Abstract
Purpose
We aimed to retrospectively evaluate the efficacy and toxicity of an irinotecan hydrochloride (CPT) and nedaplatin (N) combination therapy for recurrent and refractory endometrial carcinoma, administered based on UGT1A1 genotype.
Methods
Between 2009 and 2017, 21 patients who received CPT-N therapy for recurrent endometrial carcinoma as second- or third-line chemotherapy at our hospital were identified. The CPT-N regimen included 40–70 mg/m2 of CPT-11 on days 1, 8, and 15, and 50 mg/m2 of nedaplatin on day 1, q4 weeks.
Results
The median patient age was 63 years. The number of prior chemotherapeutic regimens ranged from 1 to 2. Two patients had prior pelvic irradiation. The response rate [ratio of complete remission (CR) to partial remission (PR)] of CPT-N therapy was 3 of 21 (14.3%), and clinical benefit rate (CBR) [the combined percentages of CR, PR, and stable disease (SD)] was 9 of 21 (42.8%). Toxicities included grade 3 neutropenia [4 (19.0%) cases], grade 3 febrile neutropenia [2 (9.5%) cases], and grade 3 diarrhea [3 (14.3%) cases]; all resolved with conservative treatment. Patients with a wild-type UGT1A1 status received higher doses of CPT-11 (p = 0.048) and had similar RR and CBR compared to those with a UGT1A1*6 and *28 status. There were no significant differences in frequencies of hematological or non-hematological toxicities, regardless of UGT1A1 status.
Conclusions
The CPT-N regimen for recurrent and refractory endometrial carcinoma had tolerable side effects and significant efficacy. This regimen is a viable treatment option for endometrial carcinoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recently, the incidence of endometrial carcinomas has been increasing [1]. The standard primary treatment for operable patients with endometrial carcinoma is surgery followed by pelvic irradiation or chemotherapy, according to classification of postoperative recurrence risk [2]. In Japan, chemotherapy as adjuvant treatment has gained popularity, based on the results of the Japanese Gynecologic Oncology Group (JGOG) 2033 [3] and the Gynecologic Oncology Group (GOG) 122 [4] studies.
The concept of platinum-free interval exists as a maker for the selection of second-line chemotherapy for ovarian carcinoma [5]. However, a similar interval to define chemo-sensitive or chemo-resistant tumor in prediction of response to second-line chemotherapy does not exist for endometrial carcinoma [6]. Recently, several drugs have been developed for recurrent endometrial carcinoma; however, the response rate (RR) ranges from 4 to 27% for cytotoxic drugs [7,8,9,10,11,12,13,14,15,16,17] and from 0 to 18% for targeted molecular therapeutic agents [18,19,20,21,22,23,24,25,26,27,28]. So far, a biomarker to aid in the choice of drugs, and an effective second-line chemotherapy regimen for recurrent endometrial carcinoma, has not been established.
An active metabolite of irinotecan hydrochloride (CPT), SN-38, was effective as an anti-proliferative agent in four of five human endometrial cancer cell lines (Ishikawa, HEC-1A, HEC-50B, HEC-59, and HEC-108), and had synergic effects with cisplatin in vitro [29]. A tetrazolium dye (MTT) assay showed that CPT had anti-tumor efficacy in about 40% of endometrial carcinomas [30]. In addition, more cases with UDP-glucuronosyltransferase 1A1 (UGT1A1) *6, *28, and *28*6 polymorphisms develop grade 3/4 toxicities than those with wild-type UGT1A1 [31]. The efficacy of combination therapy with CPT and nedaplatin (N) has not been examined yet.
The aim of the present study was to evaluate effects and toxicities of CPT-N in recurrent and refractory endometrial carcinoma as second- or third-line chemotherapy and the correlation between UGT1A1 genotype and adverse effects, retrospectively.
Materials and methods
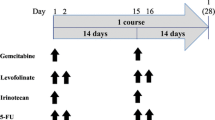
Among patients treated with endometrial carcinoma at our hospital between 2009 and 2017, 21 patients with recurrent and refractory endometrial carcinoma who received CPT-N as second- or third-line chemotherapy were identified. The CPT-N regimen consisted of 40–70 mg/m2 of CPT on days 1, 8, and 15, and 50 mg/m2 of nedaplatin on day 1, q4 weeks. The criteria for therapy administration were: granulocyte count greater than 1500/μL, platelet count greater than 100,000/μL, hemoglobin levels greater than 7 g/dL, and less than the grade 1 non-hematologic toxicity. If these criteria were not met on days 7 and 14, the drug administrations on days 8 and 15 were skipped. If these criteria were not met on day 1 at the next cycle, the administration on day 1 was delayed for 1 week. Patients who did not receive CPT-N according to these administration criteria were excluded.
