114] studied a dual drug delivery strategy involving the use of two different medications, 5-FU and paenolum. 5-fluorouracil is a hydrophilic chemotherapeutic agent that is primarily used to treat colon cancer, while paenolum is a hydrophobic molecule with anti-inflammatory properties that is used to prevent blood platelet clotting. The vesicles were synthesized by combining three surfactants: didodecyldimethylammonium bromide, cetyl trimethyl ammonium bromide (CTAB), and sodium dodecyl benzene sulfonate (SDBS). He then encapsulated these vesicles in nanocapsules produced by electrospinning a mixture of chitosan and sodium alginate. The chemotherapeutic drug was combined with vesicle formation and UV–visible spectroscopy. Its drug release exhibited a wide range of variability depending on the release rate and pH [91, 114].
Additionally, Hu et al. [115] produced colloidal structures for dual drug delivery using a block copolymer composed of methoxypoly(ethylene glycol)-block-poly(ethylene glycol) (L-lactide). He introduced two drugs: 5-FU, a water-soluble chemotherapeutic agent, and cefradine, a lipophilic antibiotic active against Gram-positive bacteria. A mixture of PEO and chitosan was infused into the external layer of the NFs, along with the drugs loaded through blend electrospinning. Without micelles, the NFs were uniform and smooth, but after micelles were added, the surface of the NFs became relatively rough, with diameters ranging from 200 to 800 nm. Additionally, some black spheres were observed having diameters of approximately 150 nm. After three days of incubation, it was discovered that this device could significantly cause reduction in the activity of HepG-2 cells while maintaining cell viability.
Radmansouri et al. [116] used nanofibers loaded with DOX hydrochloride electrospun from chitosan/cobalt ferrite/titanium oxide to concurrently treat melanoma cells (B16F10) with hyperthermia and chemotherapy. To modulate the temperature rise, the nanofibers made of chitosan are merged with titanium oxide and cobalt ferrite nanoparticles. By combining hyperthermia and chemotherapy, a synergistic effect was achieved, resulting in increased cell death with less side effects.
During the hyperthermic therapy, Fe3O4 nanoparticles have additionally been deposited with Fe+2/Fe+3 on the surface of electrospun Chitosan nanofibers. As a result of the heat produced by the magnetic composite nanofibers under the influence of an oscillating magnetic field, cancer cell proliferation was inhibited [117].
Electrospun tripolyphosphate cross-linked adenovirus/chitosan–PEG nanocomplexes were developed [118] for large-scale targeted cancer gene therapy. Although electrospinning or cross-linking with tripolyphosphate, there was no reduction in the biological activity or infectivity of adenovirus. The nanocomposite size (140 nm) was determined to be ideal for cellular absorption, and the zero potential was also determined to be positive due to the chitosan coating of the adenovirus. Due to the PEG surface conjugation, the liver absorption of Adenovirus was reduced, and the prolonged blood bioavailability was controlled. Thus, electrospun Ad/chitosan–PEG–FA nanocomposites are optimal for treating metastatic tumours while minimizing liver uptake.
Peptides
Peptides are naturally occurring short chain amino acid monomers that are connected by amide bonds. Zhang et al. built a three-dimensional scaffold made of peptide nanofibers- RADA16-I for screening anticancer drugs. These nanofibres provided an excellent site for three distinct ovarian cancer cell lines: embryonic kidney cells- 293 T, liver carcinoma cells- HepG2, and breast cancer cells-MCF-7. He had difficulties administering these medications orally due to the stomach's acidic pH [65]. Thus, the targeted delivery of nanofibers loaded with curcumin with arginine–glycine–aspartic acid motif showed good results since the drug is successfully targeted to a specific location.
Yang et al. [119] also concluded that the in vivo and in vitro stabilities of D- and L-peptide nanofibers were different in mice, resulting in altered biodistribution. Collagen peptide was used as a chemosensitivity model for gastric cancer. Choi synthesized three-dimensional electrospun scaffolds from poly(3-hydroxybutyrate-co-3-hydroxyvalerate) and used a higher concentration of anticancer drugs during the three-dimensional processing. This was done in order to achieve significant cytotoxic effects.
Additionally, polyhydroxybutyrate-co-valerate (PHBV) and collagen peptide (CP) were used to shape nanofibers containing five different anticancer drugs. This mechanism was used to assess the presence of three-dimensional tumours in gastric MKN28 cancer cells. The size of drug-loaded nanofibers was seen to decrease to 270 nm on increasing the concentration of CP, compared to the size of pure nanofibers, which were 520 nm. The size of the nanofibers was reduced because the solution's viscosity was inversely proportional to the concentration of CP. Additionally, a 7:3 molecular mass ratio of PHBV and collagen peptide (CP) was stated to exhibit substantial proliferation when compared to other mass ratios.
