Abstract
Purpose
Sarcomas are a rare and heterogeneous variant of cancer. The standard of care treatment involves surgical resection with radiation in high-risk patients. Despite appropriate treatment approximately 50 % of patients will suffer and die from recurrent disease. The purpose of this article is to review the current evidence concerning the use of neoadjuvant chemotherapy with or without radiation in soft tissue sarcomas.
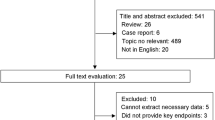
Methods
An in-depth literature search was conducted using Ovid Medline and PubMed.
Results
The most active chemotherapeutic agents in sarcoma are anthracyclines and ifosfamide. Adjuvant chemotherapy trials show only minimal benefit. Neoadjuvant chemotherapy offers the potential advantage of reducing the extent of surgery, increasing the limb salvage rate, early exposure of micrometastatic disease to chemotherapy, and assessment of tumor response to chemotherapy. Some retrospective and phase II trials suggest a benefit to neoadjuvant chemotherapy. Unfortunately, no clearly positive phase III prospectively randomized trials exist for neoadjuvant therapy in soft tissue sarcomas.
Conclusions
The current neoadjuvant chemotherapy trials that do exist are heterogeneous resulting in conflicting results. However, neoadjuvant chemotherapy with or without radiation can be considered in patients with high-risk disease in an attempt to improve long-term outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sarcomas are a rare form of cancer, representing only ~1 % of all adult malignancies [1]. There are over 50 different histologic subtypes of sarcoma [2], emphasizing that sarcomas are multiple diseases with only a questionable basis for inclusion in the same diagnostic category. There are ~13,000 cases of adult sarcomas per year in the USA [3]. Unfortunately ~50 % of sarcoma patients will still die from their disease, despite appropriate and effective local treatment [1]. The primary management of these tumors is wide local surgical excision [4]. The addition of radiation therapy in high-risk patients, such as those with higher-grade tumors or positive resection margins, is beneficial and considered a standard of care [5–7], with a definite increase in local disease control. Neoadjuvant radiation compared to adjuvant radiation has similar efficacies, though differing side-effect profiles, and both are acceptable treatment modalities [8]. Additionally, adjuvant chemotherapy is used in many cases of trunk and extremity soft tissue sarcomas, though the data for efficacy are limited [9–11]. Interpretation of these studies is hampered by the heterogeneous nature of the soft tissue sarcomas. The soft tissue sarcomas included in these studies have varied in size, grade, location, and histologic subtype. These factors may influence the effect of adjuvant chemotherapy, and lead to confounding variables that may be a basis for overall negative results in larger studies [9]. In reality, there may be certain sarcoma populations that benefit from adjuvant chemotherapy, as has been observed in small studies. This benefit may be more in terms of improvement in progression-free survival as the data are limited for improvement in overall survival.
Large-size tumors, higher-grade tumors, and tumors located in the extremity are all tumor characteristics which have been associated with progression-free survival and to some extent an overall survival benefit with adjuvant chemotherapy [9]. These factors are by themselves prognostic for soft tissue sarcomas. Additionally, studies have shown that age, sex, depth, histologic subtype, and extent of surgical resection are all prognostic factors in soft tissue sarcomas [12–24]. For retroperitoneal sarcomas, sex, grade, histology, and extent of surgical resection are the most important prognostic factors [25–33]. Unfortunately, despite advances in surgical resection, neoadjuvant or adjuvant radiation therapy, and adjuvant chemotherapy, the overall prognosis for soft tissue sarcomas has not changed over the last 20 years, and the 5-year overall survival for stage III soft tissue sarcomas is still ~50 % [34]. Clearly, new strategies or techniques are needed to improve this outcome. One possible methodology is the use of neoadjuvant chemotherapy.
The theoretical benefit of neoadjuvant therapy is multifaceted. First, neoadjuvant therapy may help to shrink the tumor and improve limb salvage rates after primary surgical resection. In addition, neoadjuvant therapy leads to the meaningful downstaging of the extent of surgery, resulting in sparing of nerves and muscle groups. Both the reduction in limb amputations and improvement in limb function would result in improved functional outcomes for patients; significantly improving their quality of life. A second potential benefit of neoadjuvant therapy is an improvement in the rate of achievement of negative surgical resection margins, as positive margins are associated with increased risk of local recurrence and worse survival [15, 17–19, 23, 35–37]. Third, neoadjuvant therapy may result in improved local and distant recurrence-free survival as well as improved disease-specific and overall survival by eradication of micrometastatic disease. Since at least 50 % of high-grade soft tissue sarcomas recur, despite adequate treatment at the primary site, recurrence must be the result of undetectable metastatic disease at diagnosis, and earlier initiation of chemotherapy may be more effective in this “low-volume” disease, ideally increasing the chance of cure. Finally, pathologic examination of tumors after neoadjuvant chemotherapy can determine tumor response to therapy. A significant response to neoadjuvant therapy may correlate with outcomes, and be useful as an additional prognostic factor. This methodology is currently useful in osteosarcomas [38]. If there is a poor response to neoadjuvant therapy, at the very least this indicates that a change in the type of chemotherapy in an adjuvant or post-recurrence setting is required. This strategy is currently under investigation in pediatric osteosarcomas [39]. Overall, there are many theoretical benefits of neoadjuvant therapy. However, many difficulties remain.
This article will review the issues and difficulties that exist in the current interpretation of data in the use of neoadjuvant therapy in soft tissue sarcomas. The current state of evidence for the use of neoadjuvant therapy, chemotherapy alone and chemotherapy in combination with radiation therapy in soft tissue sarcomas will be reviewed. Recommendation for future trial and research will be made.
Materials and methods
An in-depth literature search was conducted using Ovid Medline and PubMed using the search terms of sarcomas, soft tissue sarcoma, neoadjuvant, adjuvant, chemotherapy, radiation, concurrent chemoradiation, hyperthermia, doxorubicin, ifosfamide, limb perfusion, intra-arterial, AIM, MAID, and epirubicin.
Issues with neoadjuvant therapy
Patient selection
There are a variety of factors to consider when including a patient in neoadjuvant therapy trials. One difficulty in current neoadjuvant therapy trials is the differences in the patient inclusion criteria. Patients with a higher risk of local or distant recurrences should be included in these trials, but what constitutes a “high-risk patient”? Certainly, patients with higher-grade tumors are at increased risk [24]. However, there is no universal soft tissue grading system. The two most commonly used systems are the national cancer institute (NCI) grading system, and the Federation Nationale des Centres de Lutte Contre le Cancer (FNCLCC) grading system. Both of these systems divide patients into three groups, low grade or grade 1, intermediate grade or grade 2, and high grade or grade 3, and are roughly equivalent in predicting patient outcomes [40]. Patients with low-grade tumors are at the lowest risk of recurrence and need not be included in neoadjuvant therapy trials. Conversely, high-grade patients are at the highest risk of recurrence and are the obvious candidates for neoadjuvant therapy trials. Patients with intermediate grade tumors have a 70 % 5-year overall survival [40]. So, the majority of these patients may not derive benefit from neoadjuvant therapy, though there is no universal agreement on this point. Additionally, given differences in pathology interpretation, any neoadjuvant therapy trial in soft tissue sarcomas should include a centralized pathology review to ensure concordance among grade determination.
Tumor size is an important prognostic factor as well. Patients with a large tumor >5 cm are at significantly increased risk of recurrence [24]. In fact, increasing tumor size correlates with worsening patient survival [13]. However, what tumor size constitutes the highest risk of recurrence and thus inclusion in neoadjuvant therapy trials has not yet been determined. Size cutoffs previously used included ≥5, ≥8, or ≥10 cm. Patients with greater than 5 cm have a ~50 % [13] chance of tumor recurrence. So, while some of these patients may benefit from neoadjuvant therapy in hopes to improve their chances of cure, 50 % of patients will be unnecessarily exposed to the short-term and long-term consequences of neoadjuvant therapy. A tumor size cutoff of ≥8 or ≥10 cm may be more appropriate for neoadjuvant studies. Soft tissue sarcoma staging is simply a marker for tumor depth, size, and grade [41]. Thus, only patients with high grade and large tumors, which corresponds to stage II and III patients, should be included in these trials.
Other important patient selection criteria include tumor location, histologic subtype, surgical criteria, and patient characteristics. Adjuvant chemotherapy is potentially beneficial in extremity soft tissue sarcomas [10]. Many neoadjuvant therapy trials are limited to patients with extremity or trunk sarcomas. However, is there an intrinsic difference in tumor biology at one location or another, or is the difference in outcomes by tumor location a result of the differences in being able to obtain an adequate surgical resection? Sarcomas located in the abdomen, retroperitoneum, thorax or head and neck represent more surgically challenging cases than those located in the extremities or trunk. If the latter is the case, then perhaps patients with non-extremity/trunk soft tissue sarcomas may derive an increased benefit from neoadjuvant chemotherapy. The type of tumor locations to include in neoadjuvant therapy trials should be evaluated on a per-trial basis, depending on the proposed intervention.
There are many histologic subtypes of soft tissue sarcomas, some of which are intrinsically more sensitive to chemotherapy than other subtypes, such as synovial sarcoma and angiosarcoma. Any neoadjuvant therapy trial will likely include a heterogeneous population of soft tissue sarcomas, and differences in the chemoresponsiveness of different tumors must be accounted for in the pre-planned subgroup analysis.
The surgical selection criteria for neoadjuvant therapy trials vary greatly, and, unfortunately, there is no current consensus for the ideal soft tissue sarcoma patient from a surgical perspective. Most patients who are candidates for limb salvage operations would be candidates for neoadjuvant therapies. However, which patients are considered able to undergo limb salvage operations is a very surgeon-dependent, subjective decision.
Also, any treatment, surgical, radiation, or chemotherapy will have its complications and side effects. Patients will have to be healthy enough, with intact organ function, and intact functional status, to be able to tolerate such an intensive therapy. Given that differences in organ function and functional status can vary among patients of the same age, age should not be used to exclude patients from neoadjuvant trials. Rather a patient’s functional status and expected organ reserve should be used as markers to predict their ability to handle intensive chemotherapy and radiation, and thus their suitability for neoadjuvant therapy trials.
Overall patients with high-grade tumors, ≥5 cm tumors, stage II or III patients, who have adequate functional status and organ status, and are candidates for limb salvage, should be considered for neoadjuvant therapy trials. However, this is still a rough estimate of which patients are at “high risk.” A nomogram, including age, size, depth, grade, location, and histologic subtype, for postoperative 12-year sarcoma-specific death, has been developed by Memorial Sloan-Kettering Cancer Center [42]. This nomogram has been adapted to include a three-tier grading system [43]. It has also been prospectively validated in a separate cohort [44]. This nomogram provides an estimation of the postoperative 12-year risk of death from soft tissue sarcomas. Perhaps a similar methodology needs to be applied to neoadjuvant therapy trials, with pre-planned subgroup analysis for tumor size, grade, location, and histologic subtype. With an eventual plan for the development of preoperative nomogram that can predict the patients at high risk for recurrence, and thus, those that might be considered for neoadjuvant therapy. Unfortunately, the rarity of soft tissue sarcoma does make such an analysis difficult to accomplish.
Finally, even when appropriate inclusion criteria are defined, recruitment into neoadjuvant chemotherapy trials for soft tissue sarcomas can be challenging in such a rare disease. Patients may be treated by local oncologists with surgery, radiation or even chemotherapy, prior to presentation to a tertiary care center specialized in the treatment of soft tissue sarcomas, invalidating them for any neoadjuvant chemotherapy trial. Given the limited number of centers with expertise in soft tissue sarcomas, it is not uncommon for patients to present after initiation of therapy locally. Additionally, the financial cost of traveling to and remaining at a specialized sarcoma treatment center for purposes of undergoing a clinical trial can be limiting for many patients. Furthermore, patients may have preconceived notions regarding the effectiveness of chemotherapy for soft tissue sarcomas. Depending on whether patients believe that chemotherapy would provide a benefit, some patients may decide to spare themselves the toxicity associated with anthracycline-based regimens versus other patients may not want to be randomized to a potentially inferior treatment arm. In addition to patient derived reasons for not enrolling in sarcoma neoadjuvant therapy trials, many physicians may choose not to enroll patients. Any phase III trial in neoadjuvant chemotherapy is by necessity a multicenter study, as a single institution is unlikely to be able to accrue sufficient patients. This requires agreement among sarcoma experts with regard to the neoadjuvant therapy regimen, which can be difficult to achieve. Sarcoma physicians may have preconceived treatment philosophies and may not want to enroll patients on a neoadjuvant therapy trial which could randomize a patient to, in their view, a potentially inferior treatment. These reasons make it particularly difficult to enroll sufficient patients for neoadjuvant chemotherapy trials in soft tissue sarcomas.
