Abstract
Purpose
With the aim to determine effective therapeutic window of electrochemotherapy, we analyzed bleomycin pharmacokinetic parameters in elderly patients.
Methods
In prospective clinical study in the treatment of tumors with electrochemotherapy, blood samples of patients older than 65 years were collected after the bolus intravenous injection of bleomycin (15,000 IU/m2). In serum samples, quantitative analysis was performed with liquid chromatography coupled to high-resolution mass spectrometry. Based on the data, the pharmacokinetic parameters of bleomycin elimination were determined.
Results
Pharmacokinetic analysis of the data revealed a monophasic serum clearance curve, which demonstrates slow elimination of bleomycin, being less than 500 ml/min and a half-time of 30 min.
Conclusions
Slow monophasic elimination of bleomycin from serum in elderly patients implies on the longer therapeutic window, from 8 to up to 40 min or even longer post-bleomycin injection for electrochemotherapy. However, prolonged therapeutic bleomycin serum concentrations may also affect the possible adverse effects, such as lung fibrosis and extensive necrosis of tumors due to the uptake of toxic bleomycin concentrations into the tumors. This may imply on lowering of bleomycin dosage, in particular in the elderly patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
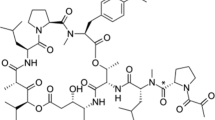
Bleomycin, a fermentation product of Streptomyces verticullus, is an unusual cytotoxic drug. The drug is a mixture of 2-copper-chelating peptides, bleomycins A 2 and B 2 differing in terminal amino acid. Bleomycin is not very often used in chemotherapeutic regimens; however, it proved effective for Hodgkin lymphoma, testicular tumor and Kaposi’s sarcoma [1]. Skin and lung are the main organs affected by bleomycin toxicity, and bleomycin-induced pneumonitis is a limiting factor for its use as chemotherapeutic agent [2].
Due to hydrophilic nature, the entry of bleomycin into the cells is very restricted and it enters the cells only via an endocytotic process [3]. In the cell, bleomycin action requires the presence of oxygen and a reducing agent; the metal-containing bleomycin becomes activated and functions as ferrous oxidase. Bleomycin causes oxidative damage to deoxyribose of nucleotides. In particular, the deoxyribose of thymidylate leads to single- and double-stranded breaks in DNA. Multiple DNA breaks lead to cell apoptosis [4].
Bleomycin is degraded by a specific hydrolase found in various normal tissues, including the liver. However, the activity of this enzyme is low in skin and lung, leading to tissue-specific toxicity. Bleomycin-resistant tumor cells have either increased hydrolase activity, decreased ability to take up bleomycin, efficient strand break repair mechanisms or inactivate bleomycin using thiols or thiol-rich compounds [5, 6].
Bleomycin is not absorbed from the gut and must be given by either bolus intravenous (i.v.), subcutaneous (s.c.) or intramuscular (i.m.) injection, continuous infusion or locally (e.g., into the tumor). Half to two-thirds of administered bleomycin is excreted by the kidneys, so renal insufficiency can delay bleomycin elimination. Reports regarding elimination half-time of bleomycin are scarce and not conclusive. There are reports about monophasic elimination (half-time 3 h) [7], 155 min [8] after intramuscular application, 5 h [9] and 6 h after intraperitoneal application [10] and biphasic elimination (initial half-time 0.26 h and terminal half-time 2.3 h) after intravenous injection [11].
Recently, bleomycin use has been revived by its employment in a therapy termed electrochemotherapy, for the treatment of various cancer histiotypes [12, 13]. Namely, electrochemotherapy is based on the use of electroporation, a physical method, where application of defined electric pulses to the tumor tissue enhances the cell membrane permeabilization and consequently significantly increases the cellular uptake of bleomycin [14]. In preclinical studies, its cytotoxicity was potentiated several thousand-fold by the use of electroporation [12]. Thus, the effective cytotoxic dose of bleomycin can be significantly lowered, compared to the dose used in standard chemotherapeutic regimens [12]. Currently, electrochemotherapy is used in many European oncological centers for treatment of mainly skin cancers and skin metastases in elderly patients [15]. However, despite high local effectiveness of electrochemotherapy, certain open questions regarding the optimization of treatment remain to be elucidated. One of them is the time interval between the intravenous bolus injection of bleomycin and application of electric pulses (8–28 min), which was set empirically, based on the observed antitumor effect in one patient [16], and is currently used in standard operating procedures for electrochemotherapy [17].
