Abstract
Background
Soft tissue sarcomas (STS) are rare mesenchymal neoplasms with a variety of histological subtypes. However, in Japan, data on the clinical characteristics and prognostic profiles of these tumors are lacking. The purpose of the present study was to clarify the clinical features and outcomes of Japanese patients with retroperitoneal and abdominal STS.
Methods
We reviewed and analyzed retrospectively the data for 82 patients who underwent surgery for retroperitoneal and abdominal STS at Osaka University and affiliated hospitals from 2000 to 2007. The factors analyzed included patient demographics and clinical features.
Results
The histological subtypes included leiomyosarcoma in 32 patients (39.0%), liposarcoma in 30 (36.6%), malignant fibrous histiocytoma in 10 (12.2%), and other miscellaneous subtypes in 10 (12.2%). The overall survivals were 92, 69, and 62%, respectively, at 1, 3, and 5 years after primary surgery. The overall survival of patients with low-grade sarcoma was significantly better than that of patients with high-grade sarcoma. Complete resection was done in 63 patients (77%) and their recurrence-free survivals were 73, 34, and 23%, respectively, at 1, 3, and 5 years after the surgery. Subgroup analysis of differences between leiomyosarcoma and liposarcoma revealed that liposarcomas were mainly located in the retroperitoneum and leiomyosarcomas were located equally in the retroperitoneum and abdominal cavity. The tumor size of liposarcomas was larger than that of leiomyosarcomas; however, the recurrence-free survival was better in patients with liposarcoma than in those with leiomyosarcoma.
Conclusion
Our results showed the clinical features and prognoses of retroperitoneal and abdominal STS in Japan. Further large-scale nationwide studies are required to clarify the detailed clinical behavior of retroperitoneal and abdominal STS in Japan.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Soft tissue sarcomas (STS) are rare mesenchymal neoplasms arising from nonepithelial connective tissue sources. STS are a heterogeneous group of tumors with a wide range of clinical features, behaviors, and prognoses [1]. STS represent only 1% of human malignancies [2], and retroperitoneal and abdominal/visceral STS account for one-third of all STS [3–5].
The clinical characteristics of retroperitoneal and abdominal/visceral STS have been reported mostly from high-volume centers in the United States and Europe [3, 4, 6–8]. Tumor size is considered to be one of the most important prognostic factors in STS [9–13]. The retroperitoneum and abdominal cavity have such a large capacity that tumors can grow without exhibiting any symptoms or recognizable signs on conventional physical examination. This feature, along with their generally noninvasive and slow growth, as well as the paucity of symptoms, contributes to a late presentation and a far-advanced stage at diagnosis. Consequently, STS in the retroperitoneum and abdominal cavity tend to be relatively large compared with those in the extremities or superficial STS, resulting in poor prognoses of retroperitoneal and abdominal STS [6]. Retroperitoneal and abdominal STS, however, have been infrequently reported in Asian countries. In Japan, Hashimoto et al. [14] documented the histomorphological factors and prognoses in 1116 cases of STS, including 186 cases of retroperitoneal and mesenteric STS. However, no systematic analysis concerning the clinical features and prognosis of retroperitoneal and abdominal STS has been done in Japan.
In this study, we retrospectively analyzed the data obtained from patients with retroperitoneal and abdominal STS who underwent surgery at Osaka University and affiliated hospitals, to clarify the clinical features and prognoses of retroperitoneal and abdominal STS in Japan.
Patients and methods
From 1 January 2000 through 31 December 2007, operative and pathological reports from Osaka University Hospital and 14 affiliated hospitals were reviewed to collect data on patients with intraabdominal, visceral, and retroperitoneal STS. Gastrointestinal stromal tumor (GIST) was excluded in this study because its characteristics and treatment modalities are totally different from those of other STS. The pathological specimens were rereviewed and reclassified by pathologists familiar with sarcomas, and 143 patients were selected. In this study, superficial STS in the abdomen and pediatric STS were excluded because of their different clinical behaviors and prognoses. Thus, data from 82 adult patients who had undergone surgery for abdominal STS were finally included in this study.
Potential prognostic factors including age at initial visit, gender, initial symptoms, location of the main tumor, presentation, curability of surgery, operative status, and tumor size were checked. Tumor size was measured in the resected specimen, or if not completely resected, by radiological examination. Histological subtypes were diagnosed by H&E staining and immunohistochemical staining, using KIT, CD34, α-smooth muscle actin, desmin, S-100, and Ki-67. Because of the limited number of patients involved in this study, we assessed histological grade by a 2-tier system. Tumors were graded according to the French Federation of Cancer Centres system [15], and grade 1 tumors were classified as low grade and grades 2 and 3 were classified as high grade, as suggested by Deyrup and Weiss [10]. The Ki-67 labeling index was used to measure cellular proliferation. Postsurgical management and follow up were done according to the therapeutic strategies of each institution and hospital. Survival was calculated from the date of surgery to the date of last contact or death.
