Abstract
Purpose
A prospective study was performed to compare the outcome for metastatic breast cancer (MBC) patients treated with docetaxel plus thiotepa (DT) or docetaxel plus capecitabine (DC), and to explore the value of CYP1A1*2C polymorphisms in predicting clinical efficacy of these chemotherapies.
Methods
MBC patients (n = 130) were randomized to treatment with DT (n = 65) or DC (n = 65). Response rate, disease control rate, progression-free and overall survival were monitored. Genotyping of CYP1A1*2C was performed in all patients.
Results
DT and DC produced similar overall disease control rates (76.9 vs 69.2%), median PFS (6.7 vs. 7.5 months) and OS (20.1 vs. 21.0 months) (P > 0.05 for all comparisons); however, DT exhibited a higher rate of control of localized liver metastases (78.6 vs 41.2%, P = 0.023). Among patients homozygous for wild-type CYP1A1*1 genotype (AA), DT treatment was associated with a significantly longer PFS (8.4 vs. 6.4 months, P = 0.019) and OS (33.4 vs. 15.8 months, P = 0.018). Conversely, among patients carrying the variant CYP1A1*2C genotype (AG/GG), DC treatment was associated with a significantly longer PFS (8.4 vs. 5.5 month, P = 0.005), and OS (28.5 vs. 19.6 months, P = 0.010). After adjusting for competing risk factors, CYP1A1*2C genotype was confirmed to be an independent predictor of PFS and OS for each chemotherapy combination.
Conclusions
Overall, DT and DC result in similar clinical efficacy for MBC patients; however, efficacy for each therapy differs depending on CYP1A1*2C genotype.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
There are numerous chemotherapeutic options having similar efficacy against metastatic breast cancer (MBC) [1]; however, pharmacogenomic analysis offers the promise that personalized regimens may be identified for individuals who might have more favorable outcomes with certain chemotherapies [2, 3]. Specifically, because genetic variation in metabolic enzymes is one determinant of drug concentration, pharmacogenomics has been proposed as an approach to tailor drug choice or dose to optimize efficacy and reduce toxicity of cancer treatments [4, 5].
Docetaxel plus capecitabine is among the combination regimens recommended by the National Comprehensive Cancer Network guidelines [6] for MBC patients previously treated with anthracyclines. Indeed, we previously showed that docetaxel plus capecitabine was effective for Chinese MBC patients. Moreover, using the Affymetrix drug-metabolizing enzymes and transporters (DMET) genotyping platform, we identified 79 single nucleotide polymorphisms (SNPs) of cytochrome P450 (CYP45) whose minor allele frequency was ≥ 10% in the Chinese population and then applied this database to 69 MBC patients who were treated with docetaxel plus capecitabine. Only the CYP1A1 rs1048943 A > G (Ile462Val) polymorphism influenced progression-free survival [7].
Thiotepa is an alkylating anticancer agent previously used to treat a variety of solid and hematologic malignancies and which carries a US Food and Drug Administration (FDA) indication for treatment of breast adenocarcinoma [8, 9]. It has been practical to administer at a range of dose levels including high-dose chemotherapy for refractory breast cancers in part, because pharmacokinetic parameters appear to correlate with some of its effects such as myelosuppression [10,11,12,13]. Moreover, we have found that thiotepa could kill breast cancer stem cells in vivo and in vitro when combined with docetaxel and/or adoptive T cell immunotherapy [14, 15]. In our previous clinical experience, docetaxel plus thiotepa demonstrated promising overall survival, especially in those patients with certain metabolic enzyme genotypes. In a case–control series, we found that the efficacy of the combination of thiotepa and docetaxel compared favorably with that of docetaxel plus capecitabine [16,17,18]. We, therefore, designed a prospective randomized clinical trial to compare the clinical benefits of these two combination regimens and further to explore the value of CYP1A1*2C polymorphisms in identifying patients more likely to benefit from a particular chemotherapy regimens.