Performance status was evaluated by the World Health Organization (WHO) performance status. Surgical stage was evaluated according to the International Federation of Gynecology and Obstetrics 2014 staging system. Tumor response was evaluated using Response Evaluation Criteria in Solid Tumors (RECIST) [32]. Response rate (RR) was defined as the ratio of complete remission (CR) to partial remission (PR). Clinical benefit rate (CBR) was defined as the combined percentages of CR, PR, and stable disease (SD). Serum levels of tumor markers including cancer antigen 125 (CA-125) were not used for evaluating progression in this study. Assessment of toxicities was carried out and graded according to the National Cancer Institute Common Toxicity Criteria Version 4.0 (CTCAE v3.0).
Polymorphisms of UGT1A1 were analyzed using the Invader UGT1A1 Molecular Assay (BML, Kawagoe, Japan). The UGT1A1*6 and *28 polymorphisms were defined as non-wild type.
The Stat View software ver. 5.0 (SAS Institution Inc., NC, USA) was used for statistical analysis. Progression-free survival (PFS) was calculated from the date of administration of CPT-N to recurrence or cancer-specific death. Overall survival (OS) was calculated from the date of the administration of CPT-N to cancer-specific death. Survival curves of PFS and OS were generated by Kaplan–Meier analysis. The Fisher exact test was used to evaluate differences in the correlations between UGT1A1 polymorphisms, treatment efficacy, and toxicities. Statistical significance was defined as a p < 0.05.
Results
The patient characteristics are summarized in Table 1. The median age of patients was 63 years (range: 41–77). Seventeen patients out of 21 (81%) had a performance status of 0 or 1. Four patients had stage Ib, 1 had stage IIIa, 2 had stage IIIc1, 1 had stage IIIc2, and 14 had stage IVb disease. All patients had received at least 1 course of platinum-based chemotherapy as prior chemotherapy. Two (9.5%) patients had a history of prior radiation therapy.
The details of drug cycles and response to chemotherapy are listed in Table 2. The median number of cycles was 3 (range 1–6). Three patients had CR, 6 patients had SD, and 12 patients had progressive disease (PD). The RR and CBR were 14 and 43%, respectively. The hematologic and non-hematologic adverse effects observed in patients are shown in Table 3. Four (19%) patients experienced grade 3 neutropenia. Among them, 3 (14%) patients developed grade 3 febrile neutropenia, but recovered with antibiotic therapy. Three (14%) patients developed grade 3 diarrhea which resolved naturally within 1 day. No treatment-related deaths were reported. The PFS and OS are presented in Fig. 1.
The UGT1A1 genotyping results revealed a wild-type status in ten patients, UGT1A1*6 polymorphism in eight patients, UGT1A1*28 polymorphism in 2 patients, and UGT1A1*6*28 polymorphism in one patient. Compared with patients presenting with non-wild-type status, more patients with a wild-type status received a higher dose of CPT (p = 0.048). There were no statistical differences in RR and CBR between wild-type and non-wild-type patients (p = 0.59 and p = 0.67, respectively). Furthermore, there were no statistical significant differences in frequencies of hematological and non-hematological toxicities, regardless of UGT1A1 status (Table 4).
Discussion
Tables 5 and 6 list several cytotoxic drugs and targeted molecular therapeutic agents that have been evaluated as second-line chemotherapy for recurrent endometrial carcinoma in the GOG phase II study. The RR of cytotoxic agents described in the literature ranges from 4 to 27% [7,8,9,10,11,12,13,14,15,16,17], and drugs with high efficacies have not been developed yet. Due to the anti-tumor effects displayed in recurrent ovarian cancer, bevacizumab, an anti-angiogenic agent, [33, 34] along with other anti-angiogenic agents including thalidomide, bevacizumab, aflibercept, sorafenib, sunitinib, brivanib, nintedanib, and trebananib, were expected to also show anti-tumor efficacy. However, none among these drugs has proved to be significantly effective. On the other hand, mammalian target of rapamycin (mTOR) inhibitors such as temsirolimus and evelorimus has shown significant efficacy in endometrial carcinoma, which may be due to the dysregulation of phosphatase and tensin homolog (PTEN) expression and activation of the phosphatidylinositol-3-kinase (PI3K)/AKT/ mTOR pathway in such carcinomas [21, 22]. However, all targeted molecular therapeutic agents displayed a lower RR, ranging from 0 to 14%. Although RR may not be the only relevant metric for drug selection, it is clear that there are no definitive single agent therapies for recurrent and refractory endometrial carcinomas.