Due to the lack of a reliable method to determine bleomycin in tissues and blood, the pharmacology parameters for optimal electrochemotherapy have not been set yet. For this purpose, we developed a method for bleomycin determination, based on modern analytical methods, to determine bleomycin in serum and calculate pharmacokinetic parameters in elderly cancer patients (>65 years), who received bleomycin intravenously for treatment of tumors located in the head and neck region with electrochemotherapy. Based on the data, a prolongation of the effective therapeutic window of electrochemotherapy is indicated for the elderly patients.
Patients and methods
Patients
The prospective study was conducted between March 2014 and February 2015 on 24 patients with non-melanoma skin cancers or recurrent and/or metastatic disease or second primary tumor in the head and neck region, who were not suitable for conventional treatments or refused them. All patients were treated with electrochemotherapy at the Department of Otorhinolaryngology and Cervicofacial Surgery, University Medical Centre, Ljubljana, Slovenia. The study was approved by the National Ethics Committee of the Republic of Slovenia (182/02/14). The treatment with electrochemotherapy was previously agreed by multidisciplinary board, and written informed consents were obtained from all eligible patients. All the inclusion criteria (biopsy-verified cancer, lesions suitable for application of electric pulses, age >18 years, life expectancy >3 months) and none of the exclusion criteria (bone invasion, major blood vessel infiltration, bleomycin hypersensitivity, cumulative bleomycin dose >240,000 IU, pregnancy, chronic renal dysfunction, uncontrolled coagulation disorders, acute lung infection or symptoms of poor lung function) were met.
A total of 24 patients (11 males, 13 females) with 47 tumor nodules were treated with electrochemotherapy for cancers in the head and neck region. The mean patient age was 78 years (range, 65–89). Among all the patients, 17 underwent electrochemotherapy due to either basal or squamous cell skin cancer. Four patients had deep-seated metastases in the neck, two patients had recurrent oropharyngeal cancer, and one patient had secondary primary tumor of the oral cavity (Table 1). Response to treatment was evaluated according to the RECIST criteria 1.1 3 months after electrochemotherapy. (Table 1) [18].
Procedure
The procedure was performed according to the standard operating procedures for electrochemotherapy [17] under general anesthesia. The procedure consisted of bolus (in 2 min) intravenous injection of bleomycin (Bleomycin medac, Medac, Wedel, Germany) in a dose of 15,000 IU/m2 body surface area (1000 IU is equal to the 1 mg of bleomycin activity). The application of electric pulses was 8 min after the injection of bleomycin, predominantly by electrodes with fixed geometry (hexagonal, needle row or plate electrodes), and three patients were treated by long needle electrodes with the aid of treatment plan and navigation system [19]. Electric pulses for electrochemotherapy were generated by Cliniporator pulse generator (IGEA, s.r.l., Carpi, Italy). For hexagonal electrodes 12 pulses with voltage 730 V, pulse duration 100 µs and frequency 5000 Hz were applied, for needle row eight pulses with voltage 400 V, pulse duration 100 µs and frequency 5000 Hz were applied, and for plate electrodes eight pulses with voltage 720 V (for 6 mm electrodes) or 960 V (for 8 mm electrodes), pulse duration 100 µs and frequency 5000 Hz were applied [15, 20]. Pulse parameters for tumors treated with long single-needle electrodes were adjusted for each patient separately, according to personalized treatment plan. Five single-needle electrodes were used, one placed in the tumor center while other four around the tumor to cover also the safety margin. In general, eight pulses with voltage 1000–1800 V (voltage varied between each electrode pair), pulse duration 100 µs and frequency 5000 Hz were applied.
Blood samples collection
Two milliliters of arterial blood sample were taken from each patient at predetermined time pull points (5, 10, 20, 30 and 40 min after bleomycin administration, where 0 is a time of bleomycin injection) into the blood collection tubes (BD Vacutainer, Franklin Lakes, New Jersey, USA). Samples were centrifuged at 3000 rpm for 10 min at room temperature. Serum was carefully transferred to a new Eppendorf tube (Golias Labortehnika, Ljubljana, Slovenia), and all samples were stored at −20 °C until they were analyzed.