Conclusion
Although the present existing techniques for treating cancer cells using nanofibers are very advantageous compared to traditional chemotherapy, the major downside is the harmful solvents that may interfere with the drug, destroying the aim, for which they have been chosen. The solvent residue, if entrapped, will cause harm to the body (through normal cell damage). The water-soluble polymer is a benefit, but it also has the major problem about the burst release of the captured drug due to the hydrophilicity of these polymers [39, 120]. The burst release problem can be resolved by chemical/physical interlinking but due to the gradual breakdown of these polymers the release time of drugs cannot be compared with hydrophobic polymers. A mixed approach of incorporating hydrophobic and hydrophilic medication in one system can be used to target many kinds of cancer cells from one kind of drug-laden nanofibres. These nanofibers will also be promising candidates for successful cancer therapy with less side effects and greater effectiveness [113, 121].
However, the targeted drug distribution through oral supply of nanofibers is a problem, as its main application in local areas is limited by a larger volume of the drug. In addition, treating nanofibre-based metastatic carcinogens is an issue as those fibres are unable to travel easily as nanoparticles in the bloodstream [101, 114, 122].
The transition of these nanofibers from laboratory to clinic remains an important task, since most experiments are still conducted exclusively in pre-clinical trials. The challenge is that vast volumes of these nanofibers would have to be reproduced in addition to various formulations and approvals before eventually reaching the market. The outcomes of clinical trials are significant before commercializing these nanofibers, since no performance or result particularly good in vitro can also be performed similarly in the in vivo or complex biological environments [91, 114, 123].
Nanotechnology has brought research to new horizons each day as targeted and sustained drug release is a favourable technique for these nanocarriers. In comparison to free drugs nanofibres have survived drug release and thus better perform against different kinds of cancer cells.
In deciding the best combination for continuous drug delivery, the choice of drugs and polymer is very critical [124]. At this phase, although the nanofibers are advantageous in the delivery of cancer drugs, commercial products are not successfully launched. Study on organic and inorganic drugs alone or in conjunction may be further investigated to improve the effectiveness of the mechanism of the system to launch these nanofibers in the market for the successful treatment of cancer.
Abbreviations
- NFs:
-
Nanofibers
References
Pillay V, Dott C, Choonara YE et al (2013) A review of the effect of processing variables on the fabrication of electrospun nanofibers for drug delivery applications. J Nanomater. https://doi.org/10.1155/2013/789289
Doshi J, Reneker DH (1995) Electrospinning process and applications of electrospun fibers. J Electrostat 35:151–160. https://doi.org/10.1016/0304-3886(95)00041-8
MacDiarmid AG, Jones WE, Norris ID et al (2001) Electrostatically-generated nanofibers of electronic polymers. Synth Met 119:27–30. https://doi.org/10.1016/S0379-6779(00)00597-X
Reneker DH, Chun I (1996) Nanometre diameter fibres of polymer, produced by electrospinning. Nanotechnology 7:216. https://doi.org/10.1088/0957-4484/7/3/009
Yu J, Qiu Y, Zha X et al (2008) Macromolecular nanotechnology production of aligned helical polymer nanofibers by electrospinning 9:2838–2844. https://doi.org/10.1016/j.eurpolymj.2008.05.020
Kessick R, Tepper G (2004) Microscale polymeric helical structures produced by electrospinning. Appl Phys Lett 84:1182. https://doi.org/10.1063/1.1762704
Bretcanu O, Misra SK, Yunos DM et al (2009) Electrospun nanofibrous biodegradable polyester coatings on Bioglass®-based glass-ceramics for tissue engineering. Mater Chem Phys 118:420–426. https://doi.org/10.1016/j.matchemphys.2009.08.011
Taylor GI (1969) Electrically driven jets. In: Proceedings of the Royal Society of London. A mathematical and physical sciences, vol 313, pp 453–475. https://doi.org/10.1098/RSPA.1969.0205