Although literature evidence suggests that CPT displays antitumor effects in endometrial cancer cells [29], the clinical benefit of a CPT regimen has not been examined previously. The results of our study demonstrated that CPT-N conferred a RR comparable to other agents without side effects (an important factor to consider in the case of recurrent or refractory endometrial carcinomas). As the view point, there was the biomarker to predict the developing side effects using CPT. The active metabolite of CPT, SN-38, is glucuronidated by UGT1A1 and inactivated. The toxicities of CPT were associated with UGT1A1 polymorphisms [35, 36]. Particularly, patients with a UGT1A1*6 genotype developed more severe toxicities compared to those with a wild-type genotype [31]. In this study, CPT dose modification according to UGT1A1 status ensured that a lower dose of CPT was administered to patients with a non-wild-type genotype. Interestingly, even with a lower dose of CPT, such patients showed RRs and toxicities comparable to those with a wild-type genotype. Thus, CPT dose modification based on UGT1A1 polymorphism status could decrease adverse effects and preserve RR in endometrial carcinoma patients.
Literature evidence shows that in colon cancer, a CPT-containing regimen, conferred a significant clinical benefit, and loss of tumor microsatellite instability (MSI) may serve as an effective biomarker to predict improved outcome in patients [37]. MSI was discovered in 40% of endometrioid carcinomas [38], and since CPT is efficacious against endometrioid carcinoma, further studies examining the association between MSI and response to CPT regimen in endometrial carcinoma patients would be useful.
This limitation of our study was that it was a single-institutional and retrospective study with a small sample size. In addition, CPT-N did not confer a higher RR than other popular regimens, although the side effects profile was relatively better.
In conclusion, this study showed that the CPT-N regimen tested here had a satisfactory RR with tolerable adverse effects. Furthermore, utilizing UGT1A1 polymorphism status to aid in dose determination might lower the incidence of side effects while preserving anti-tumor effects. The CPT-N regimen needs to be further explored as a candidate second-line chemotherapy option for endometrial carcinomas.
References
Matsuda T, Marugame T, Kamo KI, Katanoda K, Ajiki W, Sobue T, The Japan Cancer Surveillance Research Group (2011) Cancer incidence and incidence rates in Japan in 2005: based on data from 12 population-based cancer registries in the monitoring of cancer incidence in Japan (MCIJ) project. Jpn J Clin Oncol 41:139–147. doi:10.1093/jjco/hyq169
Nagase S, Katabuchi H, Hiura M, Sakuragi N, Aoki Y, Kigawa J, Saito T, Hachisuga T, Ito K, Uno T, Katsumata N, Komiyama S, Susumu N, Emoto M, Kobayashi H, Metoki H, Konishi I, Ochiai K, Mikami M, Sugiyama T, Mukai M, Sagae S, Hoshiai H, Aoki D, Ohmichi M, Yoshikawa H, Iwasaka T, Udagawa Y, Yaegashi N, Japan Society of Gynecologic Oncology (2010) Evidence-based guidelines for treatment of uterine body neoplasm in Japan: Japan Society of Gynecologic Oncology (JSGO) 2009 edition. Int J Clin Oncol 15:531–542. doi:10.1007/s10147-010-0138-6
Susumu N, Sagae S, Udagawa Y, Niwa K, Kuramoto H, Satoh S, Kudo R (2008) Randomized phase III trial of pelvic radiotherapy versus cisplatin-based combined chemotherapy in patients with intermediate- and high-risk endometrial cancer: a Japanese Gynecologic Oncology Group study. Gynecol Oncol 108:226–233. doi:10.1016/j.ygyno.2007.09.029