Chemical analysis
Sample preparation
Serum samples were prepared for analysis by solid-phase extraction using Oasis HLB 30 mg/1 cc cartridges (Waters Corp., Milford, MA, USA). The cartridges were preconditioned with 1 ml of methanol and equilibrated with MilliQ water acidified to pH 2 with hydrochloric acid. 200 µl samples were diluted to 3 ml with 0.1 % formic acid and filtered through 0.45-μm Minisart® NML (Sartorius, Göttingen, Germany) surfactant-free cellulose acetate syringe filters. After the sample filtrates were loaded onto the cartridges, the sorbent was dried under vacuum for 30 min and subsequently eluted using 0.5 ml of MilliQ water/methanol (6/4) and twice with 0.5 ml acetonitrile solution containing 1 µg/ml methotrexate. The latter drug was employed as an internal standard. As follows, the sample extracts were blown down to 1 ml using nitrogen and were then kept frozen until LC–MS analysis, which was performed within 1 month.
Instrumental analysis
Quantitative analysis was performed with Waters Acquity ultra-performance liquid chromatograph (UPLC, Waters Corp., Milford, MA, USA) coupled to a Waters Premier hybrid quadrupole orthogonal acceleration time-of-flight mass spectrometer (QTOF MS). The UPLC was equipped with a binary solvent delivery system and an auto sampler. The injection volume was 7.5 µl. Separation was achieved at 40 °C by using a 5-cm-long Acquity UPLC® BEH Amide (Waters Corp.) column with 1.7 μm particle size and 2.1 mm internal diameter. Bleomycin was analyzed under electrospray ionization in positive mode. The mobile phases were (A) 10 mM ammonium formate with 0.1 % formic acid and (B) acetonitrile. The gradient started with 90 % B, which was decreased to 40 % in 4 min, increased back to 90 % in 0.5 min and kept so until 6 min. The flow rate was 0.3 ml/min. The UPLC system was coupled to QTOF MS equipped with an electrospray ionization interface. The capillary voltage was set to 3.0 kV, while the sampling cone voltage was 30 V. The source and desolvation temperatures were set to 130 and 350 °C, respectively. The nitrogen desolvation gas flow rate was 600 l/h. The first quadrupole was operated in rf-only mode, while detection was performed in the TOF mass analyzer. MS data were acquired over a m/z range of 450–750 at a collision energy of 5 V. Data were collected in a centroid mode, with a scan accumulation time set to 0.200 s and an interscan delay of 0.025 s. The data station operating software was MassLynx v4.1. Prior to analysis, the instrument was calibrated over a mass range of 50–1000, using a sodium formate calibration solution. Reproducible and accurate mass measurements at a mass resolution of 10 000 FWHM were obtained using an electrospray dual sprayer with leucine enkephalin ([M + H]+ 554.2615, [M − H]− 556.2271) as the reference compound. The latter was introduced into the mass spectrometer alternating with the sample via a Waters Lock Spray device. For bleomycin, its ion at m/z 707.2109 ± 5 ppm was followed.
The validation of the analytical method proved the inherent selectivity, sensitivity (lower limit of detection 50 ng/ml), linearity (R 2 0.99), precision (injection repeatability RSD 1.1–2.6 %, method repeatability RSD 2.5–9.4 %), accuracy (RSD 5.5 %) and stability (1 month freeze–thaw) of the analytical method.
Pharmacokinetic data analysis
Bleomycin serum concentrations versus time of each patient and combined data of all 24 patients were analyzed. We determined the following pharmacokinetic parameters:
C 0 (concentration of bleomycin in serum at the time 0) value was extrapolated from ln concentration versus time plot for each patient as well as for the pooled data. Further on, the area under the serum concentration–time curve (AUC) was calculated using the trapezoid method from time 0 to infinity (∞)(AUC0→∞) and serum clearance (CL) calculated.
Elimination rate constant k el was determined from the slope of ln (concentration) versus time curve and half-time was calculated using
and volume of distribution
Results
Patients’ characteristics
In the study were included 24 patients older than 65. These elderly patients were treated with electrochemotherapy using bleomycin, given intravenously by bolus injection. This patient population was used for the pharmacological study of bleomycin. For this purpose, patients gave blood samples on several time points, and bleomycin was determined in sera of these patients (Table 1).
Pharmacokinetics data
Bleomycin concentrations in patients’ sera were determined by the new analytical method, using liquid chromatography coupled to high-resolution mass spectrometry. The blood sample was taken from each patient at predetermined time pull points (5, 10, 20, 30 and 40 min after bleomycin administration, where 0 is a time of bleomycin injection).