Assessment of tumor response
A second difficulty in designing neoadjuvant sarcoma trials is how to assess tumor response and its correlation with improved survival. Different imaging modalities used in sarcomas are CT scans, MRI scans, and more recently PET scans. The standard response criteria employed in most clinical trials is RECIST or RECIST 1.1 [45], which defines tumor responses based solely on changes in tumor size, with partial response defined as a ≥30 % decrease from baseline and progressive disease defined as a ≥20 % increase from baseline Two retrospective series reported improvement in overall survival with tumor shrinkage [46, 47]. Conversely, increase in tumor size does not necessarily correlate with prognosis [48]. Reconciling these retrospective reports is possible, as soft tissue sarcomas may have varying responses to neoadjuvant therapy. Rarely, patients will have shrinkage of their tumors which usually does correspond to a histologic response. Patients with an increase in their tumor size may still have a pathologic response, with tumor swelling from cystic transformation, hemorrhage or necrosis [49]. Thus, RECIST or RECIST 1.1 may be inadequate for assessment of response in soft tissue sarcomas [50].
Alternative response criteria utilize density changes on CT scan or FDG changes on PET scan. Both of these modalities have been studied in retrospective reports in soft tissue sarcoma. Choi criteria are based on changes in tumor size and tumor density on CT scan [51]. Choi criteria are used in the assessment of response of gastrointestinal stromal tumors to tyrosine kinase inhibitor therapy [52]. Choi criteria have been shown to correlate better with pathologic response than RECIST in a retrospective series of 37 patients, though response did not correlate with progression-free survival or overall survival [53]. A follow-up retrospective analysis of 69 patients treated on a phase III trial of neoadjuvant chemotherapy with epirubicin/ifosfamide showed improved correlation of overall survival with Choi criteria versus RECIST [54]. In fact, Choi criteria may better differentiate between patients with stable disease versus progressive disease [55]. However, these reports are limited by their small sample size and retrospective nature. No prospective validation of Choi criteria versus RECIST in soft tissue sarcomas exists. At the present time, Choi criteria cannot replace RECIST in the radiographic assessment of tumor response in soft tissue sarcomas. An appropriate strategy is to include both RECIST 1.1 and Choi criteria on future prospective trials of neoadjuvant chemotherapy in soft tissue sarcomas.
Another alternative imaging modality to assess tumor response is PET scans. Early metabolic response to neoadjuvant chemotherapy as determined by PET may correlate with improved tumor survival [56, 57]. However, which PET criterion is the best predictor of response to therapy and overall survival in soft tissue sarcoma has yet to be determined. One retrospective report showed that a >35 % reduction in FDG uptake had a sensitivity of 100 % for a histopathologic response, defined as ≥95 % pathologic necrosis, and a specificity of 67 % [58]. A second retrospective report showed that patients with an SUV max of ≥6 and a <40 % decrease in FDG uptake were at a high risk of recurrence, ~90 % at 4 years, versus those with a ≥40 % decrease in FDG uptake [59]. These reports are intriguing, but limited by their small sample size and retrospective nature. Future studies are required to evaluate the role of PET imaging in neoadjuvant soft tissue sarcoma trials. The EORTC defines complete metabolic response (CMR) as complete resolution of 18F-FDG uptake, partial metabolic response (PMR) as a reduction of 15 ± 25 % in tumor 18F-FDG SUV after one cycle of chemotherapy and >25 % reduction after more than one cycle of chemotherapy, stable metabolic disease (SMD) as a <25 % increase or <15 % decrease in tumor 18F-FDG SUV, and progressive metabolic disease (PMD) as a >25 % increase in tumor 18F-FDG SUV [50]. PET response criteria in solid tumors (PERCIST) have, also, been defined. PERCIST defines CMR as complete resolution of 18F-FDG uptake as compared to mean SUV uptake in the liver or surrounding background blood-pool. PMR as a 30 % reduction in tumor 18F-FDG SUV, SMD as not meeting criteria for CMR, PMR, or PMD, and PMD as a >30 % increase in tumor 18F-FDG SUV [50]. No prospective validation of PERCIST or EORTC PET response criteria versus RECIST in soft tissue sarcomas currently exists, but these are standardized criteria for assessing response on PET scans, which can be applied to future soft tissue sarcoma neoadjuvant clinical trials. A significant downside to the use of PET scans is the added cost of PET imaging versus contrast enhanced CT scan, ~250.00 versus ~700.00 € [60]. The added financial cost of including PET scans in neoadjuvant therapy trials must be considered.
Unfortunately, most neoadjuvant therapy trials have shown the development of progressive disease in ~10 % of patients. These patients may lose the chance for a limb salvage operation or cure, and do not derive any benefit from neoadjuvant therapy due to non-responsiveness of their disease. Currently, RECIST is inadequate in determining which patients will be treatment failures, as an increase in size does not correlate with prognosis [48]. Furthermore, conventional radiographic findings with CT or MRI are not concordant with pathologic findings [61–63]. Choi criteria may have improved correlation with pathologic response than RECIST [53, 54]. As noted previously, a reduction in FDG uptake from PET scans may be a better predictor of pathologic response [58]. The utility of Choi criteria or response on PET imaging to predictive pathologic response has to be prospectively validated in future clinical trials.
An additional problem is that pathologic response has been inconsistent in predicting survival or recurrence. Some retrospective studies reported positive [64–69] and some reported negative results [70, 71]. Typically, response was defined as percent necrosis, with different cutoffs used to define response, >90 % necrosis, >95 % necrosis, or >98 % necrosis [70]. Complicating the matter is the fact that necrosis is a component of tumor grade and has intrinsic prognosis value irrespective of neoadjuvant treatment. Many soft tissue sarcomas have extensive preexisting necrosis. It is difficult to distinguish preexisting necrosis from post-treatment necrosis [49]. Thus, necrosis may not be the best histopathologic marker to assess response to treatment. There was no previously defined histopathologic assessment for treated soft tissue sarcomas. Recently, the EORTC proposed a soft tissue sarcoma response score, with five response grades depending on the amount of stainable tumor cells: grade A no stainable tumor cells; grade B single stainable tumor cells; grade C ≥ 1 to <10 % stainable tumor cells; grade D ≥ 10 to <50 % stainable tumor cells; and grade E ≥ 50 % stainable tumor cells [49]. This histopathologic criterion may be used in future neoadjuvant therapy trials to assess pathologic response to therapy. Overall, the imaging response criteria used in neoadjuvant studies and their correlation with pathologic response and improved survival must be further studied and improved.
Outcome measures in neoadjuvant therapy trials
Similar to patient selection criteria and tumor response assessment criteria, outcome measures have greatly varied in previous neoadjuvant therapy trials. The primary outcome for all neoadjuvant therapy trials should be overall survival. It is only by this criterion that an estimation of the long-term impact of neoadjuvant therapy can be obtained. Disease-specific survival, local recurrence-free survival, distant recurrence-free survival, and progression-free survival can be included as secondary outcomes. Several neoadjuvant therapy trials have included tumor response as a surrogate marker for overall survival; however, this has yet to be definitively proven. So, it will be essential to note the rates of complete response, partial response, stable disease, and progressive disease both by radiographic and by pathologic criteria to help identify whether there is an accurate surrogate outcome for overall survival. Also, the limb salvage rates and rates of amputation should be reported in any neoadjuvant therapy trial. If the therapy is effective, then the rates of limb salvage should increase, limb functionality after surgery should improve, and the rate of amputations should decrease.
Due to the intensive nature of chemotherapy regimens used in soft tissue sarcomas, the toxicities and side effects of chemotherapy will have to be carefully assessed. The short-term toxicities, such as wound complication rate, and long-term toxicities, such as cardiomyopathy and myelodysplasia, will need to be reported, as well as the fraction of patients completing the planned chemotherapy regimen, the fraction of patients that require chemotherapy dose reductions, and the death rate from chemotherapy. Effect of chemotherapy on surgical morbidity is a concern as well. There is, at least, one retrospective report that shows neoadjuvant chemotherapy does not affect the morbidity of surgical resections [72]. So, this concern may be unfounded and should not preclude a patient from undergoing neoadjuvant chemotherapy. The inclusion of these criteria as secondary outcomes will be important in evaluating any neoadjuvant therapy trial in soft tissue sarcomas.
Choice of regimen
The choice of the neoadjuvant chemotherapy regimen is a most important variable when designing a neoadjuvant therapy trial. Neoadjuvant radiation therapy has been shown to be as effective as adjuvant radiation therapy, with a local recurrence rate of only ~10 % though radiation therapy does not influence distant recurrence or overall survival [8]. Thus, radiation therapy alone is likely to be insufficient therapy to improve cure rates. Chemotherapy must be included to improve cure rates. In deciding a neoadjuvant therapy regimen with chemotherapy, choices include chemotherapy alone, concurrent chemoradiation, or more commonly used is sequential chemotherapy and then radiation. Various chemotherapy regimens have been tried, usually anthracycline-based, which has been the most effective agent for soft tissue sarcomas since its introduction in the 1970s [73]. The most active regimen in the adjuvant setting is the combination of an anthracycline and ifosfamide [9–11] [epirubicin/ifosfamide, doxorubicin/ifosfamide/mesna (AIM)]. Both infusional doxorubicin and bolus doxorubicin were studied in the neoadjuvant setting [74]. Infusional doxorubicin is associated with a lower cardiac side-effect profile [75].
A considerable “downside” to these regimens is their significant toxicity. Patients without favorable performance status or with significant co-morbidities cannot be included in neoadjuvant chemotherapy trials. Additionally, the long-term toxicities of these regimens include acute leukemia and heart failure, which must be weighed against an uncertain contribution of these regimens to cure. In patients with more than a 50 % chance of cure, the long-term risks of these regimens may outweigh the benefits. More recently, non-anthracycline-based regimens with improved side-effect profiles include trabectedin [76] and gemcitabine/docetaxel [77, 78] which have been studied in some neoadjuvant/adjuvant sarcoma trials particularly in myxoid liposarcoma and uterine leiomyosarcoma. Eribulin was recently FDA-approved for liposarcomas, and represents another chemotherapeutic which could be moved from the metastatic to neoadjuvant setting [79]. Pazopanib was studied in the neoadjuvant setting as well as in combination with gemcitabine and docetaxel [80]. Chemotherapy used concurrently with radiation has included doxorubicin [81–85], ifosfamide [86, 87], ifosfamide and doxorubicin [88] razoxane [89], iododeoxyuridine [90, 91], temozolomide [92], bevacizumab [93], sorafenib [94], and pazopanib [95]. Additionally, intra-arterial chemotherapy and limb perfusion have been used in neoadjuvant sarcoma trials [96]. There is currently no defined superior neoadjuvant chemotherapy regimen for soft tissue sarcomas. The status of current neoadjuvant therapy trials in soft tissue sarcomas is reviewed below.
Current neoadjuvant therapy trials in soft tissue sarcomas
Neoadjuvant chemotherapy
Neoadjuvant chemotherapy has been studied in the treatment of soft tissue sarcomas since the 1980s [97]. Initial small, retrospective or single-institution experiences suggested responses to chemotherapy and a benefit to neoadjuvant chemotherapy with an improved survival in those patients who obtained a response [97–100]. However, a retrospective review of 76 patients with stage IIIb soft tissue sarcoma treated at MD Anderson Cancer Center with doxorubicin-based neoadjuvant chemotherapy, without ifosfamide, showed a 5-year disease-free survival of 52 % and a 5-year overall survival of 46 % [101]. This result was similar to results with surgery alone or postoperative chemotherapy. A larger retrospective review of 674 patients from Memorial Sloan-Kettering Cancer Center and MD Anderson Cancer Center identified 214 patients treated with neoadjuvant chemotherapy and 112 patients treated with adjuvant chemotherapy. The treatment regimens included AIM, MAID (MESNA/doxorubicin/ifosfamide/dacarbazine), doxorubicin alone, ADIC (doxorubicin/dacarbazine), and CyADIC (cyclophosphamide/doxorubicin/dacarbazine). There was an initial response to chemotherapy with improved survival in the first year, but this trend was not sustained over time. The 5-year overall disease-free survival was 47 % for patients treated with chemotherapy and 49 % for patients who received no chemotherapy [102]. These results were disappointing. The chemotherapy regimen associated with the highest response rates in the adjuvant setting is doxorubicin and ifosfamide [9]. This regimen has the highest tumor response rates of ~45–47 %, in the neoadjuvant setting, as well [103]. Further retrospective neoadjuvant chemotherapy trials have included a doxorubicin/ifosfamide-based regimen; Table 1.
A retrospective experience with the use of doxorubicin, intra-arterial cisplatin, and ifosfamide was reported by Henshaw et al. [66]. There were increased complications with arterial thrombosis and myocutaneous necrosis, but the 5-year overall survival was 88 %, a significant improvement from historical controls [66]. A more extensive retrospective experience was reported by Grobmyer et al. in 2004, with 74 patients who received an average of three cycles of AIM chemotherapy compared to 282 patients treated with surgery alone. The greatest effect of chemotherapy was seen in patients with a >10 cm tumor. The disease-specific mortality hazard ratio was 0.45 (95 % CI 0.25–0.83) for patients receiving chemotherapy, compared to those who received surgery alone. The 3-year disease-specific survival was 83 % for those receiving chemotherapy and 62 % for those with surgery alone [104]. These results support the hypothesis that patients with larger tumors do benefit, at least, upfront, from neoadjuvant therapy with a doxorubicin/ifosfamide-based regimen, though a follow-up of only 3 years is too short to determine whether the effect of chemotherapy will be long term. A further retrospective report from the French sarcoma group showed no benefit to adjuvant or neoadjuvant chemotherapy in patients with synovial sarcoma, though only 19 % of patients were treated with neoadjuvant chemotherapy, and only 59 % of the chemotherapy regimens were doxorubicin/ifosfamide-containing [105]. A retrospective study from Japan in 2013, using MAID neoadjuvant chemotherapy, showed a 5-year overall survival of 86 % and 5-year disease-free survival of 77 % for patients with grade 2 or 3 extremity or trunk STS [106]. This result compares favorably with historical controls. Overall, retrospective reviews and single-institutional experience suggest a benefit of neoadjuvant doxorubicin/ifosfamide-based chemotherapy for large, extremity STS. Unfortunately, prospective studies to confirm this have been limited, Table 1.
