Abstract
Purpose
The repeated use of doxorubicin is limited due to dose-limiting cardiac toxicity. Pegylated liposomal doxorubicin (PEG-LD, Duomeisu) has a reduced cardiac toxicity. This phase I study aimed to investigate the maximum tolerated doses (MTDs) and dose-limiting toxicities (DLTs) of the PEG-LD and cisplatin combination in patients with metastatic and recurrent osteosarcoma.
Methods
Patients were given PEG-LD at a dose of 40, 50, or 60 mg/m2 on day 1 of each 21-day cycle, according to a 3 + 3 approach for dose escalation. Cisplatin was administered as a fixed dose of 100 mg/m2 for every cycle. Toxicities and tumor response were observed.
Results
A total of 15 patients were enrolled in this trial, and nine of the patients had received prior doxorubicin. The MTD of PEG-LD was reached at 50 mg/m2 in this regimen, with neutropenic fever and stomatitis as DTLs. The main adverse event (AE) was myelosuppression. The most common non-hematological AEs were vomiting, hypoproteinemia, stomatitis and transient sinus arrhythmia. Grade 3–4 toxicity was neutropenia, leukopenia, thrombocytopenia, anemia and stomatitis in the whole cohort. All the AEs were relieved after symptomatic and supportive treatment. Totally, the overall response rate was 13.3% and disease control rate was 66.7%. For the six patients who have not received prior doxorubicin, one partial response and five stable diseases were observed.
Conclusion
We provide the data showing that PEG-LD 50 mg/m2 combined with cisplatin 100 mg/m2 demonstrated an acceptable safety profile and promising clinical activity in advanced osteosarcoma, which merits further evaluation in phase II studies.
Trial registration
ChiCTR1900021550.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma is the most common primary malignant bone tumor in children and young adults, with a worldwide incidence of 3.4 per million people per year [1]. The addition of neo-adjuvant and adjuvant chemotherapy to surgery has improved the prognosis of patients with localized disease at presentation, leading to a cure rate of 50–70% [2]. Moreover, 90–95% of patients can be successfully treated with limb-sparing approaches rather than amputation with this mode of treatment [3]. However, 10–20% of patients present with distant metastatic disease at diagnosis [4], and survival rates continue to be unsatisfactory in the metastatic and relapse setting [5, 6]. The outcome for patients with metastatic and recurrent osteosarcoma has not been improved obviously in spite of the development of multi-agent chemotherapy regimens [7].
Doxorubicin combined with cisplatin is one of the most commonly recommended first-line chemotherapy regimens for osteosarcoma, which can achieve good histological response in 41% of patients and significantly improve survival [8]. In addition, doxorubicin is also active for patients with recurrent osteosarcoma [6, 9], who may have previously received the limit dose of doxorubicin in the neoadjuvant and adjuvant therapy stage. However, the repeated use of doxorubicin in metastatic and recurrent osteosarcoma is limited because of dose-limiting cardiac toxicity and poor tolerability beyond a few doses. Therefore, exploring alternative agents to overcome the dose limit of doxorubicin is of great significance for the treatment of osteosarcoma.
Studies have shown that encapsulation of doxorubicin by PEGylated liposomes (PEGylated liposomal doxorubicin; PEG-LD) improves the tissue distribution and pharmacokinetics of doxorubicin [10]. Replacement of doxorubicin with PEG-LD was reported to have a comparable efficacy but significantly reduce the cardiac toxicity in a variety of tumors [11,12,13]. In recent years, PEG-LD has been widely used in various tumors, such as breast cancer, ovarian cancer, multiple myeloma, and lymphoma [11, 12]. In osteosarcoma, whether PEG-LD can replace conventional doxorubicin to form a combined chemotherapy regimen, and what is the optimal dosage in patients, is currently rarely reported. A phase II trial by the EORTC Soft Tissue and Bone Sarcoma Group demonstrated that PEG-LD, which was administered at a dose of 50 mg/m2 every 4 weeks, had equivalent anti-tumor activity in patients advanced soft tissue sarcoma, with reduced toxicity compared with doxorubicin, which was given at a dose of 75 mg/m2 every 3 weeks [14]. Our previous study also found that PEG-LD 50 mg/m2 every 3 weeks can achieve similar good histological response as compared with doxorubicin 60–75 mg/m2 [15]. Therefore, PEG-LD 50 mg/m2 every 3 weeks was set as the effective reference dose, and PEG-LD 40 mg/m2 every 3 weeks was selected as the starting dose in this study.