Statistical analysis was performed with Statview ver. 5.0 (SAS Institute, Cary, NC, USA) using Student’s t test, or Fisher’s exact test. Results are expressed as medians and ranges. The logrank test was used to compare survival within the variables studied. These comparisons were performed on an intention-to-treat basis. Statistical significance was defined as p < 0.05.
Results
Patient demographics
Patient demographics and clinical characteristics are presented in Table 1. There were 34 male and 48 female patients, with a median age of 60 years (range, 22–83 years). More than half of the STS (n = 51, 62.2%) were located in the retroperitoneum and 31 cases were in the abdominal cavity or visceral organs. With regard to previous medical history, 69 patients (84.1%) had had no prior surgical treatment, and 13 patients (15.9%) had undergone a prior treatment. Initial presentation included 27 patients with an abdominal mass, 19 with abdominal pain, 8 with bleeding, 10 unknown, 6 “others”, and 12 (14.6%) patients without any symptoms in whom the diseases were discovered incidentally by radiographic examinations. Pathological examinations showed 32 (39.0%) leiomyosarcomas, 30 (36.6%) liposarcomas, 10 (12.2%) malignant fibrous histiocytomas (MFH), and 10 (12.2%) tumors that were categorized as “miscellaneous other”. The histological grade was low in 44 patients, high in 31, and unknown in 7. The Ki-67 labeling index ranged from 1 to 80% (median 10%) in 64 patients. The median size of the tumors was 11 cm (range, 1.5–38 cm). Distant metastasis at diagnosis was observed in 11 patients, with peritoneal dissemination observed at diagnosis in 10 patients. Macroscopic complete resection was carried out in 63 patients (76.8%) and 19 patients underwent macroscopically noncurative resection. The median follow-up period was 2.0 years (range 0.1–8.9 years).
Prognosis after surgery
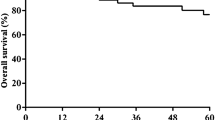
The overall survival (OS) and recurrence-free-survival (RFS) of the entire cohort are shown in Fig. 1a. The 1-, 3-, and 5-year OS was 92.1% (95% confidence interval [CI]; 95.2–89.0%), 68.6% (95% CI; 62.5–74.7%), and 62.2% (95% CI; 55.2–69.2%), respectively. After complete resection, the 1-, 3-, and 5-year RFS of all patients were 72.6% (95% CI; 79.1–66.1%), 34.1% (95% CI; 26.0–42.2%), and 22.7% (95% CI; 14.2–31.2%), respectively. In patients with complete resection, the 5-year OS was 67.1%, whereas it decreased to 46.9% in those with incomplete resection (Fig. 1b). Local recurrences (n = 22), distant metastatic recurrences (n = 17), or peritoneal disseminations (n = 9) were observed in 45 patients, including patients with more than one site (Table 2). Treatment for recurrences included surgery in 27 patients, surgery after neoadjuvant chemotherapy in 2 patients, chemotherapy in 3 patients, transarterial chemoembolization for liver metastasis in 1 patient, radiotherapy for bone metastasis in 1 patient, and best supportive care in 6 patients. In seven patients, the details of their treatment were unknown.