Patients and methods
Study enrollment
This study (ClinicalTrials.gov identifier, NCT01199393) (https://register.clinicaltrials.gov/) was approved by the ethics committee of Peking University Cancer Hospital. All participants provided written informed consent for the treatment and the genetic polymorphism analysis before enrollment. The study was carried out in accordance with Declaration of Helsinki. Patients meeting the following criteria were eligible for enrollment: female, age ≥ 18 years with histologically proven MBC, measurable disease per response evaluation criteria in solid tumors (RECIST) [19], and not previously treated for metastatic disease; Eastern Cooperative Oncology Group (ECOG) performance status [20] of 0–2; adequate bone marrow, cardiac, renal and liver function; not pregnant or lactating; no serious or uncontrolled medical conditions; no history of other malignancies; estimated life expectancy of at least 3 months; and, at least 6 months since last adjuvant/neoadjuvant chemotherapy administration before registration. Prior hormonal or radiation therapy was allowed if completed at least 4 weeks before enrollment and if less than 25% of the bone marrow had previously been irradiated. Prior trastuzumab was also permitted.
Therapeutic protocol
Patients were randomly assigned to either docetaxel plus thiotepa (DT) or docetaxel plus capecitabine (DC). They were stratified by presence or absence of liver metastases. For the DT group, patients received docetaxel (Aventis Pharma S. A.) 35 mg/m2 intravenously on days 1 and 8, and thiotepa (Shanghai Xu-dong-hai-pu Pharma) 60 mg/m2, intravenously on day 1. For the DC group, patients received docetaxel (Aventis Pharma S. A.) 75 mg/m2 intravenously on day 1 and capecitabine (Roche Pharma Ltd) 2000 mg/m2 by mouth divided into two doses on days 1–14. Cycles of both regimens were repeated every 21 days until disease progression, unacceptable toxicity or patient refusal. Premedication consisted of oral dexamethasone 7.5 mg daily beginning on the day before the docetaxel infusion and continuing for a total of 3 days. 5-Hydroxytryptamine-3 receptor antagonists were administered to prevent emesis.
Response and adverse event assessments
Tumor responses were evaluated by contrasted CT or MRI scans after every two cycles to evaluate clinical responses according to RECIST criteria version 1.0. Responses were confirmed with repeat imaging 4 weeks later. In a subgroup of patients with liver metastases, we solely measured the change in the liver lesions. Toxicity was graded according to the National Cancer Institute Common Toxicity Criteria version 3.0.
Genotyping
Prior to chemotherapy, genomic DNA was extracted from peripheral blood samples (4 ml) using a standard phenol–chloroform method. Genetic polymorphisms of CYP1A1*2C were detected by polymerase chain reaction (PCR) and subsequent direct sequencing.
Statistical analysis
All data were analyzed by SPSS for Windows version 15.0 (SPSS Inc., Chicago, IL, USA). Categorical variables and variant genotypes were analyzed by the Chi-square test and continuous variables were analyzed by T test. Progression-free survival (PFS) and overall survival (OS) were estimated by the Kaplan–Meier method. Log-rank tests were used to determine whether survival differed between different treatments, clinical factors, or genotypes.
Significant variables in log-rank tests were further analyzed by Cox proportional hazard regression models with confounder adjustment. All tests were two tailed and the significance level was 0.05.
Results
Patients’ characteristics
From August 2010 to June 2012, 130 patients were enrolled, of whom 65 patients were randomized to DT and 65 were randomized to DC. All patients completed the efficacy evaluations and genetic polymorphism analysis. Patient characteristics were well balanced between the two treatment groups (Table 1). Patients were mostly postmenopausal (mean age 53.1 years) and the majority had the Luminal A subtype of breast cancer. More than 63% had visceral metastasis. The proportion of patients harboring CYP1A1*2C mutant genotypes (AA/AG) was slight higher in the DT group than the DC group (P = NS).
Clinical response and survival
There was no significant difference in objective response rates between the two treatments. The overall disease control rates were 76.9 versus 69.2% in DT and DC groups, respectively (P = 0.429); however, among the 45 patients with liver metastases, the clinical benefit rate (CR + PR + SD) was significant higher in the DT group than in the DC group (78.6 versus 41.2%, P = 0.023).
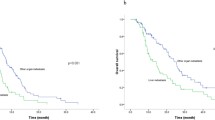
In total, 114 patients experienced disease progression (56 patients in the DT group and 58 in the DC group). Neither PFS nor OS were significantly different between the two groups (Fig. 1). The median PFS was 6.7 months (95% CI, 5.3–8.1) in the DT group and 7.5 months (95% CI, 6.5–8.5) in the DC group (P > 0.05). There were 84 deaths (38 in the DT group and 46 in the DC group). The median OS was 20.1 months (95% CI, 13.7–26.5) in the DT group and 21.0 months (95% CI, 18.7–23.3) in the DC group (P > 0.05).