Randall ME, Filiaci VL, Muss H, Spirtos NM, Mannel RS, Fowler J, Thigpen JT, Benda JA (2006) Randomized phase III trial of whole-abdominal irradiation versus doxorubicin and cisplatin chemotherapy in advanced endometrial carcinoma: a Gynecologic Oncology Group study. J Clin Oncol 24:36–44. doi:10.1200/JCO.2004.00.7617
Markman M, Rothman R, Hakes T, Reichman B, Hoskins W, Rubin S, Jones W, Almadrones L, Lewis JL Jr (1991) Second-line platinum therapy in patients with ovarian cancer previously treated with cisplatin. J Clin Oncol 9:389–93. doi:10.1200/JCO.1991.9.3.389
Moore KN, Tian C, McMeekin DS, Thigpen JT, Randall ME, Gallion HH (2010) Does the progression-free interval after primary chemotherapy predict survival after salvage chemotherapy in advanced and recurrent endometrial cancer?: a Gynecologic Oncology Group ancillary data analysis. Cancer 116:5407–5414. doi:10.1002/cncr.25480
Lincoln S, Blessing JA, Lee RB, Rocereto TF (2003) Activity of paclitaxel as second-line chemotherapy in endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 88:277–281. doi:10.1016/S0090-8258(02)00068-9
Moore DH, Blessing JA, Dunton C, Buller RE, Reid G (1999) Dactinomycin in the treatment of recurrent or persistent endometrial carcinoma: a phase II study of the Gynecologic Oncology Group. Gynecol Oncol 75:473–475. doi:10.1006/gyno.1999.5652
Muggia FM, Blessing JA, Sorosky J, Reid GC (2002) Phase II trial of the pegylated liposomal doxorubicin in previously treated metastatic endometrial cancer: a Gynecologic Oncology Group study. J Clin Oncol 20:2360–2364. doi:10.1200/JCO.2002.08.171
Plaxe S, Blessing JA, Husseindazeh N, Webster K, Rader J, Dunton C (2002) Evaluation of pyrazoloacridine (PZA) (NSC #366140) in the treatment of recurrent or persistent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 84:241–244. doi:10.1006/gyno.2001.6491
Miller DS, Blessing JA, Lentz SS, Waggoner S (2002) Evaluation of topotecan in the treatment of recurrent or persistent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 87:247–251. doi:10.1006/gyno.2002.6804
Fracasso PM, Blessing JA, Molpus KL, Adler LM, Sorosky JI, Rose PG (2006) Phase II study of oxaliplatin as second-line chemotherapy in endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 103:523–526. doi:10.1016/j.ygyno.2006.03.043
Schilder R, Blessing JA, Pearl ML, Rose PG (2004) Evaluation of irofulven (MGI-114) in the treatment of recurrent or persistent endometrial carcinoma: a phase II study of the Gynecologic Oncology Group. Invest New Drugs 22:343–349. doi:10.1023/B:DRUG.0000026262.77502.31
Garcia A, Blessing J, Nolte S, Mannel R (2008) phase II evaluation of weekly docetaxel in the treatment of recurrent or persistent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 111:22–26. doi:10.1016/j.ygyno.2008.06.013
Miller DS, Blessing JA, Drake RD, Higgins R, McMeekin DS, Puneky LV, Krasner CN (2009) A phase II evaluation of pemetrexed (ALIMTA, LY231514, IND #40061) in the treatment of recurrent or persistent endometrial carcinoma: a Phase II study of the Gynecologic Oncology Group. Gynecol Oncol 115:443–446. doi:10.1016/j.ygyno.2009.09.004
Dizon DS, Blessing JA, McMeekin S, Sharma SK, DiSilvestro P, Alvarez RD (2009) Phase II trial of Ixabepilone as second-line treatment in advanced endometrial cancer: Gynecologic Oncology Group trial 129P. J Clin Oncol 27:3104–3108. doi:10.1200/JCO.2008.20.6995
Tait DL, Blessing JA, Hoffman JS, Moore KN, Spirtos N, Lachance JA, Rotmensch J, Miller DS (2011) A phase II study of gemcitabine (GEMZAR, LY188011) in the treatment of recurrent or persistent endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 121:118–121. doi:10.1016/j.ygyno.2010.11.027