Next, we evaluated the prognostic impact of histological subtypes. The 3-year OS rates of liposarcoma, leiomyosarcoma, MFH, and others were 83.5, 70.1, 33.3, and 65.6%, respectively (Fig. 2a) and the 3-year RFS of liposarcoma, leiomyosarcoma, MFH, and others were 58.9, 10, 33.3, and 0%, respectively (Fig. 2b). We analyzed OS and RFS according to the histological grade. The 3-year OS rates of low-grade and high-grade sarcomas were 77.8 and 50.6%, respectively (Fig. 3a) and the OS of low-grade sarcoma was significantly better than that of high grade (p = 0.0182). The 3-year RFS rates of low-grade and high-grade sarcomas were 42.3 and 29.3% (Fig. 3b). Next, we evaluated OS and RFS according to the Ki-67 labeling index. Patients were divided into two groups, less than 10: Ki-67 labeling index was less than 10%, and more than 10: the index was more than 10%. The 3-year OS rates of the less than 10 and more than 10 groups were 72.9 and 60.1%, respectively (Fig. 4a). The 3-year RFS rates of the less than 10 and more than 10 groups were 55.3 and 26.0%, respectively (Fig. 4b). Because of the limited sample size, the following prognostic analysis was undertaken for patients with leiomyosarcoma and liposarcoma. No differences in terms of age, presentation, distant metastasis at diagnosis, peritoneal dissemination, and follow-up period were observed between patients with leiomyosarcoma and those with liposarcoma (Table 3). Leiomyosarcomas were located both in the retroperitoneum and in the abdominal cavity (50.0 and 50.0%, respectively), whereas most of the liposarcomas (83.3%) were located in the retroperitoneum (Table 3). The tumor size of the liposarcomas was significantly larger (median, 17 cm; range, 3.8–38 cm) than that of the leiomyosarcomas (median, 8 cm; range, 1.5–16 cm). The histological grade was significantly higher in leiomyosarcomas compared with liposarcomas. The Ki-67 labeling index was higher in leiomyosarcomas (median, 25.0%; range, 1–80%) than in liposarcomas (median, 5%; range 1–50%). Complete resection was performed in 26 patients (86.6%) with liposarcoma and in 24 patients (75.0%) with leiomyosarcoma (Table 3). The 3- and 5-year RFS of liposarcoma was 58.9 and 35.4%, respectively, whereas that of leiomyosarcoma was 10.0 and 10.0%, respectively (Fig. 2b). The RFS of liposarcoma was significantly better than that of leiomyosarcoma (p = 0.022). As for recurrence, 15 of the patients with leiomyosarcoma developed distant metastases, whereas no patient with liposarcoma developed distant metastases (Table 2). Of the patients with liposarcoma, 12 (85.7%) suffered from local recurrence. Two of them also had peritoneal dissemination. For the recurrence 10 of 12 patients with liposarcoma and 10 of 16 patients with liposarcoma underwent repeated surgery. The OS was similar for liposarcoma and leiomyosarcoma (Fig. 2a).
Discussion
STS are a heterogeneous group of mesenchymal tumors showing various histological types, each of which was exhibited in a small number of patients. Genetic mutations have been reported in some STS; however, no standard treatment based on genotype is known, except for GIST. One-third of STS occur in the retroperitoneum or abdominal cavity. Some large-scale studies from the United States have documented these rare tumors [3, 4, 8, 16] and have clarified the clinicopathological features of STS in Western countries. There is, however, only one report [14] concerning retroperitoneal and abdominal STS from Asia, including Japan.
In the present study, we analyzed the clinicopathological features and prognoses of retroperitoneal and abdominal STS. As for the clinical features of patients in this study, age, gender, previous medical history, initial presentation, histology, and the rate of complete resection were similar to these features in previous Western reports [3, 7, 16]. The median tumor size of 11 cm in the present study was slightly smaller than that reported previously [3, 4, 7, 17]. The resection rate in our study was 77% and the 5-year OS was 62%, suggesting relatively favorable results compared with previous reports of a 5-year OS of 50% [4, 8, 16]. Histological grade and the Ki-67 labeling index are considered to be very important prognostic factors [4, 18, 19]. We analyzed the impact of the histological grade the Ki-67 labeling index on OS and RFS. The OS rate in the low-grade group was significantly higher than that in the high-grade group. However, we did not detect a significant difference in RFS in relation to either of these factors.
Liposarcoma and leiomyosarcoma are the major STS in the retroperitoneum and abdominal cavity. We compared their clinical features and outcomes after surgery. Liposarcomas were found to be larger tumors than leiomyosarcomas:, however the RFS of liposarcoma was better than that of leiomyosarcoma. This seems to be mainly due to differences in the biological malignant potential and behavior of these tumors. In fact, the histological grade and Ki-67 labeling index of liposarcomas were significantly lower than those of leiomyosarcomas. Most of the liposarcomas recurred at local sites, and distant metastasis was rare in liposarcoma patients after complete resection. This is especially true for well-differentiated liposarcoma. Bautista et al. [6] documented that multiple surgical resections for repeated local recurrence may yield a substantial survival benefit for patients with liposarcoma. Thus, aggressive surgical resection of local recurrence may result in the long-term survival of patients with retroperitoneal and abdominal liposarcoma.
The rarity of leiomyosarcoma, liposarcoma, and MFH makes it difficult to investigate their clinical behaviors. Some large-scale studies have documented these rare tumors in the United States [3, 4, 8, 16]. There is no large-scale study concerning the clinical characteristics and surgical outcomes of retroperitoneal and abdominal STS in Japan. To elucidate the clinical characteristics and outcomes in Japan, a large-scale nationwide study of retroperitoneal and abdominal STS is required.
In summary, the present study examined, retrospectively, the clinical features and prognoses of retroperitoneal and abdominal STS in Japanese patients. The OS and RFS of leiomyosarcoma and liposarcoma appeared to be favorable compared with results in previous reports from the United States and Europe. A large-scale prospective study of Japanese sarcoma patients is required for the clarification of the clinical characteristics and outcomes of retroperitoneal and abdominal STS in Japan.