Cloupeau M, Prunet-Foch B (1990) Electrostatic spraying of liquids: main functioning modes. J Electrostat 25:165–184. https://doi.org/10.1016/0304-3886(90)90025-Q
Grace JM, Marijnissen JCM (1994) A review of liquid atomization by electrical means. J Aerosol Sci 25:1005–1019. https://doi.org/10.1016/0021-8502(94)90198-8
Yarin AL, Koombhongse S, Reneker DH (2001) Bending instability in electrospinning of nanofibers. J Appl Phys 89:3018. https://doi.org/10.1063/1.1333035
Deitzel JM, Kleinmeyer J, Harris D, Beck Tan NC (2001) The effect of processing variables on the morphology of electrospun nanofibers and textiles. Polymer 42:261–272. https://doi.org/10.1016/S0032-3861(00)00250-0
Haider S, Al-Zeghayer Y, Ahmed Ali FA et al (2013) Highly aligned narrow diameter chitosan electrospun nanofibers. J Polym Res. https://doi.org/10.1007/S10965-013-0105-9
Bae HS, Haider A, Selim KMK et al (2013) Fabrication of highly porous PMMA electrospun fibers and their application in the removal of phenol and iodine. J Polym Res. https://doi.org/10.1007/S10965-013-0158-9
Frenot A, Chronakis IS (2003) Polymer nanofibers assembled by electrospinning. Curr Opinion Colloid Interface Sci 8:64–75. https://doi.org/10.1016/S1359-0294(03)00004-9
Huang ZM, Zhang YZ, Kotaki M, Ramakrishna S (2003) A review on polymer nanofibers by electrospinning and their applications in nanocomposites. Compos Sci Technol 63:2223–2253. https://doi.org/10.1016/S0266-3538(03)00178-7
Ryu YJ, Kim HY, Lee KH et al (2003) Transport properties of electrospun nylon 6 nonwoven mats. Eur Polym J 39:1883–1889. https://doi.org/10.1016/S0014-3057(03)00096-X
Li D, Wang Y, Xia Y (2003) Electrospinning of polymeric and ceramic nanofibers as uniaxially aligned arrays. Nano Lett 3:1167–1171. https://doi.org/10.1021/NL0344256
Khajavi R, Abbasipour M (2012) Electrospinning as a versatile method for fabricating coreshell, hollow and porous nanofibers. Sci Iran 19:2029–2034. https://doi.org/10.1016/J.SCIENT.2012.10.037
Chen Z, Foster MD, Zhou W et al (2001) Structure of poly(ferrocenyldimethylsilane) in electrospun nanofibers. Macromolecules 34:6156–6158. https://doi.org/10.1021/MA991857N
Jaeger R, Scho H, Vancso GJ (1996) Chain packing in electro-spun poly(ethylene oxide) visualized by atomic force microscopy
Pedicini A, Farris RJ (2003) Mechanical behavior of electrospun polyurethane. Polymer 44:6857–6862. https://doi.org/10.1016/J.POLYMER.2003.08.040
Yount WC, Loveless DM, Craig SL (2005) Small-molecule dynamics and mechanisms underlying the macroscopic mechanical properties of coordinatively cross-linked polymer networks. J Am Chem Soc 127:14488–14496. https://doi.org/10.1021/JA054298A/SUPPL_FILE/JA054298ASI20050820_022128.PDF
Luo X, Xie C, Wang H et al (2012) Antitumor activities of emulsion electrospun fibers with core loading of hydroxycamptothecin via intratumoral implantation. Int J Pharm 425:19–28. https://doi.org/10.1016/J.IJPHARM.2012.01.012
Cheng S, Du Y, Ma B, Tan D (2009) Total synthesis of a furostan saponin, timosaponin BII. Org Biomol Chem 7:3112–3118. https://doi.org/10.1039/B905091D
Weinberg BD, Blanco E, Gao J (2008) Polymer implants for intratumoral drug delivery and cancer therapy. J Pharm Sci 97:1681–1702. https://doi.org/10.1002/JPS.21038
Long-circulating and target-specific nanoparticles: theory to practice-PubMed. https://pubmed.ncbi.nlm.nih.gov/11356986/. Accessed 25 Dec 2021
Moghimi S, Hunter AC, Murray JC (2001) Long-circulating and target-specific nanoparticles: theory to practice. Pharmacol Rev 53(2):283–318
Lasprilla AJR, Martinez GAR, Lunelli BH et al (2012) Poly-lactic acid synthesis for application in biomedical devices—a review. Biotechnol Adv 30:321–328. https://doi.org/10.1016/J.BIOTECHADV.2011.06.019
Rancan F, Papakostas D, Hadam S et al (2009) Investigation of polylactic acid (PLA) nanoparticles as drug delivery systems for local dermatotherapy. Pharm Res 26:2027–2036. https://doi.org/10.1007/S11095-009-9919-X
EY Gómez-Pachón, R Vera-Graziano, RM Campos 2014 Structure of poly(lactic-acid) PLA nanofibers scaffolds prepared by electrospinning. IOP conference series: materials science and engineering. Vol 59, p 012003 https://doi.org/10.1088/1757-899X/59/1/012003