Grendys E, Blessing J, Burger R, Hoffman J (2005) A phase II evaluation of flavorpiridol as second-line chemotherapy of endometrial carcinoma: a Gynecologic Oncology Group study. Gynecol Oncol 98:249–253. doi:10.1016/j.ygyno.2005.05.017
McMeekin DS, Sill MW, Benbrook D, Darcy KM, Stearns-Kurosawa DJ, Eaton L, Yamada SD; Gynecologic Oncology Group (2007) A phase II trial of thalidomide in patients with refractory endometrial cancer and correlation with angiogenesis biomarkers: a Gynecologic Oncology Group study. Gynecol Oncol 105:508–516. doi:10.1016/j.ygyno.2007.01.019
Aghajanian C, Sill MW, Darcy KM, Greer B, McMeekin DS, Rose PG, Rotmensch J, Barnes MN, Hanjani P, Leslie KK (2011) Phase II trial of bevacizumab in recurrent or persistent endometrial cancer: a Gynecologic Oncology Group study. J Clin Oncol 29:2259–2265. doi:10.1200/JCO.2010.32.6397
Oza AM, Elit L, Tsao MS, Kamel-Reid S, Biagi J, Provencher DM, Gotlieb WH, Hoskins PJ, Ghatage P, Tonkin KS, Mackay HJ, Mazurka J, Sederias J, Ivy P, Dancey JE, Eisenhauer EA (2011) Phase II study of temsirolimus in women with recurrent or metastatic endometrial cancer: a trial of the NCIC Clinical Trials Group. J Clin Oncol 29:3278–3285. doi:10.1200/JCO.2010.34.1578
Slomovitz BM, Lu KH, Johnston T, Coleman RL, Munsell M, Broaddus RR, Walker C, Ramondetta LM, Burke TW, Gershenson DM, Wolf J (2010) A phase 2 study of the oral mammalian target of rapamycin inhibitor, everolimus, in patients with recurrent endometrial carcinoma. Cancer 116:5415–5419. doi:10.1002/cncr.25515
Coleman RL, Sill MW, Lankes HA, Fader AN, Finkler NJ, Hoffman JS, Rose PG, Sutton GP, Drescher CW, McMeekin DS, Hu W, Deavers M, Godwin AK, Alpaugh RK, Sood AK (2012) A phase II evaluation of aflibercept in the treatment of recurrent or persistent endometrial cancer: a Gynecologic Oncology Group study. Gynecol Oncol 127:538–543. doi:10.1016/j.ygyno.2012.08.020
Nimeiri HS, Oza AM, Morgan RJ, Huo D, Elit L, Knost JA, Wade JL 3rd, Agamah E, Vokes EE, Fleming GF (2010) A phase II study of sorafenib in advanced uterine carcinoma/carcinosarcoma: a trial of the Chicago, PMH, and California Phase II Consortia. Gynecol Oncol 117:37–40. doi:10.1016/j.ygyno.2010.01.013
Castonguay V, Lheureux S, Welch S, Mackay HJ, Hirte H, Fleming G, Morgan R, Wang L, Blattler C, Ivy PS, Oza AM (2014) A phase II trial of sunitinib in women with metastatic or recurrent endometrial carcinoma: a study of the Princess Margaret, Chicago and California Consortia. Gynecol Oncol 134:274–280. doi:10.1016/j.ygyno.2014.05.016
Powell MA, Sill MW, Goodfellow PJ, Benbrook DM, Lankes HA, Leslie KK, Jeske Y, Mannel RS, Spillman MA, Lee PS, Hoffman JS, McMeekin DS, Pollock PM (2014) A phase II trial of brivanib in recurrent or persistent endometrial cancer: an NRG Oncology/Gynecologic Oncology Group Study. Gynecol Oncol 135:38–43. doi:10.1016/j.ygyno.2014.07.083
Dizon DS, Sill MW, Schilder JM, McGonigle KF, Rahman Z, Miller DS, Mutch DG, Leslie KK (2014) A phase II evaluation of nintedanib (BIBF-1120) in the treatment of recurrent or persistent endometrial cancer: an NRG Oncology/Gynecologic Oncology Group Study. Gynecol Oncol 135:441–445. doi:10.1016/j.ygyno.2014.10.001
Moore KN, Sill MW2, Tenney ME, Darus CJ, Griffin D, Werner TL, Rose PG, Behrens R (2015) A phase II trial of trebananib (AMG 386; IND#111071), a selective angiopoietin 1/2 neutralizing peptibody, in patients with persistent/recurrent carcinoma of the endometrium: An NRG/Gynecologic Oncology Group trial. Gynecol Oncol 138:513–518. doi:10.1016/j.ygyno.2015.07.006
Hiramatsu HP, Kikuchi Y, Seto H, Nagata I (2000) In vitro sensitivity of human endometrial cancer cell lines to paclitaxel or irinotecan (CPT-11) in combination with other aniticancer drugs. Anticancer Drugs 11:573–578