A phase II study reported 2001 by Gortzak et al. [107] showed a 5-year overall survival of 64 % in the surgery-alone arm compared to 65 % in the neoadjuvant chemotherapy arm, p = 0.22. There were only 67 patients in each arm, so this study may not have been appropriately powdered to detect a difference. Due to slow accrual, a planned phase III trial was never completed. In addition, lower-risk patients with <8 cm tumors or grade II tumors were included, and these patients may not have benefited from neoadjuvant chemotherapy as much as high grade or large tumors. Finally, the chemotherapy regimen used was doxorubicin 50 mg/m2 day 1 and ifosfamide 5 g/m2 as a 24 h continuous infusion day 1, a dosing schedule that was much lower when compared to the regimens used in the retrospective studies that suggested a benefit to neoadjuvant chemotherapy. A second phase II study was conducted in the pediatric population with advanced non-rhabdomyosarcoma soft tissue sarcomas using vincristine (1.5 mg/m2 weekly for 13 doses), ifosfamide (3 g/m2 daily for 3 days every 3 weeks for seven cycles), and doxorubicin (30 mg/m2 daily for 2 days for six cycles) [108]. There was no control group though the patients with clinical group III disease did have a 3-year overall survival of 80 %. The majority of patients who responded to chemotherapy had synovial sarcoma. A third phase II study conducted in Japan with adriamycin 30 mg/m2 day 1, 2 and ifosfamide 2 gm/m2 day 1–5 given for three cycles preoperatively and two cycles postoperatively showed a 5-year overall survival of 82.6 %, a promising result [109, 110]. However, a phase III randomized controlled trial of a high-dose doxorubicin/ifosfamide (AIM)-based neoadjuvant chemotherapy regimen still needs to be conducted in patients with extremity, high grade, large soft tissue sarcomas to confirm the ~80 % 5-year overall survival and if this benefit is durable.
High-dose doxorubicin and ifosfamide have considerable toxicities with risks for heart failure, acute myeloid leukemia, neutropenic fever, infection, and even death. Unfortunately, these are the most active chemotherapeutic agents in soft tissue sarcomas. A recent neoadjuvant chemotherapy phase II study of a new agent, trabectedin, in myxoid liposarcoma showed a 13 % complete pathologic response and a 24 % partial response by RECIST [76]. This agent was well tolerated. These results and the tolerability of this agent suggest that this drug should be studied further in the treatment of myxoid liposarcomas particularly in the neoadjuvant setting. Another alternative which can be applied to soft tissue sarcomas is gemcitabine/docetaxel, which has shown improved progression-free and overall survival in uterine leiomyosarcoma compared to historical controls. However, follow-up in these phase II studies was only 2–3 years [77, 78]. A phase Ib/II study of gemcitabine/docetaxel and pazopanib was conducted. However, the study was terminated early due to significant hepatic and myelotoxicity. Only five patients were enrolled, and no objective responses occurred [80].
Neoadjuvant chemotherapy with radiation
One of the important goals of neoadjuvant chemotherapy is producing a local response to decrease the extent of resection and improve the limb salvage rate. Not all patients will respond to chemotherapy, so the addition of radiation therapy to the primary tumor may rescue poor chemotherapy responders in terms of local response. Additionally, chemotherapy may potentiate the effect of radiation. Thus, the combination of chemotherapy with radiation in the neoadjuvant setting may improve local response rates and still increase the chances of a long-term cure. Chemotherapy can be given alternating with radiation therapy or concurrently. Chemotherapy regimens given sequentially with radiation include MAID, epirubicin/ifosfamide, and ifosfamide/mitomycin/doxorubicin/cisplatin (IMAP). Each of the MAID chemotherapy drugs as a single agent has a ~20 % response rate in sarcomas, so the combination is reasonable [73, 74, 111, 112]. This regimen has been studied and is active in soft tissue sarcomas. A phase II study showed an overall response rate of 47 % in advanced soft tissue sarcomas [113]. A second phase II study of MAID chemotherapy showed a 49 % response rate in adult osteosarcoma, Ewing’s sarcoma and rhabdomyosarcoma [114]. Later, a phase III study was conducted of doxorubicin and dacarbazine versus doxorubicin, ifosfamide, and dacarbazine [115]. This study showed an overall response rate of 32 % in 340 patients with significantly longer time to progression, though no difference in overall survival. Given good responses in the advanced and metastatic setting, it is reasonable to consider the use of MAID chemotherapy in the neoadjuvant setting, particularly because of the higher response rates which are important in the neoadjuvant setting before surgical resection. MAID has been studied in this setting, particularly in the Delaney experience [116–118], the RTOG 9514 trial [119, 120], and in the Ogura et al. [106] experience. These results, shown in Table 2, have been encouraging, but caution must still be advised [121].
In the initial Delaney retrospective experience, reported in 2003, 48 patients were treated with three cycles of preoperative MAID chemotherapy alternating with 44 Gy of radiation, and then three cycles of postoperative MAID chemotherapy with an additional 16 Gy of radiation for positive surgical margins. These results showed a significant improvement at 5 years in freedom from distant metastasis 75 versus 44 %, p = 0.0016, disease-free survival 70 versus 42 %, p = 0.0002, and overall survival 87 versus 58 %, p = 0.0003 compared to historical controls [116]. Only one patient developed a fatal myelodysplastic syndrome. The long-term results of this retrospective experience, reported in 2012, showed a 10-year disease-free survival of 65 % compared to 30 % in the control group p = 0.0002, and a 10-year overall survival of 66 versus 38 %, p = 0.003 [117]. While there were relapses and death from sarcoma after 5 years, the benefit of chemotherapy was still seen at 10 years. This result contradicts the Cormier et al. [102] retrospective experience which suggested that the benefit from adjuvant chemotherapy decreases with time. In an additional report from the Delaney group, a retrospective experience over 10 years of 66 patients showed a similar disease-specific survival of 89 % and overall survival of 86 % at 5 years with local recurrence of only ~10 % [118]. It should be noted that this is similar to the Ogura et al. [106] retrospective experience which had an 86 % 5-year overall survival. There are differences between these two experiences, in particular only six patients received preoperative radiation therapy in addition to chemotherapy, and nine patients received postoperative chemotherapy, out of a total of 40 patients. Also, while the total dose of doxorubicin per cycle was 60 mg/m2, in both reports the amount of ifosfamide per cycle 7.5 versus 6 gm/m2 and dacarbazine per cycle 900 versus 1000 mg/m2 is different between the Ogura and Delany retrospective experiences. Despite these differences, outcomes were similar.
An additional phase II study with similar “sandwiching” of chemotherapy and radiation was conducted by the radiation therapy oncology group, RTOG 9514. Short-term results at 3 years showed a disease-free survival of 56.6 %, distant disease-free survival of 64.5 %, and overall survival of 75.1 % [119]. Longer-term results at 5 years showed a disease-free survival of 56.1 %, distant disease-free survival of 64.1 %, and overall survival of 71.2 % [120]. These results are slightly inferior to the Delany or Ogura retrospective experiences. Two possible explanations are the chemotherapy completion rate, which was 83 % in the Delany retrospective experience and only 59 % in the RTOG study, or the chemotherapy doses. There was significantly more toxicity in the RTOG trial with three treatment-related deaths, one from infection, and two from acute leukemia. The RTOG trial used 7.5 gm/m2 of Ifosfamide per cycle compared to the Delany retrospective experience of 6 gm/m2, and only 675 mg/m2 of dacarbazine compared to 1000 mg/m2 in the Delany retrospective experience. In addition, these are small phase II studies and difference in outcome could be due to patient selection or random chance.
Overall, the Delany retrospective experience, the Ogura retrospective experience, and the RTOG Phase II trial suggest that in appropriately selected patients, the neoadjuvant use of MAID chemotherapy with radiation can improve local control with only an ~10 % failure rate, and produce a durable overall survival benefit, ~70–80 % at 5 years which is an improvement compared to historical controls. Historically, patients with large ≥8 cm high-grade tumors are predicted to have only a ~50 % 5 year overall survival. Despite these encouraging results, problems do still exist. These trials were small or retrospective, so prone to error from selection bias. Particularly in the Delany retrospective experience, the control group differed from the treatment group in terms of the portion of grade 2 and 3 tumors and by tumor histologic subtype [118]. A phase III trial that would eliminate such difficulties has not yet been conducted, but would be helpful in proving the benefit of this neoadjuvant approach.
Questions remain in the design of such a trial. With respect to patient selection, patients with large primary tumors should be included, but whether this should be limited to grade 3 tumors, which are at highest risk of recurrence or grade 2 and 3 tumors, is problematic. Furthermore, should large tumors be defined as ≥5, ≥8, or ≥10 cm. Additionally, only 15 patients in the Ogura retrospective experience received radiation, but 5-year overall survival was similar to the Delany retrospective experience. So, is radiation necessary in all patients or just those with positive margins, and when is the best timing of radiation? Furthermore, is dacarbazine necessary, as a neoadjuvant chemotherapy alone trial with only doxorubicin and ifosfamide showed a similar ~80 % 5 year overall survival [110]. Excluding dacarbazine would allow optimization of the dose of the two most active agents, doxorubicin and ifosfamide. Additionally, the dosing of dacarbazine and ifosfamide differed between these small studies. The best balance between chemotherapy dose and toxicity is unknown. Certainly, high doses of doxorubicin, ifosfamide and dacarbazine are required to produce a higher response rate in soft tissue sarcomas, but higher doses predictably lead to more toxicity and a lower therapy completion rate which may produce inferior outcomes. All of these questions remain unanswered, and given different preferences at different sarcoma centers and the need for a phase III trial in sarcomas to be a multicenter affair, a phase III trial with MAID or AIM chemotherapy is unlikely to be undertaken.
Further circumstantial evidence for the utility of a combined neoadjuvant radiation and chemotherapy approach comes from two phase II trials and one phase III trial with IMAP and epirubicin and ifosfamide. In 2001, Edmonson et al. [122] reported the results of a phase II trial of preoperative ifosfamide, mitomycin, doxorubicin and cisplatin for two cycles and 45 Gy of radiation, with three cycles of postoperative mitomycin, doxorubicin, and ifosfamide with a postoperative radiation boost to a total of 65 Gy. Local recurrence-free survival at 5 years was 92 %, and 5-year overall survival was 80 %, comparable to the Delany and Ogura retrospective experiences. In 2008, Ryan et al. [123] reported a phase II trial of epirubicin and ifosfamide for 25 patients with intermediate or high-grade >5 cm soft tissue sarcomas. Two-year overall survival was 84 %, and the toxicity of the regimen was similar to other neoadjuvant therapy trials. Later, a phase III trial of epirubicin and ifosfamide was conducted by Gronchi et al. [124, 125]. In this trial, patients received three cycles of preoperative chemotherapy with epirubicin 120 mg/m2 per cycle and Ifosfamide 9 gm/m2 per cycle and were then randomized to receive two further postoperative cycles of chemotherapy. Radiation was delivered either preoperatively or postoperatively. Five-year overall survival was 73 %, and the addition of two cycles of postoperative chemotherapy did not influence outcomes. These trials suggest alternative chemotherapy regimens that can have similar efficacy as MAID or AIM chemotherapy though still do not represent conclusive phase III randomized controlled evidence of the benefit of the neoadjuvant radiation and chemotherapy as compared to adjuvant chemotherapy or just radiation therapy alone. None of these results can be considered practice changing, and there remains no standard of care for neoadjuvant therapy in soft tissue sarcomas. Despite this, it is reasonable to consider treating a healthy high-risk (≥5–10 cm, extremity, high grade) sarcoma patients per these protocols, after discussing the risks and potential benefits with the patient, in an attempt to improve their overall survival.