Zeng J, Yang L, Liang Q et al (2005) Influence of the drug compatibility with polymer solution on the release kinetics of electrospun fiber formulation. J Controll Release 105:43–51. https://doi.org/10.1016/J.JCONREL.2005.02.024
Thangaraju E, Srinivasan NT, Kumar R et al (2012) Fabrication of electrospun poly l-lactide and curcumin loaded poly l-lactide nanofibers for drug delivery. Fibers Polym 13(7):823–830. https://doi.org/10.1007/S12221-012-0823-3
Xu X, Chen X, Xu X et al (2006) BCNU-loaded PEG-PLLA ultrafine fibers and their in vitro antitumor activity against Glioma C6 cells. J Controll Release 114:307–316. https://doi.org/10.1016/J.JCONREL.2006.05.031
Chen P, Wu QS, Ding YP et al (2010) A controlled release system of titanocene dichloride by electrospun fiber and its antitumor activity in vitro. Eur J Pharm Biopharm 76:413–420. https://doi.org/10.1016/J.EJPB.2010.09.005
Zhang Z, Liu S, Qi Y et al (2016) Time-programmed DCA and oxaliplatin release by multilayered nanofiber mats in prevention of local cancer recurrence following surgery. J Controll Release 235:125–133. https://doi.org/10.1016/J.JCONREL.2016.05.046
Qiu K, He C, Feng W et al (2013) Doxorubicin-loaded electrospun poly(l-lactic acid)/mesoporous silica nanoparticles composite nanofibers for potential postsurgical cancer treatment. J Mater Chem B 1:4601–4611. https://doi.org/10.1039/C3TB20636J
Ignatova MG, Manolova NE, Toshkova RA et al (2010) Electrospun nanofibrous mats containing quaternized chitosan and polylactide with in vitro antitumor activity against HeLa cells. Biomacromol 11:1633–1645. https://doi.org/10.1021/BM100285N
Ignatova M, Yossifova L, Gardeva E et al (2011) Antiproliferative activity of nanofibers containing quaternized chitosan and/or doxorubicin against MCF-7 human breast carcinoma cell line by apoptosis. J Bioact Compat Polym 26:539–551. https://doi.org/10.1177/0883911511424655
Toshkova R, Manolova N, Gardeva E et al (2010) Antitumor activity of quaternized chitosan-based electrospun implants against Graffi myeloid tumor. Int J Pharm 400:221–233. https://doi.org/10.1016/J.IJPHARM.2010.08.039
Hasegawa M, Yagi K, Iwakawa S, Hirai M (2001) Chitosan induces apoptosis via caspase-3 activation in bladder tumor cells. Jpn J Cancer Res 92:459–466. https://doi.org/10.1111/J.1349-7006.2001.TB01116.X
Lv G, He F, Wang X et al (2008) Novel nanocomposite of nano Fe3O4 and polylactide nanofibers for application in drug uptake and induction of cell death of leukemia cancer cells. Langmuir 24:2151–2156. https://doi.org/10.1021/LA702845S
Xu X, Chen X, Ma P et al (2008) The release behavior of doxorubicin hydrochloride from medicated fibers prepared by emulsion-electrospinning. Eur J Pharm Biopharm 70:165–170. https://doi.org/10.1016/J.EJPB.2008.03.010
Zhang H, Niu Q, Wang N et al (2015) Thermo-sensitive drug controlled release PLA core/PNIPAM shell fibers fabricated using a combination of electrospinning and UV photo-polymerization. Eur Polym J 71:440–450. https://doi.org/10.1016/J.EURPOLYMJ.2015.08.023
Xie J, Liu W, Macewan MR et al (2014) Neurite outgrowth on electrospun nanofibers with uniaxial alignment: the effects of fiber density, surface coating, and supporting substrate. ACS Nano 8:1878–1885. https://doi.org/10.1021/NN406363J/SUPPL_FILE/NN406363J_SI_003.PDF
Bagó JR, Pegna GJ, Okolie O et al (2016) Electrospun nanofibrous scaffolds increase the efficacy of stem cell-mediated therapy of surgically resected glioblastoma. Biomaterials 90:116–125. https://doi.org/10.1016/j.biomaterials.2016.03.008
Electrospun fibers of poly(l‐lactic acid) containing lovastatin with potential applications in drug delivery. https://en.x-mol.com/paper/article/1234178612260786176. Accessed 25 Dec 2021
Zhu Y, Pyda M, Cebe P (2017) Electrospun fibers of poly(l-lactic acid) containing lovastatin with potential applications in drug delivery. J Appl Polym Sci. https://doi.org/10.1002/APP.45287
Zhang Z, Liu S, Xiong H et al (2015) Electrospun PLA/MWCNTs composite nanofibers for combined chemo—and photothermal therapy. Acta Biomater 26:115–123. https://doi.org/10.1016/J.ACTBIO.2015.08.003