Genotype associated with PFS and OS varies by chemotherapy regimen
Genotype distribution of CYP1A1*2C followed the Hardy–Weinberg equivalence (HWE). Because there were only five individuals with homozygous variants (GG) (four in the DT group and one in the DC group), the mutant carriers (AG/GG) were grouped together for analysis. There was no relationship between CYP1A1*2C genotype and clinical outcome in the entire study group as a whole (Table 2) or among those with liver metastases (Table 3); however, among patients homozygous for wild-type CYP1A1*1 (AA), those treated with DT had significantly longer PFS [median, 8.4 (95% CI, 3.3–13.5) vs. 5.5 (95% CI, 1.7–9.3) months, P = 0.004] and OS [median, 33.4 (95% CI, 19.7–47.1) vs. 19.6 (95% CI, 14.0–25.2) months, P = 0.045], compared with patients treated with DC (Fig. 2). Conversely, among patients carrying the variant CYP1A1*2C genotypes (AG/GG), those treated with DC had significantly longer PFS [median, 8.4 (95% 3.4–13.4) vs. 6.4 (95% CI, 5.6–7.2) months, P = 0.046], and OS [median, 28.5 (95% CI, 22.650–34.350) vs. 15.8 (95% CI, 8.713–22.887) months, P = 0.005], compared with patients treated with DT (Fig. 3).
Predictors associated with clinical outcomes
On univariate analysis, patients with wild genotype (AA) had longer PFS (8.4 vs. 6.4 months, P = 0.019) and OS (33.4 vs. 15.8 moths, P = 0.018), compared with the variant CYP1A1*2C genotype (AG/GG) in DT group. Conversely, for the DC group, mutant genotype (AG/GG) carriers had superior clinical outcomes in both PFS (8.4 vs. 5.5 months, P = 0.005) and OS (28.5 vs. 19.6 moths, P = 0.010) (shown in Table 4).
Cox proportional hazards models were then employed to quantify the prognostic significance of risk factors after multivariable adjustment. A multivariable analysis was performed to assess the factors that demonstrated significant effects in univariate analysis. After adjusting for competing risk factors, ER-negative status was associated with inferior PFS (but not OS) for patients treated with DT (HR 1.785, 95% CI 1.019–3.127, P = 0.043).
The mutant genotypes (AG/GG) of CYP1A1*2C were confirmed to be independent risk predictors of PFS (HR 1.90, 95% CI 1.04–3.50, P = 0.038) and OS (HR 2.24, 95% CI 1.03–4.8, P = 0.042) for the DT group, whereas in the DC group, the mutant genotypes (AG/GG) were confirmed to reduce the risks for both progression (HR 0.412, 95% CI 0.229–0.742, P = 0.003) and death (HR 0.406, 95% CI 0.198–0.833, P = 0.014). The details are shown in Table 4.
Treatment-related toxicity
Chemotherapy-induced toxicities were assessed in all enrolled patients. Grades 3 and 4 toxicities are summarized in Table 5 and the incidence rates are presented in suppl. table 1. The majority of patients experienced hematotoxicity, generally mild and tolerable. More patients in the DT group suffered serious leukopenia than in the DC group (43.1 vs. 20.8%, P = 0.004). Severe hand–foot syndrome only occurred in the DC group (P < 0.001). All toxicities were manageable and no treatment-related mortality occurred. While the rates of severe hematotoxicity were slightly higher in the wild-type genotype (AA) carriers of CYP1A1*1, there were no significant differences in toxicities between different genotypes.
Discussion
Because of the risks of anthracyclines, especially in elderly patients, DC is an effective regimen frequently used as a first-line treatment for MBC [21, 22]. In this prospective randomized clinical trial, we have demonstrated that DT also represents an efficacious option for the first-line treatment of MBC. The response rates, PFS and OS were not significantly different in the DT group and the DC group, and the clinical outcomes were equivalent to the results reported in other docetaxel-containing clinical trials of patients with MBC pretreated with anthracyclines, in which the median overall survivals were 19.9–23.6 months [23,24,25].