Neoadjuvant concurrent chemotherapy
Undoubtedly, there will be those patients that choose to forgo neoadjuvant chemotherapy due to patient preference or concerns related to toxicity and those patients with too many co-morbid medical conditions. Most of those patients will receive radiation therapy alone. However, this may not be sufficient to reduce local recurrence, improve surgical outcomes, and limb salvage rates. An alternative strategy is to use radiation concurrently with chemotherapy. Though this may help local response, the doses of chemotherapy used are unlikely to affect distance recurrences. Trials using concurrent chemoradiation in soft tissue sarcomas are listed in Table 3. The first agents studied concurrently with radiation include the chemotherapeutic agents with the highest response rates in sarcoma, doxorubicin, and ifosfamide. Using low-dose doxorubicin 4 mg/m2 bolus and then daily continuous infusion for 4 days concurrently with radiation was shown to be feasible with acceptable toxicities, though with few complete responses [81, 82]. Increasing the dose of doxorubicin to 12 mg/m2 per day does increase the response rate to a complete response rate of 11 % and partial response rate of 56 % [83]. This result, however, has not yet been shown to improve clinical outcomes. In fact, a phase II study of concurrent doxorubicin with radiation had a 5-year overall survival of only 63 % [84]. Ifosfamide has been tried currently with radiation as well. A retrospective study showed a pathologic complete response rate of 14 % and >90 % necrosis in another 43 % with ifosfamide concurrently with radiation [86]. A prospective phase I/II study, however, only showed a radiographic response rate of 8 % and 5-year overall survival of 59 % [87]. In a combination approach, a retrospective series of concurrent doxorubicin with radiation followed by adjuvant doxorubicin and ifosfamide had only a 58.3 % 5-year overall survival [85]. These studies do not indicate improved outcomes with the use of concurrent doxorubicin or ifosfamide. A German phase I/II study 60–64 Gy of radiation with doxorubicin 50 mg/m2 on day 2 and day 30 and ifosfamide 1.5 gm/m2 on days 1–5 and 29–33 showed an 83 % 3-year overall survival [88]. These doses of doxorubicin and ifosfamide are higher than those used in the other concurrent chemoradiation trials, though lower than the neoadjuvant MAID regimens discussed above. These phase II and retrospective reports seem to indicate that it is the dosing of doxorubicin and ifosfamide that matter, rather than the use concurrently with radiation. This outcome supports the hypothesis that the best use of doxorubicin and ifosfamide is alternating with radiation, as a higher dosing of these medications can be obtained with acceptable toxicity when dosed separately from radiation.
With a lack of significant improvement in local response with doxorubicin and ifosfamide concurrently with radiation, newer chemotherapeutic agents have been studied concurrently with radiation. Unfortunately, these agents have failed to show a benefit over radiation alone, Table 3. Razoxane is a radio-sensitizer. In a phase III trial, razoxane 150 mg/m2 was given orally during radiation compared to radiation alone. There was no difference in local control or overall survival of 65 % in the radiation alone group and 55 % in the radiation plus razoxane group [89]. Another radio-sensitizer iododeoxyuridine was tested in two early-phase clinical trials, but no significant improvement in local responses was seen, and overall survival was only 39 % [90] and 16.6 % [91]. Additionally, temozolomide [92], bevacizumab [93], sorafenib [94] and pazopanib [95] were studied in combination with radiation therapy in small phase I or phase II trials. In particular sorafenib combined with radiation showed near-complete pathologic response (pCR) in 38 % of patients and pazopanib combined with radiation showed near pCR in 40 % of patients, with near pCR defined as necrosis greater than 95 % [94, 95]. These regimens were well tolerated, and improvements in local responses were suggested but have yet to be tested in a randomized controlled setting. An alternative approach is the inclusion of immunotherapy. A phase I/II trial tested the feasibility of intratumoral injection of dendritic cells during radiation therapy [126]. An immune response was induced in ~50 % of patients, but overall survival at 3 years was only 23.5 %. However, the approach of combining immunotherapy with radiation therapy does warrant further study in future clinical trials. Overall, the experience with concurrent chemoradiation using doxorubicin, ifosfamide, radio-sensitizers (razoxane, iododeoxyuridine) or newer agents (temozolomide, bevacizumab, sorafenib, pazopanib) has shown no definitive benefit over radiation alone, or chemotherapy alternating with radiation. It is still worthwhile conducting studies of concurrent chemoradiation, particularly with sorafenib or pazopanib, or concurrent immunotherapy and radiation in hopes to improve local response rates, but these regimens can only be considered investigational and not standard therapies at this time.
Neoadjuvant chemotherapy with radiation and regional hyperthermia
A further therapy under investigation is the addition of regional hyperthermia to neoadjuvant radiation and chemotherapy, Table 3. Radiation with neoadjuvant chemotherapy, etoposide, doxorubicin, and ifosfamide has been combined with regional hyperthermia in two phase II trials. The first included high-grade soft tissue sarcomas >8 cm and showed a response rate of 17 % with a 5-year overall survival of 49 % [127]. The second included high-grade retroperitoneal and visceral sarcomas and showed a response rate of 13 % with a 5-year overall survival of 32 % [128]. Neither of these studies showed a dramatic improvement in local response rates or long-term survival with the addition of regional hyperthermia. A third retrospective review of 28 patients who received radiation ± concurrent ifosfamide ± regional hyperthermia showed a 3-year overall survival of 72 % and no difference in local control rates with the addition of regional hyperthermia [129]. Thus, regional hyperthermia by itself does not add significantly to local control of soft tissue sarcomas.
Neoadjuvant intra-arterial chemotherapy and isolated limb perfusion therapy
Another method to improve local response rates in soft tissue sarcomas is the use of intra-arterial chemotherapy. This technique has been applied since the 1970s [96], with the use of agents such as doxorubicin, cisplatin, and melphalan [130]. The use of intra-arterial doxorubicin chemotherapy has shown a reasonable local response rate, but this comes at a price, with significant local toxicities. The southeastern cancer study group showed a 95 % limb salvage rate and 98.5 % local control rate with 90 mg of intra-arterial doxorubicin and 30–45 Gy of radiation [131–133]. However, the postoperative wound complication occurred in 41 % of patients [132]. Additionally, 54 % of patients developed distant disease, and the 5-year overall survival was 59 % [132]. These results are not clearly superior to historical controls. The addition of hyperthermic limb perfusion with intra-arterial doxorubicin or cisplatin and radiation has shown improved local responses 94–98 % and limb preservation rates of 91–97 % [134–136]. Again, overall survival is not clearly improved, with a median overall survival of 12 months in one phase II study [135]. However, there have been no randomized controlled trials that have compared intra-arterial chemotherapy and radiation or intra-arterial limb hyperthermic perfusion and radiation to neoadjuvant or adjuvant sequential high-dose chemotherapy and radiation.
Further advances in loco-regional therapy lead to the development of isolated limb perfusion (ILP) [137]. Such a technique allows for higher concentrations of chemotherapy, as long as exposure to the systemic circulation is limited. The inclusion of tumor necrosis alpha in regional limb perfusion increased local response rates in soft tissue sarcomas to 82 % [138, 139]. Standard dosing of TNFα is 1 mg, as higher doses increase toxicity, but not response [140–142]. This technique is limited by significant toxicities including delayed wound healing, wound infections, tissue fibrosis, sensor and motor neuropathies, lymphoceles, and arterial thrombosis [138, 143]. These complications can be severe enough to require limb amputation [144]. The Wieberdink scale grades toxicity from grade I no reaction, grade II mild edema and hyperemia, grade III severe edema and blistering, grade IV epidermolysis and compartment syndrome, to grade V tissue necrosis and amputation. Local toxicity is lower with melphalan-based versus doxorubicin-based TNFα ILP [145]. Grade IV and grade V reactions occur in 2–7.5 % of patients treated with melphalan-based TNFα ILP versus ~10 % in doxorubicin-based TNFα ILP with a TNFα dosing of 1 mg [144, 146–148]. Additional toxicity results from systemic leakage. Reports of systemic leakage vary from 2 to 13 % [145, 149]. Systemic exposure to chemotherapy can lead to cytopenias, and systemic exposure to TNFα can lead to hypotension and shock.
Counterbalancing these severe toxicities is improved local response rates, limb salvage rates, and decrease in local recurrence. In retrospective series of 186 patients with grade II or III soft tissue sarcomas, with median tumor size of 16 cm, treatment with hyperthermic isolated limb perfusion with melphalan and TNFα leads to a radiograph complete response of 18 %, partial response of 57 %, and stable disease of 22 % [146]. The limb salvage rate was 82 % [146]. Another retrospective series of 106 patients treated with doxorubicin and TNFα ILP showed a 22 % complete response, 77 % partial response, and 77 % limb salvage rate [148]. Many of these patients would have required amputation prior to treatment with ILP. The addition of radiation after ILP significantly improves local control rates, 96 versus 52 % in one retrospective series of 77 patients [150]. These retrospective studies have led to the approval of ILP with TNFα in Europe for soft tissue sarcomas.
However, there have been no randomized controlled trials that have compared isolated limb perfusion therapy with doxorubicin or melphalan ± radiation and TNFα to neoadjuvant or adjuvant sequential high-dose chemotherapy and radiation. The majority of patients with soft tissue sarcomas die from metastatic disease, not local recurrence. Loco-regional therapies, such as ILP with melphalan and TNFα, may be effective in increasing local response rates (63–91 %) leading to limb salvage operations (58–97 %) particularly in the setting of large tumors [145]. This limb salvage rate is not definitely improved compared to sequential radiation and chemotherapy, especially in the absence of a randomized trial. Furthermore, the goal of neoadjuvant therapy in soft tissue sarcomas is not only tumor response and limb salvage, but also to cure the patient. Loco-regional therapies such as ILP do not have improved overall survival (40–60 %) compared to historical controls [147, 150]. Retrospective neoadjuvant chemotherapy trials with an anthracycline and ifosfamide do suggest an improved survival compared to historical controls (60–80 %). Without an improvement in overall survival, the increased toxicities associated with ILP are hard to justify in most patients. Additionally, TNFα, arguable the most important agent in ILP, is not approved in the USA. Thus, ILP is rarely performed in the USA. TNFα ILP was approved in Europe for the treatment of advanced soft tissue sarcomas in 1988 [145]. ILP with TNFα is used in many specialized European centers experienced with its delivery for soft tissue sarcoma patients with large, extremity, non-operable tumors. ILP with TNFα has been reported not to impact the ability to give high-dose systemic chemotherapy [151, 152]. The role of ILP with TNFα may be in soft tissue sarcoma patients with large, extremity, tumors that are still in-operable after high-dose chemotherapy and radiation. However, this needs to be studied in a randomized fashion.
Conclusions
The long-term mortality from soft tissue sarcomas despite surgical resection and adjuvant or neoadjuvant radiation remains unacceptable high. Better strategies are required in high-risk patients, those with large and high-grade tumors who have a <50 % 5-year overall survival. Neoadjuvant chemotherapy offers the potential benefit of improved long-term survival [153–155]. There is no universally accepted neoadjuvant therapy standard of care. Based on retrospective series and phase II trials, neoadjuvant therapy with doxorubicin and ifosfamide (AIM), epirubicin and ifosfamide, or doxorubicin, ifosfamide and dacarbazine (MAID) with or without radiation therapy are possible treatment options. These small studies suggest improved survival in high-risk patients compared to historical controls to 70–80 % at 5 years. However, there is a lack of randomized phase III trials comparing these regimens to each other and to observation alone, which would prove a benefit. Additionally, unanswered questions which remain are the benefit of dacarbazine when added to ifosfamide and an anthracycline, and the timing of radiation therapy in regards to neoadjuvant chemotherapy. Another complication is the toxicity of these regimens and inability of older patients or patients with multiple medical co-morbidities to tolerate these regimens. Further, investigation of regimens with lower side-effect profiles, such as gemcitabine/docetaxel, trabectedin, eribulin, pazopanib or sorafenib in the neoadjuvant setting, is required. Overall treatment decisions must be individualized between the patient and provider. There is a role for neoadjuvant chemotherapy in select patients. Neoadjuvant chemotherapy with or without radiation should, at least, be considered in patients with high-risk disease, large (>5 or >8 cm), high-grade, extremity tumors, who are young and healthy enough to be able to tolerate the neoadjuvant chemotherapy. However, without randomized controlled trial evidence, the routine use of neoadjuvant chemotherapy cannot be recommended in all patients with soft tissue sarcomas.
The use of radiation should be considered in all high-risk patients to decrease the risk of local recurrence, but this is unlikely to affect overall survival, and radiation can be delivered in a neoadjuvant or adjuvant fashion. For older patients with more medical co-morbidities, who would not be able to tolerate AIM or MAID chemotherapy, current evidence does not support a definitive benefit for lower-toxicity treatments, such has concurrent chemoradiation and cannot be recommended at this time. Additionally, limb perfusion in soft tissue sarcomas has not been studied in randomized clinical trials and has the cost of significant toxicity. These treatment strategies cannot be recommended in the USA outside of the context of a clinical trial.
Future directions to improve our treatment of soft tissue sarcomas would be to conduct phase III randomized controlled trials to definitively answer the question of whether neoadjuvant chemotherapy with the AIM or MAID regimens results in an overall survival benefit as well as directly compare these regimens to determine the added benefit of dacarbazine. Though, conducting such trials in a rare very heterogeneous disease, without an agreement on what constitutes high-risk patients, can be quite challenging. Furthermore, as new techniques and strategies are being applied to the metastatic setting, such as recently FDA-approved trabectedin, eribulin, pazopanib, or immunotherapy, those that show a significant benefit will need to be applied to the adjuvant and neoadjuvant setting. Currently, the Italian, Spanish and French Sarcoma groups are enrolling a histology tailored phase III neoadjuvant chemotherapy trial comparing epirubicin (120 mg/m2) and ifosfamide (9 gm/m2) to gemcitabine/docetaxel (900, 75 mg/m2) in undifferentiated pleomorphic sarcoma, trabectedin (1.3 mg/m2) in myxoid liposarcomas, high-dose ifosfamide (14 mg/m2) in synovial sarcoma, ifosfamide/etoposide (9 gm/m2, 450 mg/m2) for malignant peripheral nerve sheath tumor, and gemcitabine/dacarbazine (1800, 500 mg/m2) for leiomyosarcoma, NCT01710176. Immunotherapy may permit improved overall survival with limited toxicity. The effectiveness of immunotherapy in the metastatic setting of soft tissue sarcomas is currently being studied. We await the results of these trials with great anticipation.