References
Borden EC, Baker LH, Bell RS et al (2003) Soft tissue sarcomas of adults: state of the translational science. Clin Cancer Res 9:1941–1956
Kotilingam D, Lev DC, Lazar AJ et al (2006) Staging soft tissue sarcoma: evolution and change. CA Cancer J Clin 56:282–291 (quiz pp 314–315)
Dalal KM, Kattan MW, Antonescu CR et al (2006) Subtype specific prognostic nomogram for patients with primary liposarcoma of the retroperitoneum, extremity, or trunk. Ann Surg 244:381–391
Gutierrez JC, Perez EA, Franceschi D et al (2007) Outcomes for soft-tissue sarcoma in 8249 cases from a large state cancer registry. J Surg Res 141:105–114
Windham TC, Pisters PW (2005) Retroperitoneal sarcomas. Cancer Control 12:36–43
Bautista N, Su W, O’Connell TX (2000) Retroperitoneal soft-tissue sarcomas: prognosis and treatment of primary and recurrent disease. Am Surg 66:832–836
Pacelli F, Tortorelli AP, Rosa F et al (2008) Retroperitoneal soft tissue sarcoma: prognostic factors and therapeutic approaches. Tumori 94:497–504
Perez EA, Gutierrez JC, Moffat FL Jr et al (2007) Retroperitoneal and truncal sarcomas: prognosis depends upon type not location. Ann Surg Oncol 14:1114–1122
Coindre JM, Terrier P, Guillou L et al (2001) Predictive value of grade for metastasis development in the main histologic types of adult soft tissue sarcomas: a study of 1240 patients from the French Federation of Cancer Centers Sarcoma Group. Cancer 91:1914–1926
Deyrup AT, Weiss SW (2006) Grading of soft tissue sarcomas: the challenge of providing precise information in an imprecise world. Histopathology 48:42–50
Kilkenny JW 3rd, Bland KI, Copeland EM 3rd (1996) Retroperitoneal sarcoma: the University of Florida experience. J Am Coll Surg 182:329–339
Miyajima K, Oda Y, Oshiro Y et al (2002) Clinicopathological prognostic factors in soft tissue leiomyosarcoma: a multivariate analysis. Histopathology 40:353–359
Oda Y, Tamiya S, Oshiro Y et al (2002) Reassessment and clinicopathological prognostic factors of malignant fibrous histiocytoma of soft parts. Pathol Int 52:595–606
Hashimoto H, Daimaru Y, Takeshita S et al (1992) Prognostic significance of histologic parameters of soft tissue sarcomas. Cancer 70:2816–2822
Trojani M, Contesso G, Coindre JM et al (1984) Soft-tissue sarcomas of adults; study of pathological prognostic variables and definition of a histopathological grading system. Int J Cancer 33:37–42
Anaya DA, Lahat G, Wang X et al (2009) Establishing prognosis in retroperitoneal sarcoma: a new histology-based paradigm. Ann Surg Oncol 16:667–675
Gronchi A, Lo Vullo S, Fiore M et al (2009) Aggressive surgical policies in a retrospectively reviewed single-institution case series of retroperitoneal soft tissue sarcoma patients. J Clin Oncol 27:24–30
Coindre JM (2006) Grading of soft tissue sarcomas: review and update. Arch Pathol Lab Med 130:1448–1453
Ueda T, Aozasa K, Tsujimoto M et al (1989) Prognostic significance of Ki-67 reactivity in soft tissue sarcomas. Cancer 63:1607–1611
Acknowledgments
We thank Dr. Iwase: Osaka General Medical Center, Dr. Akamatsu: Osaka Police Hospital, Dr. Izukura: Rinku General Medical Center, Dr. Koseki: National Hospital Organization Kure Medical Center, Dr. Tsukahara: Toyonaka Municipal Hospital, Dr. Tamura: Kansai Rosai Hospital, Dr. Yano: Osaka Medical Center for Cancer and Cardiovascular Diseases, Dr. Nagaoka: Social Insurance Kinan Hospital, Dr. Nezu: Osaka Rosai Hospital, Dr. Nakaba: Otemae Hospital, Dr. Yamasaki: Osaka Kosei-Nenkin Hospital, Dr. Hiratsuka: Itami City Hospital, and Dr. Yano: NTT West Osaka Hospital for providing patients’ data.
Conflict of interest statement
Toshirou Nishida received a research grant from Novartis. The other authors have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Nishimura, J., Morii, E., Takahashi, T. et al. Abdominal soft tissue sarcoma: a multicenter retrospective study. Int J Clin Oncol 15, 399–405 (2010). https://doi.org/10.1007/s10147-010-0075-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10147-010-0075-4