Koshiyama M, Fujii H, Kinezaki M, Ohgi S, Konishi M, Hidetaka N, Hayashi M, Yoshida M (2000) Chemosensitivity testing of irinotecan (CPT-11) in ovarian and endometrial carcinomas: a comparison with cisplatin. Anticancer Res 20:1353–1358
Takano M, Kato M, Yoshikawa T, Sasaki N, Hirata J, Furuya K, Takahashi M, Yokota H, Kino N, Horie K, Goto T, Fujiwara K, Ishii K, Kikuchi Y, Kita T (2009) Clinical significance of UDP-glucuronosyltransferase 1A1*6 for toxicities of combination chemotherapy with irinotecan and cisplatin in gynecologic cancers: a prospective multi-institutional study. Int Soc Cell 76:315–321. doi:10.1159/000209335
Therasse P, Arbuck SG, Eisenhauer EA, Wanders J, Kaplan RS, Rubinstein L, Verweij J, Van Glabbeke M, van Oosterom AT, Christian MC, Gwyther SG (2000) New guidelines to evaluate the response to treatment in solid tumors. European Organization for Research and Treatment of Cancer, National Cancer Institute of the United States, National Cancer Institute of Canada. J Natl Cancer Inst 92:205–216. doi:10.1093/jnci/92.3.205
Burger RA, Sill MW, Monk BJ, Greer BE, Sorosky JI (2007) Phase II trial of bevacizumab in persistent or recurrent epithelial ovarian cancer or primary peritoneal cancer: a Gynecologic Oncology Group Study. J Clin Oncol 25:5165–5171. doi:10.1200/JCO.2007.11.5345
Cannistra SA, Matulonis UA, Penson RT, Hambleton J, Dupont J, Mackey H, Douglas J, Burger RA, Armstrong D, Wenham R, McGuire W (2007) Phase II study of bevacizumab in patients with platinum-resistant ovarian cancer or peritoneal serous cancer. J Clin Oncol 25:5180–5186. doi:10.1200/JCO.2007.12.0782
Iyer L, King CD, Whitington PF, Green MD, Roy SK, Tephly TR, Coffman BL, Ratain MJ (1998) Genetic predisposition to the metabolism of irinotecan (CPT-11). Role of uridine diphosphate glucuronosyltransferase isoform 1A1 in the glucuronidation of its active metabolite (SN-38) in human liver microsomes. J Clin Invest 101:847–854. doi:10.1172/JCI915
Ciotti M, Basu N, Brangi M, Owens IS (1999) Glucuronidation of 7-ethyl-10-hydroxycamptothecin (SN-38) by the human UDP-glucuronosyltransferases encoded at the UGT1 locus. Biochem Biophys Res Commun 260:199–202. doi:10.1006/bbrc.1999.0453
Bertagnolli MM, Niedzwiecki D, Compton CC, Hahn HP, Hall M, Damas B, Jewell SD, Mayer RJ, Goldberg RM, Saltz LB, Warren RS, Redston M (2009) Microsatellite instability predicts improved response to adjuvant therapy with irinotecan, fluorouracil, and leucovorin in stage III colon cancer: Cancer and Leukemia Group B Protocol 89803. J Clin Oncol 27:1814–1821. doi:10.1200/JCO.2008.18.2071
Cancer Genome Atlas Research Network, Kandoth C, Schultz N, Cherniack AD, Akbani R, Liu Y, Shen H, Robertson AG, Pashtan I, Shen R, Benz CC, Yau C, Laird PW, Ding L, Zhang W, Mills GB, Kucherlapati R, Mardis ER, Levine DA (2013) Integrated genomic characterization of endometrial carcinoma. Nature 497:67–73. doi:10.1038/nature12113
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
None.
Conflict of interest
All authors declare no conflict of interest.
Ethical approval
This research was approved by the Ethics Committee of the National Defense Medical College, Tokorozawa, Japan. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Miyamoto, M., Takano, M., Kuwahara, M. et al. Efficacy of combination chemotherapy using irinotecan and nedaplatin for patients with recurrent and refractory endometrial carcinomas: preliminary analysis and literature review. Cancer Chemother Pharmacol 81, 111–117 (2018). https://doi.org/10.1007/s00280-017-3454-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-017-3454-y