References
Siegel R, Ma J, Zou Z, Jemal A (2014) Cancer statistics, 2014. CA Cancer J Clin 64(1):9–29. doi:10.3322/caac.21208
WHO Classification of Tumours of Soft Tissue and Bone (2013) World Health Organization classification of tumours, 4th edn. International Agency for Research on Cancer (IARC), Lyon
SEER Cancer Statistics Review, 1975–2012 (2015) National cancer institute. http://seer.cancer.gov/csr/1975_2012/. Accessed Apr 2015
Hueman MT, Thornton K, Herman JM, Ahuja N (2008) Management of extremity soft tissue sarcomas. Surg Clin N Am 88(3):539–557. doi:10.1016/j.suc.2008.04.003
Ravo V, Marrone I, Morra A, Manzo R, Murino P, Cammarota F, Muto P (2010) Multimodality treatment of locally advanced soft-tissue sarcomas of the extremities. Rep Pract Oncol Radiother 15(5):119–124. doi:10.1016/j.rpor.2010.08.006
Strander H, Turesson I, Cavallin-ståhl E (2003) A systematic overview of radiation therapy effects in soft tissue sarcomas. Acta Oncol 42(5–6):516–531. doi:10.1080/02841860310014732
NCCN Clinical Practice Guidelines in Oncology: Soft Tissue Sarcoma (2014) National comprehensive cancer network. http://www.nccn.org/professionals/physician_gls/pdf/sarcoma.pdf. Accessed 23 Jan 2016
O’Sullivan B, Davis AM, Turcotte R, Bell R, Catton C, Chabot P, Wunder J, Kandel R, Goddard K, Sadura A, Pater J, Zee B (2002) Preoperative versus postoperative radiotherapy in soft-tissue sarcoma of the limbs: a randomised trial. The Lancet 359(9325):2235–2241. doi:10.1016/s0140-6736(02)09292-9
Woll PJ, Reichardt P, Le Cesne A, Bonvalot S, Azzarelli A, Hoekstra HJ, Leahy M, Van Coevorden F, Verweij J, Hogendoorn PCW, Ouali M, Marreaud S, Bramwell VHC, Hohenberger P (2012) Adjuvant chemotherapy with doxorubicin, ifosfamide, and lenograstim for resected soft-tissue sarcoma (EORTC 62931): a multicentre randomised controlled trial. Lancet Oncol 13(10):1045–1054. doi:10.1016/s1470-2045(12)70346-7
Tierney JF, Stewart LA, Parmar MKB, Fletcher CD, Jones G, Mosseri V, Patel M, Ruiz de Elvira MC, Souhami RL, Stewart LA, Sylvester R, Tursz T (1997) Adjuvant chemotherapy for localised resectable soft-tissue sarcoma of adults: meta-analysis of individual data. The Lancet 350(9092):1647–1654. doi:10.1016/s0140-6736(97)08165-8
Pervaiz N, Colterjohn N, Farrokhyar F, Tozer R, Figueredo A, Ghert M (2008) A systematic meta-analysis of randomized controlled trials of adjuvant chemotherapy for localized resectable soft-tissue sarcoma. Cancer 113(3):573–581. doi:10.1002/cncr.23592
Coindre JM, Terrier P, Bui NB, Bonichon F, Collin F, Le Doussal V, Mandard AM, Vilain MO, Jacquemier J, Duplay H, Sastre X, Barlier C, Henry-Amar M, Mace-Lesech J, Contesso G (1996) Prognostic factors in adult patients with locally controlled soft tissue sarcoma. A study of 546 patients from the French Federation of Cancer Centers Sarcoma Group. J Clin Oncol 14(3):869–877
Coindre JM, Terrier P, Guillou L, Le Doussal V, Collin F, Ranchere D, Sastre X, Vilain MO, Bonichon F, N’Guyen Bui B (2001) Predictive value of grade for metastasis development in the main histologic types of adult soft tissue sarcomas: a study of 1240 patients from the French Federation of Cancer Centers Sarcoma Group. Cancer 91(10):1914–1926
Collin CF, Friedrich C, Godbold J, Hajdu S, Brennan MF (1988) Prognostic factors for local recurrence and survival in patients with localized extremity soft-tissue sarcoma. Semin Surg Oncol 4(1):30–37
Le Doussal V, Coindre JM, Leroux A, Hacene K, Terrier P, Bui NB, Bonichon F, Collin F, Mandard AM, Contesso G (1996) Prognostic factors for patients with localized primary malignant fibrous histiocytoma: a multicenter study of 216 patients with multivariate analysis. Cancer 77(9):1823–1830. doi:10.1002/(SICI)1097-0142(19960501)77:9<1823:AID-CNCR10>3.0.CO;2-1
LeVay J, O’Sullivan B, Catton C, Bell R, Fornasier V, Cummings B, Hao Y, Warr D, Quirt I (1993) Outcome and prognostic factors in soft tissue sarcoma in the adult. Int J Radiat Oncol Biol Phys 27(5):1091–1099
Mandard AM, Petiot JF, Marnay J, Mandard JC, Chasle J, de Ranieri E, Dupin P, Herlin P, de Ranieri J, Tanguy A et al (1989) Prognostic factors in soft tissue sarcomas. A multivariate analysis of 109 cases. Cancer 63(7):1437–1451
Markhede G, Angervall L, Stener B (1982) A multivariate analysis of the prognosis after surgical treatment of malignant soft-tissue tumors. Cancer 49(8):1721–1733
Pisters PW, Leung DH, Woodruff J, Shi W, Brennan MF (1996) Analysis of prognostic factors in 1,041 patients with localized soft tissue sarcomas of the extremities. J Clin Oncol 14(5):1679–1689
Rooser B, Attewell R, Berg NO, Rydholm A (1987) Survival in soft tissue sarcoma. Prognostic variables identified by multivariate analysis. Acta Orthop Scand 58(5):516–522
Singer S, Corson JM, Gonin R, Labow B, Eberlein TJ (1994) Prognostic factors predictive of survival and local recurrence for extremity soft tissue sarcoma. Ann Surg 219(2):165–173
Trovik CS, Bauer HC, Alvegard TA, Anderson H, Blomqvist C, Berlin O, Gustafson P, Saeter G, Walloe A (2000) Surgical margins, local recurrence and metastasis in soft tissue sarcomas: 559 surgically-treated patients from the Scandinavian Sarcoma Group Register. Eur J Cancer 36(6):710–716
Vraa S, Keller J, Nielsen OS, Sneppen O, Jurik AG, Jensen OM (1998) Prognostic factors in soft tissue sarcomas: the Aarhus experience. Eur J Cancer 34(12):1876–1882
Zagars GK, Ballo MT, Pisters PW, Pollock RE, Patel SR, Benjamin RS, Evans HL (2003) Prognostic factors for patients with localized soft-tissue sarcoma treated with conservation surgery and radiation therapy: an analysis of 1225 patients. Cancer 97(10):2530–2543. doi:10.1002/cncr.11365
Anaya DA, Lahat G, Wang X, Xiao L, Tuvin D, Pisters PW, Lev DC, Pollock RE (2009) Establishing prognosis in retroperitoneal sarcoma: a new histology-based paradigm. Ann Surg Oncol 16(3):667–675. doi:10.1245/s10434-008-0250-2
Ferrario T, Karakousis CP (2003) Retroperitoneal sarcomas: grade and survival. Arch Surg 138(3):248–251
Lewis JJ, Leung D, Woodruff JM, Brennan MF (1998) Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg 228(3):355–365
Nishimura J, Morii E, Takahashi T, Souma Y, Nakajima K, Doki Y, Nishida T (2010) Abdominal soft tissue sarcoma: a multicenter retrospective study. Int J Clin Oncol 15(4):399–405. doi:10.1007/s10147-010-0075-4
Perez EA, Gutierrez JC, Moffat FL Jr, Franceschi D, Livingstone AS, Spector SA, Levi JU, Sleeman D, Koniaris LG (2007) Retroperitoneal and truncal sarcomas: prognosis depends upon type not location. Ann Surg Oncol 14(3):1114–1122. doi:10.1245/s10434-006-9255-x
Stoeckle E, Coindre JM, Bonvalot S, Kantor G, Terrier P, Bonichon F, Nguyen Bui B, French Federation of Cancer Centers Sarcoma G (2001) Prognostic factors in retroperitoneal sarcoma: a multivariate analysis of a series of 165 patients of the French Cancer Center Federation Sarcoma Group. Cancer 92(2):359–368
Toulmonde M, Bonvalot S, Ray-Coquard I, Stoeckle E, Riou O, Isambert N, Bompas E, Penel N, Delcambre-Lair C, Saada E, Lecesne A, Le Pechoux C, Blay JY, Piperno-Neumann S, Chevreau C, Bay JO, Brouste V, Terrier P, Ranchere-Vince D, Neuville A, Italiano A, French Sarcoma G (2014) Retroperitoneal sarcomas: patterns of care in advanced stages, prognostic factors and focus on main histological subtypes: a multicenter analysis of the French Sarcoma Group. Ann Oncol 25(3):730–734. doi:10.1093/annonc/mdt576
Tseng W, Martinez SR, Tamurian RM, Borys D, Canter RJ (2012) Histologic type predicts survival in patients with retroperitoneal soft tissue sarcoma. J Surg Res 172(1):123–130. doi:10.1016/j.jss.2010.07.056
Youssef E, Fontanesi J, Mott M, Kraut M, Lucas D, Mekhael H, Ben-Josef E (2002) Long-term outcome of combined modality therapy in retroperitoneal and deep-trunk soft-tissue sarcoma: analysis of prognostic factors. Int J Radiat Oncol Biol Phys 54(2):514–519
Weitz J, Antonescu CR, Brennan MF (2003) Localized extremity soft tissue sarcoma: improved knowledge with unchanged survival over time. J Clin Oncol 21(14):2719–2725. doi:10.1200/JCO.2003.02.026
McKee MD, Liu DF, Brooks JJ, Gibbs JF, Driscoll DL, Kraybill WG (2004) The prognostic significance of margin width for extremity and trunk sarcoma. J Surg Oncol 85(2):68–76. doi:10.1002/jso.20009
Stojadinovic A, Leung DH, Hoos A, Jaques DP, Lewis JJ, Brennan MF (2002) Analysis of the prognostic significance of microscopic margins in 2,084 localized primary adult soft tissue sarcomas. Ann Surg 235(3):424–434
Zagars GK, Ballo MT, Pisters PW, Pollock RE, Patel SR, Benjamin RS (2003) Surgical margins and reresection in the management of patients with soft tissue sarcoma using conservative surgery and radiation therapy. Cancer 97(10):2544–2553. doi:10.1002/cncr.11367
Bernthal NM, Federman N, Eilber FR, Nelson SD, Eckardt JJ, Eilber FC, Tap WD (2012) Long-term results (>25 years) of a randomized, prospective clinical trial evaluating chemotherapy in patients with high-grade, operable osteosarcoma. Cancer 118(23):5888–5893. doi:10.1002/cncr.27651
Chou AJ, Geller DS, Gorlick R (2008) Therapy for osteosarcoma: where do we go from here? Paediatr Drugs 10(5):315–327
Guillou L, Coindre JM, Bonichon F, Nguyen BB, Terrier P, Collin F, Vilain MO, Mandard AM, Le Doussal V, Leroux A, Jacquemier J, Duplay H, Sastre-Garau X, Costa J (1997) Comparative study of the National Cancer Institute and French Federation of Cancer Centers Sarcoma Group grading systems in a population of 410 adult patients with soft tissue sarcoma. J Clin Oncol 15(1):350–362
Edge SB, Compton CC (2010) The American Joint Committee on Cancer: the 7th Edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 17(6):1471–1474. doi:10.1245/s10434-010-0985-4
Kattan MW, Leung DH, Brennan MF (2002) Postoperative nomogram for 12-year sarcoma-specific death. J Clin Oncol Off J Am Soc Clin Oncol 20(3):791–796
Mariani L, Miceli R, Kattan MW, Brennan MF, Colecchia M, Fiore M, Casali PG, Gronchi A (2005) Validation and adaptation of a nomogram for predicting the survival of patients with extremity soft tissue sarcoma using a three-grade system. Cancer 103(2):402–408. doi:10.1002/cncr.20778
Eilber FC, Brennan MF, Eilber FR, Dry SM, Singer S, Kattan MW (2004) Validation of the postoperative nomogram for 12-year sarcoma-specific mortality. Cancer 101(10):2270–2275. doi:10.1002/cncr.20570
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247. doi:10.1016/j.ejca.2008.10.026
Meric F, Hess KR, Varma DG, Hunt KK, Pisters PW, Milas KM, Patel SR, Benjamin RS, Plager C, Papadopoulos NE, Burgess MA, Pollock RE, Feig BW (2002) Radiographic response to neoadjuvant chemotherapy is a predictor of local control and survival in soft tissue sarcomas. Cancer 95(5):1120–1126. doi:10.1002/cncr.10794