This is the first phase I study to investigate the maximum tolerated dose (MTD) of PEG-LD when combined with cisplatin, to identify the toxicity profile and antitumor activity in Chinese patients with advanced osteosarcoma. This study will provide a basis for further randomized controlled clinical trials.
Patients and methods
Patients
Patients were eligible if they met the following criteria: (i) histologically confirmed high grade osteosarcoma; (ii) un-resectable newly diagnosed patients or metastatic and recurrent patients who have not received systemic therapy after tumor relapse; (iii) 14–65 years of age; (iv) Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0–1; (v) life expectancy at least 6 months; (vi) adequate bone marrow activity (white blood cell count > 3 × 109/L, absolute neutrophil count > 1.5 × 109/L, platelet count > 8 × 109/L, and hemoglobin level > 90 g/L), adequate hepatic function (serum total bilirubin level < 1.5 times the normal upper limit, transaminase < 2.5 times the normal upper limit), adequate renal function (serum creatinine level < 1.5 times the normal upper limit), and adequate cardiac function (left ventricular ejection fraction [LVEF] > 50%) by echocardiography; (viii) no severe complications, such as uncontrollable infections, congenital heart disease or pericardial disease, arrhythmia requiring drug intervention.
Patients with other malignancies, or were allergic to similar chemical composition were excluded from this study. Pregnancy or breastfeeding was not allowed in this study. Before the study, each patient signed a written informed consent. The study was approved by the Scientific and Ethics Committees of Sun Yat-sen University Cancer Center.
Study design
This was an open label, phase I study, with standard 3 + 3 dose-escalation design. Three escalating doses of PEG-LD (Duomeisu) were planned (40, 50, 60 mg/m2) with the fixed dose of cisplatin (100 mg/m2). At each dose level, three patients were scheduled to be included. At least three patients were observed for acute toxicity for a minimum of 3 weeks before doses were escalated to the next dose level. Three additional patients were scheduled for treatment at the same dose level if any of the predefined dose-limiting toxicities (DLTs) was observed in one of the initial three patients. Intra-patient dose escalation was not allowed. Each patient planned to receive 2 cycles of study treatment. The DLTs in this study were defined as follows: (i) grade 3 or grade 4 non-hematological toxicities except for nausea/vomiting, anorexia and general malaise; (ii) grade 4 neutropenia lasting greater than 5 days or febrile neutropenia; (iii) grade 4 thrombocytopenia lasting greater than 5 days; and (iv) failure to administer treatment within 14 days of the planned drug administration for next cycle due to delayed recovery of treatment-related toxicity to grade ≤ 1 or baseline. The patients who got a DLT were permitted to continue treatment at the lower dose level in the subsequent cycles. Only the toxicity of the first cycle was used to determine the DLT.
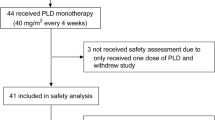
The MTD was defined as one dose level above which DLT was observed in two or more patients of the six patients following the first cycle of treatment. Six additional patients were added at the defined MTD to fully evaluate any toxicity at this level. Treatment schedule and dose-escalation levels are shown in Fig. 1.