Zhao X, Yuan Z, Yildirimer L et al (2015) Tumor-triggered controlled drug release from electrospun fibers using inorganic caps for inhibiting cancer relapse. Small 11:4284–4291. https://doi.org/10.1002/SMLL.201500985
Xu X, Chen X, Wang Z, Jing X (2009) Ultrafine PEG-PLA fibers loaded with both paclitaxel and doxorubicin hydrochloride and their in vitro cytotoxicity. Eur J Pharm Biopharm 72:18–25. https://doi.org/10.1016/J.EJPB.2008.10.015
Xie J, Wang CH (2006) Electrospun micro—and nanofibers for sustained delivery of paclitaxel to treat C6 Glioma in vitro. Pharm Res 23:1817–1826. https://doi.org/10.1007/S11095-006-9036-Z
Kim K, Luu YK, Chang C et al (2004) Incorporation and controlled release of a hydrophilic antibiotic using poly(lactide-co-glycolide)-based electrospun nanofibrous scaffolds. J Controll Release 98:47–56. https://doi.org/10.1016/J.JCONREL.2004.04.009
Ranganath SH, Fu Y, Arifin DY et al (2010) The use of submicron/nanoscale PLGA implants to deliver paclitaxel with enhanced pharmacokinetics and therapeutic efficacy in intracranial glioblastoma in mice. Biomaterials 31:5199–5207. https://doi.org/10.1016/J.BIOMATERIALS.2010.03.002
Chen Y, Wei J, Hu J et al (2014) Multiple drug-loaded electrospun PLGA/gelatin composite nanofibers encapsulated with mesoporous ZnO nanospheres for potential postsurgical cancer treatment. RSC Adv 4:28011–28019. https://doi.org/10.1039/C4RA03722G
Vashisth P, Kumar N, Sharma M, Pruthi V (2015) Biomedical applications of ferulic acid encapsulated electrospun nanofibers. Biotechnol Rep (Amst) 8:36–44. https://doi.org/10.1016/J.BTRE.2015.08.008
Mehrasa M, Asadollahi MA, Nasri-Nasrabadi B et al (2016) Incorporation of mesoporous silica nanoparticles into random electrospun PLGA and PLGA/gelatin nanofibrous scaffolds enhances mechanical and cell proliferation properties. Mater Sci Eng C Mater Biol Appl 66:25–32. https://doi.org/10.1016/J.MSEC.2016.04.031
Mehrasa M, Asadollahi MA, Ghaedi K et al (2015) Electrospun aligned PLGA and PLGA/gelatin nanofibers embedded with silica nanoparticles for tissue engineering. Int J Biol Macromol 79:687–695. https://doi.org/10.1016/J.IJBIOMAC.2015.05.050
Qi RL, Tian XJ, Guo R et al (2016) Controlled release of doxorubicin from electrospun MWCNTs/PLGA hybrid nanofibers. Chin J Polym Sci 34(9):1047–1059. https://doi.org/10.1007/S10118-016-1827-Z
Sasikala ARK, Unnithan AR, Yun YH et al (2016) An implantable smart magnetic nanofiber device for endoscopic hyperthermia treatment and tumor-triggered controlled drug release. Acta Biomater 31:122–133. https://doi.org/10.1016/J.ACTBIO.2015.12.015
Lei C, Cui Y, Zheng L et al (2013) Development of a gene/drug dual delivery system for brain tumor therapy: potent inhibition via RNA interference and synergistic effects. Biomaterials 34:7483–7494. https://doi.org/10.1016/J.BIOMATERIALS.2013.06.010
Chen S, Boda SK, Batra SK et al (2018) Emerging roles of electrospun nanofibers in cancer research. Adv Healthcare Mater 7:e1701024. https://doi.org/10.1002/ADHM.201701024
Natu MV, de Sousa HC, Gil MH (2010) Effects of drug solubility, state and loading on controlled release in bicomponent electrospun fibers. Int J Pharm 397:50–58. https://doi.org/10.1016/J.IJPHARM.2010.06.045
Khor E, Lim LY (2003) Implantable applications of chitin and chitosan. Biomaterials 24:2339–2349. https://doi.org/10.1016/S0142-9612(03)00026-7
Liu X, Lin T, Gao Y et al (2012) Antimicrobial electrospun nanofibers of cellulose acetate and polyester urethane composite for wound dressing. J Biomed Mater Res B Appl Biomater 100:1556–1565. https://doi.org/10.1002/JBM.B.32724
Fischer S, Thümmler K, Volkert B et al (2008) Properties and applications of cellulose acetate. Macromol Symp 262:89–96. https://doi.org/10.1002/MASY.200850210
Assessment UENC for E (2009) Electrospun cellulose acetate fiber mats containing curcumin and release characteristic of the herbal substance
Akaraonye E, Keshavarz T, Roy I (2010) Production of polyhydroxyalkanoates: the future green materials of choice. J Chem Technol Biotechnol 85:732–743. https://doi.org/10.1002/JCTB.2392
(PDF) Polyhydroxyalkanoates: bio-based microbial plastics and their properties. https://www.researchgate.net/publication/228650294_Polyhydroxyalkanoates_Bio-based_microbial_plastics_and_their_properties. Accessed 26 Dec 2021