The site of organ metastasis of breast cancer is associated with clinical outcome and therapies targeting specific sites are attracting increasing interest [26,27,28]. After lymph nodes and lung, the liver ranks as the third most frequent site of breast cancer metastases and the presence of liver metastases is associated with unfavorable prognosis [29]. The more effective treatment for liver metastases, locoregional or systemic therapy, is unknown. In the present study, DT achieved control of liver metastases in 78.6% of affected patients and was more effective than DC. Schrama et al. reported that 22% (2/9) patients with liver metastasis achieved long-term PFS (over 18 months) treated with a thiotepa-containing regimen [30]. A potential explanation for this benefit of thiotepa-containing regimens for liver metastases is suggested by previous observations suggesting that the liver is an important site of thiotepa biotransformation in vivo, as thiotepa is metabolized by oxidative desulfuration to yield the active metabolite tepa in the liver [31, 32].
It is well established that genetic factors are strong determinants of in vivo drug-related therapeutic efficacy and toxicity, and pharmacogenetics is poised to assume a leading role in precision medicine [33, 34]; however, few pharmacogenomic biomarkers are routinely used to choose potentially more efficacious regimens for cancer patients [1, 35]. Our previous study of SNPs in genes encoding phase I and phase II drug-metabolizing enzymes showed that these polymorphisms could affect drug responses in MBC patients [7, 17, 18]. We were also interested in whether any pharmacogenomic biomarkers would be predictive of benefit for such chemotherapy.
Polymorphisms in the drug-metabolizing enzyme CYP1A1 have been extensively studied. CYP1A1*2C, one of the common genetic mutant sites, is strongly associated with susceptibility to various cancers [36,37,38]. Presence of the SNP in CYP1A1*2C characterized by an A to G mutation at nucleotide 2,455 in exon 7 results in an amino acid change from isoleucine to valine at codon 462 and increased catalytic activity leading to enhanced DNA adduct formation [39]. These DNA adducts might be responsible for causing mutations in tumor suppressor genes and oncogenes, leading to malignancy, but also affecting the response of tumor cells to certain therapy [40]. However, to our knowledge, little information is available on the role of CYP1A1 in relation to the clinical outcomes of MBC patients undergoing chemotherapy.
The results of this study demonstrate that patients with specific polymorphisms in CYP1A1 may benefit more from certain chemotherapy regimens. The wild-type CYP1A1*1 genotype (AA) benefitted more from DT while those the carrying mutant CYP1A1 gene polymorphisms benefitted more from DC, consistent with our previous results in a single-arm study [7]. The clinical benefits associated with these polymorphisms extend to other chemotherapies and targeted therapies. Heubner et al. observed a statistically significant association between the 462Val allele and platinum resistance in ovarian cancer [41]. A favorable clinical response to imatinib was reported for patients with chronic myeloid leukemia patients and the heterozygous genotype (AG) [40]. Although further confirmation is needed, these findings indicate that the CYP1A1*2C polymorphism could serve as a useful therapeutic marker in predicting response to multiple therapies.
Our study has several limitations. We have only investigated the predictive value of common variants of CYP1A1 and other polymorphisms in drug-metabolizing enzymes might also play roles in determining clinical outcomes to the DC and DT regimens. Similarly, factors unrelated to metabolic enzyme level or function such as patient compliance and absorption of oral drugs could affect therapeutic benefit. Validation studies with larger numbers of patients are warranted.
In conclusion, we have demonstrated that the DT regimen is well-effective and tolerable first-line chemotherapy for MBC patients who have been pretreated with anthracycline, especially with liver metastasis. To further improve the therapeutic efficacy, the polymorphism of CYP1A1*2C might act as predict biomarker for MBC patients who are administered DT or DC therapy.