Treatment and evaluation
PEG-LD (Duomeisu) was provided by CSPC Ouyi Pharmaceutical Co., Ltd. PEG-LD was administered as a 90-min intravenous (i.v.) infusion on day 1. Cisplatin was administered at 25 mg/m2/d on day 1–4. Prophylactic recombinant human granulocyte colony-stimulating factor (rhG-CSF) was administered subcutaneously (48 h after chemotherapy) at a dose of 150 ug/d for 5 days. The treatment was repeated every 3 weeks. Patients were monitored for toxicity in each cycle. Hematological toxicity was monitored with at least complete blood counts, differential counts twice a week, and, in case of grade 3–4 toxicity, daily counts until recovery. Blood chemistries as well as a detailed toxicity questionnaire and a physical examination were performed before each cycle. To detect potential cardiotoxicity, electrocardiograms (ECG) and markers of myocardial injury were performed before and after each cycle of chemotherapy. Cardiac function (left ventricular ejection fraction (LVEF) measurement) was monitored by echocardiogram at baseline and after the second cycle of treatment. Toxicities were graded according to the Common Terminology Criteria for Adverse Events (CTCAE) version 4.0.
Although the major thrust of a phase I study is to evaluate dose-ranging experience and the toxicity observed, an attempt was made to evaluate the efficacy of this drug combination in this patient population. Patients received CT or MRI examination at baseline and after 2 cycles of treatment. Tumor response was assessed according to the RECIST 1.1 criteria.
Statistical analysis
The primary objective of this trial was to define MTD of PEG-LD in combination with cisplatin, based on the DLTs observed during the first cycle of treatment. Secondary objective were to explore the antitumor activity, in terms of objective response rate, and to assess the safety profile of two cycles of combination therapy, especially cardiac toxicity. The MTD was considered to have been reached if two patients at the same dose level experienced DLTs. Toxicity in relationship to dose-escalation patterns was assessed through the use of descriptive statistics. Categorical variables were reported as the frequency ratio. Quantitative variables were represented by median values, as well as minimum and maximum values. Differences in demographic and clinical variables of two groups were tested using the Fisher’s exact test. A difference of 0.05 was considered significant in all analyses.
Results
Patient characteristics
Between December 2018 and November 2019, a total of 15 patients were enrolled into the study. Demographic and clinical characteristics of these patients are summarized in Table 1 and Supplementary table 1. There were five women and ten men and the median age was 20 years (ranging from 14 to 43). One patient at dose level 1 did not perform hematological assessment according to the protocol in the second cycle of the treatment. This patient was included in all analyses. Nine patients had received prior doxorubicin contained adjuvant chemotherapy and six patients were chemotherapy naïve. The tumors originated from the long bones of the lower limbs in nine patients. Two cases originated from upper limbs, and the other four from the trunk or skull. All the patients had metastatic tumors, 12 with lung metastases and 3 with lymph nodes metastases.
Treatment and toxicity
In the first cycle of the treatment, no evidence of hematological or non-hematological DLTs occurred in patients at dose level 1 or level 2. DLT was observed in two consecutive patients enrolled at dose level 3, both showing neutropenic fever accompanied by grade 3 stomatitis. Thus, the third patient was not included in this dose level. The MTD was reached at dose level 2 and a further 6 patients were enrolled to fully evaluate the possible toxicities. Of the additional six patients at dose level 2, one patient developed DLT (grade 4 thrombocytopenia lasting for 4 days). The treatment dose and the occurrence of DLTs are detailed in Table 2.
Treatment-related toxicity is summarized in Table 3. The main treatment-related toxicity was myelosuppression. Grade 3–4 hematological toxicity was neutropenia (11/15), leucopenia (9/15), thrombocytopenia (6/15) and anemia (2/15). There were two patients who experienced febrile neutropenia, both in PEG-LD 60 mg/m2 group. The nadir time to leukopenia and neutropenia was approximately 2 weeks after treatment initiation. All the nine patients receiving PEG-LD 50 mg/m2 experienced hematological toxicity, of which the grade 3 toxicity was leukopenia (4/9), neutropenia (4/9) and thrombocytopenia (1/9). In addition, two patients in PEG-LD 50 mg/m2 group experienced grade 4 neutropenia, one accompanied with grade 4 leukopenia and the other with grade 4 thrombocytopenia. Non-hematologic toxicity mainly included hypoproteinemia, nausea/vomiting, sinus arrhythmia and stomatitis. No hand-foot syndrome was observed in this study. One patient experienced infusion reaction manifested as dyspnea and facial flushing at the initiating phase of the first cycle of PEG-LD infusion, which was relieved after antihistamine and short-acting corticosteroid, and reinfused at a slower rate. The ECG follow-up 24 h after chemotherapy indicated that there were four patients with sinus arrhythmia without clinical symptoms, recovering in a short time. Treatment-related reduction in LVEF was not observed by echocardiography (Supplementary table 2). Except for two patients in the PLD 60 mg/m2 group who had grade 3 oral mucocitis, all the other non-hematological toxicities were mild and recovered quickly.