Chen Y, Yang Y, Wang C, Shi Y (2013) Radiographic response to neoadjuvant therapy and its impact on scope of surgery and prognosis in stage IIB/III soft tissue sarcomas. BMC Cancer 13:591. doi:10.1186/1471-2407-13-591
Delisca GO, Alamanda VK, Archer KR, Song Y, Schwartz HS, Holt GE (2013) Tumor size increase following preoperative radiation of soft tissue sarcomas does not affect prognosis. J Surg Oncol 107(7):723–727. doi:10.1002/jso.23322
Wardelmann E, Haas RL, Bovee JV, Terrier P, Lazar A, Messiou C, LePechoux C, Hartmann W, Collin F, Fisher C, Mechtersheimer G, DeiTos AP, Stacchiotti S, Jones RL, Gronchi A, Bonvalot S (2016) Evaluation of response after neoadjuvant treatment in soft tissue sarcomas; the European Organization for Research and Treatment of Cancer-Soft Tissue and Bone Sarcoma Group (EORTC-STBSG) recommendations for pathological examination and reporting. Eur J Cancer 53:84–95. doi:10.1016/j.ejca.2015.09.021
Wahl RL, Jacene H, Kasamon Y, Lodge MA (2009) From RECIST to PERCIST: evolving Considerations for PET response criteria in solid tumors. J Nucl Med 50(Suppl 1):122S–150S. doi:10.2967/jnumed.108.057307
Choi H, Charnsangavej C, Faria SC, Macapinlac HA, Burgess MA, Patel SR, Chen LL, Podoloff DA, Benjamin RS (2007) Correlation of computed tomography and positron emission tomography in patients with metastatic gastrointestinal stromal tumor treated at a single institution with imatinib mesylate: proposal of new computed tomography response criteria. J Clin Oncol 25(13):1753–1759. doi:10.1200/JCO.2006.07.3049
Choi H (2008) Response evaluation of gastrointestinal stromal tumors. Oncologist 13(Suppl 2):4–7. doi:10.1634/theoncologist.13-S2-4
Stacchiotti S, Collini P, Messina A, Morosi C, Barisella M, Bertulli R, Piovesan C, Dileo P, Torri V, Gronchi A, Casali PG (2009) High-grade soft-tissue sarcomas: tumor response assessment—pilot study to assess the correlation between radiologic and pathologic response by using RECIST and Choi criteria. Radiology 251(2):447–456. doi:10.1148/radiol.2512081403
Stacchiotti S, Verderio P, Messina A, Morosi C, Collini P, Llombart-Bosch A, Martin J, Comandone A, Cruz J, Ferraro A, Grignani G, Pizzamiglio S, Quagliuolo V, Picci P, Frustaci S, Dei Tos AP, Casali PG, Gronchi A (2012) Tumor response assessment by modified Choi criteria in localized high-risk soft tissue sarcoma treated with chemotherapy. Cancer 118(23):5857–5866. doi:10.1002/cncr.27624
Taieb S, Saada-Bouzid E, Tresch E, Ryckewaert T, Bompas E, Italiano A, Guillemet C, Peugniez C, Piperno-Neumann S, Thyss A, Maynou C, Clisant S, Penel N, French Sarcoma G (2015) Comparison of response evaluation criteria in solid tumours and Choi criteria for response evaluation in patients with advanced soft tissue sarcoma treated with trabectedin: a retrospective analysis. Eur J Cancer 51(2):202–209. doi:10.1016/j.ejca.2014.11.008
Herrmann K, Benz MR, Czernin J, Allen-Auerbach MS, Tap WD, Dry SM, Schuster T, Eckardt JJ, Phelps ME, Weber WA, Eilber FC (2012) 18F-FDG-PET/CT Imaging as an early survival predictor in patients with primary high-grade soft tissue sarcomas undergoing neoadjuvant therapy. Clin Cancer Res 18(7):2024–2031. doi:10.1158/1078-0432.CCR-11-2139
Tateishi U, Kawai A, Chuman H, Nakatani F, Beppu Y, Seki K, Miyake M, Terauchi T, Moriyama N, Kim EE (2011) PET/CT allows stratification of responders to neoadjuvant chemotherapy for high-grade sarcoma: a prospective study. Clin Nucl Med 36(7):526–532. doi:10.1097/RLU.0b013e3182175856
Benz MR, Czernin J, Allen-Auerbach MS, Tap WD, Dry SM, Elashoff D, Chow K, Evilevitch V, Eckardt JJ, Phelps ME, Weber WA, Eilber FC (2009) FDG-PET/CT imaging predicts histopathologic treatment responses after the initial cycle of neoadjuvant chemotherapy in high-grade soft-tissue sarcomas. Clin Cancer Res 15(8):2856–2863. doi:10.1158/1078-0432.CCR-08-2537
Schuetze SM, Rubin BP, Vernon C, Hawkins DS, Bruckner JD, Conrad EU 3rd, Eary JF (2005) Use of positron emission tomography in localized extremity soft tissue sarcoma treated with neoadjuvant chemotherapy. Cancer 103(2):339–348. doi:10.1002/cncr.20769
Orlacchio A, Ciarrapico AM, Schillaci O, Chegai F, Tosti D, D’Alba F, Guazzaroni M, Simonetti G (2014) PET-CT in oncological patients: analysis of informal care costs in cost-benefit assessment. Radiol Med (Torino) 119(4):283–289. doi:10.1007/s11547-013-0340-5
Canter RJ, Martinez SR, Tamurian RM, Wilton M, Li CS, Ryu J, Mak W, Monsky WL, Borys D (2010) Radiographic and histologic response to neoadjuvant radiotherapy in patients with soft tissue sarcoma. Ann Surg Oncol 17(10):2578–2584. doi:10.1245/s10434-010-1156-3
Roberge D, Skamene T, Nahal A, Turcotte RE, Powell T, Freeman C (2010) Radiological and pathological response following pre-operative radiotherapy for soft-tissue sarcoma. Radiother Oncol 97(3):404–407. doi:10.1016/j.radonc.2010.10.007
Stahl R, Wang T, Lindner LH, Abdel-Rahman S, Santl M, Reiser MF, Issels RD (2009) Comparison of radiological and pathohistological response to neoadjuvant chemotherapy combined with regional hyperthermia (RHT) and study of response dependence on the applied thermal parameters in patients with soft tissue sarcomas (STS). Int J Hyperth 25(4):289–298. doi:10.1080/02656730902873616
Donahue TR, Kattan MW, Nelson SD, Tap WD, Eilber FR, Eilber FC (2010) Evaluation of neoadjuvant therapy and histopathologic response in primary, high-grade retroperitoneal sarcomas using the sarcoma nomogram. Cancer 116(16):3883–3891. doi:10.1002/cncr.25271
Eilber FC, Rosen G, Eckardt J, Forscher C, Nelson SD, Selch M, Dorey F, Eilber FR (2001) Treatment-induced pathologic necrosis: a predictor of local recurrence and survival in patients receiving neoadjuvant therapy for high-grade extremity soft tissue sarcomas. J Clin Oncol 19(13):3203–3209
Henshaw RM, Priebat DA, Perry DJ, Shmookler BM, Malawer MM (2001) Survival after induction chemotherapy and surgical resection for high-grade soft tissue sarcoma. Is radiation necessary? Ann Surg Oncol 8(6):484–495
MacDermed DM, Miller LL, Peabody TD, Simon MA, Luu HH, Haydon RC, Montag AG, Undevia SD, Connell PP (2010) Primary tumor necrosis predicts distant control in locally advanced soft-tissue sarcomas after preoperative concurrent chemoradiotherapy. Int J Radiat Oncol Biol Phys 76(4):1147–1153. doi:10.1016/j.ijrobp.2009.03.015
Matsubara T, Eimoto T, Okabe M, Miyabe S, Fujiyoshi Y, Matsushita Y, Mizutani J, Yamada S, Otsuka T (2008) Proliferation and apoptosis of tumour cells before and after neoadjuvant therapy for high-grade extremity sarcomas: divergent associations with tumour response and prognosis. Histopathology 52(6):706–716. doi:10.1111/j.1365-2559.2008.03015.x
Shah D, Borys D, Martinez SR, Li CS, Tamurian RM, Bold RJ, Monjazeb A, Canter RJ (2012) Complete pathologic response to neoadjuvant radiotherapy is predictive of oncological outcome in patients with soft tissue sarcoma. Anticancer Res 32(9):3911–3915
Lucas DR, Kshirsagar MP, Biermann JS, Hamre MR, Thomas DG, Schuetze SM, Baker LH (2008) Histologic alterations from neoadjuvant chemotherapy in high-grade extremity soft tissue sarcoma: clinicopathological correlation. Oncologist 13(4):451–458. doi:10.1634/theoncologist.2007-0220
Menendez LR, Ahlmann ER, Savage K, Cluck M, Fedenko AN (2007) Tumor necrosis has no prognostic value in neoadjuvant chemotherapy for soft tissue sarcoma. Clin Orthop Relat Res 455:219–224. doi:10.1097/01.blo.0000238864.69486.59
Meric F, Milas M, Hunt KK, Hess KR, Pisters PW, Hildebrandt G, Patel SR, Benjamin RS, Plager C, Papadopolous NE, Burgess MA, Pollock RE, Feig BW (2000) Impact of neoadjuvant chemotherapy on postoperative morbidity in soft tissue sarcomas. J Clin Oncol 18(19):3378–3383
Benjamin RS, Wiernik PH, Bachur NR (1975) Adriamycin: a new effective agent in the therapy of disseminated sarcomas. Med Pediatr Oncol 1(1):63–76
Casper ES, Gaynor JJ, Hajdu SI, Magill GB, Tan C, Friedrich C, Brennan MF (1991) A prospective randomized trial of adjuvant chemotherapy with bolus versus continuous infusion of doxorubicin in patients with high-grade extremity soft tissue sarcoma and an analysis of prognostic factors. Cancer 68(6):1221–1229
Zalupski M, Metch B, Balcerzak S, Fletcher WS, Chapman R, Bonnet JD, Weiss GR, Ryan J, Benjamin RS, Baker LH (1991) Phase III comparison of doxorubicin and dacarbazine given by bolus versus infusion in patients with soft-tissue sarcomas: a Southwest Oncology Group study. J Natl Cancer Inst 83(13):926–932
Gronchi A, Bui BN, Bonvalot S, Pilotti S, Ferrari S, Hohenberger P, Hohl RJ, Demetri GD, Le Cesne A, Lardelli P, Perez I, Nieto A, Tercero JC, Alfaro V, Tamborini E, Blay JY (2012) Phase II clinical trial of neoadjuvant trabectedin in patients with advanced localized myxoid liposarcoma. Ann Oncol 23(3):771–776. doi:10.1093/annonc/mdr265
Hensley ML, Ishill N, Soslow R, Larkin J, Abu-Rustum N, Sabbatini P, Konner J, Tew W, Spriggs D, Aghajanian CA (2009) Adjuvant gemcitabine plus docetaxel for completely resected stages I–IV high grade uterine leiomyosarcoma: results of a prospective study. Gynecol Oncol 112(3):563–567. doi:10.1016/j.ygyno.2008.11.027
Hensley ML, Wathen JK, Maki RG, Araujo DM, Sutton G, Priebat DA, George S, Soslow RA, Baker LH (2013) Adjuvant therapy for high-grade, uterus-limited leiomyosarcoma: results of a phase 2 trial (SARC 005). Cancer 119(8):1555–1561. doi:10.1002/cncr.27942
Schoffski P, Chawla S, Maki RG, Italiano A, Gelderblom H, Choy E, Grignani G, Camargo V, Bauer S, Rha SY, Blay JY, Hohenberger P, D’Adamo D, Guo M, Chmielowski B, Le Cesne A, Demetri GD, Patel SR (2016) Eribulin versus dacarbazine in previously treated patients with advanced liposarcoma or leiomyosarcoma: a randomised, open-label, multicentre, phase 3 trial. Lancet. doi:10.1016/S0140-6736(15)01283-0
Munhoz RR, D’Angelo SP, Gounder MM, Keohan ML, Chi P, Carvajal RD, Singer S, Crago AM, Landa J, Healey JH, Qin LX, Hameed M, Ezeoke MO, Singh AS, Agulnik M, Chmielowski B, Luke JJ, Van Tine BA, Schwartz GK, Tap WD, Dickson MA (2015) A phase Ib/II study of gemcitabine and docetaxel in combination with pazopanib for the neoadjuvant treatment of soft tissue sarcomas. Oncologist 20(11):1245–1246. doi:10.1634/theoncologist.2015-0245
Pisters PW, Ballo MT, Fenstermacher MJ, Feig BW, Hunt KK, Raymond KA, Burgess MA, Zagars GK, Pollock RE, Benjamin RS, Patel SR (2003) Phase I trial of preoperative concurrent doxorubicin and radiation therapy, surgical resection, and intraoperative electron-beam radiation therapy for patients with localized retroperitoneal sarcoma. J Clin Oncol 21(16):3092–3097. doi:10.1200/JCO.2003.01.143