References
Huntington SF, Gross CP (2016) Negative studies in cancer research: why the negativity? JAMA Oncol 2(7):865–866. https://doi.org/10.1001/jamaoncol.2015.6540
McLeod HL (2013) Cancer pharmacogenomics: early promise, but concerted effort needed. Science 339(6127):1563–1566. https://doi.org/10.1126/science.1234139
Sadee W (2011) Pharmacogenomic biomarkers: validation needed for both the molecular genetic mechanism and clinical effect. Pharmacogenomics 12(5):675–680. https://doi.org/10.2217/pgs.11.23
Zembutsu H (2015) Pharmacogenomics toward personalized tamoxifen therapy for breast cancer. Pharmacogenomics 16(3):287–296. https://doi.org/10.2217/pgs.14.171
Harper AR, Topol EJ (2012) Pharmacogenomics in clinical practice and drug development. Nat Biotechnol 30(11):1117–1124. https://doi.org/10.1038/nbt.2424
Gradishar WJ, Anderson BO, Balassanian R, Blair SL, Burstein HJ, Cyr A, Elias AD, Farrar WB, Forero A, Giordano SH, Goetz M, Goldstein LJ, Hudis CA, Isakoff SJ, Marcom PK, Mayer IA, McCormick B, Moran M, Patel SA, Pierce LJ, Reed EC, Salerno KE, Schwartzberg LS, Smith KL, Smith ML, Soliman H, Somlo G, Telli M, Ward JH, Shead DA, Kumar R (2015) NCCN guidelines insights breast cancer, Version 1.2016. J Natl Compr Canc Netw 13(12):1475–1485
Dong N, Yu J, Wang C, Zheng X, Wang Z, Di L, Song G, Zhu B, Che L, Jia J, Jiang H, Zhou X, Wang X, Ren J (2012) Pharmacogenetic assessment of clinical outcome in patients with metastatic breast cancer treated with docetaxel plus capecitabine. J Cancer Res Clin Oncol 138(7):1197–1203. https://doi.org/10.1007/s00432-012-1183-5
Thiotepa (2011). Report on carcinogens. Carcinog Profiles 12:406–407
Dardis C, Milton K, Ashby L (2015) Whither thiotepa (for patients in the USA)? J Neuro-oncol 124(3):529–530. https://doi.org/10.1007/s11060-015-1856-4
Berry DA, Ueno NT, Johnson MM, Lei X, Caputo J, Rodenhuis S, Peters WP, Leonard RC, Barlow WE, Tallman MS, Bergh J, Nitz UA, Gianni AM, Basser RL, Zander AR, Coombes RC, Roche H, Tokuda Y, de Vries EG, Hortobagyi GN, Crown JP, Pedrazzoli P, Bregni M, Demirer T (2011) High-dose chemotherapy with autologous stem-cell support as adjuvant therapy in breast cancer: overview of 15 randomized trials. J Clin Oncol 29(24):3214–3223. https://doi.org/10.1200/JCO.2010.32.5910
Rodenhuis S, Bontenbal M, van Hoesel QG, Smit WM, Nooij MA, Voest EE, van der Wall E, Hupperets P, van Tinteren H, Peterse JL, van de Vijver MJ, de Vries EG, Netherlands Working Party on Autologous Transplantation in Solid T (2006) Efficacy of high-dose alkylating chemotherapy in HER2/neu-negative breast cancer. Ann Oncol 17 (4):588–596. https://doi.org/10.1093/annonc/mdl001
Wang X, Ren J, Zhang J, Yan Y, Jiang N, Yu J, Di L, Song G, Che L, Jia J, Zhou X,Yang H, Lyerly HK (2016) Prospective study of cyclophosphamide, thiotepa, carboplatin combined with adoptive DC-CIK followed by metronomic cyclophosphamide therapy as salvage treatment for triple negative metastatic breast cancers patients (aged < 45). Clin Trans Oncol 18 (1):82–87. https://doi.org/10.1007/s12094-015-1339-2
Hagen B (1991) Pharmacokinetics of thio-TEPA and TEPA in the conventional dose-range and its correlation to myelosuppressive effects. Cancer Chemother Pharmacol 27(5):373–378
Lu Z, Jia J, Di L, Song G, Yuan Y, Ma B, Yu J, Zhu Y, Wang X, Zhou X, Ren J (2011) DNA methyltransferase inhibitor CDA-2 synergizes with high-dose thiotepa and paclitaxel in killing breast cancer stem cells. Front Biosci (Elite Ed) 3:240–249