Based on the data, the pharmacokinetic parameters of bleomycin elimination were determined. Serum concentration–time profile following intravenous bolus administration of bleomycin is shown in Fig. 1.
Following a single bolus injection of bleomycin (23,000–30,000 IU i.v., mean dose 25,625 ± 437 IU), serum concentration after 5 min was 3.133 ± 0.129 mg/l.
The concentration of bleomycin declined gradually with elimination constant (k el) of 0.023 min−1 and reached the value of 1.417 ± 0.065 mg/l at 40 min after injection.
The disappearance of bleomycin from the serum of elderly (>65 years old) patients fits best to the first-order elimination kinetics. The apparent volume of distribution (Vd), area under the curve (AUC) and total body clearance (CL) were calculated to be: 12.98 l, 86.20 mg min/l and 300 ml/min, respectively. Elimination half-time of bleomycin in the elderly was 30 min.
Discussion
Bleomycin concentrations after a single intravenous bolus dose were determined in serum by a new analytical method in elderly patients with head and neck cancers aged more than 65. Pharmacokinetic analysis of these data revealed a monophasic serum clearance curve, which demonstrates slower elimination of bleomycin, being less than 500 ml/min [21] and a half-time of 30 min. Our data are not in accordance with previously determined pharmacokinetic parameters of bleomycin, showing biphasic plasma elimination in pediatric and adult patients. In both studies, the bleomycin plasma concentrations were determined with radioimmunoassay and elimination half-times of bleomycin were found to be 20 min and 3.2 h in pediatric patients receiving the dose of 20–30 mg of bleomycin/m2 [22] and 24.4 min and 4 h in adult patients who were administered 13.7–19.9 U/m2 [23].
Our study demonstrates new pharmacokinetic parameters values of bleomycin that are specific for the elderly population of patients, older than 65 years. Aging is manifested by progressive, but not uniform impairment of body functions. The most consistent is the age-dependent loss of functional units (e.g., nephrons, alveoli, neurons) and different composition of the organism [24]. With advancing age, significant changes in body composition occur. There is a progressive decline in the total body water and lean body mass, resulting in a relative increase in body fat [25]. This affects the distribution parameters of water-soluble drugs, including bleomycin, which volume of distribution is reduced in the elderly and consequently higher plasma or serum levels are achieved, as it is observed in our case. The reduction in volume of distribution of water-soluble drugs in the elderly patients is at least partly balanced by the reduced rate of the clearance, so the elimination half-time is not significantly prolonged. Despite the decline in glomerular filtration rate, this feature is not accompanied by a concomitant increase in plasma creatinine, because the production of creatinine is decreased due to age-related reduction in skeletal muscle mass. Also, our patient population had normal creatinine levels. Another, a more reliable marker of glomerular filtration rate than plasma creatinine level monitoring should be used in the elderly population.
Bleomycin determination is now possible with new and sophisticated analytical approaches and can be determined with high specificity also in low concentrations. By using high-resolution mass spectrometry for detection, this analytical method is able to distinguish between the bleomycins A 2, B 2 and other minor bleomycin fractions, as well as between metal-free bleomycin, its copper chelates and other metal complexes. The method briefly described here and in extension in a publication in submission was developed to measure bleomycin in serum samples of patients given in a bolus injection. The bolus injection is used in treatment with electrochemotherapy. This new method for bleomycin determination could be further adapted for the determination of the drug within the tumors. Such studies could also provide evidence of the minimal drug concentration in the tumors for effective electrochemotherapy with bleomycin.
Electrochemotherapy is a already well-established local ablative technique that utilizes electroporation for bleomycin delivery to cells in the tumors [12, 26]. It is being used for the treatment of cutaneous and also deep-seated tumors in over 150 cancer centers over Europe [15, 27]. The approach is based on intravenous bolus injection of 15,000 IU/m2 bleomycin, and after 8 min electric pulses are applied to the tumors to be treated, in order to increase bleomycin uptake into the cells. The 8-min interval is needed for the drug to distribute in the tumor tissue [17]. Based on the initial study of Mir et al. [17], a therapeutic window of 20 min (8–28 min post-drug injection) was determined, a time frame in which adequate concentration of bleomycin can be taken up into tumors to obtain good tumor response, and is currently used in clinical protocols according to the standard operating procedures. However, the study was performed on a single patient where several nodules were treated over time, and based on the tumor response this therapeutic window was determined [16]. Due to the lack of suitable methods to measure serum and tumor bleomycin concentrations, a pharmacological study was not possible. Thus, the results of the present study have several important clinical implications.