Peng SW, Guo XY, Shang GG et al (2011) An assessment of the risks of carcinogenicity associated with polyhydroxyalkanoates through an analysis of DNA aneuploid and telomerase activity. Biomaterials 32:2546–2555. https://doi.org/10.1016/J.BIOMATERIALS.2010.12.051
Mottina AC, Ayres E, Orefice RL, Câmara JJD (2016) What changes in Poly(3-Hydroxybutyrate) (PHB) when processed as electrospun nanofibers or thermo-compression molded film? Mater Res 19:57–66. https://doi.org/10.1590/1980-5373-MR-2015-0280
O’Connor S, Szwej E, Nikodinovic-Runic J et al (2013) The anti-cancer activity of a cationic anti-microbial peptide derived from monomers of polyhydroxyalkanoate. Biomaterials 34:2710–2718. https://doi.org/10.1016/j.biomaterials.2012.12.032
Huang C, Soenen SJ, Rejman J et al (2012) Magnetic electrospun fibers for cancer therapy. Adv Func Mater 22:2479–2486. https://doi.org/10.1002/ADFM.201102171
Song M, Guo D, Pan C et al (2008) The application of poly(N-isopropylacrylamide)-co-polystyrene nanofibers as an additive agent to facilitate the cellular uptake of an anticancer drug. Nanotechnology. https://doi.org/10.1088/0957-4484/19/16/165102
Elsner JJ, Zilberman M (2010) Novel antibiotic-eluting wound dressings: an in vitro study and engineering aspects in the dressing’s design. J Tissue Viability 19:54–66. https://doi.org/10.1016/J.JTV.2009.11.001
Han SW, Koh WG (2016) Hydrogel-framed nanofiber matrix integrated with a microfluidic device for fluorescence detection of matrix metalloproteinases-9. Anal Chem 88:6247–6253. https://doi.org/10.1021/ACS.ANALCHEM.5B04867
Abid S, Raza ZA, Rehman A (2016) Synthesis of poly(3-hydroxybutyrate) nanospheres and deposition thereof into porous thin film. Mater Res Express 3:105042. https://doi.org/10.1088/2053-1591/3/10/105042
Zhao Y, Fan Z, Shen M et al (2015) Hyaluronic acid-functionalized electrospun polyvinyl alcohol/polyethyleneimine nanofibers for cancer cell capture applications. Adv Mater Interfaces 2:1500256. https://doi.org/10.1002/admi.201500256
Fan ZY, Zhao YL, Zhu XY et al (2016) Folic acid modified electrospun poly(vinyl alcohol)/polyethyleneimine nanofibers for cancer cell capture applications. Chin J Polym Sci 34:755–765. https://doi.org/10.1007/S10118-016-1792-6
Kumar S, Rai P, Sharma JG et al (2016) PEDOT:PSS/PVA-nanofibers-decorated conducting paper for cancer diagnostics. Adv Mater Technol. https://doi.org/10.1002/ADMT.201600056
Dong J, Chen JF, Smalley M et al (2020) Nanostructured substrates for detection and characterization of circulating rare cells: from materials research to clinical applications. Adv Mater 32:e1903663. https://doi.org/10.1002/ADMA.201903663
Yang G, Wang J, Wang Y et al (2015) An implantable active-targeting micelle-in-nanofiber device for efficient and safe cancer therapy. ACS Nano 9:1161–1174. https://doi.org/10.1021/NN504573U
Barzegar F, Bello A, Fabiane M et al (2015) Preparation and characterization of poly(vinyl alcohol)/graphene nanofibers synthesized by electrospinning. J Phys Chem Solids 77:139–145. https://doi.org/10.1016/J.JPCS.2014.09.015
Wang C, Ma C, Wu Z et al (2015) Enhanced bioavailability and anticancer effect of curcumin-loaded electrospun nanofiber. in vitro and in vivo study. Nanoscale Res Lett 10:1–10. https://doi.org/10.1186/S11671-015-1146-2/FIGURES/8
Zhang N, Deng Y, Tai Q et al (2012) Electrospun TiO2 nanofiber-based cell capture assay for detecting circulating tumor cells from colorectal and gastric cancer patients. Adv Mater 24:2756–2760. https://doi.org/10.1002/ADMA.201200155
Munaweera I, Levesque-Bishop D, Shi Y et al (2014) Radiotherapeutic bandage based on electrospun polyacrylonitrile containing holmium-166 iron garnet nanoparticles for the treatment of skin cancer. ACS Appl Mater Interfaces 6:22250–22256. https://doi.org/10.1021/AM506045K
Jung HS, Kong WH, Sung DK et al (2014) Nanographene oxide-hyaluronic acid conjugate for photothermal ablation therapy of skin cancer. ACS Nano 8:260–268. https://doi.org/10.1021/NN405383A/SUPPL_FILE/NN405383A_SI_001.PDF
Gelain F, Unsworth LD, Zhang S (2010) Slow and sustained release of active cytokines from self-assembling peptide scaffolds. J Controll Release 145:231–239. https://doi.org/10.1016/J.JCONREL.2010.04.026