Ren J, Di L, Song G, Yu J, Jia J, Zhu Y, Yan Y, Jiang H, Liang X, Che L, Zhang J, Wan F, Wang X, Zhou X, Lyerly HK (2013) Selections of appropriate regimen of high-dose chemotherapy combined with adoptive cellular therapy with dendritic and cytokine-induced killer cells improved progression-free and overall survival in patients with metastatic breast cancer: reargument of such contentious therapeutic preferences. Clin Trans Oncol 15(10):780–788. https://doi.org/10.1007/s12094-013-1001-9
Yu J, Lj DI, Song G, Che L, Jiang H, Zhu Y, Liang X, Jia J, Zhang J, Yang H, Wang X, Zhou X, Ren J (2011) Randomized clinical case-control trial for the comparison of docetaxel plus thiotepa versus docetaxel plus capecitabine in patients with metastatic breast cancer. Beijing Da Xue Xue Bao 43(1):151–156
Song Q, Zhou X, Yu J, Dong N, Wang X, Yang H, Ren J, Lyerly HK (2015) The prognostic values of CYP2B6 genetic polymorphisms and metastatic sites for advanced breast cancer patients treated with docetaxel and thiotepa. Sci Rep 5:16775. https://doi.org/10.1038/srep16775
Zhou X, Wang X, Song Q, Yang H, Zhu X, Yu J, Song G, Di L, Ren J, Shao H, Lyerly HK (2015) Transformation of alkylating regimen of thiotepa into tepa determines the disease progression through GSTP1 gene polymorphism for metastatic breast cancer patients receiving thiotepa containing salvage chemotherapy. Int J Clin Pharmacol Ther 53(11):914–922. https://doi.org/10.5414/CP202391
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92(3):205–216
de Kock I, Mirhosseini M, Lau F, Thai V, Downing M, Quan H, Lesperance M, Yang J (2013) Conversion of Karnofsky Performance Status (KPS) and Eastern Cooperative Oncology Group Performance Status (ECOG) to Palliative Performance Scale (PPS), and the interchangeability of PPS and KPS in prognostic tools. J Palliat Care 29(3):163–169
O’Shaughnessy J, Miles D, Vukelja S, Moiseyenko V, Ayoub JP, Cervantes G, Fumoleau P, Jones S, Lui WY, Mauriac L, Twelves C, Van Hazel G, Verma S, Leonard R (2002) Superior survival with capecitabine plus docetaxel combination therapy in anthracycline-pretreated patients with advanced breast cancer: phase III trial results. J Clin Oncol 20(12):2812–2823. https://doi.org/10.1200/JCO.2002.09.002
Li J, You J, Si W, Zhu Y, Chen Y, Yang B, Han C, Linghu R, Zhang X, Jiao S, Yang J (2015) Docetaxel/S-1 versus docetaxel/capecitabine as first-line treatment for advanced breast cancer: a retrospective study. Medicine (Baltimore) 94(41):e1340. https://doi.org/10.1097/MD.0000000000001340
John M, Hinke A, Stauch M, Wolf H, Mohr B, Hindenburg HJ, Papke J, Schlosser J, Group FS (2012) Weekly paclitaxel plus trastuzumab in metastatic breast cancer pretreated with anthracyclines—a phase II multipractice study. BMC cancer 12:165. https://doi.org/10.1186/1471-2407-12-165
Fabi A, Giannarelli D, Malaguti P, Ferretti G, Vari S, Papaldo P, Nistico C, Caterino M, De Vita R, Mottolese M, Iacorossi L, Cognetti F (2015) Prospective study on nanoparticle albumin-bound paclitaxel in advanced breast cancer: clinical results and biological observations in taxane-pretreated patients. Drug Des Devel Ther 9:6177–6183. https://doi.org/10.2147/DDDT.S89575
Vici P, Fabi A, Metro G, Sergi D, Giannarelli D, Di Lauro L, Bepler G, Tomao F, Cognetti F, Conti F, Lopez M (2011) Phase I–II trial of prolonged gemcitabine infusion plus paclitaxel as a biweekly schedule for advanced breast cancer patients pretreated with anthracyclines. Cancer Chemother Pharmacol 67(3):687–693. https://doi.org/10.1007/s00280-010-1369-y
Redig AJ, McAllister SS (2013) Breast cancer as a systemic disease: a view of metastasis. J Intern Med 274(2):113–126. https://doi.org/10.1111/joim.12084
Venur VA, Leone JP (2016) Targeted therapies for brain metastases from breast cancer. Int J Mol Sci 17 (9). https://doi.org/10.3390/ijms17091543