Pisters PW, Patel SR, Prieto VG, Thall PF, Lewis VO, Feig BW, Hunt KK, Yasko AW, Lin PP, Jacobson MG, Burgess MA, Pollock RE, Zagars GK, Benjamin RS, Ballo MT (2004) Phase I trial of preoperative doxorubicin-based concurrent chemoradiation and surgical resection for localized extremity and body wall soft tissue sarcomas. J Clin Oncol 22(16):3375–3380. doi:10.1200/JCO.2004.01.040
Toma S, Canavese G, Grimaldi A, Ravera G, Ugolini D, Percivale P, Badellino F (2003) Concomitant chemo-radiotherapy in the treatment of locally advanced and/or metastatic soft tissue sarcomas: experience of the National Cancer Institute of Genoa. Oncol Rep 10(3):641–647
Mack LA, Crowe PJ, Yang JL, Schachar NS, Morris DG, Kurien EC, Temple CL, Lindsay RL, Magi E, DeHaas WG, Temple WJ (2005) Preoperative chemoradiotherapy (modified Eilber protocol) provides maximum local control and minimal morbidity in patients with soft tissue sarcoma. Ann Surg Oncol 12(8):646–653. doi:10.1245/ASO.2005.03.064
Aguiar Junior S, Ferreira Fde O, Rossi BM, Santos EM, Salvajoli JV, Lopes A (2009) Neoadjuvant chemoradiation therapy for soft tissue sarcomas of the extremities. Clinics 64(11):1059–1064. doi:10.1590/S1807-59322009001100005
Cormier JN, Patel SR, Herzog CE, Ballo MT, Burgess MA, Feig BW, Hunt KK, Raney RB, Zagars GK, Benjamin RS, Pisters PW (2001) Concurrent ifosfamide-based chemotherapy and irradiation. Analysis of treatment-related toxicity in 43 patients with sarcoma. Cancer 92(6):1550–1555
Gronchi A, De Paoli A, Dani C, Merlo DF, Quagliuolo V, Grignani G, Bertola G, Navarria P, Sangalli C, Buonadonna A, De Sanctis R, Sanfilippo R, Dei Tos AP, Stacchiotti S, Giorello L, Fiore M, Bruzzi P, Casali PG (2014) Preoperative chemo-radiation therapy for localised retroperitoneal sarcoma: a phase I-II study from the Italian Sarcoma Group. Eur J Cancer 50(4):784–792. doi:10.1016/j.ejca.2013.11.021
Sauer R, Schuchardt U, Hohenberger W, Wittekind C, Papadopoulos T, Grabenbauer GG, Fietkau R (1999) Neoadjuvant radiochemotherapy in soft tissue sarcomas. Optimization of local functional tumor control. Strahlentherapie und Onkologie: Organ der Deutschen Röntgengesellschaft 175(6):259–266
Rhomberg W, Hassenstein EO, Gefeller D (1996) Radiotherapy vs. radiotherapy and razoxane in the treatment of soft tissue sarcomas: final results of a randomized study. Int J Radiat Oncol Biol Phys 36(5):1077–1084
Sondak VK, Robertson JM, Sussman JJ, Saran PA, Chang AE, Lawrence TS (1998) Preoperative idoxuridine and radiation for large soft tissue sarcomas: clinical results with five-year follow-up. Ann Surg Oncol 5(2):106–112
Goffman T, Tochner Z, Glatstein E (1991) Primary treatment of large and massive adult sarcomas with iododeoxyuridine and aggressive hyperfractionated irradiation. Cancer 67(3):572–576
Jakob J, Wenz F, Dinter DJ, Strobel P, Hohenberger P (2009) Preoperative intensity-modulated radiotherapy combined with temozolomide for locally advanced soft-tissue sarcoma. Int J Radiat Oncol Biol Phys 75(3):810–816. doi:10.1016/j.ijrobp.2008.11.032
Yoon SS, Duda DG, Karl DL, Kim TM, Kambadakone AR, Chen YL, Rothrock C, Rosenberg AE, Nielsen GP, Kirsch DG, Choy E, Harmon DC, Hornicek FJ, Dreyfuss J, Ancukiewicz M, Sahani DV, Park PJ, Jain RK, Delaney TF (2011) Phase II study of neoadjuvant bevacizumab and radiotherapy for resectable soft tissue sarcomas. Int J Radiat Oncol Biol Phys 81(4):1081–1090. doi:10.1016/j.ijrobp.2010.07.024
Canter RJ, Borys D, Olusanya A, Li CS, Lee LY, Boutin RD, Christensen SD, Tamurian RM, Monjazeb AM (2014) Phase I trial of neoadjuvant conformal radiotherapy plus sorafenib for patients with locally advanced soft tissue sarcoma of the extremity. Ann Surg Oncol 21(5):1616–1623. doi:10.1245/s10434-014-3543-7
Haas RL, Gelderblom H, Sleijfer S, van Boven HH, Scholten A, Dewit L, Borst G, van der Hage J, Kerst JM, Nout RA, Hartgrink HH, de Pree I, Verhoef C, Steeghs N, van Coevorden F (2015) A phase I study on the combination of neoadjuvant radiotherapy plus pazopanib in patients with locally advanced soft tissue sarcoma of the extremities. Acta Oncol 54(8):1195–1201. doi:10.3109/0284186X.2015.1037404
Rahoty P, Konya A (1993) Results of preoperative neoadjuvant chemotherapy and surgery in the management of patients with soft tissue sarcoma. Eur J Surg Oncol 19(6):641–645
Rouesse JG, Friedman S, Sevin DM, le Chevalier T, Spielmann ML, Contesso G, Sarrazin DM, Genin JR (1987) Preoperative induction chemotherapy in the treatment of locally advanced soft tissue sarcomas. Cancer 60(3):296–300
Pezzi CM, Pollock RE, Evans HL, Lorigan JG, Pezzi TA, Benjamin RS, Romsdahl MM (1990) Preoperative chemotherapy for soft-tissue sarcomas of the extremities. Ann Surg 211(4):476–481
Wiklund T, Saeter G, Strander H, Alvegard T, Blomqvist C (1997) The outcome of advanced soft tissue sarcoma patients with complete tumour regression after either chemotherapy alone or chemotherapy plus surgery. The Scandinavian Sarcoma Group experience. Eur J Cancer 33(3):357–361
Merimsky O, Meller I, Issakov J, Kollender Y, Oron D, Flusser G, Gutman M, Lev-Chelouche D, Inbar M (1999) Adriamycin-ifosfamide induction chemotherapy for extremity soft tissue sarcoma: comparison of two non-randomized protocols. Oncol Rep 6(4):913–920
Pisters PW, Patel SR, Varma DG, Cheng SC, Chen NP, Nguyen HT, Feig BW, Pollack A, Pollock RE, Benjamin RS (1997) Preoperative chemotherapy for stage IIIB extremity soft tissue sarcoma: long-term results from a single institution. J Clin Oncol 15(12):3481–3487
Cormier JN, Huang X, Xing Y, Thall PF, Wang X, Benjamin RS, Pollock RE, Antonescu CR, Maki RG, Brennan MF, Pisters PW (2004) Cohort analysis of patients with localized, high-risk, extremity soft tissue sarcoma treated at two cancer centers: chemotherapy-associated outcomes. J Clin Oncol 22(22):4567–4574. doi:10.1200/JCO.2004.02.057
Azzarelli A, Quagliuolo V, Casali P, Fissi S, Montalto F, Santoro A (1993) Preoperative doxorubicin plus ifosfamide in primary soft-tissue sarcomas of the extremities. Cancer Chemother Pharmacol 31(Suppl 2):S210–S212
Grobmyer SR, Maki RG, Demetri GD, Mazumdar M, Riedel E, Brennan MF, Singer S (2004) Neo-adjuvant chemotherapy for primary high-grade extremity soft tissue sarcoma. Ann Oncol 15(11):1667–1672. doi:10.1093/annonc/mdh431
Italiano A, Penel N, Robin YM, Bui B, Le Cesne A, Piperno-Neumann S, Tubiana-Hulin M, Bompas E, Chevreau C, Isambert N, Leyvraz S, du Chatelard PP, Thyss A, Coindre JM, Blay JY (2009) Neo/adjuvant chemotherapy does not improve outcome in resected primary synovial sarcoma: a study of the French Sarcoma Group. Ann Oncol Off J Eur Soc Med Oncol 20(3):425–430. doi:10.1093/annonc/mdn678
Ogura K, Goto T, Imanishi J, Shinoda Y, Okuma T, Tsuda Y, Kobayashi H, Akiyama T, Hirata M, Yamamoto A, Kawano H (2013) Neoadjuvant and adjuvant chemotherapy with modified mesna, adriamycin, ifosfamide, and dacarbazine (MAID) regimen for adult high-grade non-small round cell soft tissue sarcomas. Int J Clin Oncol 18(1):170–176. doi:10.1007/s10147-011-0360-x
Gortzak E, Azzarelli A, Buesa J, Bramwell VH, van Coevorden F, van Geel AN, Ezzat A, Santoro A, Oosterhuis JW, van Glabbeke M, Kirkpatrick A, Verweij J, Group EORTCSTBS, the National Cancer Institute of Canada Clinical Trials Group/Canadian Sarcoma G (2001) A randomised phase II study on neo-adjuvant chemotherapy for ‘high-risk’ adult soft-tissue sarcoma. Eur J Cancer 37(9):1096–1103
Pappo AS, Devidas M, Jenkins J, Rao B, Marcus R, Thomas P, Gebhardt M, Pratt C, Grier HE (2005) Phase II trial of neoadjuvant vincristine, ifosfamide, and doxorubicin with granulocyte colony-stimulating factor support in children and adolescents with advanced-stage nonrhabdomyosarcomatous soft tissue sarcomas: a Pediatric Oncology Group Study. J Clin Oncol 23(18):4031–4038. doi:10.1200/JCO.2005.03.209
Tanaka K, Kawamoto H, Saito I, Yoshimura K, Fukuda H, Iwamoto Y (2009) Preoperative and postoperative chemotherapy with ifosfamide and adriamycin for adult high-grade soft-tissue sarcomas in the extremities: Japan Clinical Oncology Group Study JCOG0304. Jpn J Clin Oncol 39(4):271–273. doi:10.1093/jjco/hyn153
Tanaka K, Mizusawa J, Fukuda H, Araki N, Chuman H, Takahashi M, Ozaki T, Hiruma T, Tsuchiya H, Morioka H, Hatano H, Iwamoto Y (2015) Perioperative chemotherapy with ifosfamide and doxorubicin for high-grade soft tissue sarcomas in the extremities (JCOG0304). Jpn J Clin Oncol 45(6):555–561. doi:10.1093/jjco/hyv042
Antman KH, Ryan L, Elias A, Sherman D, Grier HE (1989) Response to ifosfamide and mesna: 124 previously treated patients with metastatic or unresectable sarcoma. J Clin Oncol 7(1):126–131
Buesa JM, Mouridsen HT, van Oosterom AT, Verweij J, Wagener T, Steward W, Poveda A, Vestlev PM, Thomas D, Sylvester R (1991) High-dose DTIC in advanced soft-tissue sarcomas in the adult. A phase II study of the E.O.R.T.C. Soft Tissue and Bone Sarcoma Group. Ann Oncol 2(4):307–309
Elias A, Ryan L, Sulkes A, Collins J, Aisner J, Antman KH (1989) Response to mesna, doxorubicin, ifosfamide, and dacarbazine in 108 patients with metastatic or unresectable sarcoma and no prior chemotherapy. J Clin Oncol 7(9):1208–1216
Antman K, Crowley J, Balcerzak SP, Kempf RA, Weiss RB, Clamon GH, Baker LH (1998) A Southwest Oncology Group and Cancer and Leukemia Group B phase II study of doxorubicin, dacarbazine, ifosfamide, and mesna in adults with advanced osteosarcoma, Ewing’s sarcoma, and rhabdomyosarcoma. Cancer 82(7):1288–1295
Antman K, Crowley J, Balcerzak SP, Rivkin SE, Weiss GR, Elias A, Natale RB, Cooper RM, Barlogie B, Trump DL et al (1993) An intergroup phase III randomized study of doxorubicin and dacarbazine with or without ifosfamide and mesna in advanced soft tissue and bone sarcomas. J Clin Oncol 11(7):1276–1285
DeLaney TF, Spiro IJ, Suit HD, Gebhardt MC, Hornicek FJ, Mankin HJ, Rosenberg AL, Rosenthal DI, Miryousefi F, Ancukiewicz M, Harmon DC (2003) Neoadjuvant chemotherapy and radiotherapy for large extremity soft-tissue sarcomas. Int J Radiat Oncol Biol Phys 56(4):1117–1127. doi:10.1016/s0360-3016(03)00186-x
Mullen JT, Kobayashi W, Wang JJ, Harmon DC, Choy E, Hornicek FJ, Rosenberg AE, Chen YL, Spiro IJ, DeLaney TF (2012) Long-term follow-up of patients treated with neoadjuvant chemotherapy and radiotherapy for large, extremity soft tissue sarcomas. Cancer 118(15):3758–3765. doi:10.1002/cncr.26696
Look Hong NJ, Hornicek FJ, Harmon DC, Choy E, Chen YL, Yoon SS, Nielsen GP, Szymonifka J, Yeap BY, DeLaney TF, Mullen JT (2013) Neoadjuvant chemoradiotherapy for patients with high-risk extremity and truncal sarcomas: a 10-year single institution retrospective study. Eur J Cancer 49(4):875–883. doi:10.1016/j.ejca.2012.10.002
Kraybill WG, Harris J, Spiro IJ, Ettinger DS, DeLaney TF, Blum RH, Lucas DR, Harmon DC, Letson GD, Eisenberg B, Radiation Therapy Oncology Group T (2006) Phase II study of neoadjuvant chemotherapy and radiation therapy in the management of high-risk, high-grade, soft tissue sarcomas of the extremities and body wall: radiation Therapy Oncology Group Trial 9514. J Clin Oncol 24(4):619–625. doi:10.1200/JCO.2005.02.5577