Sridhar R, Ravanan S, Venugopal JR et al (2014) Curcumin- and natural extract-loaded nanofibres for potential treatment of lung and breast cancer: in vitro efficacy evaluation. J Biomater Sci Polym Ed 25:985–998. https://doi.org/10.1080/09205063.2014.917039
Yohe ST, Herrera VLM, Colson YL, Grinstaff MW (2012) 3D superhydrophobic electrospun meshes as reinforcement materials for sustained local drug delivery against colorectal cancer cells. J Controll Release 162:92–101. https://doi.org/10.1016/J.JCONREL.2012.05.047
Yohe ST, Colson YL, Grinstaff MW (2012) Superhydrophobic materials for tunable drug release: using displacement of air to control delivery rates. J Am Chem Soc 134:2016–2019. https://doi.org/10.1021/JA211148A
Fu Y, Li X, Ren Z et al (2018) Multifunctional electrospun nanofibers for enhancing localized cancer treatment. Small 14:e1801183. https://doi.org/10.1002/SMLL.201801183
Shao S, Li L, Yang G et al (2011) Controlled green tea polyphenols release from electrospun PCL/MWCNTs composite nanofibers. Int J Pharm 421:310–320. https://doi.org/10.1016/J.IJPHARM.2011.09.033
Jiang J, Xie J, Ma B et al (2014) Mussel-inspired protein-mediated surface functionalization of electrospun nanofibers for pH-responsive drug delivery. Acta Biomater 10:1324–1332. https://doi.org/10.1016/J.ACTBIO.2013.11.012
Xue R, Behera P, Xu J et al (2014) Polydimethylsiloxane core-polycaprolactone shell nanofibers as biocompatible, real-time oxygen sensors. Sens Actuators B Chem 192:697. https://doi.org/10.1016/J.SNB.2013.10.084
Agudelo-Garcia PA, de Jesus JK, Williams SP et al (2011) Glioma cell migration on three-dimensional nanofiber scaffolds is regulated by substrate topography and abolished by inhibition of STAT3 signaling. Neoplasia 13:831–840. https://doi.org/10.1593/NEO.11612
Sims-Mourtada J, Niamat RA, Samuel S et al (2014) Enrichment of breast cancer stem-like cells by growth on electrospun polycaprolactone-chitosan nanofiber scaffolds. Int J Nanomed 9:995. https://doi.org/10.2147/IJN.S55720
Jain A, Betancur M, Patel GD et al (2014) Guiding intracortical brain tumour cells to an extracortical cytotoxic hydrogel using aligned polymeric nanofibres. Nat Mater 13:308–316. https://doi.org/10.1038/NMAT3878
Hartman O, Zhang C, Adams EL et al (2010) Biofunctionalization of electrospun PCL-based scaffolds with perlecan domain IV peptide to create a 3-D pharmacokinetic cancer model. Biomaterials 31:5700–5718. https://doi.org/10.1016/J.BIOMATERIALS.2010.03.017
Hesami P, Holzapfel BM, Taubenberger A et al (2014) A humanized tissue-engineered in vivo model to dissect interactions between human prostate cancer cells and human bone. Clin Exp Metas 31:435–446. https://doi.org/10.1007/S10585-014-9638-5
Ravanan S, Prema AA, Xavier RJ, Sahayaraj PA (2016) Anti-cancer activity (A431 cancer cells) and cytotoxic efficiency (HaCaT skin cells) of Curcumin/Neem loaded polycaprolactone (PCL) nanofibres. Der Pharma Chem 8:104–111
Lin WC, Yeh IT, Niyama E et al (2018) Electrospun poly (ε-caprolactone) nanofibrous mesh for imiquimod delivery in melanoma therapy. Polymers 10:231. https://doi.org/10.3390/POLYM10030231
Garrett R, Niiyama E, Kotsuchibashi Y et al (2015) Biodegradable nanofiber for delivery of immunomodulating agent in the treatment of basal cell carcinoma. Fibers 3:478–490. https://doi.org/10.3390/FIB3040478
Ramírez-Agudelo R, Scheuermann K, Gala-García A et al (2018) Hybrid nanofibers based on poly-caprolactone/gelatin/hydroxyapatite nanoparticles-loaded Doxycycline: Effective anti-tumoral and antibacterial activity. Mater Sci Eng C Mater Biol Appl 83:25–34. https://doi.org/10.1016/J.MSEC.2017.08.012
Zhu LF, Zheng Y, Fan J et al (2019) A novel core-shell nanofiber drug delivery system intended for the synergistic treatment of melanoma. Eur J Pharm Sci. https://doi.org/10.1016/J.EJPS.2019.105002
Janani I, Lakra R, Kiran MS, Korrapati PS (2018) Selectivity and sensitivity of molybdenum oxide-polycaprolactone nanofiber composites on skin cancer: Preliminary in-vitro and in-vivo implications. J Trace Elements Med Biol 49:60–71. https://doi.org/10.1016/J.JTEMB.2018.04.033