Biskup E, Cai F, Vetter M (2017) Bone targeted therapies in advanced breast cancer. Swiss Med Wkly 100:w14440. doi:smw.2017.14440
Disibio G, French SW (2008) Metastatic patterns of cancers: results from a large autopsy study. Arch Pathol Lab Med 132(6):931–939. https://doi.org/10.1043/1543-2165(2008)132[931:MPOCRF]2.0.CO;2
Schrama JG, Baars JW, Holtkamp MJ, Schornagel JH, Beijnen JH, Rodenhuis S (2001) Phase II study of a multi-course high-dose chemotherapy regimen incorporating cyclophosphamide, thiotepa, and carboplatin in stage IV breast cancer. Bone Marrow Transplant 28(2):173–180. https://doi.org/10.1038/sj.bmt.1703105
Miller B, Tenenholz T, Egorin MJ, Sosnovsky G, Rao NU, Gutierrez PL (1988) Cellular pharmacology of N,N’,N’’-triethylene thiophosphoramide. Cancer Lett 41(2):157–168
Chang TK, Chen G, Waxman DJ (1995) Modulation of thiotepa antitumor activity in vivo by alteration of liver cytochrome P450-catalyzed drug metabolism. J Pharmacol Exp Ther 274(1):270–275
Scott SA (2011) Personalizing medicine with clinical pharmacogenetics. Genet Med 13(12):987–995. https://doi.org/10.1097/GIM.0b013e318238b38c
Patel JN (2016) Cancer pharmacogenomics, challenges in implementation, and patient-focused perspectives. Pharmgenomics Pers Med 9:65–77. https://doi.org/10.2147/PGPM.S62918
Twelves C, Jove M, Gombos A, Awada A (2016) Cytotoxic chemotherapy: Still the mainstay of clinical practice for all subtypes metastatic breast cancer. Crit Rev Oncol Hematol 100:74–87. https://doi.org/10.1016/j.critrevonc.2016.01.021
Abd El Wahab N, Shafik NF, Shafik RE, Taha Sh A, Shafik HE, Darwish AD (2017) Association of CYP3A5*3 and CYP1A1*2C polymorphism with development of acute myeloid leukemia in Egyptian patients. Asian Pac J Cancer Prev 18(3):747–752. https://doi.org/10.22034/APJCP.2017.18.3.747
Jain V, Ratre YK, Amle D, Mishra PK, Patra PK (2017) Polymorphism of CYP1A1 gene variants rs4646903 and rs1048943 relation to the incidence of cervical cancer in Chhattisgarh. Environ Toxicol Pharmacol 52:188–192. https://doi.org/10.1016/j.etap.2017.04.009
Cho YA, Lee J, Oh JH, Chang HJ, Sohn DK, Shin A, Kim J (2017) Dietary flavonoids, CYP1A1 genetic variants, and the risk of colorectal cancer in a Korean population. Sci Rep 7(1):128. https://doi.org/10.1038/s41598-017-00117-8
Zhou SF, Liu JP, Chowbay B (2009) Polymorphism of human cytochrome P450 enzymes and its clinical impact. Drug Metab Rev 41(2):89–295. https://doi.org/10.1080/03602530902843483
Lakkireddy S, Aula S, Avn S, Kapley A, Rao Digumarti R, Jamil K (2015) Association of the common CYP1A1*2C variant (Ile462Val polymorphism) with chronic myeloid leukemia (CML) in patients undergoing imatinib therapy. Cell J 17(3):510–519
Heubner M, Wimberger P, Riemann K, Kasimir-Bauer S, Otterbach F, Kimmig R, Siffert W (2010) The CYP1A1 Ile462Val polymorphism and platinum resistance of epithelial ovarian neoplasms. Oncol Res 18(7):343–347
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
This study was funded by Susan G Komen for Cure Foundation (no. SPCHIN1201), Youth Foundation of Beijing Shijitan Hospital of Capital Medical University (no. 2013-q-04) and China Railway Corporation Research Project (2016-A44).
Conflict of interest
The authors declared that they have no conflicts of interest related to this work.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Zhou, X., Qiao, G., Wang, X. et al. CYP1A1 genetic polymorphism is a promising predictor to improve chemotherapy effects in patients with metastatic breast cancer treated with docetaxel plus thiotepa vs. docetaxel plus capecitabine. Cancer Chemother Pharmacol 81, 365–372 (2018). https://doi.org/10.1007/s00280-017-3500-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3500-9