The elimination rate of bleomycin in elderly patients indicates that the therapeutic window of 20 min, starting 8 min from the bleomycin intravenous injection for electrochemotherapy, can be prolonged. The results of our study determine prolonged therapeutic window at least up to 40 min. Due to the slow elimination rate of bleomycin, the therapeutic window for electrochemotherapy could be even longer than 40 min, but we must determine first the uptake of bleomycin in tumors, when lower plasma concentrations of bleomycin are present (less than 40 % of maximal plasma concentration). Most of the patients that are treated with electrochemotherapy are elderly patients and the majority of them also heavily pre-treated [13, 28]. So, this observation applies to the vast majority of patients treated with electrochemotherapy and is clinically important, since electrochemotherapy is often used also in the treatment of multiple metastases, and deep-seated tumors, like in the liver. The prolongation of the therapeutic window is primarily important in the treatment of multiple metastases and when more time for the placement of the electrodes is needed [29, 30].
Skin belongs to highly perfused tissues of the human body. Its perfusion with bleomycin starts a few moments after intravenous injection, but its therapeutic concentration is achieved later; therefore, a choice for 8-min time frame to begin electrochemotherapy is justified. However, the optimal time at which the application of electric pulses should start in other organs needs to be determined.
Besides the implication on the therapeutic window of electrochemotherapy, these data raise questions about the bleomycin dosage for electrochemotherapy and the possible adverse effects. In the SOP for electrochemotherapy, a dose of 15,000 IU/m2 is prescribed. Based on the pharmacological parameters, we suggest that the dose of bleomycin could be reduced to 10,000 IU/m2, with equally good antitumor effect in the elderly patients. In the first clinical studies [31], a dose of 10,000 IU was used and then changed to 15,000 IU/m2 based on comparison of the effects between the two doses used [16]. We have to question these data and its interpretation and based on our pharmacological data, we recommend to reduce the dose to 10,000 IU. However, it has to be confirmed with clinical evidence.
Prolonged higher bleomycin levels can also have clinically negative implications. Bleomycin can induce lung fibrosis, which was not reported in electrochemotherapy. However, it has to be taken into account that such side effects can be attributed also to electrochemotherapy with bleomycin, specifically after multiple consecutive sessions.
Tumor drug accumulation is also affected by the pharmacokinetics of bleomycin. In this respect, slower elimination rate results in prolonged blood circulation of bleomycin and eventually in higher concentration of bleomycin within the tumors. Therefore, we have to conduct studies to determine how the changed pharmacokinetics affects the bleomycin deposition and efficacy in tumors. Further on, it should be investigated which bleomycin concentration is still effective and does not cause tissue ulceration. It is known that high concentrations of bleomycin in the cells induce necrotic cell death, whereas the lower ones induce apoptotic or mitotic like cell death [32]. Therefore, in some over reactions in tumor responses, a toxic intratumor bleomycin concentration might have been reached, due to slower clearance of the bleomycin, resulting in extensive tumor necrosis.
To our best knowledge, this is the first study on pharmacokinetics of bleomycin in elderly patients after a bolus injection. The data are based on the newly developed analytical method for determination of bleomycin in serum samples in the patients, with high specificity and sensitivity. Slower monophasic elimination of bleomycin was determined. The data imply on longer therapeutic window, from 8 min to up to at least 40 post-bleomycin injection for electrochemotherapy in elderly patients. However, prolonged bleomycin serum concentration may also affect the possible adverse effects of the electrochemotherapy with bleomycin, such as lung fibrosis and the overdosing of bleomycin in tumors resulting in tumor exulceration in such patients. To avoid this, lowering of the bleomycin dosage in electrochemotherapy should be considered, in particular in the elderly patients.