Kraybill WG, Harris J, Spiro IJ, Ettinger DS, DeLaney TF, Blum RH, Lucas DR, Harmon DC, Letson GD, Eisenberg B (2010) Long-term results of a phase 2 study of neoadjuvant chemotherapy and radiotherapy in the management of high-risk, high-grade, soft tissue sarcomas of the extremities and body wall: Radiation Therapy Oncology Group Trial 9514. Cancer 116(19):4613–4621. doi:10.1002/cncr.25350
O’Sullivan B, Bell RS (2003) Has “MAID” made it in the management of high-risk soft-tissue sarcoma? Int J Radiat Oncol Biol Phys 56(4):915–916. doi:10.1016/s0360-3016(03)00185-8
Edmonson JH, Petersen IA, Shives TC, Mahoney MR, Rock MG, Haddock MG, Sim FH, Maples WJ, O’Connor MI, Gunderson LL, Foo ML, Pritchard DJ, Buckner JC, Stafford SL (2002) Chemotherapy, irradiation, and surgery for function-preserving therapy of primary extremity soft tissue sarcomas: initial treatment with ifosfamide, mitomycin, doxorubicin, and cisplatin plus granulocyte macrophage-colony-stimulating factor. Cancer 94(3):786–792
Ryan CW, Montag AG, Hosenpud JR, Samuels B, Hayden JB, Hung AY, Mansoor A, Peabody TD, Mundt AJ, Undevia S (2008) Histologic response of dose-intense chemotherapy with preoperative hypofractionated radiotherapy for patients with high-risk soft tissue sarcomas. Cancer 112(11):2432–2439. doi:10.1002/cncr.23478
Gronchi A, Frustaci S, Mercuri M, Martin J, Lopez-Pousa A, Verderio P, Mariani L, Valagussa P, Miceli R, Stacchiotti S, Dei Tos AP, De Paoli A, Longhi A, Poveda A, Quagliuolo V, Comandone A, Casali PG, Picci P (2012) Short, full-dose adjuvant chemotherapy in high-risk adult soft tissue sarcomas: a randomized clinical trial from the Italian Sarcoma Group and the Spanish Sarcoma Group. J Clin Oncol 30(8):850–856. doi:10.1200/JCO.2011.37.7218
Gronchi A, Verderio P, De Paoli A, Ferraro A, Tendero O, Majo J, Martin J, Comandone A, Grignani G, Pizzamiglio S, Quagliuolo V, Picci P, Frustaci S, Dei Tos AP, Palassini E, Stacchiotti S, Ferrari S, Fiore M, Casali PG (2013) Quality of surgery and neoadjuvant combined therapy in the ISG-GEIS trial on soft tissue sarcomas of limbs and trunk wall. Ann Oncol 24(3):817–823. doi:10.1093/annonc/mds501
Finkelstein SE, Iclozan C, Bui MM, Cotter MJ, Ramakrishnan R, Ahmed J, Noyes DR, Cheong D, Gonzalez RJ, Heysek RV, Berman C, Lenox BC, Janssen W, Zager JS, Sondak VK, Letson GD, Antonia SJ, Gabrilovich DI (2012) Combination of external beam radiotherapy (EBRT) with intratumoral injection of dendritic cells as neo-adjuvant treatment of high-risk soft tissue sarcoma patients. Int J Radiat Oncol Biol Phys 82(2):924–932. doi:10.1016/j.ijrobp.2010.12.068
Issels RD, Abdel-Rahman S, Wendtner C, Falk MH, Kurze V, Sauer H, Aydemir U, Hiddemann W (2001) Neoadjuvant chemotherapy combined with regional hyperthermia (RHT) for locally advanced primary or recurrent high-risk adult soft-tissue sarcomas (STS) of adults: long-term results of a phase II study. Eur J Cancer 37(13):1599–1608
Wendtner CM (2002) Response to neoadjuvant chemotherapy combined with regional hyperthermia predicts long-term survival for adult patients with retroperitoneal and visceral high-risk soft tissue sarcomas. J Clin Oncol 20(14):3156–3164. doi:10.1200/jco.2002.07.146
Eckert F, Gani C, Kluba T, Mayer F, Kopp HG, Zips D, Bamberg M, Muller AC (2013) Effect of concurrent chemotherapy and hyperthermia on outcome of preoperative radiotherapy of high-risk soft tissue sarcomas. Strahlentherapie und Onkologie: Organ der Deutschen Röntgengesellschaft 189(6):482–485. doi:10.1007/s00066-013-0312-7
Klaase JM, Kroon BB, Benckhuijsen C, van Geel AN, Albus-Lutter CE, Wieberdink J (1989) Results of regional isolation perfusion with cytostatics in patients with soft tissue tumors of the extremities. Cancer 64(3):616–621
Wanebo HJ, Temple WJ, Popp MB, Douvill CE, Yablonski M (1990) Combination regional therapy for extremity sarcoma. A tricenter study. Arch Surg 125(3):355–359
Wanebo HJ, Temple WJ, Popp MB, Constable W, Aron B, Cunningham SL (1995) Preoperative regional therapy for extremity sarcoma. A tricenter update. Cancer 75(9):2299–2306
Temple WJ, Temple CL, Arthur K, Schachar NS, Paterson AH, Crabtree TS (1997) Prospective cohort study of neoadjuvant treatment in conservative surgery of soft tissue sarcomas. Ann Surg Oncol 4(7):586–590
Otsuka T, Yonezawa M, Kamiyama F, Matsushita Y, Matsui N (2001) Results of surgery and radio-hyperthermo-chemotherapy for patients with soft-tissue sarcoma. Int J Clin Oncol 6(5):253–258
Rossi CR, Vecchiato A, Foletto M, Nitti D, Ninfo V, Fornasiero A, Sotti G, Tregnaghi A, Melanotte P, Lise M (1994) Phase II study on neoadjuvant hyperthermic-antiblastic perfusion with doxorubicin in patients with intermediate or high grade limb sarcomas. Cancer 73(8):2140–2146
Di Filippo F, Giannarelli D, Botti C, Carlini S, Cavaliere F, Garinei R, Schiratti M, Casaldi V, Tedesco M, Cavaliere R (1992) Hyperthermic antiblastic perfusion for the treatment of soft tissue limb sarcoma. Ann Oncol 3(Suppl 2):S71–S74
Krementz ET, Carter RD, Sutherland CM, Hutton I (1977) Chemotherapy of sarcomas of the limbs by regional perfusion. Ann Surg 185(5):555–564
Lienard D, Ewalenko P, Delmotte JJ, Renard N, Lejeune FJ (1992) High-dose recombinant tumor necrosis factor alpha in combination with interferon gamma and melphalan in isolation perfusion of the limbs for melanoma and sarcoma. J Clin Oncol Off 10(1):52–60
Lejeune FJ, Pujol N, Lienard D, Mosimann F, Raffoul W, Genton A, Guillou L, Landry M, Chassot PG, Chiolero R, Bischof-Delaloye A, Leyvraz S, Mirimanoff RO, Bejkos D, Leyvraz PF (2000) Limb salvage by neoadjuvant isolated perfusion with TNFalpha and melphalan for non-resectable soft tissue sarcoma of the extremities. Eur J Surg Oncol 26(7):669–678. doi:10.1053/ejso.2000.0979
Rossi CR, Foletto M, Di Filippo F, Vaglini M, Anza M, Azzarelli A, Pilati P, Mocellin S, Lise M (1999) Soft tissue limb sarcomas: italian clinical trials with hyperthermic antiblastic perfusion. Cancer 86(9):1742–1749
Rossi CR, Mocellin S, Pilati P, Foletto M, Campana L, Quintieri L, De Salvo GL, Lise M (2005) Hyperthermic isolated perfusion with low-dose tumor necrosis factor alpha and doxorubicin for the treatment of limb-threatening soft tissue sarcomas. Ann Surg Oncol 12(5):398–405. doi:10.1245/ASO.2005.12.038
Rossi CR, Foletto M, Mocellin S, Pilati P, Quintieri L, De Salvo GL, Nitti D, Lise M (2004) Hyperthermic isolated perfusion with low-dose TNFalpha and doxorubicin in patients with locally advanced soft tissue limb sarcomas. J Chemother 16(Suppl 5):58–61
Vrouenraets BC, Keus RB, Nieweg OE, Kroon BB (1997) Complications of combined radiotherapy and isolated limb perfusion with tumor necrosis factor alpha ± interferon gamma and melphalan in patients with irresectable soft tissue tumors. J Surg Oncol 65(2):88–94
Noorda EM, Vrouenraets BC, Nieweg OE, van Coevorden F, van Slooten GW, Kroon BB (2003) Isolated limb perfusion with tumor necrosis factor-alpha and melphalan for patients with unresectable soft tissue sarcoma of the extremities. Cancer 98(7):1483–1490. doi:10.1002/cncr.11648
Taeger G, Grabellus F, Podleska LE, Muller S, Ruchholtz S (2008) Effectiveness of regional chemotherapy with TNF-alpha/melphalan in advanced soft tissue sarcoma of the extremities. Int J Hyperth 24(3):193–203. doi:10.1080/02656730701868387
Eggermont AM, Koops HS, Klausner JM, Kroon BB, Schlag PM, Lienard D, van Geel AN, Hoekstra HJ, Meller I, Nieweg OE, Kettelhack C, Ben-Ari G, Pector JC, Lejeune FJ (1996) Isolated limb perfusion with tumor necrosis factor and melphalan for limb salvage in 186 patients with locally advanced soft tissue extremity sarcomas. The cumulative multicenter European experience. Ann Surg 224(6):756–764 (discussion 764-755)
Eggermont AM, Schraffordt Koops H, Lienard D, Kroon BB, van Geel AN, Hoekstra HJ, Lejeune FJ (1996) Isolated limb perfusion with high-dose tumor necrosis factor-alpha in combination with interferon-gamma and melphalan for nonresectable extremity soft tissue sarcomas: a multicenter trial. J Clin Oncol 14(10):2653–2665
Di Filippo F, Garinei R, Anza M, Cavaliere F, Giannarelli D, Cagol PP, Rossi CR, Santinami M, Deraco M, Botti C, Perri P, Di Filippo S, Piarulli L, Bruno P (2003) Doxorubicin in isolation limb perfusion in the treatment of advanced limb soft tissue sarcoma. J Exp Clin Cancer Res CR 22(4 Suppl):81–87
Bonvalot S, Laplanche A, Lejeune F, Stoeckle E, Le Pechoux C, Vanel D, Terrier P, Lumbroso J, Ricard M, Antoni G, Cavalcanti A, Robert C, Lassau N, Blay JY, Le Cesne A (2005) Limb salvage with isolated perfusion for soft tissue sarcoma: could less TNF-alpha be better? Ann Oncol 16(7):1061–1068. doi:10.1093/annonc/mdi229
Thijssens KM, van Ginkel RJ, Pras E, Suurmeijer AJ, Hoekstra HJ (2006) Isolated limb perfusion with tumor necrosis factor alpha and melphalan for locally advanced soft tissue sarcoma: the value of adjuvant radiotherapy. Ann Surg Oncol 13(4):518–524. doi:10.1245/ASO.2006.02.005
Grunhagen DJ, de Wilt JH, ten Hagen TL, Eggermont AM (2006) Technology insight: utility of TNF-alpha-based isolated limb perfusion to avoid amputation of irresectable tumors of the extremities. Nat Clin Pract Oncol 3(2):94–103. doi:10.1038/ncponc0426
Grunhagen DJ, de Wilt JH, Graveland WJ, van Geel AN, Eggermont AM (2006) The palliative value of tumor necrosis factor alpha-based isolated limb perfusion in patients with metastatic sarcoma and melanoma. Cancer 106(1):156–162. doi:10.1002/cncr.21547
Phan A, Patel S (2003) Advances in neoadjuvant chemotherapy in soft tissue sarcomas. Curr Treat Options Oncol 4(6):433–439
Reynoso D, Subbiah V, Trent JC, Guadagnolo BA, Lazar AJ, Benjamin R, Pollock RE, Ludwig JA (2010) Neoadjuvant treatment of soft-tissue sarcoma: a multimodality approach. J Surg Oncol 101(4):327–333. doi:10.1002/jso.21481
Hohenberger P, Wysocki WM (2008) Neoadjuvant treatment of locally advanced soft tissue sarcoma of the limbs: which treatment to choose? Oncologist 13(2):175–186. doi:10.1634/theoncologist.2007-0165
Acknowledgments
The authors thank Gabriela Steier for her support in the editing of this review.
Funding
NCI/NIH P30 CA134274.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interests to report, and no disclaimers.
Rights and permissions
About this article
Cite this article
Nathenson, M.J., Sausville, E. Looking for answers: the current status of neoadjuvant treatment in localized soft tissue sarcomas. Cancer Chemother Pharmacol 78, 895–919 (2016). https://doi.org/10.1007/s00280-016-3055-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-016-3055-1