Nakadaira H, Endoh K, Yamamoto M, Katoh K (1995) Distribution of selenium and molybdenum and cancer mortality in Niigata, Japan. Arch Environ Health 50:374–380. https://doi.org/10.1080/00039896.1995.9935970
Xi Y, Ge J, Guo Y et al (2018) Biomimetic elastomeric polypeptide-based nanofibrous matrix for overcoming multidrug-resistant bacteria and enhancing full-thickness wound healing/skin regeneration. ACS Nano 12:10772–10784. https://doi.org/10.1021/ACSNANO.8B01152/SUPPL_FILE/NN8B01152_SI_001.PDF
Yu DG, Li XY, Wang X et al (2015) Nanofibers fabricated using triaxial electrospinning as zero order drug delivery systems. ACS Appl Mater Interfaces 7:18891–18897. https://doi.org/10.1021/ACSAMI.5B06007/SUPPL_FILE/AM5B06007_SI_001.PDF
Jayakumar R, Prabaharan M, Nair SV, Tamura H (2010) Novel chitin and chitosan nanofibers in biomedical applications. Biotechnol Adv 28:142–150. https://doi.org/10.1016/J.BIOTECHADV.2009.11.001
Ignatova M, Manolova N, Rashkov I (2007) Novel antibacterial fibers of quaternized chitosan and poly(vinyl pyrrolidone) prepared by electrospinning. Eur Polym J 43:1112–1122. https://doi.org/10.1016/J.EURPOLYMJ.2007.01.012
Ma G, Liu Y, Peng C et al (2011) Paclitaxel loaded electrospun porous nanofibers as mat potential application for chemotherapy against prostate cancer. Carbohyd Polym 86:505–512. https://doi.org/10.1016/J.CARBPOL.2011.04.082
Ardeshirzadeh B, Anaraki NA, Irani M et al (2015) Controlled release of doxorubicin from electrospun PEO/chitosan/graphene oxide nanocomposite nanofibrous scaffolds. Mater Sci Eng C Mater Biol Appl 48:384–390. https://doi.org/10.1016/J.MSEC.2014.12.039
Li W, Luo T, Yang Y et al (2015) Formation of controllable hydrophilic/hydrophobic drug delivery systems by electrospinning of vesicles. Langmuir 31:5141–5146. https://doi.org/10.1021/LA504796V
Achille C, Sundaresh S, Chu B, Hadjiargyrou M (2012) Cdk2 silencing via a DNA/PCL electrospun scaffold suppresses proliferation and increases death of breast cancer cells. PLoS ONE 7:e52356. https://doi.org/10.1371/JOURNAL.PONE.0052356
Radmansouri M, Bahmani E, Sarikhani E et al (2018) Doxorubicin hydrochloride—Loaded electrospun chitosan/cobalt ferrite/titanium oxide nanofibers for hyperthermic tumor cell treatment and controlled drug release. Int J Biol Macromol 116:378–384. https://doi.org/10.1016/J.IJBIOMAC.2018.04.161
Lin TC, Lin FH, Lin JC (2012) In vitro feasibility study of the use of a magnetic electrospun chitosan nanofiber composite for hyperthermia treatment of tumor cells. Acta Biomater 8:2704–2711. https://doi.org/10.1016/J.ACTBIO.2012.03.045
Park Y, Kang E, Kwon OJ et al (2010) Ionically crosslinked Ad/chitosan nanocomplexes processed by electrospinning for targeted cancer gene therapy. J Controll Release 148:75–82. https://doi.org/10.1016/J.JCONREL.2010.06.027
Yang C, Chu L, Zhang Y et al (2015) Dynamic biostability, biodistribution, and toxicity of L/D-peptide-based supramolecular nanofibers. ACS Appl Mater Interfaces 7:2735–2744. https://doi.org/10.1021/AM507800E
Krishnan R, Sundarrajan S, Ramakrishna S (2013) Green processing of nanofibers for regenerative medicine. Macromol Mater Eng 298:1034–1058. https://doi.org/10.1002/MAME.201200323
Poláková L, Širc J, Hobzová R et al (2019) Electrospun nanofibers for local anticancer therapy: review of in vivo activity. Int J Pharm 558:268–283. https://doi.org/10.1016/J.IJPHARM.2018.12.059
Tort S, Han D, Steckl AJ (2020) Self-inflating floating nanofiber membranes for controlled drug delivery. Int J Pharm 579:119164. https://doi.org/10.1016/J.IJPHARM.2020.119164
Garkal A, Kulkarni D, Musale S et al (2021) Electrospinning nanofiber technology: a multifaceted paradigm in biomedical applications. New J Chem 45:21508–21533. https://doi.org/10.1039/D1NJ04159B
Dziemidowicz K, Sang Q, Wu J et al (2021) Electrospinning for healthcare: recent advancements. J Mater Chem B 9:939–951. https://doi.org/10.1039/D0TB02124E
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Jagtiani, E., Sabnis, A.S. Recent advancements of electrospun nanofibers for cancer therapy. Polym. Bull. 80, 1215–1242 (2023). https://doi.org/10.1007/s00289-022-04153-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00289-022-04153-x