References
Fyfe AJ, McKay P (2010) Toxicities associated with bleomycin. J R Coll Phys Edinb 40:213–215. doi:10.4997/JRCPE.2010.306
Della Latta V, Cecchettini A, Del Ry S, Morales MA (2015) Bleomycin in the setting of lung fibrosis induction: from biological mechanisms to counteractions. Pharmacol Res 97:122–130. doi:10.1016/j.phrs.2015.04.012
Pron G, Mahrour N, Orlowski S, Tounekti O, Poddevin B, Belehradek J, Mir LM (1999) Internalisation of the bleomycin molecules responsible for bleomycin toxicity: a receptor-mediated endocytosis mechanism. Biochem Pharmacol 57:45–56. doi:10.1016/S0006-2952(98)00282-2
Sugiura Y, Uesawa Y, Takahashi Y, Kuwahara J, Golik J, Doyle TW (1989) Nucleotide-specific cleavage and minor-groove interaction of DNA with esperamicin antitumor antibiotics. Proc Natl Acad Sci USA 86:7672–7676
Ferrando AA, Velasco G, Campo E, Lopez-Otin C (1996) Cloning and expression analysis of human bleomycin hydrolase, a cysteine proteinase involved in chemotherapy resistance. Cancer Res 56:1746–1750
Pron G, Belehradek J Jr, Mir LM (1993) Identification of a plasma membrane protein that specifically binds bleomycin. Biochem Biophys Res Commun 194:333–337. doi:10.1006/bbrc.1993.1824
Buxton IO, Benet LZ (2011) Pharmacokinetics: the dynamics of drug absorption, distribution, metabolism, and elimination. In: Brunton LL, Chabner BA, Knollmann BC (eds) Goodman & Gilman’s the pharmacological basis of therapeutics, 12th edn. McGraw-Hill, New York
Oken MM, Crooke ST, Elson MK, Strong JE, Shafer RB (1981) Pharmacokinetics of bleomycin after im administration in man. Cancer Treat Rep 65:485–489
Bitran JD (1985) Intraperitoneal bleomycin. Pharmacokinetics and results of a phase II trial. Cancer 56:2420–2423
Howell SB, Schiefer M, Andrews PA, Markman M, Abramson I (1987) The pharmacology of intraperitoneally administered bleomycin. J Clin Oncol 5:2009–2016
Hall SW, Strong JE, Broughton A, Frazier ML, Benjamin RS (1982) Bleomycin clinical pharmacology by radioimmunoassay. Cancer Chemother Pharmacol 9:22–25
Sersa G, Miklavcic D, Cemazar M, Rudolf Z, Pucihar G, Snoj M (2008) Electrochemotherapy in treatment of tumours. Eur J Surg Oncol 34:232–240. doi:10.1016/j.ejso.2007.05.016
Testori A, Tosti G, Martinoli C, Spadola G, Cataldo F, Verrecchia F, Baldini F, Mosconi M, Soteldo J, Tedeschi I, Passoni C, Pari C, Di Pietro A, Ferrucci PF (2010) Electrochemotherapy for cutaneous and subcutaneous tumor lesions: a novel therapeutic approach. Dermatol Ther 23:651–661. doi:10.1111/j.1529-8019.2010.01370.x
Yarmush ML, Golberg A, Sersa G, Kotnik T, Miklavcic D (2014) Electroporation-based technologies for medicine: principles, applications, and challenges. Ann Rev Biomed Eng 16:295–320. doi:10.1146/annurev-bioeng-071813-104622
Miklavcic D, Mali B, Kos B, Heller R, Sersa G (2014) Electrochemotherapy: from the drawing board into medical practice. Biomed Eng Online 13:29. doi:10.1186/1475-925X-13-29
Domenge C, Orlowski S, Luboinski B, De Baere T, Schwaab G, Belehradek J Jr, Mir LM (1996) Antitumor electrochemotherapy: new advances in the clinical protocol. Cancer 77:956–963
Mir LM, Gehl J, Sersa G, Collins CG, Garbaya JR, Billarda V, Geertsend PF, Rudolf Z, O’Sullivanf GC, Marty M (2006) Standard operating procedures of the electrochemotherapy: instructions for the use of bleomycin or cisplatin administered either systemically or locally and electric pulses delivered by the CliniporatorTM by means of invasive or non-invasive electrodes. EJC Supp 4:14–25
Eisenhauera EA, Therasseb P, Bogaertsc J, Schwartzd LH, Sargente D, Fordf R, Danceyg J, Arbuckh Gwytheri S, Mooneyg M, Rubinsteing L, Shankarg L, Doddg L, Kaplanj R, Lacombec D, Verweijk J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45:228–247. doi:10.1016/j.ejca.2008.10.026