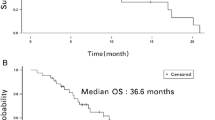
Response
After two cycles of treatment, all patients were evaluable for response (Table 4, Supplementary table 3). One partial response (PR) and one complete response (CR) have been observed at dose level 1. The CR case was observed in a patient who presented only two lung metastasis sites. The PR case was observed in a patient who was newly diagnosed as osteosarcoma of the right mandible, and whose tumor burden was shrank by 31.7% after two cycles of combination chemotherapy. At dose level 2, six of nine patients were stable disease (SD) as best response. Both patients at dose level 3 showed stable disease. The overall response rate and the disease control rate was 13.3% and 66.7%, respectively, for the whole cohort. All the six patients who had not been exposed to doxorubicin before enrollment showed clinical benefit (1 PR and 5 SD).
Discussion
Treatment of metastatic or recurrent osteosarcoma remains an important clinical challenge. Doxorubicin is an important therapeutic agent in this setting [6, 9], but cumulative dose-dependent myocardial damage associated with doxorubicin may result in life-threatening toxicity and entail often a significant dose compromise and even treatment interruption in responding patients. Thus, it is rational for the replacement of conventional doxorubicin with PEG-LD, which has a markedly different toxicity profile. Compared with conventional doxorubicin, PEG-LD has been demonstrated to have significantly less cardiac toxicity and a higher drug concentration in tumor tissues [12, 16, 17]. These features contribute to a better therapeutic index than with conventional doxorubicin, as demonstrated by a randomized phase III trial suggesting non-inferior efficacy with PEG-LD, with significantly reduced risk of cardiac toxicity [16]. The less cardiac toxicity was also confirmed by endomyocardial biopsies in patients treated with high cumulative doses of PEG-LD [17]. Moreover, PEG-LD was demonstrated to be well tolerated and active in patients pretreated with neoadjuvant or adjuvant anthracyclines [18, 19]. However, there is still a lack of research on the safety and efficacy of PEG-LD in osteosarcoma.
In this phase I study, we investigated the feasibility of combination chemotherapy with PEG-LD–cisplatin in advanced osteosarcoma patients. To our knowledge, this study is the first to evaluate the safety and efficacy of PEG-LD in osteosarcoma. We found that PEG-LD 50 mg/m2 and cisplatin 100 mg/m2 every 3 weeks with growth factor support represent the MTD as first-line treatment in un-resectable or recurrent osteosarcoma patients regardless of whether or not receiving prior doxorubicin. This combination showed clinical activity with manageable toxic effects. The main DLTs were a combination of stomatitis and febrile neutropenia, both of which appeared in PEG-LD 60 mg/m2 dose level. At the MDT dose level, nine patients were treated; only one patient developed DLT, which was grade 4 thrombocytopenia. More attention, the recommended MDT dose should be used carefully in the older patients since most patients included in this study are young with a median age of 20 years.