Groselj A, Kos B, Cemazar M, Urbancic J, Kragelj G, Bosnjak M, Veberic B, Strojan P, Miklavcic D, Sersa G (2015) Coupling treatment planning with navigation system: a new technological approach in treatment of head and neck tumors by electrochemotherapy. Biomed Eng Online 14(Suppl 3):S2. doi:10.1186/1475-925X-14-S3-S2
Campana LG, Mali B, Sersa G, Valpione S, Giorgi CA, Strojan P, Miklavcic D, Rossi CR (2014) Electrochemotherapy in non-melanoma head and neck cancers: a retrospective analysis of the treated cases. Br J Oral Maxillofac Surg 52:957–964. doi:10.1016/j.bjoms.2014.08.004
Kenakin TP (ed) (2014) Tecniques for more effective and strategic drug discovery. In: A pharmacology primer, 4 edn. Academic Press, San Diego, pp 213–253
Yee GC, Crom WR, Lee FH, Smyth RD, Evans WE (1983) Bleomycin disposition in children with cancer. Clin Pharmacol Ther 33:668–673
Alberts DS, Chen HS, Woolfenden JM, Moon TE, Chang SY, Hall JN, Himmelstein KJ, Gross J, Salmon SE (1979) Pharmacokinetics of bleomycin in man. III. Bleomycin 57Co Vs bleomycin. Cancer Chemother Pharmacol 3:33–40
Mangoni AA, Jackson SH (2004) Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 57:6–14
Fulop T, Worum I, Csongor J, Foris G, Leovey A (1985) Body-composition in elderly people. 1. Determination of body-composition by multiisotope method and the elimination kinetics of these isotopes in healthy elderly subjects. Gerontology 31:6–14
Mali B, Jarm T, Snoj M, Sersa G, Miklavcic D (2013) Antitumor effectiveness of electrochemotherapy: a systematic review and meta-analysis. Eur J Surg Oncol 39:4–16. doi:10.1016/j.ejso.2012.08.016
Cadossi R, Ronchetti M, Cadossi M (2014) Locally enhanced chemotherapy by electroporation: clinical experiences and perspective of use of electrochemotherapy. Future Oncol 10:877–890. doi:10.2217/fon.13.235
Valpione S, Campana LG, Pigozzo J, Chiarion-Sileni V (2015) Consolidation electrochemotherapy with bleomycin in metastatic melanoma during treatment with dabrafenib. Radiol Oncol 49:71–74. doi:10.2478/raon-2014-0035
Edhemovic I, Brecelj E, Gasljevic G, Marolt Music M, Gorjup V, Mali B, Jarm T, Kos B, Pavliha D, Grcar Kuzmanov B, Cemazar M, Snoj M, Miklavcic D, Gadzijev EM, Sersa G (2014) Intraoperative electrochemotherapy of colorectal liver metastases. J Surg Oncol 110:320–327. doi:10.1002/jso.23625
Solari N, Spagnolo F, Ponte E, Quaglia A, Lillini R, Battista M, Queirolo P, Cafiero F (2014) Electrochemotherapy for the management of cutaneous and subcutaneous metastasis: a series of 39 patients treated with palliative intent. J Surg Oncol 109:270–274. doi:10.1002/jso.23481
Belehradek M, Domenge C, Luboinski B, Orlowski S, Belehradek J Jr, Mir LM (1993) Electrochemotherapy, a new antitumor treatment. First clinical phase I–II trial. Cancer 72:3694–3700
Mir LM, Tounekti O, Orlowski S (1996) Bleomycin: revival of an old drug. Gen Pharmacol 27:745–748
Acknowledgments
The authors acknowledge the financial support from the state budget by the Slovenian Research Agency (Program Nos. P3-0003, P1-0143, P3-0067, J3-5505, J1-6744). The research was conducted in the scope of LEA EBAM (French–Slovenian European Associated Laboratory: Pulsed Electric Fields Applications in Biology and Medicine) and is a result of networking efforts within COST TD1104 Action. We would like to thank Mira Lavric (Institute of Oncology Ljubljana, Ljubljana, Slovenia) and Biserka Veberic (Department of Otorhinolaryngology and Cervicofacial Surgery, University Medical Centre Ljubljana) for all the valuable work they contributed to this research.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Additional information
Ales Groselj and Mojca Krzan have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Groselj, A., Krzan, M., Kosjek, T. et al. Bleomycin pharmacokinetics of bolus bleomycin dose in elderly cancer patients treated with electrochemotherapy. Cancer Chemother Pharmacol 77, 939–947 (2016). https://doi.org/10.1007/s00280-016-3004-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00280-016-3004-z