The most common reported treatment-related adverse events with PEG-LD were myelosuppression, palmar-plantar erythrodysesthesia (PPE) and stomatitis [20, 21]. The main toxicity of cisplatin is nephrotoxicity and vomiting. In the present study, a relatively higher rate of grade 3/4 neutropenia and thrombocytopenia was observed although granulocyte stimulating factors were used after chemotherapy. However, the time of recovering from severe neutropenia was relatively short and, in all cases, within 7 days. Nevertheless, we should pay more attention to the possibility of a synergistic myelosuppressive effect of PEG-LD combined with cisplatin. Three patients (3/15) developed treatment-related stomatitis, of which two cases were grade 3, both at PEG-LD 60 mg/m2 dose level, and the other one is mild at PEG-LD 50 mg/m2 dose level. This is similar to previous reports [21]. Some studies have also shown that the incidence and severity of mucositis are higher when the PEG-LD dose exceeds the level of 60 mg/m2 [22]. Conversely, no PPE was observed in the present study. This is probably due to the low cumulative doses of the drug administered and short observation time. It is reported that PPE mostly occurs after 2–3 cycles of medication [23]. Besides, an accelerated clearance of PEG-LD in patients receiving the cisplatin-PEG-LD combination was reported [21], which may be another explanation of the low incidence of PPE observed in this study. An important and encouraging observation of the present study was that many patients in this study were previously treated with conventional anthracycline, none of them developing significant cardiotoxicity, which suggests the fact that PEG-LD has lower cardiotoxicity. However, a longer follow-up time is needed to evaluate the cardiotoxicity exactly.
In this trial, clinical benefit was observed in the majority of the patients regardless of whether or not receiving prior doxorubicin. The efficacy of PEG-LD in osteosarcoma is rarely studied. The efficacy of PEG-LD (Doxil) 55 mg/m2 every 4 weeks in patients with sarcoma was evaluated in a phase II trial, which included six previously treated osteosarcomas [10]. Of them, two patients achieved a minor response for 3 months, and one had SD for 11 months [10]. Limited by the small sample size and the complexity of baseline conditions, the efficacy of this regimen in osteosarcoma needs to be further verified. Nevertheless, these results collectively indicate that PEG-LD is active in osteosarcoma patients.
In conclusion, this phase I dose-escalation trial provided the data showing that the PEG-LD–cisplatin combination is well tolerated in patients with osteosarcoma. The drugs could be combined safely at doses close to the recommended monotherapy dose. The antitumor activity and cumulative tolerance merit further evaluation in phase II and III clinical trials.
Availability of data and material
Data supporting the results reported in this study are not publicly available but are accessible from the corresponding author on reasonable request.
References
Mirabello L, Troisi RJ, Savage SA (2009) International osteosarcoma incidence patterns in children and adolescents, middle ages and elderly persons. Int J Cancer 125:229–234. https://doi.org/10.1002/ijc.24320
Bacci G, Briccoli A, Rocca M, Ferrari S, Donati D, Longhi A, Bertoni F, Bacchini P, Giacomini S, Forni C, Manfrini M, Galletti S (2003) Neoadjuvant chemotherapy for osteosarcoma of the extremities with metastases at presentation: recent experience at the Rizzoli Institute in 57 patients treated with cisplatin, doxorubicin, and a high dose of methotrexate and ifosfamide. Ann Oncol 14:1126–1134. https://doi.org/10.1093/annonc/mdg286
Nagarajan R, Neglia JP, Clohisy DR, Robison LL (2002) Limb salvage and amputation in survivors of pediatric lower-extremity bone tumors: what are the long-term implications? J Clin Oncol 20:4493–4501. https://doi.org/10.1200/JCO.2002.09.006
Meyers PA, Heller G, Healey JH, Huvos A, Applewhite A, Sun M, LaQuaglia M (1993) Osteogenic sarcoma with clinically detectable metastasis at initial presentation. J Clin Oncol 11:449–453. https://doi.org/10.1200/JCO.1993.11.3.449
Luetke A, Meyers PA, Lewis I, Juergens H (2014) Osteosarcoma treatment—where do we stand? A state of the art review. Cancer Treat Rev 40:523–532. https://doi.org/10.1016/j.ctrv.2013.11.006
Leary SE, Wozniak AW, Billups CA, Wu J, McPherson V, Neel MD, Rao BN, Daw NC (2013) Survival of pediatric patients after relapsed osteosarcoma: the St. Jude Children’s Research Hospital experience. Cancer 119:2645–2653. https://doi.org/10.1002/cncr.28111
Lagmay JP, Krailo MD, Dang H, Kim A, Hawkins DS, Beaty O 3rd, Widemann BC, Zwerdling T, Bomgaars L, Langevin AM, Grier HE, Weigel B, Blaney SM, Gorlick R, Janeway KA (2016) Outcome of patients with recurrent osteosarcoma enrolled in seven phase II trials through Children’s Cancer Group, Pediatric Oncology Group, and Children’s Oncology Group: learning from the past to move forward. J Clin Oncol 34:3031–3038. https://doi.org/10.1200/JCO.2015.65.5381
Bramwell VH, Burgers M, Sneath R, Souhami R, van Oosterom AT, Voute PA, Rouesse J, Spooner D, Craft AW, Somers R et al (1992) A comparison of two short intensive adjuvant chemotherapy regimens in operable osteosarcoma of limbs in children and young adults: the first study of the European Osteosarcoma Intergroup. J Clin Oncol 10:1579–1591. https://doi.org/10.1200/JCO.1992.10.10.1579
Huang YJ, He AN, Sun YJ, Shen Z, Min DL, Yao Y (2015) Continuous-infusion ifosfamide and doxorubicin combination as second-line chemotherapy for recurrent or refractory osteosarcoma patients in China: a retrospective study. Asian Pac J Cancer Prev 16:2391–2395. https://doi.org/10.7314/apjcp.2015.16.6.2391
Skubitz KM (2003) Phase II trial of pegylated-liposomal doxorubicin (Doxil) in sarcoma. Cancer Invest 21:167–176. https://doi.org/10.1081/cnv-120016412
Schmitt CJ, Dietrich S, Ho AD, Witzens-Harig M (2012) Replacement of conventional doxorubicin by pegylated liposomal doxorubicin is a safe and effective alternative in the treatment of non-Hodgkin’s lymphoma patients with cardiac risk factors. Ann Hematol 91:391–397. https://doi.org/10.1007/s00277-011-1308-y
Duggan ST, Keating GM (2011) Pegylated liposomal doxorubicin: a review of its use in metastatic breast cancer, ovarian cancer, multiple myeloma and AIDS-related Kaposi’s sarcoma. Drugs 71:2531–2558. https://doi.org/10.2165/11207510-000000000-00000
Ferrandina G, Corrado G, Licameli A, Lorusso D, Fuoco G, Pisconti S, Scambia G (2010) Pegylated liposomal doxorubicin in the management of ovarian cancer. Ther Clin Risk Manag 6:463–483. https://doi.org/10.2147/TCRM.S3348
Judson I, Radford JA, Harris M, Blay JY, van Hoesel Q, le Cesne A, van Oosterom AT, Clemons MJ, Kamby C, Hermans C, Whittaker J, Donato di Paola E, Verweij J, Nielsen S (2001) Randomised phase II trial of pegylated liposomal doxorubicin (DOXIL/CAELYX) versus doxorubicin in the treatment of advanced or metastatic soft tissue sarcoma: a study by the EORTC Soft Tissue and Bone Sarcoma Group. Eur J Cancer 37:870–877. https://doi.org/10.1016/s0959-8049(01)00050-8
Li Y, Huang Z, Shan HC, Xu HR, Sun Y, Niu XH (2019) Single-center, non-randomized controlled study of doxorubicin and doxorubicin in neoadjuvant chemotherapy for osteosarcoma. Chin J Cancer Prev Treat 26:1124–1128. https://doi.org/10.16073/j.cnki.cjcpt.2019.15.013
O’Brien ME, Wigler N, Inbar M, Rosso R, Grischke E, Santoro A, Catane R, Kieback DG, Tomczak P, Ackland SP, Orlandi F, Mellars L, Alland L, Tendler C, Group CBCS (2004) Reduced cardiotoxicity and comparable efficacy in a phase III trial of pegylated liposomal doxorubicin HCl (CAELYX/Doxil) versus conventional doxorubicin for first-line treatment of metastatic breast cancer. Ann Oncol 15:440–449. https://doi.org/10.1093/annonc/mdh097
Safra T, Muggia F, Jeffers S, Tsao-Wei DD, Groshen S, Lyass O, Henderson R, Berry G, Gabizon A (2000) Pegylated liposomal doxorubicin (doxil): reduced clinical cardiotoxicity in patients reaching or exceeding cumulative doses of 500 mg/m2. Ann Oncol 11:1029–1033. https://doi.org/10.1023/a:1008365716693
Al-Batran SE, Guntner M, Pauligk C, Scholz M, Chen R, Beiss B, Stopatschinskaja S, Lerbs W, Harbeck N, Jager E (2010) Anthracycline rechallenge using pegylated liposomal doxorubicin in patients with metastatic breast cancer: a pooled analysis using individual data from four prospective trials. Br J Cancer 103:1518–1523. https://doi.org/10.1038/sj.bjc.6605961
Sparano JA, Makhson AN, Semiglazov VF, Tjulandin SA, Balashova OI, Bondarenko IN, Bogdanova NV, Manikhas GM, Oliynychenko GP, Chatikhine VA, Zhuang SH, Xiu L, Yuan Z, Rackoff WR (2009) Pegylated liposomal doxorubicin plus docetaxel significantly improves time to progression without additive cardiotoxicity compared with docetaxel monotherapy in patients with advanced breast cancer previously treated with neoadjuvant-adjuvant anthracycline therapy: results from a randomized phase III study. J Clin Oncol 27:4522–4529. https://doi.org/10.1200/JCO.2008.20.5013
Ansari L, Shiehzadeh F, Taherzadeh Z, Nikoofal-Sahlabadi S, Momtazi-Borojeni AA, Sahebkar A, Eslami S (2017) The most prevalent side effects of pegylated liposomal doxorubicin monotherapy in women with metastatic breast cancer: a systematic review of clinical trials. Cancer Gene Ther 24:189–193. https://doi.org/10.1038/cgt.2017.9
Lyass O, Hubert A, Gabizon AA (2001) Phase I study of doxil-cisplatin combination chemotherapy in patients with advanced malignancies. Clin Cancer Res 7:3040–3046
Marina NM, Cochrane D, Harney E, Zomorodi K, Blaney S, Winick N, Bernstein M, Link MP (2002) Dose escalation and pharmacokinetics of pegylated liposomal doxorubicin (Doxil) in children with solid tumors: a pediatric oncology group study. Clin Cancer Res 8:413–418
Lyseng-Williamson KA, Duggan ST, Keating GM (2013) Pegylated liposomal doxorubicin: a guide to its use in various malignancies. BioDrugs 27:533–540. https://doi.org/10.1007/s40259-013-0070-1
Acknowledgements
We are grateful to our patients and their families for participating in this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
XZW, XHN and XZ designed the study. XZW, QZP, BSX, WX, DSW, JJZ, HRX, ZH and XZ conducted the study and collected the data. XZW, QZP, XHN and XZ analyzed the data and interpreted the results. XZW, QZP, XHN and XZ wrote the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no completing interests.
Ethical approval
The study was approved by the Scientific and Ethics Committees of Sun Yat-sen University Cancer Center (Number B2018-102-05).
Consent to participate
Each patient signed a written informed consent before participating to this study (Trial Registration: ChiCTR, ChiCTR1900021550).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wen, Xz., Pan, Qz., Xu, Bs. et al. Phase I study of pegylated liposomal doxorubicin and cisplatin in patients with advanced osteosarcoma. Cancer Chemother Pharmacol 89, 209–215 (2022). https://doi.org/10.1007/s00280-021-04371-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-021-04371-6